Abstract
Background
Subjective data and physical examinations of patients after total hip arthroplasty are used to assess the outcome. But regarding the physical activity, no objective data can be delivered by existing scores. The level of activity can be measured objectively by counting gait cycles. The aim of this study was to measure activity levels of patients before and after total hip arthroplasty (THA).
Methods
Forty-six patients were included in this prospective study. Western Ontario and McMaster Universities Arthritis Index (WOMAC), Harris Hip Score (HHS), and physical activity level based on the number of steps per day were assessed 1 week before surgery, 6 weeks postoperatively, and 3 months postoperatively. To assess the general constitution of the patients, the American Society of Anesthesiologists (ASA) score and BMI were determined. The physical activity level was measured by StepWatch 3™ Activity Monitor (SAM; Orthocare Innovations, Seattle, WA, USA). The number of GCs per day was assessed. Spearman’s rank correlation coefficients were used to identify an association between age, body mass index (BMI), and American Society of Anesthesiologists classification with the number of gait cycles and to detect correlation between GCs and HHS and GCs and WOMAC.
Results
From preoperatively to 6 weeks postoperatively, the number of gait cycles did not alter significantly. Three months postoperatively, the number of GC/d and GC/h improved significantly. HHS and WOMAC improved significantly from before surgery to 6 weeks and to 3 months follow-up. The number of gait cycles per day did not correlate with the HHS and the WOMAC score at any point of measurement. Age, BMI, and ASA classification did not influence the results.
Conclusion
By using a StepWatch 3™ Activity Monitor objective data about physical activity before and after THA can be measured reliable. Subjective and objective data in the postoperative period show different results. Physical activity seems to take longer to reach significantly improved values. By counting gait cycles, surgeons do have an additional tool to measure success after THA.
Similar content being viewed by others
Background
For patients with osteoarthritis of the hip, total hip arthroplasty (THA) is a highly successful procedure in end stage of the disease. Pain relief, functional recovery, and improving quality of life are the most important factors for the patients. Subjective data of the patients and physical examinations are used to assess the outcome after THA. There are many studies in which it could be shown that after hip arthroplasty, the patients improved significantly measured by scores like Western Ontario and McMaster Universities Arthritis Index (WOMAC) and Harris Hip Score (HHS) in a short and long term [1, 2]. Several studies could show good results after minimal invasive THA in the early postoperative period measured by HHS and WOMAC [3,4,5].
But regarding the physical activity, no objective data can be delivered by existing scores to show improvements after THA. In the literature, the level of activity can be measured objectively by counting gait cycles. Furthermore, recommendations on how many steps per day do represent an active life style can be done [6].
The aim of this study was to measure activity levels of patients with osteoarthritis of the hip before minimal invasive surgery (MIS) THA and after MIS THA. Cofactors influencing the results should be identified. Objective results were compared with existing scoring systems.
Methods
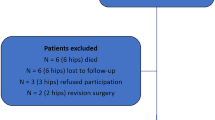
Forty-six patients (female n = 25, male n = 21, mean age 63.3 ± 10.5 years, mean BMI 27.1 ± 4.0 kg/m2) with THA in minimal invasive technique using the direct anterior approach were included in this prospective study. The indications for THA were osteoarthritis n = 43 and femoral head necrosis n = 3. Postoperative protocol included full weight-bearing from the first postoperative day.
In 37 patients, cementless fixation was used and in 9 patients, hybrid fixation was used. In all patients, 36-mm ceramic heads with X3™ polyethylene, (Stryker Orthopedics) were used. Exclusion criteria were patients with femoral neck fractures, hip arthroplasty because of metastasis or tumor diseases, and patients with partial weight-bearing postoperatively.
WOMAC [1], HHS [2], and physical activity level (PAL) based on the number of steps per day were assessed 1 week before surgery, 6 weeks postoperatively, and 3 months postoperatively. To assess the general constitution of the patients, the ASA score and BMI were determined [7]. The PAL was measured by StepWatch 3™ Activity Monitor (SAM; Orthocare Innovations, Seattle, WA, USA). The patients worn the StepWatch 3™ for 1 week preoperative, 6 weeks postoperative, and 3 months postoperative. The device is an uniaxial accelerometer, which can be worn comfortably above the ankle due to its low size and weight (7.5 × 5 × 2 cm, 43 g). The SAM stores the number of gait cycles (GC, one GC = 2 steps) in intervals of 1 min. It gives no feedback and cannot be manipulated by the subject. The SAM is well validated and has an accuracy of 99% in detecting steps in intervals of 1 min [8, 9]. Other accelerometers have also shown that objective data can be collected to assess physical activity levels [10]. Patients were instructed to wear the SAM at the right leg lateral above the lateral malleolus for the whole day from getting up to going to bed and were asked to record the non-wear times. The SAM was programmed according to the individual height and gait dynamics of the patient. The number of GCs was assessed in intervals of 1 min and transferred to a computer via the StepWatch™ USB Dock. The number of GCs per day and the number of GCs per hour were assessed taking into account the different wear times. Movement intensity was defined by the number of gait cycles per minute.
Minutes with more than 50 GCs were counted as moderate-to-vigorous physical activity (MVPA) [6]. Wear times and duration are listed in Table 1.
Trends in improvement of longitudinal data of activity parameters, WOMAC and HHS were analyzed using generalized estimating equations (GEE). Statistical significance was set at p value < 0.05. All statistical data analyses were created by IBM SPSS Statistics (version 19 or 20).
Spearman’s rank correlation coefficients were used to identify an association between age, body mass index (BMI), and American Society of Anesthesiologists (ASA) classification with the number of gait cycles (GCs) and to detect correlation between GCs and HHS and GCs and WOMAC.
Results
From preoperatively to 6 weeks postoperatively, the number of gait cycles did not alter significantly. Three months postoperatively, the number of GC/d and GC/h improved significantly by 18 and 15% compared to the preoperative measurement (p < 0.05). The number of minutes with more than 50 GCs did not change at 6 weeks follow-up (p = 0.372), but at 3 months, it increased significantly by 58% (p < 0.01).
HHS improved significantly from 50 (± 13) before surgery to 82 (± 13) at 6 weeks and to 93 (± 6) at 3 months follow-up (both p < 0.01).
The WOMAC score increased significantly from 42 (± 19) before surgery to 76 (± 15) at 6 weeks (p < 0.01) and to 82 (± 13) at 3 months follow-up (p < 0.01) gait cycles, and scores are listed in Table 2.
Between patients younger than 65 and older than 65, no significant differences could be found in GCs per day at any point of measurements.
BMI did not influence number of GC (group 1 BMI < 30, group 2 BMI > 30).
The ASA classification did not influence the number of GC per day.
The number of gait cycles per day did not correlate with the HHS and the WOMAC score at any point of measurement.
Discussion
Total hip arthroplasty is a very common and successful procedure in patients with end-stage osteoarthritis. For the patients’ reduced pain, improved physical function and activity, and regained quality of life are the most important factors after the procedure. By using scoring system pain, physical function and subjective physical activity are measured by the surgeons to evaluate the success of THA [1, 2, 11]. From other studies, we know that counting gait cycles per day is a possibility to get information about physical activity by objective measurements [6, 12].
Tudor-Locke stated that 10,000 steps/day are necessary for an “active” lifestyle. As expected, mobility with end-stage osteoarthritis is restricted. This restricted mobility is also reflected in significantly lower results in HHS and WOMAC. In terms of active, healthy lifestyle, the 4015 GCs found preoperatively in our study can be considered as “somewhat active” [6]. This activity level was comparable with that reported by Winter et al. for patients with end-stage osteoarthritis of the hip (3994 GCs) [13].
After THA, it is expected that pain is reduced. With reduced pain function, the joint is expected to get better. These things are the precondition for a more active behavior. Therefore, it is comprehensible that an increased mobility (gait cycles/day) can only be measured at a later onset than parameters like pain and function measured by the used scores.
In a study of end-stage hip and knee osteoarthritis patients, the authors came to the conclusion that the patients’ perception of physical functioning does not always correspond to the objective measured physical activity [14]. These results can be confirmed. In our study group, no correlation could be found between WOMAC, HHS, and gait cycles per day. In another study of total hip and knee arthroplasties, subjective parameters like pain relief, stiffness, and self-reported physical function showed a large improvement postoperatively. In contrast, the objective results of physical activity measured by an activity monitor with accelerometers were less than expected by 6 months after surgery respectively, and no improvement after 6 months could be measured [15,16,17].
Our patients could increase their objective physical activity significantly 3 months after surgery with 4756 GCs per day. After 6 weeks, GCs per day showed no significant improvement, whereas HHS and WOMAC showed significant improvements already after 6 weeks and again after 3 months.
Similar results at 8 weeks follow-up were reported by Brandes et al. for patients undergoing total knee replacement, and activity levels at this point of time were similar than preoperative whereas the knee society score improved significantly after 8 weeks [18].
In another study of patients after TKA, SF 36 and the Physical Activity Scale for the Elderly (PASE) increased significantly already after 3 months after the operation. The number of steps per day was 2693 at 3 months and 3518 at 6 months after the operation [19].
In 2016, Toogood et al. compared patients after minimal invasive (MIS) THA with conventional THA 30 days after the operation. In average, the number of steps per day was 2563 and in the MIS group, the level of activity was significantly higher [20].
In our collective, the activity level after 6 weeks and 3 months was higher than in the studies mentioned above. Although we could not found any differences in GCs/per day independence of age, patients in the other studies were about 10 years older in average [19, 20]. From the literature, we know that steps per day decrease with increasing age and physical activity decreases with age [12, 21].
But also, the MIS approach can be a reason for a higher activity level postoperatively.
Other factors like comorbidities and BMI with influence on activity levels are discussed in the literature. In our patients, ASA and BMI had no influence on objective activity level. Toogood et al. also showed that BMI greater or less than 30 kg/m2 had no influence on objective activity level [20]. In contrast to these results, self-reported physical activity at 1–2 years postoperatively after THA and TKA was lower depending on BMI, female sex, and specific comorbidities [22].
There are some limitations of our study. Although we used a prospective design, no control group was included. So, we cannot say if MIS surgery has a positive influence on activity level. The group of patients included was small. As a university hospital, most of the patients did not fulfill the inclusion criteria. Because we used the ASA classification, no information about comorbidities in detail were available. So, we could not detect individual diseases, which might have a negative influence on the level of activity.
The follow-up was limited to 3 months postoperatively, although we know that results do also improve in the following months [15].
Conclusion
By using a StepWatch 3™ Activity Monitor, objective data about physical activity before and after THA can be measured reliable. As shown, subjective and objective data in the postoperative period show different results and although scores improve significantly already 6 weeks after the operations, objective physical activity seems to take longer to reach significantly improved values. By counting gait cycles, surgeons do have an additional tool to measure success after THA with regard on a healthy lifestyle. Maybe online measurements after discharge from hospital can be used to control and intervene if necessary to bring the patient back to an appropriate activity.
Abbreviations
- ASA:
-
American Society of Anesthesiologists
- BMI:
-
Body mass index
- GCs:
-
Gait cycles
- GEE:
-
Generalized estimating equations
- HHS:
-
Harris Hip Score
- MIS:
-
Minimal invasive surgery
- MVPA:
-
Moderate-to-vigorous physical activity
- PAL:
-
Physical activity level
- THA:
-
Total hip arthroplasty
- WOMAC:
-
Western Ontario and McMaster Universities Arthritis Index
References
Stucki G, Meier D, Stucki S, Michel BA, Tyndall AG, Dick W, Theiler R. Evaluation of a German version of WOMAC (Western Ontario and McMaster Universities) Arthrosis Index. Z Rheumatol. 1996;55(1):40–9.
Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51(4):737–55.
Graves SC, Dropkin BM, Keeney BJ, Lurie JD, Tomek IM. Does surgical approach affect patient-reported function after primary THA? Clin Orthop Relat Res. 2016;474(4):971–81.
Christensen CP, Jacobs CA. Comparison of patient function during the first six weeks after direct anterior or posterior total hip arthroplasty (THA): a randomized study. J Arthroplast. 2015;30(9 Suppl):94–7.
Restrepo C, Parvizi J, Pour AE, Hozack WJ. Prospective randomized study of two surgical approaches for total hip arthroplasty. J Arthroplast. 2010;25(5):671–9. e671
Tudor-Locke C, Hatano Y, Pangrazi RP, Kang M. Revisiting “how many steps are enough?”. Med Sci Sports Exerc. 2008;40(7 Suppl):S537–43.
Bjorgul K, Novicoff WM, Saleh KJ. Evaluating comorbidities in total hip and knee arthroplasty: available instruments. J Orthop Traumatol. 2010;11(4):203–9.
Foster RC, Lanningham-Foster LM, Manohar C, McCrady SK, Nysse LJ, Kaufman KR, Padgett DJ, Levine JA. Precision and accuracy of an ankle-worn accelerometer-based pedometer in step counting and energy expenditure. Prev Med. 2005;41(3-4):778–83.
Shepherd EF, Toloza E, McClung CD, Schmalzried TP. Step activity monitor: increased accuracy in quantifying ambulatory activity. J Orthop Res. 1999;17(5):703–8.
Stefani L, Mascherini G, Scacciati I, De Luca A, Maffulli N, Galanti G. Positive effect of the use of accelerometry on lifestyle awareness of overweight hypertensive patients. Asian J Sports Med. 2013;4(4):241–8.
Lubbeke A, Zimmermann-Sloutskis D, Stern R, Roussos C, Bonvin A, Perneger T, Peter R, Hoffmeyer P. Physical activity before and after primary total hip arthroplasty: a registry-based study. Arthritis Care Res (Hoboken). 2014;66(2):277–84.
Tudor-Locke C, Schuna JM Jr, Barreira TV, Mire EF, Broyles ST, Katzmarzyk PT, Johnson WD. Normative steps/day values for older adults: NHANES 2005-2006. J Gerontol A Biol Sci Med Sci. 2013;68(11):1426–32.
Winter CC, Brandes M, Muller C, Schubert T, Ringling M, Hillmann A, Rosenbaum D, Schulte TL. Walking ability during daily life in patients with osteoarthritis of the knee or the hip and lumbar spinal stenosis: a cross sectional study. BMC Musculoskelet Disord. 2010;11:233.
de Groot IB, Bussmann JB, Stam HJ, Verhaar JA. Actual everyday physical activity in patients with end-stage hip or knee osteoarthritis compared with healthy controls. Osteoarthr Cartil. 2008;16(4):436–42.
de Groot IB, Bussmann HJ, Stam HJ, Verhaar JA. Small increase of actual physical activity 6 months after total hip or knee arthroplasty. Clin Orthop Relat Res. 2008;466(9):2201–8.
Harding P, Holland AE, Delany C, Hinman RS. Do activity levels increase after total hip and knee arthroplasty? Clin Orthop Relat Res. 2014;472(5):1502–11.
Lin BA, Thomas P, Spiezia F, Loppini M, Maffulli N. Changes in daily physical activity before and after total hip arthroplasty. A pilot study using accelerometry. Surgeon. 2013;11(2):87–91.
Brandes M, Ringling M, Winter C, Hillmann A, Rosenbaum D. Changes in physical activity and health-related quality of life during the first year after total knee arthroplasty. Arthritis Care Res (Hoboken). 2011;63(3):328–34.
Tsonga T, Kapetanakis S, Papadopoulos C, Papathanasiou J, Mourgias N, Georgiou N, Fiska A, Kazakos K. Evaluation of improvement in quality of life and physical activity after total knee arthroplasty in greek elderly women. Open Orthop J. 2011;5:343–7.
Toogood PA, Abdel MP, Spear JA, Cook SM, Cook DJ, Taunton MJ. The monitoring of activity at home after total hip arthroplasty. Bone Joint J. 2016;98-B(11):1450–4.
Kinkel S, Wollmerstedt N, Kleinhans JA, Hendrich C, Heisel C. Patient activity after total hip arthroplasty declines with advancing age. Clin Orthop Relat Res. 2009;467(8):2053–8.
Paxton EW, Torres A, Love RM, Barber TC, Sheth DS, Inacio MC. Total joint replacement: a multiple risk factor analysis of physical activity level 1-2 years postoperatively. Acta Orthop. 2016;87(Suppl 1):44–9.
Acknowledgements
None.
Funding
The study was not funded.
Availability of data and materials
Not applicable.
Author information
Authors and Affiliations
Contributions
SH made substantial contribution to conception and design. AB made substantial contribution to acquisition of the data. GG made critical revision of the manuscript for content. RD made substantial contribution to acquisition and analysis of the data. CW made substantial contribution to acquisition of the data. DR made contribution to analysis and interpretation of the data. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the local institution’s Ethics Committee at the University of Muenster, Germany (reference no. 2013-206-f-S) and was conducted in accordance with the Helsinki Declaration. All patients provided informed written consent to participate in the investigation.
Consent for publication
Consent for publication was obtained from the participants.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Höll, S., Blum, A., Gosheger, G. et al. Clinical outcome and physical activity measured with StepWatch 3™ Activity Monitor after minimally invasive total hip arthroplasty. J Orthop Surg Res 13, 148 (2018). https://doi.org/10.1186/s13018-018-0775-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-018-0775-4