Abstract
Background
Ineffective breastfeeding technique is one of the factors contributing to mothers practicing non-exclusive breastfeeding. Inappropriate breastfeeding technique is the leading cause of nipple pain in Ethiopia, as in other countries. However, no studies have examined breastfeeding technique and associated factors in eastern Ethiopia. Therefore, this study was conducted with the aim of assessing breastfeeding technique and associated factors among breastfeeding mothers.
Method
We conducted an institution based cross-sectional study in selected governmental health facilities of Harar city, Eastern, Ethiopia, from January to February 2017. Systematic random sampling technique was used to select 422 study participants. Data were collected using pretested observational checklist and interviewer administered questionnaires containing sociodemographic, maternal and infant characteristics. The variables, positioning, attachment and suckling, were used to assess the outcome variable of breastfeeding technique. Descriptive, bivariate and multivariate logistic regression analysis was done to identify independent predictors of BFT after controlling for confounding variables.
Result
The proportion of mothers practicing an effective breastfeeding technique was 43.4% (179/412). Effective breastfeeding technique was 2.3 times more common among mothers with at least secondary school educational status compared to mothers with no formal education (Adjusted Odds Ratio [AOR] 2.3; 95% Confidence Interval [CI] 1.1, 3.9). The practice of effective breastfeeding technique was significantly associated with mothers who had immediate breastfeeding technique counseling after birth (AOR 1.7, 95% CI 1.1, 2.8) and at least two postnatal visits (AOR 5.9; 95% CI 2.1, 15.9) compared to one visit. Absence of breast problems and having previous breastfeeding experience were also associated with the likelihood of effective breastfeeding technique practice (AOR 4.0; 95% CI 1.4, 10.9) and (AOR 3.3; 95% CI 1.1, 10.7) respectively.
Conclusion
The practice of effective breastfeeding technique was low. Effective breastfeeding technique practice was associated with higher educational status, previous information about breastfeeding technique, previous breastfeeding experience, absence of breast problems, receiving breastfeeding technique counseling immediately after birth and at least two postnatal visits. Therefore; health services should provide education about effective breastfeeding techniques and ensure postnatal care for all women, particularly primipara.
Similar content being viewed by others
Background
Breastfeeding technique is the composite of positioning attachment and suckling [1]. Positioning refers to the technique in which the infant is held in relation to the mother’s body and attachment refers to whether the infant has enough areola and breast tissue in the mouth [2]. Proper positioning of the mother, good attachment of the baby to the breast and effective suckling is a function of effective breastfeeding technique [3, 4]. Performing effective breastfeeding technique (BFT) has been shown to be important to establish breastfeeding, to ensure milk transfer and to prevent breastfeeding problems [5,6,7,8,9,10,11].
Although breastfeeding technique is a natural act or phenomenon, it is not an instinctual behavior and requires a learned skill [9,10,11,12]. Once the mother knows the steps of effective BFT, she can better prevent and cope with most breastfeeding problem that might occur [9]. Most difficulties can be avoided together if good attachment and positioning are achieved at the first and early feeds [3].
A strong correlation between the onset of sore nipples and practice of ineffective breastfeeding technique among nursing mothers has been described [13, 14]. Thus, it is one of the major contributor to cause early cessation of breastfeeding practice [15]. A small localized based study in India indicated that ineffective BFT was present in about 57% and 63% of children suffering from diarrhea and ARI respectively [16].
Ineffective BFT results in insufficient intake of breast milk and this will cause poor weight gain and stunting and the baby may also become difficult to feed. Poor positioning, attachment and suckling also leads to sharp reduction of exclusive breastfeeding practice and increase breastfeeding problem [1, 15, 17,18,19,20].
Poor BFT was the leading cause of cracked nipple among breastfeeding mothers [13, 14]. Nipple damage and mastitis were more common among mothers with poor positioning and attachment [21]. Furthermore, breastfeeding problems were 2.44 times more common among mothers who practice ineffective BFT compared to who had effective BFT practice [22].
Several studies have proposed various solutions: education and counseling of mothers about effective BFT, training of health care professional with regard to good positioning, attachment and effective suckling, and giving special attention to young, primipara and poorly educated women [21,22,23,24]. Moreover; integrated management and childhood illness (IMNCI) guideline in Ethiopia also recommend that maternal and child health care providers are expected to ensure education and counseling of mothers about effective BFT and discourage supplementary feeding before six months [1]. Results from interventional studies have indicated that training of health care providers and continuing education, combining discussion with use of educational materials and practical demonstrations for breastfeeding mothers about positioning and attachment resulted in significant improvements in practice of effective BFT [24,25,26].
Although many studies about breastfeeding practice have been conducted in Ethiopia, the issue of breastfeeding technique has been overlooked. Therefore; this study was conducted with the objective of assessing BFT and associated factors among breastfeeding mothers attending governmental health facilities in Harar city.
Method
The study was conducted in Harar city, Eastern, Ethiopia which is located 525 km from the capital city Addis Ababa. The population of the city is estimated to be 240,000 and 53,383 were women in the reproductive age group. There are 6 hospitals (4 government & 2 private hospitals) and 8 health centers which provide delivery and immunization services. The total number of eligible population in the city for antenatal care delivery and postnatal care was around 7604 [27]. This cross-sectional study design was conducted in Harar city governmental health facilities from 27 January 2017 to 26 February 2017.
Study participants
All breastfeeding mothers in governmental health facilities of Harar city were the source population. Two groups of mother infant pair were recruited from postnatal unit and expanded program of immunization (EPI) unit. The study recruited immediate postpartum mother whose neonate was alive and mother coming for postnatal care visit at postnatal unit, and mothers coming for infant immunization service at EPI unit.
Therefore, all breastfeeding mothers who were in EPI unit and postnatal care unit in selected governmental health institutions (HIs) were included as the study population. Mothers who were seriously sick and unable to breastfeed, and whose infants were actually ill and refused to feed, very preterm birth and neonate with cleft lip and cleft palate were excluded from the study.
Sample size calculation
Single population proportion formula was used to determine the sample size for this study with the assumption of 95% confidence interval (CI), margin of error 5% and 51% prevalence of effective BFT [22]. Considering 10% non-response rate, the total sample size was determined to be 422 breastfeeding mothers.
Four health facilities were selected by lottery method, and proportional allocation was done to select the sample from postnatal care unit and EPI unit of selected health facilities. Finally, systematic random sampling technique was employed to select study participant from postnatal care unit and EPI unit.
Data measures
The study was conducted by using observation checklist and interviewer administered questionnaire containing sociodemographic, maternal and infant characteristics. An observation checklist was used to assess mother and baby’s position, infant’s mouth attachment and effective suckling during breastfeeding using World Health Organization (WHO) B-R-E-A-S-T- Feed Observation form [28]. The questionnaires were developed and modified from relevant studies in order to address all the variables necessary to meet the objective of this study [11, 21, 23, 29]. Interviewer administered questionnaires were prepared first in English and then translated in to Amharic and Afan Oromo language as per the mother tongue of the participant and translated back to English for consistency by language experts. The checklist and questionnaires were pre-tested on the population of 5% of the sample size of this study in Dire Dawa Dilchora Hospital. Then, correction and modification of the tool was undertaken accordingly. The following arbitrary scoring and grading system was developed and adopted to grade positioning (mother and infant), infant’s mouth attachment and effective suckling during breastfeeding based on WHO criteria [28]. Each criterion was assigned 1 point (Table 1).
Operational definitions
Effective breastfeeding technique (BFT)
The combination of at least two criteria from positioning, three criteria from attachment and two criteria from suckling are fulfilled while mothers breastfeed their infants [22].
Parity - Indicates the number of pregnancies reaching viable gestation.
-
Low birth weight - weight at birth of less than 2.5 kg.
-
Normal birth weight – weight of neonate at birth above or equal to 2.5 kg but less than 4 kg.
-
Macrosomia – weight of neonate at birth above 4 kg.
-
Preterm birth – a neonate born before 37 completed weeks. But for this study it is operationalized as age at birth between 34 and 36 completed weeks of gestation.
-
Term - a neonate born any time after 37 completed weeks of gestation and up until 42 completed weeks of gestation.
-
Post-term - a neonate born any time after completion of the 42 weeks.
Breast problem – are problems if a woman has any of the following:
-
Inverted nipple - a portion of or the entire nipple is buried below the plane of the areola and does not evert at all (grade III) [30];
-
Engorgement – breasts are painfully overfull;
-
Cracked nipple – damage to the integrity of the skin on the nipple;
-
Mastitis – inflammatory condition of the breast, which may or may not be accompanied by infection [31].
Data collection
Eight female bachelor science (BSc.) midwives and two supervisors who were not working in the assigned health facilities were trained by the investigators on how to collect data and observe the positions of the mother and baby, infant’s mouth attachment to breast and effective suckling by using video clips and hands on practice. In addition, they observed BFT with clients at nearby health facilities. Data collectors observed the breastfeeding process for five minutes and recorded the mother and infant’s positioning, attachment to the breast and effective suckling as per WHO B-R-E-A-S-T Feed observation form. It was done by asking the mother to put her infant to the breast, if the infant had not been fed in the previous hour. If the infant had been fed during the last one hour, then the mother was asked when the infant would have the next feed and the observation assessment was planned accordingly. The investigator and supervisor closely followed the data collection process throughout the data collection period. They checked the collected data for completeness each day and corrective measures were taken accordingly.
Data processing and analysis
The data were first coded, double data entry were done by two data clerks and consistency of the entered data were cross checked by comparing the two separately entered data and cleaned using EpiData statistical software version 3.1. Entered data exported into statistical package for social science (SPSS) software version 21 for analysis. The three variables i.e. positioning, attachment and suckling were used to create a single variable of BFT [22]. The outcome variable BFT was classified as either effective BFT or ineffective BFT. Descriptive statistics of each variable was determined and the results were presented in texts, tables and graphs using summary measures such as percentages, mean and standard deviation. Hosmer-Lemeshow’s and Omnibus goodness-of-fit test was used to assess whether the necessary assumptions for the application of bivariate and multivariate logistic regression. In the Hosmer-Lemeshow test, the Pearson’s chi-square should not be significant but it should be significant in Omnibus test if the model said to be fitted. Bivariate logistic regression was carried out to identify the predictors associated with BFT. All variables with p-value of ≤0.25 in bivariate logistic regression were included in the multivariable model. In the multivariate analysis, standard enter techniques were fitted. Variables having p value ≤ 0.05 in the multivariate analysis were taken as significant predictors. Crude odd ratios (COR) and adjusted odds ratios (AOR) with their 95% confidence intervals (CI) were calculated.
Results
Sociodemographic characteristics of the participants
Of 422 study participants, 412 were observed for BFT and interviewed, giving a response rate of 97.6%. Interview and observation was done on a total of 194 (47.1%) breastfeeding mothers from postpartum ward or postnatal care unit and 218 (52.9%) breastfeeding mothers from EPI unit. About 44 % 181(43.9%) of mothers were in the age group of 20–25 years. The majority of the respondents (76.7%) were housewives, and the mean age of the study participants were 25. 8 years with SD ± 5.34 years (Table 2).
Maternal characteristics of the participants
Just over half the participants had received information about BFT (52.9%). Of the total participants, the majority (85%) did not think that breastfeeding is painful and 18.7% complained that BFT takes time. Regarding breastfeeding experience, 60% had previous breastfeeding experience; 9.3% had previous breastfeeding experience < 1 years, 56.3% and 34.4% had previous duration of breastfeeding experience 1 year to 2 years and above 2 years respectively. From 412 study participants, 35 (8.5%) were diagnosed with a breast problem at the time of data collection. Engorgement was the commonest breast problem, accounting for around 46%, followed by cracked nipple and inverted nipple (each 20%), followed by mastitis or other problems.
Obstetrics and infant factors
Nearly two thirds (61.7%) of participants were multiparous; hospitals were the commonest place for delivery (87.4%) and only 2.2% gave birth at home (Table 3).
Effective breastfeeding technique
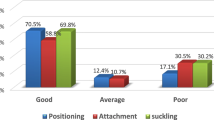
The proportion of effective BFT was 42.2% (82/194) in the postnatal unit and 44.5% (97/218) in the EPI unit. Good positioning (65.3%) and good suckling (69.2%) were observed during breastfeeding (Fig. 1). Effective BFT was more common among mothers who had at least two postnatal visits (81.3%), information about BFT (55.5%), working mothers (54.2%) and previous breastfeeding experience (50.6%) (Fig. 2).
Factors affecting breastfeeding technique
Regression analysis was run in order to identify variables with significant association with the condition of BFT. In multivariable analysis model, there was a statistically significant positive association with respect to effective BFT among mothers who have educational status of secondary school and above (AOR 2.3; 95% CI 1.1, 3.9), those who had previous breastfeeding experience (AOR 3.3; 95% CI 1.1, 10.7) and absence of breast problems (AOR 4.0; 95% CI 1.4, 10.9). Practice of effective BFT was 1.9 times more common among mothers who had information about BFT (AOR 1.8; 95% CI 1.1, 3). Likewise, mothers who had at least two postnatal visits had increased odds of performing effective BFT practice compared to their counterparts (AOR 5.9; 95% CI 2.1, 15.9). Similarly, there was an association with practice of effective BFT among mother who had immediate counseling about BFT after birth (AOR 1.7; 95% CI 1.1, 2.8) (Table 4).
Discussion
We found that the overall prevalence of effective BFT was 43.4%. The prevalance was lower than in a study done in west Denmark (52%) [22]. This discrepancy might be due to routine in service delivery of information and demonstration about effective BFT for breastfeeding mothers or it might be due to differences on awareness level of the mothers and educational status.
Our result showed that the proportion of effective BFT was nearly similar in the postnatal care unit (42.3%) and EPI unit (44.5%). This showed that the practice of effective BFT is not affected by being immediately after delivery or after a time, rather the awareness and educational level of mothers in particular and access to postnatal care services.
The educational status of the respondents had a significant impact on parctice of effective BFT. Mothers who had secondary school education and above were 2.3 times more likely to practice effective BFT compared to their counterparts. This was in accordance with a study done in Indian East Delhi, west Bengal Kolkata hospital, Saudi Heraa general hospital and Sri Lanka [11, 23, 32, 33]. This is due to the fact that more educated mothers had strong intention and willingness to breastfeed. This factor positively affected the ability of mothers to give more emphasis on instruction, guidance and support from maternal and child health care providers to have successful breastfeeding technique [34,35,36]. Moreover; this might be due to, educated mothers are more likely to acquire and observe BFT from their edacational carrier or which might be due to the fact that mothers of poor educational status take more time to adopt the correct breastfeeding technique.
The present study was able to demonstrate that mothers who had previous information about BFT was 1.9 times more likely to practice effective BFT compared to their counterparts. Likewise, lack of information about BFT in India, East Delhi had significantly influenced the practice of effective BFT [11]. The process of the association can be, mothers who had awareness are more eager to know about the importance of BFT and this made them how to apply the technique in a step wise practical fashion.
In this study, effective BFT was more commonly observed among mothers who had previous breastfeeding experience compared to mothers who had no prior experience. This was consistent with a study done in India, East Delhi and western Denmark [11, 22]. Possible explanations might be that they had acquired skills from practice or they might have access to support and guidance previously.
Breast problems like cracked nipples, mastitis and engorgement were significantly associated with prevalance of ineffective BFT. This was in congruent with studies held in Libya Benghazi hospital and Pakistan Khyber Teaching Hospital [21, 37]. Breast engorgement makes it more difficult for the newborn infant to latch-on correctly because of distension and edema of the nipple and areolar region [38]. Poor BFT can also lead to nipple damage and mastitis.
In our study, presence of routine provision of immidiate counseling and demonestration about effective BFT after delivery had significant impact on practice of effective BFT, which is consistent with several studies done in Bangladesh, Saudi Heraa general hospital, rural area of north India and rural area of Nagpur district [24, 32, 39, 40]. Moreover; having at least two postnatal visits two increased the likelihood of effective BFT (81.3%) compared to mothers who had only one postnatal visit (41%). This was true in Bangladesh among two groups of postpartum mothers, there were a significant positive association with practice of effective BFT among mothers who received both early and late postnatal care visit compared to only one visit by Community health worker [24]. This is likely to be due to the fact that psychological support for breastfeeding mothers through early counselling and hands-on support for achieving proper techniques, particularly position and attachment [33].
This study was the first of its kind to give an insight into the status of BFT in the study area. We used both an observation checklist and interview to assess BFT to ensure a methodologically sound study. However, study limitations include the lack of a validated WHO instrument and the possible Hawthorne effect [41].
Conclusions
The study showed that proportion of effective BFT was low. The practice of effective BFT was mainly affected by educational status, presence of previous breastfeeding experience, mothers access to educational counseling immediately after delivery about BFT and prior information about BFT. Moreover; there were a significant positive association with effective BFT among mothers who have postnatal care visit ≥2 and those not identified with breast problem during data collection. Harari Regional Educational Bureau in collaboration with Ministry of Health should advocate women’s education and strengthen existing positive activities. All maternal and child health care provider in Harari Regional State Health facilities expected to work on information education and communication and demonstration for breastfeeding mothers and should consider it as their routine activities. Maternal, neonatal and child health care providers and, health extension workers expected to ensure postnatal care utilization. On top of that, prime attention, guidance and support should be given for mothers, who are novice to breastfeeding and have breast problem.
References
Federal Ministry of Health. Integrated Management of Childhood Illness. Addis Ababa: Federal Ministry of Health; 2016.
Neonatal Coordinating Group. Neonatology Clinical Guidelines King Edward Memorial/Princess Margaret Hospitals. NCCU Clinical Guideline; 2014. p. 3–5. Available at: http://www.kemh.health.wa.gov.au/services/nccu/guidelines/documents/MonitoringAndObservationFrequencyGuidelines.pdf.
Dongre AR, Deshmukh PR, Rawool AP, Garg BS. Where and how breastfeeding promotion initiatives should focus its attention? A study from rural Wardha. Indian J Community Med. 2010;35:226–9.
Mulder P. A concept analysis of effective breastfeeding. J Obstet Gynecol Neonatal Nurs. 2006;35:332–9.
Coca KP, Gamba MA, Silva RS, Abrão ACFV. Does breastfeeding position influence the onset of nipple trauma? Revista da Escola de Enfermagem University of São Paulo. 2009;43:442–8.
Coca KP, Gamba MA, Silva RS, Abrão ACFV. Factors associated with nipple trauma in the maternity unit. J Pediatr. 2009;85:341–5.
Inch S. Breastfeeding problems prevention and management. Community Pract. 2006:165–7.
De Oliveira LD, Giugliani ERJ, Santo LC do E, França MCT, Weigert EML, Kohler CVF, et al. Effect of intervention to improve breastfeeding technique on the frequency of exclusive breastfeeding and lactation related problems. J Hum Lact. 2006;22:315–21.
World Health Organization. Baby Friendly Hospital Initiative, Section 3. Geneva: Breastfeeding Promotion and Support in a Baby-Friendly Hospital; 2009. p. 99–104.
Puapornpong P, Paritakul P, Suksamarnwong M, Srisuwan S, Ketsuwan S. Nipple pain incidence, the predisposing factors, the recovery period after care management, and the exclusive breastfeeding outcome. Breastfeed Med. 2017;12:169–73.
Parashar M, Singh S, Kishore J, Patavegar BN. Breastfeeding attachment and positioning technique, practices and knowledge of related issues among mothers in colony of resettlement Delhi. ICAN. 2015;7:317–22.
National Center for Health Statistics. Health, United States, 2011: With Special Feature on Socioeconomic Status and Health. Hyattsville, MD. 2012.
Cadwell K, Turner-Maffei C, Blair A, Brimdyr K, Maja McInerney Z. Pain reduction and treatment of sore nipples in nursing mothers. J Perinat Educ. 2004;13:29–35.
Santos KJ, Santana GS, Vieira Tde O, Santos CA, Giugliani ERJ, Vieira GO. Prevalence and factors associated with cracked nipples in the first month postpartum. BMC Pregnancy Childbirth. 2016;16:209.
Henderson P. Infant and Young child feeding: model chapter for textbooks for medical students and allied health professionals. Session 1- the importance of infant and young child feeding and recommended practices. In: WHO Press 20 avenue Appia, 1211 Geneva 27. Switzerland: WHO Press, World Health Organization; 2009.
Joshi H, Magon P, Raina S. Effect of mother–infant pair’s latch-on position on child’s health: a lesson for nursing care. J Family Med Primary Care. 2016;5:309–13.
Abul-Fadl AM, Shawky M, El-Taweel A, Cadwell K, Turner-Maffe C. Evaluation of mothers’ knowledge, attitudes and practice towards the ten steps to successful breastfeeding in Egypt. Breastfeed Med. 2012;7:173–8.
Central Statistics Agency. Demographic and Health Survey. Addis Ababa: Central Statistics Agency; 2011. p. 162–73.
Kent JC, Ashton E, Hardwick CM, Rowan MK, Chia ES, Fairclough KA, et al. Nipple pain in breastfeeding mothers: incidence, causes and treatments. Int J Environ Res Public Health. 2015;12:12247–63.
Suresh S, Sharma KK, Saksena M, Thukral A, Agarwal R, Vatsa M. Predictors of breastfeeding problems in the first postnatal week and its effect on exclusive breastfeeding rate at six months: experience in a tertiary care center in northern India. Indian J Public Health. 2014;58:270–3.
Goyal RC, Banginwar AS, Ziyo F, Toweir AA. Breastfeeding practices: positioning, attachment (latch-on) and effective suckling – a hospital-based study in Libya. J Family Community Med. 2011;18:74–9.
Kronborg H, Væth M. How are effective breastfeeding technique and pacifier use related to breastfeeding problems and breastfeeding duration? Birth. 2009;36:34–42.
Dasgupta U, Mallik S, Bhattacharyya K, Sarkar J, Bhattacharya SK, Halder A. Breastfeeding practices: positioning, attachment and effective suckling—a hospital based study in West Bengal/Kolkata. Indian J Mater Child Health. 2013;15:1–11.
Mannan I, Rahman SM, Sania A, Seraji HR, Arifeen SE, Winch P, et al. Can early postpartum home visits by trained community health workers improve breastfeeding of newborns? J Perinatol. 2008;28:632–40.
Barwick M, Barac R, Zlotkin S. An examination of exclusive breastfeeding implementation in Ethiopia and Mali: factors influencing change. Ontario: CARE Canada; Save the Children Canada Plan International Canada; 2015.
Ethiopian Federal Ministry of Health, 2004. National Strategy for Infant and Young Child Feeding. National Strategy for Infant and Young Child Feeding.pdf. 2004. https://extranet.who.int/nutrition/gina/sites/default/files/ETH.
Harari Regional Health Bureau. Harari health bureau planning and programming service Office 2015. http://www.hararirhb.org/index.php
World Health Organization. Breastfeeding Counselling - A Training Course Trainer's Guide, Part One, Sessions 5- Observing A Breastfeed. Geneva, Switzerland: World Health Organization, Control of Diarrheal Disease Programme, UNICEF; WHO/ Diarrheal and Acute Respiratory Disease Control /93.4 UNICEF/93.2; 1993.
Prajapati AC, Chandwan H, Rana B, Sonaliya KN. A community based assessment study of positioning, attachment and suckling during breastfeeding among 0-6 months aged infants in rural area of Gandhinagar district, Gujarat, India. Int Jf Community Med Public Health. 2016;3:1921–6.
Stevens WG, Fellows DR, Vath SD, Stoker DA. An integrated approach to the repair of inverted nipples. Aesthet Surg J. 2004;24:211–5.
World Health Organization. Section 13: Mastitis Causes and Management. Geneva: Department of Child and Adolescent Health and Development; 2000.
El-Khedr SM, Lamadah SM. Knowledge, attitude and practices of Saudi women regarding breastfeeding at Makkah al Mukkaramah. J Biol Agriculture Health Care. 2014;4:56–65.
Nagendra K, Shetty PN, Rudrappa S, Jaganath S, Nair R. Evaluation of breastfeeding techniques among postnatal mothers and effectiveness of intervention: experience in a tertiary care center. Sri Lanka J Child Health. 2017;46:39–43.
Behera D, Anil Kumar K. Predictors of exclusive breastfeeding intention among rural pregnant women in India: a study using theory of planned behavior. Rural Remote Health. 2015;15:3405.
Lee HJ, Rubio MR, Elo IT, McCollum KF, Chung EK, Culhane JF. Factors associated with intention to breastfeed among low-income, inner-city pregnant women. Matern Child Health J. 2005;9:253–61.
Al-Akour NA, Khassawneh MY, Khader YS, Ababneh AA, Haddad AM. Factors affecting intention to breastfeed among Syrian and Jordanian mothers: a comparative cross-sectional study. Int Breastfeed J. 2010;5:6.
Rahim F, Muhammad J, Ali D, Amir S. Breastfeeding practices in neonatal units. J Med Sci. 2014;22:159–63.
SSF L. Breast pain in lactating mothers. Hong Kong Med J. 2016;22:341–6.
Gupta M, Aggarwal AK. Feasibility study of integrated management of newborn and childhood illness guidelines on effective breastfeeding in a rural area of north India. Indian J Community Med. 2008;33:201–3.
Thakre SB, Thakre SS, Ughade SM, Golawar S, Thakre AD, Kale P. The breastfeeding practices: the positioning and attachment initiative among the mothers of rural Nagpur. J Clin Diagn Res. 2012;6:1215–8.
De Amici D, Klersy C, Ramajoli F, Brustia L, Politi P. Impact of the Hawthorne effect in a longitudinal clinical study: the case of anesthesia. Control Clin Trials. 2000;21:103–14.
Acknowledgements
We are very grateful to the Haramaya University for their technical and financial support of this study. Next we would like to thank all data collectors and supervisor. Last but not least, thanks to all the mothers & infants who participated in the study without them this research would not have been realized.
Funding
The funding was obtained from Haramaya University College of Health and Medical Sciences. There was no code for the budget and it was released by simple signature of the correspondent author.
Availability of data and materials
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
GT designed the study, performed the statistical analysis and drafted the manuscript. FM, BG and KS participated in the study design, implementation of the study, and contributed to the draft manuscript. All authors contributed to the data analysis, read and approved the final manuscript.
Corresponding author
Ethics declarations
Authors’ information
GT (MSc. in maternity and Neonatal care in Nursing) - Lecturer at Haramaya university, College of Health and Medical Sciences, School of Nursing and Midwifery. FM (PhD. in public health) - Lecturer at Haramaya university, College of Health and Medical Sciences, School of Nursing and Midwifery. BG (PhD. in public health) - Lecturer at Haramaya University, College of Health and Medical Sciences, School of Nursing and Midwifery. KS (MSc. in clinical midwifery) - Lecturer at Haramaya University, College of Health and Medical Science, School of Nursing and Midwifery.
Ethics approval and consent to participate
Ethical clearance was obtained from Institute of Health Research Ethical Review Committee (IHRERC) of Haramaya University College of Health and Medical Sciences, School of Nursing and Midwifery, Ethiopia. Then formal letter of cooperation was written to Harari Regional Health Bureau and to each of selected governmental health institutions. Each study participant was adequately informed about the purpose, method, anticipated benefit and risk of the study. Written informed consent was obtained from study participants. Confidentiality and cultural norms of study participants were also maintained.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Tiruye, G., Mesfin, F., Geda, B. et al. Breastfeeding technique and associated factors among breastfeeding mothers in Harar city, Eastern Ethiopia. Int Breastfeed J 13, 5 (2018). https://doi.org/10.1186/s13006-018-0147-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13006-018-0147-z