Abstract
Background
Posterior tibial tendon (PTT) insufficiency is considered as the main cause of adult acquired flat foot and is three times more frequent in females. High estrogen levels exert a positive effect on the overall collagen synthesis in tendons. We have previously demonstrated the association between some genetic single-nucleotide polymorphism (SNP) and tendinopathy. In the present study, we investigated the association of PvuII c454-397T>C (NCBI ID: rs2234693) and XbaI c454-351A>G (NCBI ID: rs9340799) SNPs in estrogen receptor alfa (ER-α) gene with PPT dysfunction.
Methods
A total of 92 female subjects with PTT dysfunction, with histopathological examination of the tendon and magnetic resonance image (MRI) evidence of tendinopathy, were compared to 92 asymptomatic females who presented an intact PPT at MRI for PvuII and XbaI SNPs in the ER-α gene. Genomic DNA was extracted from saliva and genotypes were obtained by polymerase chain reaction restriction fragment length polymorphism.
Results
The analysis of PvuII SNPs showed no significant differences in the frequency of alleles and genotypes between control and PTT dysfunction groups. The XbaI SNPs in the ER-α gene showed significant differences in the frequency of genotypes between control and test groups (p = 0.01; OR 95% 1.14 (0.55–2.33).
Conclusions
The XbaI SNP in the ERα gene may contribute to tendinopathy, and the A/A genotype could be a risk factor for PTT tendinopathy in this population. The PvuII SNP studied was not associated with PTT tendinopathy.
Similar content being viewed by others
Background
The mechanisms of tendinopathy are complex and involve mechanical stress, degenerative changes in the tendon tissue, and disorganized healing, along with the possible contribution from inflammatory processes. Some studies on the role of estrogens in tendon biology have shown that women are at a higher risk of tendon disorders, with difference according to pre- and post-menopausal status and different phases of the menstrual cycle [1,2,3,4,5,6].
An increase in estrogens exerts a positive effect on the overall collagen synthesis in tendons, while a decrease in the synthesis of collagen fibers can result from estrogens below physiological levels [7, 8]. Estrogen deficiency may contribute to the age-related decrease in the healing capacity of tendons [9] and may interfere with cell proliferation and matrix synthesis [10, 11].
Posterior tibial tendon (PTT) dysfunction is classically considered to lead to adult acquired flatfoot [12], and several risk factors have been proposed. However, many patients present PTT dysfunction without seemingly any of these risk factors or systemic conditions. It is therefore possible that an interaction between the various intrinsic and extrinsic factors with the genetic make-up of a given individual increases the likelihood of that individual developing tendinopathy. There is an association between of genetic single-nucleotide polymorphisms (SNPs) and tendinopathy [13,14,15,16], including PTT dysfunction [17,18,19,20,21].
On the other hand, studies suggest that PTT dysfunction is a consequence and not the origin of adult-acquired flatfoot deformity. The concept of posterior tibial tendon dysfunction as the origin of the deformity is an old paradigm which is being perpetuated in the literature, but we still do not know whether this is the truth [12, 16, 17].
Steroid hormones primarily influence the female reproductive tract, and they are also involved in regulating the metabolism in connective tissues, such as the bone, muscle, and cartilage. The main sources of estrogens are the ovaries and the placenta, but the male testes, the adrenal glands, and several peripheral cells and other tissues, such as osteoblasts, adipocytes, and endothelial cells, also produce small amounts of estrogens [22].
The action of estrogen is predominantly mediated by two classes of estrogen receptor: a rhodopsin-like G protein-coupled receptor, which is located in the endoplasmic reticulum, and two intracellular hormone receptors, namely estrogen receptor alfa and beta (ER-α and ER-β). The latter are members of the nuclear receptor superfamily and are unevenly distributed in many of the estrogen-sensitive tissues.
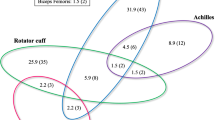
The ER-α gene is located on chromosome 6q25.1. Two well-studied polymorphisms in the ER-α gene are PvuII c454-397T>C (NCBI ID: rs2234693) and XbaI c454-351A>G (NCBI ID: rs9340799) present on intron 1 and commonly called PvuII and XbaI SNPs. These SNPs have been associated to several estrogen-sensitive traits, including osteoarthritis, scoliosis, osteoporosis, rotator cuff tearing, and breast and prostate cancer [23,24,25,26,27,28]. In addition, the presence of ER in the human tenocytes of PTT has been demonstrated [29].
Therefore, the purpose of the present study was to investigate the association of PvuII and XbaI SNPs in ER-α gene in female patients with PPT dysfunction.
Methods
Study population
This is a case–control cross-sectional study which followed the guidelines of the Declaration of Helsinki. The study protocol was approved by our institutional Ethics committee (10166/2013), and written consent was obtained from each participant.
Participants were patients from the Out-patient Clinics at Department of Orthopedics and Traumatology and Department of Gynecology of the University of São Paulo, Brazil. All were female, aged over 40, and post-menopausal, with at least 12 months of amenorrhea and a follicle-stimulating hormone level > 45 mU/mL [30]. All participants underwent standard clinical examination, including medical history, medication use, personal history of systemic diseases, and infectious or inflammatory diseases. Age, body mass index (BMI), hypertension, hypothyroidism, and age at menopause data were also collected.
Participants were divided into two groups:
-
The test group, with 92 post-menopausal females (mean age 59.5 years, range 41–59) who presented PTT dysfunction diagnosed grade II or III (Johnson and Strom Classification System). These patients underwent surgical treatment, and the PTT tendinopathy was confirmed by histopathology (myxoid degeneration associated with multifocal vascular proliferation) and by MRI (T2 image showing intermediate signal intensity and tendon thickening).
-
The control group was composed of 92 asymptomatic post-menopausal females (mean age 63.7 years, range 47–62) with no clinical history of PTT disorders and in whom no signal changes of the PTT were evident at MRI. The target population was females in their fourth to sixth decade of life.
All participants were in good general health and did not present any of the following exclusion criteria: BMI greater than 28, diabetes, rheumatic diseases, immunological disorders, liver or kidney disease, and infection or trauma of the foot and ankle. There were no significant differences between the groups in terms of BMI, hypertension, hypothyroidism, and menopause time (p > 0.05).
Genotyping
DNA from epithelial buccal cells was extracted using the procedure previously described [31]. DNA concentration (ng/μL) was estimated by measurements of optical density 260/280 nm ratio greater than 1.9.
The SNPs had previously been identified and reported in the database of the National Center for Biotechnology Information (http://www.ncbi.nlm.nih.gov/SNP/) with minor allele frequencies greater than 0.4.
Genotyping of ER-α PvuII and XbaI SNPs was performed using the polymerase chain reaction restriction fragment length polymorphism (PCR-RFLP) method. The fragment containing ER-α SNPs was amplified using forward 5′-CGTCTACTCCTATGTCTGGT-3′ and reverse 5-CGTGTAGACTGAAGGGCAT-3′ primers. PCR were carried out in a total volume of 50 μL containing 100 ng of genomic DNA, 50 mM KCl, 0.2 mM dNTPs (dATP, dCTP, dGTP, and dTTP), 5 pmol/μL of each primer, 2 mM of MgSO2, and 0.4 unit of Platinum ®Taq DNA Polymerase High Fidelity (Life Biosciences). The PCR condition was set as follows: 94 °C for 6 min, 40 cycles of 94 °C for 30 s, 54 °C for 45 s, and 72 °C for 45 s, and final extension step of 72 °C for 5 min. Then, PCR products were digested with PvuII and XbaI restriction enzymes (Fermentas, Vilnius, Lithuania) and electrophoresed onto 2% agarose. The gel was stained by ethidium bromide and observed under UV light.
Statistical analysis
Mann–Whitney U and Fisher’s exact test were used to determine any significant differences between ages, BMI, hypertension, hypothyroidism, and menopause time of both groups. The chi-square test was applied to compare the frequencies of alleles and genotypes of SNPs in ER-α gene between patients and controls. The program ARLEQUIN (v. 2.0—Schneider et al. [32]) was used to verify the Hardy–Weinberg equilibrium in the population studied.
Results
All genotype distributions were in Hardy–Weinberg equilibrium. Considering the ER-α PvuII SNPs, there were no significant differences in the frequencies of alleles and genotypes between the control and test groups (Table 1).
The ER-α XbaI SNPs showed significant differences in the frequencies of genotypes between the control and test groups. The A/A genotype was found in 36% of the test group and 18.5% of the control group (p = 0.01; OR 95% 1.14 (0.55–2.33). In the test group, the A allele was observed with a frequency of 57%, while in the control group, the most frequent genotype was the G allele, but this was not statistically different (p = 0.17) (Table 1).
Discussion
Several genes are highly associated with tendinopathy and tendon rupture and may be useful in constructing a targeted gene panel for patients who have had tendon injuries [16].
There is evidence of an association between SNPs in the estrogen-related receptor beta (ERRβ) and tendon disease. ERRβ exhibits constitutive transcriptional activity and is an orphan receptor that shares significant sequence homology with estrogen receptors ERα and ERβ. Motta et al. [33] identified two SNPs (rs4903399 and rs1676303) in the ERRβ gene which were significantly over-represented in rotator cuff patients compared to controls, while Teerlink et al. [34] showed that the SNP rs17583842 in the same gene was significantly associated with rotator cuff tears. Bonato et al. [35] identified that the SNP rs6574293 in the ERRβ gene was associated with temporomandibular disorders. Also, the SNPs rs10132091 and rs4903399 in the ERRβ gene were associated with comorbidity of temporomandibular disorders and rotator cuff tendinopathy [35].
To our knowledge, this is the first study to analyze the genetic association of SNPs in the ER-α gene in patients with tibialis posterior tendinopathy. These data were derived from 184 participants, providing solid evidence to detect a clinically relevant statistical relationship between SNPs and the condition at hand. All participants were post-menopausal women. The test group was slightly younger that the control group, but there were no significant differences in BMI, hypertension, hypothyroidism, and menopause time, thus minimizing the possible influence of systemic conditions on the pathogenesis of PTT insufficiency.
In the present case–control cross-sectional study, we identified an association between XbaI SNPs in the ER-α gene and PTT insufficiency. The A/A genotype was more prevalent in the test group, and we hypothesize that it may be a risk factor for PTT insufficiency. The A/A genotype may induce greater or faster degradation of the extracellular matrix, which may culminate in tendinopathy of the PTT. The XbaI SNPs lie in intron 1 of the ERα gene, which is part of the A/B domain, the trans-activating factor 1. This domain is a key site to stimulate transcription from certain estrogen-responsive promoters [36]. Among the possible explanations as to how this intronic polymorphism affected PTT dysfunction risk are that intronic changes may have an impact on the expression of receptors by influencing the transcription through alternative splicing of the mRNA transcript [37] or the alteration of another unidentified gene that is adjacent to the ERα gene [38].
Considering the PvuII SNP in ER-α gene, we did not detect significant differences in the frequencies of alleles and genotypes between the control and test groups. However, the effect of this SNP may be masked by SNP in different regions of a gene or other genes that participate in the complex network of mediators from the tendon region.
In addition to that, extensive studies between PvuII and XbaI SNPs in ER-α gene and different pathologies have produced inconsistent results when comparing different ethnic groups. Discrepancies between different studies may result from differences in ethnic background, indicating the probability of inherited susceptibility arising from different genomic ERα SNPs. However, replication studies in other populations as well as functional studies are needed to clarify the complex role of ERα in PTT tendinopathy.
Studies have demonstrated an altered proportion of several types of collagen in tendinopathy; specifically, PTT dysfunction shows increased type III, IV, or V collagen and decreased type I collagen which is diffusely distributed and grossly surrounded by type III fibrils [21, 39]. Since alterations in estrogen levels affect the overall collagen synthesis, the ERα XbaI SNPs might contribute to alteration in collagens in patients with PTT dysfunction.
Further understanding of the biological mechanisms underlying the tendinopathy process is an important prerequisite in developing genomics application. Early genetic identification of individuals at higher risk to develop PTT dysfunction can contribute to appropriate strategies for prevention and treatment of acquired flatfoot in adults.
Studies suggest that posterior tibial tendon dysfunction is a consequence and not the origin of flatfoot deformity. The concept of posterior tibial tendon dysfunction as the origin of the deformity is an old assumption, but it is still unclear whether a cause–effect relationship is present. In some instances, posterior tibial tendon transfer did not produce flatfoot deformity developed over time. This would support the idea that we are not looking at the whole picture and that degenerative changes must be present in multiple soft tissues (including, for example, the spring, interosseous, and subtalar ligaments) for an adult-acquired flatfoot deformity to develop [12, 16, 17, 39].
In conclusion, the XbaI SNPs in the ERα gene could be a risk factor for PTT tendinopathy. The ER-α PvuII SNP does not appear to be associated with PTT tendinopathy. Larger studies in other ethnic group may clarify the clinical impact of such findings.
Abbreviations
- BMI:
-
Body mass index
- ER-α and ER-β:
-
Estrogen receptor alfa and beta
- MRI:
-
Magnetic resonance image
- PCR-RFLP:
-
Polymerase chain reaction restriction fragment length polymorphism
- PTT:
-
Posterior tibial tendon
- SNP:
-
Single-nucleotide polymorphism
References
Wojtys EM, Huston LJ, Boynton MD, Spindler KP, Lindenfeld TN. The effect of the menstrual cycle on anterior cruciate ligament injuries in women as determined by hormone levels. Am J Sports Med. 2002;30(Suppl 2):182–8.
Zazulak BT, Paterno M, Myer GD, Romani WA, Hewett TE. The effects of the menstrual cycle on anterior knee laxity: a systematic review. Sports Med. 2006;36(Suppl 10):847–62.
Magnusson SP, Hansen M, Langberg H, Miller B, Haraldsson B, Westh EK, Koskinen S, Aagaard P, Kjaer M. The adaptability of tendon to loading differs in men and women. Int J Exp Pathol. 2007;88(Suppl 4):237–40.
Hansen M, Kjaer M. Influence of sex and estrogen on musculotendinous protein turnover at rest and after exercise. Exerc Sport Sci Rev. 2014;42(4):183–92.
de Jong JP, Nguyen JT, Sonnema AJ, Nguyen EC, Amadio PC, Moran SL. The incidence of acute traumatic tendon injuries in the hand and wrist: a 10-year population-based study. Clin Orthop Surg. 2014;6(Suppl 2):196–202.
Song CH, Gong HS, Bae KJ, Kim JH, Nam KP, Baek GH. Evaluation of female hormone-related symptoms in women undergoing carpal tunnel release. J Hand Surg Eur Vol. 2014;39(Suppl 2):155–60.
Lee CA, Lee-Barthel A, Marquino L, Sandoval N, Marcotte GR, Baar K. Estrogen inhibits lysyl oxidase and decreases mechanical function in engineered ligaments. J Appl Physiol (1985). 2015;118(Suppl 10):1250–7.
Liu SH, Al-Shaikh RA, Panossian V, Finerman GA, Lane JM. Estrogen affects the cellular metabolism of the anterior cruciate ligament. A potential explanation for female athletic injury. Am J Sports Med. 1997;25(Suppl 5):704–9.
Torricelli P, Veronesi F, Pagani S, Maffulli N, Masiero S, Frizziero A, Fini M. In vitro tenocyte metabolism in aging and oestrogen deficiency. Age (Dordr). 2013;35(Suppl 6):2125–36.
Ewies AA, Elshafie M, Li J, Stanley A, Thompson J, Styles J, White I, Al-Azzawi F. Changes in transcription profile and cytoskeleton morphology in pelvic ligament fibroblasts in response to stretch: the effects of estradiol and levormeloxifene. Mol Hum Reprod. 2008;14(Suppl 2):127–35.
Shen PC, Wang PH, Wu PT, Wu KC, Hsieh JL, Jou IM. The estrogen receptor-β expression in De Quervain’s disease. Int J Mol Sci. 2015;16(Suppl 11):26452–62.
Pomeroy GC, Pike RH, Beals TC, Manoli A 2nd. Acquired flatfoot in adults due to dysfunction of the posterior tibial tendon. J Bone Joint Surg Am. 1999;81-A:1173–82.
Salles JI, Amaral MV, Aguiar DP, Lira DA, Quinelato V, Bonato LL, Duarte ME, Vieira AR, Casado PL. BMP4 and FGF3 haplotypes increase the risk of tendinopathy in volleyball athletes. J Sci Med Sport. 2015;18(Suppl 2):150–5.
Neto JO, Machado DE, Perini JA. Vascular endothelial growth factor receptor-2 polymorphisms have protective effect against the development of tendinopathy in volleyball athletes. PLoS One. 2016;11(Suppl 12):e0167717.
Vaughn NH, Stepanyan H, Gallo RA, Dhawan A. Genetic factors in tendon injury: a systematic review of the literature. Orthop J Sports Med. 2017;5(Suppl 8):2325967117724416.
Wang C, Li H, Chen K, Wu B, Liu H. Association of polymorphisms rs1800012 in COL1A1 with sports-related tendon and ligament injuries: a meta-analysis. Oncotarget. 2017;8(Suppl 16):27627–34.
Godoy-Santos AL, Trevisan R, Fernandes TD, Santos MCLG. MMP-1 polymorphism is associated with tendinopathy primary posterior tibial tendon. J Orthop Res. 2013;31:1103–7.
Godoy-Santos A, Ortiz RT, Mattar Junior R, Fernandes TD, Santos MC. MMP-8 polymorphism is genetic marker to tendinopathy primary posterior tibial tendon. Scand J Med Sci Sports. 2014;24:220–3.
Baroneza JE, Godoy-Santos A, Ferreira Massa B, Boçon de Araujo Munhoz F, Diniz Fernandes T, Leme Godoy dos Santos MC. MMP-1 promoter genotype and haplotype association with posterior tibial tendinopathy. Gene. 2014;547:334–7.
de Araujo Munhoz FB, Baroneza JE, Godoy-Santos A, Fernandes TD, Branco FP, Alle LF, de Souza RL, Dos Santos MC. Posterior tibial tendinopathy associated with matrix metalloproteinase 13 promoter genotype and haplotype. J Gene Med. 2016;18(Suppl 11–12):325–30.
Diniz-Fernandes T, Godoy-Santos AL, Santos MC, Pontin P, Pereira CAA, Jardim YJ, Velosa APP, Maffulli N, Teodoro WR, Capelozzi VL. Matrix metalloproteinase-1 (MMP-1) and (MMP-8) gene polymorphisms promote increase and remodeling of the collagen III and V in posterior tibial tendinopathy. Histol Histopathol. 2018;33:929–936.
Leblanc DR, Schneider M, Angele P, Vollmer G, Docheva D. The effect of estrogen on tendon and ligament metabolism and function. J Steroid Biochem Mol Biol. 2017;172:106–16.
Hu W, Shuang F, Zou HX, Yang HH. Association between estrogen receptor-alpha gene PvuII and XbaI polymorphisms and osteoarthritis risk: a meta-analysis. Int J Clin Exp Med. 2015;8(Suppl 2):1956–65 eCollection 2015.
Park YS, Suh KT, Shin JK, Lee JS. Estrogen receptor gene polymorphism in patients with degenerative lumbar scoliosis. Br J Neurosurg. 2017;31(Suppl 1):63–6.
Zhu H, Jiang J, Wang Q, Zong J, Zhang L, Ma T, Xu Y, Zhang L. Associations between ERα/β gene polymorphisms and osteoporosis susceptibility and bone mineral density in postmenopausal women: a systematic review and meta-analysis. BMC Endocr Disord. 2018;18(Suppl 1):11.
Tashjian RZ, Granger EK, Zhang Y, Teerlink CC, Cannon-Albright LA. Identification of a genetic variant associated with rotator cuff repair healing. J Shoulder Elb Surg. 2016;25(Suppl 6):865–72.
Hu X, Jiang L, Tang C, Ju Y, Jiu L, Wei Y, Guo L, Zhao Y. Association of three single nucleotide polymorphisms of ESR1with breast cancer susceptibility: a meta-analysis. J Biomed Res. 2017;31(Suppl 3):213–25.
Han Z, Zhang L, Zhu R, Luo L, Zhu M, Fan L, Wang G. Relationship of oestrogen receptor alpha gene polymorphisms with risk for benign prostatic hyperplasia and prostate cancer in Chinese men. Medicine (Baltimore). 2017;96(Suppl 13):e6473.
Bridgeman JT, Zhang Y, Donahue H, Wade AM, Juliano PJ. Estrogen receptor expression in posterior tibial tendon dysfunction: a pilot study. Foot Ankle Int. 2010;31:1081–4.
Sowers MR, Zheng H, McConnell D, Nan B, Harlow S, Randolph JF Jr. Follicle stimulating hormone and its rate of change in defining menopause transition stages. J Clin Endocrinol Metab. 2008;93(Suppl 10):3958–64.
Aidar M, Line SR. A simple and cost-effective protocol for DNA isolation from buccal epithelial cells. Braz Dent. 2007;18:148–52.
Schneider S, Roessli D, Excoffier L. Arlequin v.2.000: software for population genetics data analysis. User manual: ver. 2.000. Geneva: Genetics and Biometry Laboratory, University of Geneva; 2000.
Motta Gda R, Amaral MV, Rezende E, Pitta R, Vieira TC, Duarte ME, Vieira AR, Casado PL. Evidence of genetic variations associated with rotator cuff disease. J Shoulder Elb Surg. 2014;23(Suppl 2):227–35.
Teerlink CC, Cannon-Albright LA, Tashjian RZ. Significant association of full-thickness rotator cuff tears and estrogen-related receptor-β (ESRRB). J Shoulder Elb Surg. 2015;24(Suppl 2):e31–5.
Bonato LL, Quinelato V, Pinheiro Ada R, Amaral MV, de Souza FN, Lobo JC, Aguiar DP, Augusto LM, Vieira AR, Salles JI, Cossich VR, Guimarães JA, de Gouvêa CV, Granjeiro JM, Casado PL. ESRRB polymorphisms are associated with comorbidity of temporomandibular disorders and rotator cuff disease. Int J Oral Maxillofac Surg. 2016;45(Suppl 3):323–31.
Zhao Y, Zheng X, Zhang L, Hu Q, Guo Y, Jiang H, Shi S, Zhang X. Association of estrogen receptor α PvuII and XbaI polymorphisms with prostate cancer susceptibility and risk stratification: a meta-analysis from case-control studies. Onco Targets Ther. 2017;10:3203–10.
Safarinejad MR, Safarinejad S, Shafiei N, Safarinejad S. Estrogen receptors alpha (rs2234693 and rs9340799), and beta (rs4986938 and rs1256049) genes polymorphism in prostate cancer: evidence for association with risk and histopathological tumor characteristics in Iranian men. Mol Carcinog. 2012;51(Suppl 1):E104–17.
Sundermann EE, Maki PM, Bishop JR. A review of estrogen receptor alpha gene (ESR1) polymorphisms, mood, and cognition. Menopause. 2010;17(Suppl 4):874–86.
Satomi E, Teodoro WR, Parrac ER, Fernandes TD, Velosa AP, Capelozzi VL, Yoshinari NH. Changes in histoanatomical distribution of types I, III and V collagen promote adaptative remodeling in posterior tibial tendon rupture. Clinics (Sao Paulo). 2008;63:9–14.
Acknowledgements
Not applicable
Funding
This work was supported by the FAPESP under number 2015/19635-1.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
Each individual author contributed individually and significantly to the development of this work. PAP contributed to the study conception/design acquisition of data. PRBN contributed to the data acquisition and reviewed the article. FCPF contributed to the data acquisition. CCN contributed to the data interpretation and critical revision. KCC contributed to the genetic analyses. JMSJ contributed to the data acquisition. ECB contributed to the study conception/design. TDF contributed to the data acquisition. NM contributed to the intellectual concept of the study. MCLS contributed to the intellectual concept of the study and genetic analyses. ALGS contributed to the intellectual concept of the study and the entire research and critical revision. NM helped to plan the work, interpret the results, and write and critically review the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by Ethics committee in research on human of Faculty of Medicine of the University of São Paulo (10166/2013).
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Pontin, P.A., Nogara, P.R.B., Fonseca, F.C.P. et al. ERα PvuII and XbaI polymorphisms in postmenopausal women with posterior tibial tendon dysfunction: a case control study. J Orthop Surg Res 13, 316 (2018). https://doi.org/10.1186/s13018-018-1020-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-018-1020-x