Abstract
Background
To evaluate the clinical outcomes of patients treated with 3D conformal Hypo-fractionated, deep Inspiratory breath-hold (DIBH), Partial breast radiotherapy, termed “HIP.” HIP was implemented to merge the schedule of once-daily breast hypofractionation with partial breast treatment.
Methods
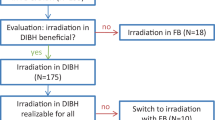
We identified 38 breast cancers in 37 patients from 2013 to 2014 treated at our institution with HIP following lumpectomy for early stage breast cancer. Patients received a hypo-fractionated course (≤ 20 fractions) of once daily radiation to the partial breast (lumpectomy cavity + margin) utilizing DIBH regardless of laterality. Clinical and treatment-related characteristics were obtained, including target volume and organ at risk (OAR) dosimetric characteristics. Patients were followed clinically and with at least yearly mammograms for up to 36 months (range 5–36 months). Acute and late toxicity was scored using the Common Terminology Criteria for Adverse Events (CTCAE) v4.03.
Results
Patients received a median dose of 42.56 Gy in 16 Fractions (Fx) (range 40.05–53.2 Gy; and 15–20 Fx). OAR doses were low, with a mean heart dose of 0.37 Gy, an ipsilateral lung V20 mean of 4%, and a contralateral lung V5 of 1%. Acute toxicity (≤ grade 2) was present in 79% (n = 30) of the cases, with dermatitis being the most common finding (63%). Late grade 1–2 toxicity was present in 42% (n = 16) of the cases, with hyperpigmentation being the most common finding (n = 9). There were no severe acute or late toxicities (≥ grade 3). At a median follow up of 21 months, there were no local, regional, or distant failures.
Conclusions
We report limited toxicity in this low risk cohort of patients with early stage breast cancer treated with HIP, a unique and logical combination of 3-D conformal external beam radiotherapy, moderate hypo-fractionation, and DIBH.
Similar content being viewed by others
Background
Breast cancer is the most commonly diagnosed malignancy among women in the United States. In 2013, there were an estimated 232,340 new cases accounting for 29% of all newly diagnosed cancers [1]. Breast conservation therapy (BCT), which includes lumpectomy (surgical resection of the tumor alone) and radiation therapy (RT), is the nationally accepted standard treatment approach for early stage breast cancer and is used in 70% of such patients [2, 3].
The use of adjuvant whole breast irradiation (WBI) following breast conservation surgery has been demonstrated in numerous clinical trials to reduce the rates of ipsilateral breast tumor recurrence (IBTR) by over 50% compared to lumpectomy alone [4, 5]. The advantage of BCT over mastectomy is avoidance of a larger surgical procedure, shorter surgical recovery time, superior cosmetic outcomes, and organ preservation; however, the disadvantage of adjuvant WBI is the prolonged treatment time of 3–7 weeks and additional radiation-induced toxicities. With strong clinical evidence to support its use, hypo-fractionation has become increasingly popular for patients in Canada and the United States for early stage breast cancer [2, 6, 7]. There is sufficient evidence from randomized clinical trials that hypo-fractionated RT is now considered the national preferred option for the majority of patients [6, 8, 9].
Approximately 75% of breast tumor recurrences occur within or near the lumpectomy cavity, triggering attempts to decrease the volume of breast treated with radiation [10,11,12]. PBI in conjunction with further hypofractionation, termed accelerated partial breast irradiation (APBI) can be delivered in several forms – brachytherapy with multicatheter balloons, brachytherapy with interstitial implants, or 3-dimensional conformal external beam radiotherapy (3D-CRT). Early data suggests that APBI is safe and effective, and it has been endorsed by the NCCN Guidelines [2]. Various selection criteria exist to guide clinicians in choosing the optimal patients for this technique, but generally, women at sufficient risk for local failure warranting adjuvant therapy, but not regional or distant failure, should be considered [13,14,15,16].
The optimal APBI dose and fractionation is currently unclear. The National Surgical Adjuvant Breast and Bowel Project (NSABP) B-39 clinical trial used a dose of 38.5 Gy in 10 fractions delivered twice daily for 3D-CRT and 34 Gy in 10 fractions for brachytherapy [17]. The 38.5 Gy dose was chosen as the biologically equivalent dose (BED) to 45 Gy in 25 fractions assuming an alpha/beta ratio of 10. This same dose was used in the Radiation Therapy Oncology Group (RTOG) 0319 clinical trial [18]. However, this dose and fractionation has led to concerns regarding the increased incidence of late cosmetic toxicity, including subcutaneous fibrosis and fat necrosis [19]. Further, some patients and providers may prefer once-daily fractionation schedules over twice-daily. IMRT has also been used with APBI, notably in the Florence NCT02104895 trial. A dose of 30 Gy in 5 daily fractions was compared to WBI of 50 Gy in 25 fractions, with a boost of 10 Gy in five fractions. In 520 patients, no significant difference was found in ipsilateral breast tumor recurrence or overall survival, and improved acute and late cosmetic outcomes were found in the APBI group [20]. The use of interstitial multicatheter brachytherapy for APBI has been studied, and Strnad et al. presented five year results of non-inferiority of local recurrence (1.44%) and side effects [21].
Taken together, there is strong evidence for the use of moderate hypo-fractionation (15–20 fractions) and PBI. A technique for hypo-fractionated PBI using 3D-CRT with deep inspiratory breath hold (HIP: hypo-fractionated inspiratory partial breast irradiation) was implemented at our institution. The 3D-CRT PBI is a particularly useful treatment technique, as it is applicable and readily available to nearly all centers. HIP merged two types of radiation therapy in a novel way by offering “Canadian” hypo-fractionation (15–20 daily fractions) with a partial breast volume. Deep inspiration breath-hold (DIBH) was employed to reduce cardiac dose [22,23,24] and improve target volume coverage by immobilizing the breast and decreasing toxicity to the ipsilateral lung [25].
This study seeks to identify early clinical outcomes of early stage breast cancer, including efficacy and toxicity associated with HIP.
Methods
Data collection
We conducted a retrospective analysis of 37 patients with 38 breast cancers treated with3D-CRT, hypo-fractionated PBI from 2013 to 2014 under our uniform institutional policy for HIP during this time period. Approval was obtained from institutional review board (IRB) prior to evaluating outcomes for these patients.
Clinical data was recorded for all eligible patients including: age, stage, histology, grade, estrogen/progesterone receptor status, Her-2-neu amplification status, lympho-vascular space invasion, multifocal disease, surgical margins, menopausal status, and adjuvant therapies (endocrine therapy or chemotherapy).
Treatment planning
CT simulation and technique
All patients underwent a computed tomography (CT) simulation positioned on a breast board in the supine position with arms raised overhead and a Vac-Lok (Med Tech Inc., Orange City, IA) for custom immobilization. Radio-dense markers were placed at the time of simulation to delineate the visible borders of breast tissue and the lumpectomy scar. DIBH technique was used for all patients regardless of laterality to increase the accuracy of the target volume location and reduce heart dose, as previously reported [26]. Patients were positioned with both arms raised over the head and custom immobilization. Then, the Varian real-time position management (RPM) system was used to initiate DIBH imaging and monitor the duration and displacement of each patient’s breath hold. This RPM signal was used as a baseline, and upper and lower limits of 0.5 cm from the baseline were established, such that treatment would only take place if the patient’s breath hold was within this displacement gate. Free breathing was allowed between treatment fields or if multiple breath holds were required for a given field [26]. All patients were treated with PBI using a once-daily fractionation schedule with a 3D conformal plan using multiple non-coplanar beams. Image-guidance included first day MV portal imaging and daily kV imaging to verify positioning and alignment.
Target volumes
The partial breast target volumes were based on the RTOG 1005 and NSABP B-39 clinical trials [17, 27]. The lumpectomy gross tumor volume (GTV) included all clinical and radiographic information of the excision cavity, architectural distortion, lumpectomy scar, seroma, and/or surgical clips. The use of surgical clips is standard for such cases at this institution. The lumpectomy clinical target volume (CTV) was defined as GTV + 10–15 mm uniform expansion and this was limited posteriorly at the anterior surface of the pectoralis muscles and anteriorly 5 mm from skin. The lumpectomy planning target volume (PTV) was defined as CTV + 7 - 10 mm. The beam apertures were chosen based on the PTV. To evaluate our target volume coverage and dose-volume constraints, the PTV was copied to create a PTV_Eval. The PTV_Eval was defined as PTV excluding the region outside of breast tissue, i.e. cropped posteriorly at the anterior border of the pectoralis muscles and anteriorly 5 mm from skin. One characteristic treatment plan is shown in Fig. 1.
Plan evaluation
Treatment related characteristics and dosimetric data were recorded including: laterality, total dose, number of fractions, and organ at risk data including heart mean dose, volume of heart receiving 20 Gy or more (heart V20), volume of ipsilateral lung receiving 20 Gy or more (ipsilateral lung V20), volume of contralateral lung receiving 5 Gy or more (contralateral lung V5), contralateral breast maximum and mean.
Treatment outcomes
During treatment, patients were evaluated by a physician at least once weekly, including the radiation and breast oncology teams. Clinical follow up data includes history, physical exam, and mammograms. Breast cancer recurrence was recorded as: ipsilateral breast tumor recurrence (IBTR) (in the PTV, outside the PTV, or skin), ipsilateral nodal recurrence, contralateral breast failure, or distant failure.
Toxicity was graded according to the Common Toxicity Criteria for Adverse Events (CTCAE v4.03) to evaluate both acute (≤ 90 days post-treatment) and late (> 90 days post-treatment) findings [28]. Toxicities were reported as fatigue, breast pain, dermatitis, pruritus, skin hyper/hypo-pigmentation, skin induration, skin ulceration, telangiectasia, breast fibrosis, lung complications, heart complications, and lymphopenia.
Results
Clinical characteristics
Of the 38 breast cancers in this study, 23.7% were stage 0, 86.8% were stage IA, 0% were stage IB, and 7.9% were stage IIA. Patient and tumor characteristics are listed in Table 1. All patients were deemed “suitable” or “cautionary” per ASTRO consensus guidelines for APBI [16]. While 78.9% of the patients were considered cautionary per the 2009 recommendations, this number decreased to 36.8% in the updated 2016 recommendations, as seen in Table 2 [29]. The recent update stated that ductal carcinoma in situ (DCIS) is suitable for APBI if it is screening-detected, low to intermediate nuclear grade, size ≤2.5 cm, and resected with margins negative at ≥3 mm. Of the cautionary patients, 43% were estrogen receptor negative, and 36% had invasive lobular carcinoma (ILC) on histologic review. Clinical outcomes using APBI with ILC have been found to be no different than those with invasive ductal histology, hence their inclusion in this study [30]. There were no unsuitable patients treated in this study.
Treatment characteristics
The median total dose was 42.56 Gy (range of 40.05–53.20 Gy), over a median 16 Fx (range of 15–20 Fx). Table 3 provides radiation treatment characteristics of the entire cohort.
Toxicity
Toxicity data is listed in Table 4. Acute toxicity of any kind was recorded in 30 of 38 cases (79%) within 90 days of completion of treatment. There were no grade 3 or greater acute toxicities. Overall, acute dermatitis (58% grade 1 and 5% grade2) was the most common finding, followed by fatigue (8% grade 1 and 5% grade 2) and hyperpigmentation (13% grade 1). There were no cases of hypopigmentation, ulceration, telangiectasia, or fibrosis.
Late toxicity of any kind was recorded in 16 of 36 cases (42%). Long term data was not available for 2 cases. There were no grade 2 or greater late toxicities. Only grade 1 toxicity was noted, and it was most commonly hyperpigmentation (24%), followed by fibrosis (21%). There were no cases of late dermatitis, pruritus, hypopigmentation, ulceration, telangiectasia, or pain.
Disease control
At a median follow up of 21 months, there were no local, regional, or distant failures, including IBTR in and out of the field, skin recurrence, and contralateral breast failure.
Discussion
Our results demonstrate a favorable rate of acute and late toxicity following HIP. The Whelan Trial reported comparable rates of good or excellent cosmetic outcomes in the control WBI group compared to the hypo-fractionated arm (71% vs. 70%) at 10 years of follow up [8]. The Royal Marsden Hospital/Gloucestershire Oncology Center (RMH/GOC) trial similarly found that 30.3–45.7% of patients recorded some change in breast appearance at 5 years [31]. Similarly, our results showed that 10 of 38 treatments resulted in breast appearance changes (26.3%). Further, our data showed no cases of telangiectasia, whereas the RMH/GOC trial showed rates of 13.8–14.3%.
Some concerns remain regarding late toxicity and poor cosmesis. The RAPID trial compared standard WBI to 38.5 Gy in 10 Fx external beam APBI, showing worse grade 1–2 toxicity and cosmesis in the experimental APBI arm at 3 years [32]. Conversely, the UK IMPORT LOW trial utilized a dose of 40 Gy in 15 Fx to the partial breast, and this trial not only found PBI at this dose to be non-inferior regarding local relapse but also adverse effects were similar to better when compared to WBI [33]. The PBI group had better late outcomes at 5 years regarding skin change, overall breast appearance, smaller breast, and breast firmness. Thus, although some data raises concern regarding APBI toxicity (e.g. the RAPID trial), there is a growing body of literature demonstrating non-inferior – or even superior – toxicity outcomes [33].
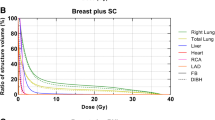
The low incidence of late adverse effects reported in our study coupled with the improved cosmesis in the IMPORT LOW study may reflect the inherent differences of dose fractionation. Late-responding normal tissues (e.g. dermal skin) are characterized by a low α/β ratio. Figure 2 demonstrates that the frequently utilized dose fractionation schedules for PBI (including 38.5 Gy in 10 Fx) have similar EQD2 and BED10 values compared to standard WBI hypo-fractionation doses (used in both these patients and the IMPORT LOW study); however, the BED3 and BED 1.5 of normal tissues is substantially higher with the 38.5 Gy in 10 Fx schedule.
Dose comparisons of various dose/fractionation schedules for breast irradiation. Blue: 38.5 Gy in 10 Fx (RAPID and NSABP B-39 trials); Red: 43.54 Gy in 16 Fx(mean HIP dose); Green: 42.56 Gy in 16 Fx (median HIP dose, Whelan/Ontario hypo-fractionation); Purple: 45 Gy in 25 Fx (conventional fractionation). Abbreviations: EQD2: equivalent dose in 2 Gy fractions, BED10: biologically effective dose for tissue/tumor with an α/β ratio of 10, 3 and 1.5 respectively
DIBH was developed to reduce cardiac dose. Epidemiological studies have found higher mortality from myocardial infarction with left-sided breast RT compared to right-sided, and reduction of cardiac dose has been shown to decrease ischemic heart disease [22,23,24]. In this study, heart V20 was 0%, and the mean heart dose was 0.37 Gy (range 0.14–0.94 Gy). Compared to brachytherapy APBI, DIBH WBI has been shown to have a lower heart dose [34]. In our study, the low heart dose is likely a combination of PBI and DIBH. DIBH also further immobilizes the breast during treatment, improving the accuracy of dose delivery and reducing radiation doses to the ipsilateral lung [35]. In this case, ipsilateral lung V20 had a mean of 4.0% (range 0–13).
The limitations of this study include the retrospective analysis by nature, which obfuscates detailed cosmetic analysis at long term intervals. The follow up of 22 months is likely insufficient time to capture many instances of IBTR, but it is sufficient to note acute toxicity and most late toxicity associated with RT. The cohort size is small, largely due to the unique scheduling and delivery method applied to this patient set.
Conclusion
We report limited toxicity without early recurrences in this low risk cohort of patients with early stage breast cancer treated with HIP, a unique combination of 3D-CRT external beam radiotherapy, moderate hypo-fractionation, and DIBH. HIP offers early recurrence and toxicity findings consistent with previous PBI trials, such as IMPORT LOW, and the addition of DIBH offers the potential to further reduce patient motion and toxicity.
Abbreviations
- ALND:
-
Axillary lymph node dissection
- APBI:
-
Accelerated partial breast irradiation
- ASTRO:
-
American Society for Radiation Oncology
- BCT:
-
Breast conservation therapy
- BED:
-
Biologically equivalent dose
- BED10 :
-
Biologically effective dose for tissue/tumor with an α/β ratio of 10, 3 and 1.5, respectively
- CT:
-
Computed tomography
- CTCAE v4.03:
-
Common Toxicity Criteria for Adverse Events
- CTV:
-
Clinical target volume
- DCIS:
-
Ductal carcinoma in situ
- DIBH:
-
Deep inspiratory breath-hold
- Dmax:
-
Maximum point dose
- EQD2:
-
Equivalent dose in 2 Gy fractions
- ER:
-
Estrogen receptor
- Fx:
-
Fractions
- GTV:
-
Gross tumor volume
- Gy:
-
Gray
- HER2:
-
Human epidermal growth factor receptor 2
- HIP:
-
Hypo-fractionated, deep Inspiratory breath-hold, Partial breast radiotherapy
- IBTR:
-
Ipsilateral breast tumor recurrence
- IRB:
-
Institutional review board
- LVSI:
-
Lympho-vascular space invasion
- NSABP:
-
National Surgical Adjuvant Breast and Bowel Project
- PBI:
-
Partial breast irradiation
- PR:
-
Progesterone receptor
- PTV:
-
Planning target volume
- RMH/GOC:
-
Royal Marsden Hospital / Gloucestershire Oncology Center
- RT:
-
Radiation therapy
- RTOG:
-
Radiation Therapy Oncology Group
- SLNBx:
-
Sentinel lymph node biopsy
- V20:
-
Volume of an organ receiving at least 20 Gy
- V5:
-
Volume of an organ receiving at least 5 Gy
- WBI:
-
Whole breast irradiation
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2017. CA Cancer J Clin. 2017;67:7–30.
Gradishar WJ, Anderson BO, Balassanian R, Blair SL, Burstein HJ, Cyr A, et al. NCCN guidelines insights breast Cancer, version 1.2016. J Natl Compr Cancer Netw. 2015;13:1475–85.
Agarwal S, Pappas L, Neumayer L, Kokeny K, Agarwal J. Effect of breast conservation therapy vs mastectomy on disease-specific survival for early-stage breast cancer. JAMA Surg. 2014;149:267–74.
Fisher B, Anderson S, Bryant J, Margolese RG, Deutsch M, Fisher ER, et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med. 2002;347:1233–41.
Veronesi U, Saccozzi R, Del Vecchio M, Banfi A, Clemente C, De Lena M, et al. Comparing radical mastectomy with quadrantectomy, axillary dissection, and radiotherapy in patients with small cancers of the breast. N Engl J Med. 1981;305:6–11.
Smith BD, Bentzen SM, Correa CR, Hahn CA, Hardenbergh PH, Ibbott GS, et al. Fractionation for whole breast irradiation: an American Society for Radiation Oncology (ASTRO) evidence-based guideline. Int J Radiat Oncol Biol Phys. 2011;81:59–68.
Tran K, Rahal R, Brundage M, Fung S, Louzado C, Milosevic M, et al. Use of low-value radiotherapy practices in Canada: an analysis of provincial cancer registry data. Curr Oncol. 2016;23:351–5.
Whelan TJ, Pignol JP, Levine MN, Julian JA, MacKenzie R, Parpia S, et al. Long-term results of hypofractionated radiation therapy for breast cancer. N Engl J Med. 2010;362:513–20.
Kim KS, et al. Hypofractionated whole breast irradiation: new standard in early breast cancer after breast-conserving surgery. Radiat Oncol J. 2016;34(2):81.
Fisher ER, Anderson S, Tan-Chiu E, Fisher B, Eaton L, Wolmark N. Fifteen-year prognostic discriminants for invasive breast carcinoma: National Surgical Adjuvant Breast and bowel project Protocol-06. Cancer. 2001;91:1679–87.
Faverly DR, Burgers L, Bult P, Holland R. Three dimensional imaging of mammary ductal carcinoma in situ: clinical implications. Semin Diagn Pathol. 1994;11:193–8.
Kurtz JM, Amalric R, Brandone H, Ayme Y, Spitalier JM. Results of wide excision for mammary recurrence after breast-conserving therapy. Cancer. 1988;61:1969–72.
Shah C, Badiyan S, Ben Wilkinson J, Vicini F, Beitsch P, Keisch M, et al. Treatment efficacy with accelerated partial breast irradiation (APBI): final analysis of the American Society of Breast Surgeons MammoSite((R)) breast brachytherapy registry trial. Ann Surg Oncol. 2013;20:3279–85.
Shah C, Vicini F, Wazer DE, Arthur D, Patel RR. The American brachytherapy society consensus statement for accelerated partial breast irradiation. Brachytherapy. 2013;12:267–77.
Polgar C, Van Limbergen E, Potter R, Kovacs G, Polo A, Lyczek J, et al. Patient selection for accelerated partial-breast irradiation (APBI) after breast-conserving surgery: recommendations of the Groupe Europeen de Curietherapie-European Society for Therapeutic Radiology and Oncology (GEC-ESTRO) breast cancer working group based on clinical evidence (2009). Radiother Oncol. 2010;94:264–73.
Smith BD, Arthur DW, Buchholz TA, Haffty BG, Hahn CA, Hardenbergh PH, et al. Accelerated partial breast irradiation consensus statement from the American Society for Radiation Oncology (ASTRO). Int J Radiat Oncol Biol Phys. 2009;74:987–1001.
Vicini FA, White J, Arthur D. NSABP B-39/RTOG 0413 protocol, A randomized phase III study of conventional whole breast irradiation (WBI) versus partial breast irradiation (PBI) for women with stage 0, I or II breast cancer. 2005.
Vicini FA, et al. Initial efficacy results of RTOG 0319: Three dimensional conformal radiation therapy (3D-CRT) confined to the region of the lumpectomy cavity for Stage I/II breast carcinoma. Int J Radiat Oncol Biol Phys. 2008;72(1):S3.
Leonard KL, Hepel JT, Hiatt JR, Dipetrillo TA, Price LL, Wazer DE. The effect of dose-volume parameters and interfraction interval on cosmetic outcome and toxicity after 3-dimensional conformal accelerated partial breast irradiation. Int J Radiat Oncol Biol Phys. 2013;85:623–9.
Livi L, et al. Accelerated partial breast irradiation using intensity-modulated radiotherapy versus whole breast irradiation: 5-year survival analysis of a phase 3 randomised controlled trial. Eur J Cancer. 2015;51(4):451–63.
Strnad V, et al. 5-year results of accelerated partial breast irradiation using sole interstitial multicatheter brachytherapy versus whole-breast irradiation with boost after breast-conserving surgery for low-risk invasive and in-situ carcinoma of the female breast: a randomised, phase 3, non-inferiority trial. Lancet. 2016;387(10015):229–38.
Rutter CE, Chagpar AB, Evans SB. Breast cancer laterality does not influence survival in a large modern cohort: implications for radiation-related cardiac mortality. Int J Radiat Oncol Biol Phys. 2014;90:329–34.
Rutqvist LE, Johansson H. Mortality by laterality of the primary tumour among 55,000 breast cancer patients from the Swedish Cancer Registry. Br J Cancer. 1990;61:866–8.
Latty D, et al. Review of deep inspiration breath-hold techniques for the treatment of breast cancer. J Med Radiat Sci. 2015;62(1):74–81.
Shim J-G, et al. Dose-volume analysis of lung and heart according to respiration in breast cancer patients treated with breast conserving surgery. J Breast Cancer. 2012;15(1):105–10.
Reardon KA, Read PW, Morris MM, Reardon MA, Geesey C, Wijesooriya K. A comparative analysis of 3D conformal deep inspiratory-breath hold and free-breathing intensity-modulated radiation therapy for left-sided breast cancer. Med Dosim. 2013;38:190–5.
Radiation Therapy Oncology Group. RTOG 1005: a phase III trial of accelerated whole breast irradiation with hypofractionation plus concurrent boost versus standard whole breast irradiation plus sequential boost for early-stage breast cancer. 2013.
US Department of Health and Human Services. Common terminology criteria for adverse events (CTCAE) version 4.0. National Institutes of Health, National Cancer Institute 4.03; 2009.
Correa C, Harris EE, Leonardi MC, Smith BD, Taghian AG, Thompson AM, et al. Accelerated partial breast irradiation: executive summary for the update of an ASTRO evidence-based consensus statement. Pract Radiat Oncol. 2017;7:73–9.
Shah C, et al. Clinical outcomes using accelerated partial breast irradiation in patients with invasive lobular carcinoma. Int J Radiat Oncol Biol Phys. 2011;81(4):e547–51.
Yarnold J, Ashton A, Bliss J, Homewood J, Harper C, Hanson J, et al. Fractionation sensitivity and dose response of late adverse effects in the breast after radiotherapy for early breast cancer: long-term results of a randomised trial. Radiother Oncol. 2005;75:9–17.
Olivotto IA, Whelan TJ, Parpia S, Kim DH, Berrang T, Truong PT, et al. Interim cosmetic and toxicity results from RAPID: a randomized trial of accelerated partial breast irradiation using three-dimensional conformal external beam radiation therapy. J Clin Oncol. 2013;31:4038–45.
Coles CE, et al. Partial-breast radiotherapy after breast conservation surgery for patients with early breast cancer (UK IMPORT LOW trial): 5-year results from a multicentre, randomised, controlled, phase 3, non-inferiority trial. Lancet. 2017;390(10099):1048–60.
Holliday EB, Kirsner SM, Thames HD, Mason BE, Nelson CL, Bloom ES. Lower mean heart dose with deep inspiration breath hold-whole breast irradiation compared with brachytherapy-based accelerated partial breast irradiation for women with left-sided tumors. Pract Radiat Oncol. 2017;7:80–5.
Essers M, Osman SO, Hol S, Donkers T, Poortmans PM. Accelerated partial breast irradiation (APBI): are breath-hold and volumetric radiation therapy techniques useful? Acta Oncol. 2014;53:788–94.
Funding
This research required no funding.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
ROK was involved in data analysis, writing and drafting the manuscript, and finalizing edits for the manuscript. KDR was also involved in data analysis, writing and drafting the manuscript, and finalizing edits for the manuscript. DMT was primarily involved in analyzing the data and finalizing edits for the manuscript. SWD assisted with editing and finalizing the manuscript. TNS helped with editing and finalizing the manuscript. MMM was involved in primary data collection and finalizing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Approval was obtained from institutional review board (IRB) prior to evaluating outcomes for these patients.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Kowalchuk, R.O., Romano, K.D., Trifiletti, D.M. et al. Preliminary toxicity results using partial breast 3D-CRT with once daily hypo-fractionation and deep inspiratory breath hold. Radiat Oncol 13, 135 (2018). https://doi.org/10.1186/s13014-018-1079-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13014-018-1079-x