Abstract
Background
This study clarified the mechanical performance of volumetric modulated arc therapy (VMAT) plans for prostate cancer generated with a commercial knowledge-based treatment planning (KBP) and whether KBP system could be applied clinically without any major problems with mechanical performance.
Methods
Thirty consecutive prostate cancer patients who underwent VMAT using extant clinical plans were evaluated. The mechanical performance and dosimetric accuracy of the single optimized KBPs, which were trained with other 51 clinical plans, were compared with the clinical plans. The mechanical performance metrics were mean field area (MFA), mean asymmetry distance (MAD), cross-axis score (CAS), closed leaf score (CLS), small aperture score (SAS), leaf travel (LT), modulation complexity score (MCSv), and monitor unit (MU). The γ passing rates were evaluated with ArcCheck and EBT3 film.
Results
The mean mechanical performance metrics (clinical plan vs. KBP) were as follows: 18.28 cm2 vs. 17.25 cm2 (MFA), 21.08 mm vs. 20.47 mm (MAD), 0.54 vs. 0.55 (CAS), 0.040 vs. 0.051 (CLS), 0.20 vs. 0.23 (SAS5mm), 458.5 mm vs. 418.8 mm (LT), 0.27 vs. 0.27 (MCSv), and 618.2 vs. 622.1 (MU), respectively. Significant differences were observed for CLS and LT. The average γ passing rates (clinical plan vs. KBP) were as follows: 99.0% vs. 99.1% (3%/3 mm) and 92.4% vs. 92.5% (2%/2 mm) with ArcCHeck, and 99.5% vs. 99.4% (3%/3 mm) and 95.2% vs. 95.4% (2%/2 mm) with EBT3 film, respectively.
Conclusions
The KBP used lower multileaf collimator (MLC) travel and more closed or small MLC apertures than the clinical plan. The KBP system of VMAT for the prostate cancer was acceptable for clinical use without any major problems.
Similar content being viewed by others
Background
In intensity-modulated radiotherapy (IMRT) and volumetric modulated arc therapy (VMAT), variations in knowledge and experience can lead to significant differences in the plan quality and may compromise the gains of high-precision radiotherapy [1, 2]. Knowledge-based treatment planning (KBP) is an approach to reduce the differences in plan quality and improve planning consistency [1]. A commercial KBP module, RapidPlan (Varian Medical Systems, Palo Alto CA, USA) has been released for the Eclipse (Varian) treatment planning system (TPS). KBP uses a statistical model generated from a library of clinically accepted plans with consistent high quality to train dose volume histograms (DVHs) [1, 3]. This model predicts an achievable DVH range and generates dose volume objectives for IMRT and VMAT plan optimization [1, 3].
Many studies have reported the KBP can generate the better or comparable dosimetric results in some anatomical sites [1,2,3,4,5,6,7,8,9]. Hussein et al. described the KBP was able to produce IMRT and VMAT treatment plans for prostate cancer with a single optimization, with sparing and conformity better than or comparable to a clinical plan [1]. In addition, Ueda et al. suggested the KBP could also reproduce the dose distributions based on the experience of institutions in the case of sharing the KBP model, although it was necessary to verify the registered DVH curves could match the plan design of each institution [10]. However, Kubo et al. found that KBP may encounter difficulties with high numbers of MUs and high modulation complexity [11]. At this time, we focused on the mechanical performance of the KBP, which has not been delineated. Additionally, dosimetric accuracy can be affected by mechanical performance [12, 13]. VMAT delivery requires extremely precise mechanical performance for a linear accelerator (Linac) due to the simultaneous gantry speed, dose rate, and multileaf collimator (MLC) aperture shape variations; this makes patient-specific quality assurance (QA) an essential prerequisite for actual patient treatment [13, 14]. The purpose of this study was to clarify the mechanical performance of the VMAT plans generated by the KBP for prostate cancer and verify patient-specific QA to assess KBP’s appropriateness in the clinical setting.
Methods
Clinical plan and KBP
The cases of 30 consecutive prostate cancer patients (between September 2016 and March 2017) who underwent VMAT with clinical plans were analyzed. We trained the KBP system with the other consecutive 51 cases of T1–T2c prostate cancer treated between August 2015 and August 2016. Written informed consent was obtained from all patients and the Institutional Ethics Committee approved this study (institutional review board number: 29–133). The KBP model configuration and training process is well-explained in the literature [5, 7, 11]. The clinical target volume (CTV) was defined as the prostate and seminal vesicle and delineated by experienced radiation oncologists. The planning target volume (PTV) was defined with a 6 mm posterior margin and a 10 mm margin in all other directions added to the CTV to reduce the dose at the prostate-rectal interface. The organ at risks (OARs) were rectal wall and bladder wall. The rectum was delineated up to 1.0 cm above and below the PTV. The rectal wall and bladder wall were delineated 4.0 mm inside the outer surface of rectum and bladder, respectively. The prescribed dose was 78 Gy in 39 fractions to 95% of the volume of the PTV minus rectum (PTV − R) using 10 MV photon beams and 2 full arcs VMAT (Gantry angle: 181°–179°, clockwise and 179°–181°, counterclockwise, collimator angles: 30° and 330°). The control point spacing was 2° angular separation. All VMAT plans were calculated with the Varian Analytic Anisotropic Algorithm (AAA) [15] using the Eclipse treatment planning system ver. 13.6 for a TrueBeam (Varian) with a Millennium 120 MLC. The goals of the treatment plan in our institution were as follows: The maximum dose (Dmax) was < 110% and the mean dose (Dmean) was 99–103% of the prescribed dose for the PTV − R; V40 Gy < 60%, V60 Gy < 35%, V70 Gy < 25%, and V78 Gy < 1% for the rectal wall; V40 Gy < 60% and V70 Gy < 35% for the bladder wall [10, 16]. The overlap region between PTV and rectal wall was covered with the 90% isodose line.
The geometry and dosimetry of the PTV − R, rectum, and bladder were registered in the KBP library. In this model, the geometry or dosimetry outliers were not excluded since the removal of statistical outliers had no significant impact on establishing the model [1]. Then, we performed the dose calculation using KBP with the single optimization in the 30 consecutive clinical cases.
KBP validation
The following parameters were compared between the 30 clinical plans and the 30 KBPs:
-
1.
The maximum (Dmax), minimum (Dmin), and mean dose (Dmean) of the PTV–R volume
-
2.
Homogeneity index (HI; defined as 100 × [D2% − D98%]/D50%), where D98%, D2%, and D50% are doses received by 98%, 2%, and 50% of the PTV − R, respectively [17]
-
3.
The 95% isodose conformity index (CI95; defined as V95%/VPTV − R), where V95% is volume covered by 95% of the prescribed dose (74.1 Gy) and VPTV − R is PTV–R volume [1]
-
4.
Dose-volume parameters of the rectal wall: V40 Gy, V60 Gy, V70 Gy, and V78 Gy
-
5.
Dose-volume parameters of the bladder wall: V40 Gy and V70 Gy
Mechanical performance metrics
For each of the 30 clinical plans and the 30 KBPs, 8 mechanical performance metrics were verified as shown in Table 1: 1. mean field area (MFA), 2. mean asymmetry distance (MAD), 3. cross-axis score (CAS), 4. closed leaf score (CLS), 5. small aperture score (SAS) [18,19,20], 6. leaf travel (LT), 7. modulation complexity score for VMAT (MCSv), and 8. total MUs [12, 13].
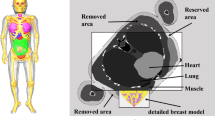
Patient-specific QA
The gamma index evaluation for patient-specific QA has been a standard technique used to evaluate measured distributions in commercial detector systems and gafchromic film against the dose distributions predicted by TPSs [21]. We employed ArcCheck (SunNuclear, Melbourne FL, USA) as a commercial detector system for patient-specific QA. The film dosimetry was also performed. The EBT3 gafchromic film (Ashland ISP Advanced Materials, Bridgewater, NJ, USA) was inserted at the sagittal plane in center of the ArcCheck. Irradiated films were scanned using Epson ES-10000G scanner (Epson Corp., Nagano, Japan) at least 24 h after irradiation with a resolution of 150 dpi from red channel. A calibration curve, film optical density versus dose, was determined for a range from 0 to 300 cGy. For analysis, the DoseLab ver. 6.70 (Mobius Medical Systems, TX, USA) was employed. An ionization chamber (CC01, IBA, Schwarzenbruck, Germany) was used for measurement of absorbed dose at the isocenter in the ArcCheck (source-to-axis distance (SAD) = 100 cm). Then we evaluated the differences in dose distribution and point dose at isocenter among plans and measurements for each clinical plan and KBP. The difference of dose distribution was evaluated using the passing rate of γ index with two tolerances in terms of dose difference (DD) and distance to agreement (DTA) (3%/3 mm and 2%/2 mm) with a threshold at 10%.
Statistical analysis
The data are expressed as the median and interquartile ranges (first quartile, third quartile), unless otherwise indicated. The Wilcoxon signed rank test was used to compare continuous variables and trends between the KBPs and the clinical plans. All statistical analyses were performed using R ver. 3.4.2 (The R Foundation for Statistical Computing, Vienna, Austria) and p < 0.05 was considered statistically significant. Peason’s correlation was considered weak for r < 0.4, moderate for 0.4 ≤ r ≤ 0.7, and strong for r > 0.7.
Results
KBP validation
Table 2 summarizes the results of comparisons between the clinical plan and the KBP of Dmax, Dmin, Dmean, HI and CI95 for PTV − R, dose-volume parameters for rectal wall and bladder wall. For the PTV − R, the Dmin and the Dmean were comparable between the clinical plan and the KBP, and the Dmax of the KBP was significantly lower than those of the clinical plan (p < 0.01). The homogeneity of PTV − R of the KBP was significantly better than those of the clinical plan (p = 0.03). In addition, the PTV − R coverage of the KBP was more conformal as indicated by the CI95 being significantly lower than the CI95 of the clinical plan (p < 0.01). For the rectal wall and the bladder wall, the dose-volume parameters of the KBP were comparable to those of the clinical plan except for the V78 Gy for the rectal wall. The V78 Gy for the rectal wall of the KBP was higher than those of the clinical plan; however, it was < 1% for all cases. The mean DVHs for the clinical plan and the KBP were shown in Fig. 1. The KBP was able to generate better or comparable dosimetric results compared to clinical plan using our training model.
The average DVHs of the clinical plan and the KBP for PTV − R (a), rectal wall (b), and bladder wall (c). For the PTV − R of the KBP, the Dmax was lower than those of the clinical plans, which improved the homogeneity. The V78 Gy for rectal wall of the KBP was higher than those of the clinical plans, however it was < 1% for all cases
Mechanical performance
Table 3 summarizes the mechanical performance metrics of MFA, MAD, CAS, CLS, SAS (thresholds: 2, 5, 10, and 20 mm), LT, MCSv, and MU for the clinical plan and the KBP. The MFA, MAD, CAS, MCSv and MU of the KBP were almost equal to those of the clinical plan. On the other hand, there were significant differences for CLS (p = 0.03) and LT (p < 0.01). The KBP used more closed leaves and less MLC travel compared to the clinical plan. The SASs for each threshold of the KBP tended to be higher than those for the clinical plans, although there were no significant differences. This suggests that KBP system may use more small apertures in the MLCs than the clinical plan at each control point. In addition, the relationships between MCSv and LT, CLS, and SAS were shown in Fig. 2. The LT, CLS, and SAS2mm were not correlated to the MCSv in Fig. 2a–c. On the other hand, negative correlations were observed between MCSv and SASs for threshold ≥10 mm in Fig. 2e, f.
Patient-specific QA
Table 4 shows the γ passing rate of each criterion for the clinical plan and the KBP. No significant differences were observed between the clinical plan and the KBP in the γ passing rate with ArcCheck and EBT3 film. The γ passing rates of the clinical plan and the KBP were > 90% for all cases for commonly used criteria of 3%/3 mm [22,23,24]. For more stringent 2%/2 mm, the cases of the clinical plan and the KBP in which the γ passing rates were > 90% with the ArcCheck were 24 and 25 cases in 30 cases, respectively. On the other hand, the cases of both the clinical plan and the KBP in which the γ passing rates were > 90% with EBT3 film were 28 cases in 30 cases. No mechanical performance metrics were correlated to the γ passing rate. The differences in absorbed dose at the isocenter for measurement compared to the TPS were − 0.40% (− 0.86%, 0.023%) and − 0.29% (− 0.50%, − 0.083%) for the clinical plan and the KBP, respectively (p = 0.48).
Discussion
In this study, we clarified the mechanical performance and evaluated the dosimetric accuracy of the VMAT generated by the KBP for prostate cancer. The KBP system can be used in clinical practice without any major problems, although the KBP created dose distributions by use of lower MLC travel and more closed or small MLC apertures compared to the clinical plan.
In the KBP model validation, Table 2 and Fig. 1 show the dose volume parameters of the KBP with the single optimization for PTV − R were better or comparable, and for rectal wall and bladder wall were comparable, to the clinical plan, respectively. The KBP also had higher homogeneity and conformity for PTV − R compared to the clinical plan. However, this model could contain a limited number of structures (e.g. femoral head, sacrum, anal canal, and bulbus penis).
In mechanical performance, the CLS and the LT values of the KBP were significantly different from the clinical plan as shown in Table 3. Additionally, the SASs for all thresholds of the KBP were higher than those of the clinical plan, although not to a significant degree. The KBP system might use lower MLC travel, and more closed or small MLC apertures at each control point than the clinical plan. The negative correlations between MCSv and SASs for threshold ≥10 mm were shown in Fig. 2e–f. The modulation complexity was increased with the proportion of small apertures increasing, which was also described by Crowe et al. [20]. Therefore, one full arc VMAT plan generated by the KBP might increase the MU and the modulation complexity compared to the clinical plan [11]. On the other hand, two full arcs VMAT plans generated by the KBP might decrease the MU and the modulation complexity. Hussein et al. also showed the MU and modulation complexity were not difference between the KBP and clinical plan for two full arcs VMAT plans [1].
The γ passing rates for all criteria of DD and DTA were not significantly different between the clinical plan and the KBP, and all cases of the clinical plan and the KBP had the γ passing rates of more than 90% for AAPM recommending criteria of 3%/3 mm [23] as shown in Table 4, although the mechanical performance of the KBP did not correspond to that of the clinical plan. A patient-specific QA passed if the γ passing rate was > 90% of points achieving the 3%/3 mm criterion, which is acceptable in the clinical setting [22,23,24], although some reports describe more stringent criteria such as 2%/2 mm [25,26,27]. It is necessary to understand the sensitivity and limitations of the gamma index analysis combined with the equipment in use [21].
Conclusions
The KBP with the single optimization used lower MLC travel and more closed or small MLC apertures compared to the clinical plan. The VMAT plan generated by the KBP for prostate cancer could be applied clinically without any major problems.
Abbreviations
- AAA:
-
Analytic Anisotropic Algorithm
- AAV:
-
Aperture area variability
- CAS:
-
Cross-axis score
- CI95 :
-
95% isodose conformity index
- CLS:
-
Closed leaf score
- CTV:
-
Clinical target volume
- DD:
-
Dose difference
- DTA:
-
Distance to agreement
- DVH:
-
Dose volume histogram
- HI:
-
Homogeneity index
- IMRT:
-
Intensity-modulated radiotherapy
- KBP:
-
Knowledge-based treatment planning
- Linac:
-
Linear accelerator
- LSV:
-
Leaf sequence variability
- LT:
-
Leaf travel
- MAD:
-
Mean asymmetry distance
- MCSv:
-
Modulation complexity score for VMAT
- MFA:
-
Mean field area
- MLC:
-
Multileaf collimator
- MU:
-
Monitor unit
- OAR:
-
Organ at risk
- PTV − R:
-
Volume of the PTV minus rectum
- PTV:
-
Planning target volume
- QA:
-
Quality assurance
- SAD:
-
Source-to-axis distance
- SAS:
-
Small aperture score
- TPS:
-
Treatment planning system
- VMAT:
-
Volumetric modulated arc therapy
References
Hussein M, South CP, Barry MA, Adams EJ, Jordan TJ, Stewart AJ, et al. Clinical validation and benchmarking of knowledge-based IMRT and VMAT treatment planning in pelvic anatomy. Radiother Oncol. 2016;120:473–9. https://doi.org/10.1016/j.radonc.2016.06.022
Tol JP, Delaney AR, Dahele M, Slotman BJ, Verbakel WFAR. Evaluation of a knowledge-based planning solution for head and neck cancer. Int J Radiat Oncol Biol Phys. 2015;91:612–20. https://doi.org/10.1016/j.ijrobp.2014.11.014
Wu H, Jiang F, Yue H, Li S, Zhang Y. A dosimetric evaluation of knowledge-based VMAT planning with simultaneous integrated boosting for rectal cancer patients. J Appl Clin Med Phys. 2016;17:78–85. https://doi.org/10.1120/jacmp.v17i6.6410
Fogliata A, Wang P-M, Belosi F, Clivio A, Nicolini G, Vanetti E, et al. Assessment of a model based optimization engine for volumetric modulated arc therapy for patients with advanced hepatocellular cancer. Radiat Oncol. 2014;9:236. https://doi.org/10.1186/s13014-014-0236-0
Fogliata A, Belosi F, Clivio A, Navarria P, Nicolini G, Scorsetti M, et al. On the pre-clinical validation of a commercial model-based optimisation engine: application to volumetric modulated arc therapy for patients with lung or prostate cancer. Radiother Oncol. 2014;113:385–91. https://doi.org/10.1016/j.radonc.2014.11.009
Fogliata A, Nicolini G, Bourgier C, Clivio A, De Rose F, Fenoglietto P, et al. Performance of a knowledge-based model for optimization of volumetric modulated arc therapy plans for single and bilateral breast irradiation. PLoS One. 2015;10:1–12. https://doi.org/10.1371/journal.pone.0145137
Fogliata A, Nicolini G, Clivio A, Vanetti E, Laksar S, Tozzi A, et al. A broad scope knowledge based model for optimization of VMAT in esophageal cancer: validation and assessment of plan quality among different treatment centers. Radiat Oncol. 2015;10:220. https://doi.org/10.1186/s13014-015-0530-5
Snyder K, Kim J, Reding A, Fraser C, Lu S, Gordon J, et al. Development and evaluation of a knowledgebased model for treatment planning of lung cancer patients using stereotactic body radiotherapy (SBRT). J Appl Clin Med Phys. 2016;17:263–75. https://doi.org/10.1120/jacmp.v17i6.6429
Chang ATY, Hung AWM, Cheung FWK, Lee MCH, Chan OSH, Philips H, et al. Comparison of planning quality and efficiency between conventional and knowledge-based algorithms in nasopharyngeal cancer patients using intensity modulated radiation therapy. Int J Radiat Oncol Biol Phys. 2016;95:981–90. https://doi.org/10.1016/j.ijrobp.2016.02.017
Ueda Y, Fukunaga J, Kamima T, Adachi Y, Nakamatsu K, Monzen H. Evaluation of multiple institutions’ models for knowledge-based planning of volumetric modulated arc therapy (VMAT) for prostate cancer. Radiat Oncol. 2018;46:46. https://doi.org/10.1186/s13014-018-0994-1
Kubo K, Monzen H, Ishii K, Tamura M, Kawamorita R, Sumida I, et al. Dosimetric comparison of RapidPlan and manually optimized plans in volumetric modulated arc therapy for prostate cancer. Phys Med. 2017;44:199–204. https://doi.org/10.1016/j.ejmp.2017.06.026
McNiven AL, Sharpe MB. Purdie TG. A new metric for assessing IMRT modulation complexity and plan deliverability. Med Phys. 2010;37:505–15. https://doi.org/10.1118/1.3276775
Masi L, Doro R, Favuzza V, Cipressi S, Livi L. Impact of plan parameters on the dosimetric accuracy of volumetric modulated arc therapy. Med Phys. 2013;40:071718. https://doi.org/10.1118/1.4810969
Li G, Zhang Y, Jiang X, Bai S, Peng G, Wu K, et al. Evaluation of the ArcCHECK QA system for IMRT and VMAT verification. Phys Med. 2013;29:295–303. https://doi.org/10.1016/j.ejmp.2012.04.005
Van EA, Tillikainen L, Huyskens DP, Tenhunen M, Helminen H, Siljämaki S, et al. Testing of the analytical anisotropic algorithm for photon dose calculation. Med Phys. 2006;33:4130–48. https://doi.org/10.1118/1.2358333
Hirose Y, Nakamura M, Tomita T, Kitsuda K, Notogawa T, Miki K, et al. Evaluation of different set-up error corrections on dose-volume metrics in prostate IMRT using CBCT images. J Radiat Res. 2014;55:966–75. https://doi.org/10.1093/jrr/rru033
Wu H, Jiang F, Yue H, Zhang H, Wang K, Zhang Y. Applying a RapidPlan model trained on a technique and orientation to another : a feasibility and dosimetric evaluation. Radiat Oncol. 2016;11:108. https://doi.org/10.1186/s13014-016-0684-9
Crowe S. Treatment plan complexity metrics for predicting IMRT pre-treatment quality assurance results. Australas Phys Eng Sci Med. 2014;37:475–82. https://doi.org/10.1007/s13246-014-0274-9
Kairn T, Crowe SB, Kenny J, Knight RT, Trapp JV. Predicting the likelihood of QA failure using treatment plan accuracy metrics. J Phys Conf Ser. 2014;489:012051. https://doi.org/10.1088/1742-6596/489/1/012051
Crowe SB, Kairn T, Middlebrook N, Sutherland B, Hill B, Kenny J, et al. Examination of the properties of IMRT and VMAT beams and evaluation against pre-treatment quality assurance results. Phys Med Biol. 2015;60:2587–601. https://doi.org/10.1088/0031-9155/60/6/2587
Hussein M, Rowshanfarzad P, Ebert MA, Nisbet A, Clark CH. A comparison of the gamma index analysis in various commercial IMRT/VMAT QA systems. Radiother Oncol. 2013;109:370–6. https://doi.org/10.1016/j.radonc.2013.08.048
Aristophanous M, Suh Y, Chi PC, Whittlesey LJ, Laneave S, Mary K. Initial clinical experience with ArcCHECK for IMRT/VMAT QA. J Appl Clin Med Phys. 2016;17:20–33. https://doi.org/10.1120/jacmp.v17i5.6118
Ezzell GA, Burmeister JW, Dogan N, LoSasso TJ, Mechalakos JG, Mihailidis D, et al. IMRT commissioning: multiple institution planning and dosimetry comparisons, a report from AAPM task group 119. Med Phys. 2009;36:5359–73. https://doi.org/10.1118/1.3238104
Crowe SB, Sutherland B, Wilks R, Seshadri V, Sylvander S, Trapp JV, et al. Technical note: relationships between gamma criteria and action levels: results of a multicenter audit of gamma agreement index results. Med Phys. 2016;43:1501–6. https://doi.org/10.1118/1.2710949
García-Vicente F, Fernández V, Bermúdez R, Gómez A, Pérez L, Zapatero A, et al. Sensitivity of a helical diode array device to delivery errors in IMRT treatment and establishment of tolerance level for pretreatment QA. J Appl Clin Med Phys. 2012;13:111–23. https://doi.org/10.1120/jacmp.v13i1.3660
Steers JM, Fraass BA. IMRT QA: Selecting gamma criteria based on error detection sensitivity. Med Phys. 2016;43:1982–94. https://doi.org/10.1118/1.4943953
Nelms BE, Opp D, Robinson J, Wolf TK, Zhang G, Moros E, et al. VMAT QA: measurement-guided 4D dose reconstruction on a patient. Med Phys. 2012;39:4228–38. https://doi.org/10.1118/1.4729709
Acknowledgements
We thank Libby Cone, MD, MA, from Edanz Group (http://www.edanzediting.com/ac) for editing a draft of this manuscript.
Funding
This work was supported by the Japan Society for the Promotion of Science KAKENHI (grant number: 16 K10406).
Availability of data and materials
The dataset used and/or analysed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
Concept and design: MT, HM. Treatment planning: MT, HM, KM, MO, MI, HD, KI, KN. Measurements: MT, KM, MO. Data analysis: MT, KK, IS, HM, DKY. Manuscript preparation: MT, HM, HD, KI, KN, YN. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by review committee with written informed consent provided by the patients (institutional review board number: 29–133).
Consent for publication
The institutional consent form was obtained from the patients.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Tamura, M., Monzen, H., Matsumoto, K. et al. Mechanical performance of a commercial knowledge-based VMAT planning for prostate cancer. Radiat Oncol 13, 163 (2018). https://doi.org/10.1186/s13014-018-1114-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13014-018-1114-y