Abstract
Background
Heterotopic pancreas most commonly occurs in the upper gastrointestinal tract of adults, usually as an incidental finding. It seldom occurs at the umbilicus, and even rarely in the pediatric age group.
Case presentation
Here we present a case of heterotopic pancreatic tissue in the omphalomesenteric duct remnant of a 9-month-old baby girl. She presented with redness at the base of the umbilicus associated with occasional mild wetness. A urachal fistula was suspected by ultrasound. Histology from subsequent resection revealed fibrous tissue with heterotopic pancreatic tissue and accompanying small bowel mucosa. The patient’s umbilical redness resolved after the surgery.
Conclusions
Upon literature search, we found only 17 other cases of heterotopic pancreas reported in the umbilicus. They described a high male to female ratio, frequent association with omphalomesenteric duct remnant and presentation of umbilical discharge. The Heinrich system is frequently used to classify heterotopic pancreas into 3 types, based on the presence of acini, islets and ducts. Several mechanisms have been proposed on the pathogenesis of heterotopic pancreas, including misplacement, metaplasia and totipotent cell theories. Heterotopic pancreas can manifest clinically with diseases of the pancreas, including malignant transformation, reported as high as 12.7% in a series. Awareness of this finding in the biopsy aids the suitable treatment decisions for the patient.
Similar content being viewed by others
Background
Umbilical discharge is a common pediatric problem. An underlying congenital anomaly should always be considered. Heterotopic pancreas is the second most common congenital anomaly of the pancreas, most commonly occurring in the upper gastrointestinal tract of adults. It seldom occurs at the umbilicus, and even rarely in the pediatric age group. Here we present a 9-month-old baby girl with heterotopic pancreatic tissue in the omphalomesenteric duct (OMD) remnant. Literature review of other 17 cases of heterotopic pancreas reported at the umbilicus has been performed [1,2,3,4,5,6,7,8,9,10,11,12].
Case presentation
Clinical presentation
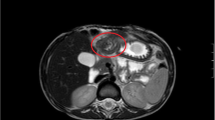
A 9-month-old baby girl presented with redness at the base of the umbilicus since her umbilical cord fell off, without accompanying discharge or smell. However, there was mild wetness in the umbilicus when she cried. The mother experienced an uneventful pregnancy and delivery. No congenital anomalies were discovered. There was no other medical history or family history of medical issues. Ultrasound revealed a tubular structure at the umbilicus with possible connection to the bladder (Fig. 1). It was clinically suspicious for a urachal fistula. The patient underwent surgery. Intraoperatively, a fibrous cord was traced from the umbilicus, but no obvious nodules were observed. There was no communication of the fibrous cord with the urinary bladder, bowel or any other intra-abdominal structure. This fibrous cord was therefore excised.
Gross and histological findings
Two separate pieces of unoriented tissue were received for histology, measuring 2 × 1 × 0.3 cm and 0.4 × 0.4 × 0.3 cm respectively. The larger piece revealed a possible sinus-like tract measuring 0.5 cm in length and 0.2 cm in diameter (Fig. 2). Haematoxylin and eosin sections showed fragments of dense fibrotic tissue with lobules of heterotopic pancreatic tissue comprising acinar elements, ducts and endocrine type cells (Figs. 3 and 4). The different components were demonstrated with immunohistochemical and special stains (Fig. 5). The smaller fragment also showed a covering small bowel mucosa with a deeply located tiny portion of pancreatic tissue close to the base of resection (Fig. 4a). No malignancy was identified.
Haematoxylin and Eosin (H&E) micrographs. The small bowel mucosa showed generally intact villous architecute, with Brunner’s glands observed in the laminia propria (black arrow). Smooth muscle bundles were haphazardly arranged in the underlying stroma, while no well-developed muscularis propria were seen (a, original magnification ×20). At the cauterized edge, there were lobules of pancreatic tissue, comprising benign acini and islets of Langerhans (b, ×100). A larger focus of pancreatic tissue was present in the fibrotic tissue (c, ×20). All three components were observed, including acini, islets of Langerhans (black arrow) and ducts (hollow arrow) (d, ×200). An intralobular nerve bundle was focally seen, adjacent to small ducts (inset, ×200)
Heterotopic pancreatic components. The haematoxylin and eosin micrograph showed exocrine and endocrine structures of pancreas (a, original magnification ×10). Ducts and pancreatic acini were highlighted by pan-cytokeratin marker AE1/3 immunostaining (b, ×10) and Periodic acid–Schiff–diastase special stain (c, ×10) respectively. The distribution of insulin-, glucagon-, and somatostatin-producing neuroendocrine cells scattered in the islets were demonstrated with respective immunohistochemistry (d to f, ×10)
Discussion
Umbilical discharge is common in children and usually due to infection. An underlying congenital anomaly should be investigated, such as umbilical hernia, urachal remnant and OMD remnant. OMD remnant, with a prevalence of only 2%, varies from patent OMD, to cysts, fibrous cords connecting the umbilicus to the distal ileum, granulation tissue at the umbilicus, umbilical hernias, and diverticulum of Meckel [13]. OMD remnant causes umbilical discharge generally through patency between the gut and umbilicus, rarely due to the presence of heterotopic pancreas.
First described in 1729 by Jean-Schultz, heterotopic or ectopic pancreas is defined as the presence of an abnormally located focus of normally developed pancreatic tissue outside the boundaries of the orthotopic pancreas, without anatomical or vascular connections. It is considered as the second most common congenital anomaly of the pancreas, after divisum. The prevalence has been reported to be 0.55 to 13.7% at autopsy and 0.2% at laparotomy [14]. It is most often discovered in fifth and sixth decades of life, and infrequently reported in the pediatric age group [11]. Seventy to 90% of heterotopic pancreas occurs in the upper gastrointestinal tract, while it can also be found anywhere [15]. It usually presents as an asymptomatic incidental finding, but it can cause symptoms as well depending on the size, location and pathological changes.
Umbilicus is an uncommonly reported location for heterotopic pancreas. Only 18 cases were found at the umbilicus, including ours (Table 1). The age ranges from newborn to 60 years old. Fifteen of them were below 2 years old, one adolescent, one young adult and only one elderly. Fourteen were male and 3 were female, one not indicated in the report. Most of them presented with umbilical discharge. Five were described to have coexisting small intestinal and/or gastric mucosa, which suggested the presence of heterotopic pancreas in the OMD remnant.
The Heinrich system is frequently used to classify heterotopic pancreas into 3 types. Type 1 contains acini, islets and ducts. Type 2 contains acini and ducts only, but no islets. Type 3 contains ducts alone [16]. In the described heterotopic pancreas at the umbilicus, type 1 was most commonly encountered.
Several mechanisms have been proposed for the pathogenesis of heterotopic pancreas, including the misplacement of embryonic tissue developing into pancreatic tissue, the metaplasia of endodermal tissue that migrates to the submucosa during embryogenesis into pancreatic tissue, and the differentiation of totipotent endodermal cells lining the gut or OMD into pancreatic tissue [12].
Heterotopic pancreas can manifest clinically with diseases of the pancreas, such as pancreatitis, pancreatic cyst, neuroendrocrine tumour and pancreatic carcinoma [17]. The incidence of malignant transformation is reported as high as 12.7% in a Japanese series [18]. Therefore, follow up is suggested if incompletely excised, although heterotopic pancreas itself is a benign condition. In this case, heterotopic pancreatic tissue was present at the cauterized edge of the specimen, which raised the possibility of residual pancreatic tissue left behind. Till now, on the follow-up of the patient, her umbilical redness resolved. Limited local excision appeared to be a safe and adequate procedure in the current setting.
Conclusions
In conclusion, heterotopic pancreas at the umbilicus is an uncommon condition, predominantly occurring in infants despite a wide range of ages. It demonstrates a high male to female ratio, frequent association with omphalomesenteric duct remnant and presentation of umbilical discharge. Radiology may not be helpful. Diagnosis is usually straight forward on the histologic evaluation of resection specimen, complemented with immunohistochemistry. Awareness of this finding in biopsy aids in the suitable treatment decisions for the patient.
Abbreviations
- OMD:
-
omphalomesenteric duct
References
Harris LE, Wenzl JE. Heterotopic pancreatic tissue and intestinal mucosa in the umbilical cord: report of a case. N Engl J Med. 1963;268:721–2.
Caberwal D, Kogan SJ, Levitt SB. Ectopic pancreas presenting as an umbilical mass. J Pediatr Surg. 1977;12(4):593–9.
Kondoh S, Taniki T, Umemoto A, Kajikawa A, Sogame M, Tanaka K, et al. A case of umbilical polyp with aberrant pancreas and small intestinal mucosa--analysis of cases of umbilical polyp reported in Japan. Nihon Geka Gakkai Zasshi. 1994;95(10):786–9.
Avolio L, Cerritello A, Verga L. Heterotopic pancreatic tissue at umbilicus. Eur J Pediatr Surg. 1998;8(6):373–5.
Pérez-Martínez A, Gonzálvez-Piñera J, Marco-Macián A. Iñiguez de Ozoño L, Goñi-Orayen C, Moya-Marchante M. Wet umbilicus caused by pancreatic heterotopia in urachal remains. Pediatr Surg Int. 1999;15(2):143–4.
Tan HL, Yoong A, Yu CC. Ectopic pancreatic rests: a rare cause of persistent umbilical discharge. Pediatr Surg Int. 2000;16(1–2):116–7.
Tillig B, Gerein V, Coerdt W, Vahdad R, Engert J. Large supraumbilical pseudocystic tumour due to ectopic pancreatic tissue located in a rest of the omphaloenteric duct. Eur J Pediatr Surg. 2004;14(2):126–9.
Lee WT, Tseng HI, Lin JY, Tsai KB, Lu CC. Ectopic pancreatic tissue presenting as an umbilcal mass in a newborn: a case report. Kaohsiung J Med Sci. 2005;21(2):84–7.
de Silva WD, Samarasinghe MC, Dias MN, Perera CS. Ectopic gastric and pancreatic tissue: a rare cause of umbilical discharge. Ann Trop Paediatr. 2010;30(1):73–5.
Abdelgabar A, Wojciechowski M, Van de Vijver E, Ruppert M, Hubens G, Balliu L, et al. Ectopic pancreatic tissue at the umbilicus in childhood: a case report and review of the literature. Acta Chir Belg. 2013;113(6):452–4.
Sharma S, Maheshwari U, Bansal N. Ectopic pancreatic, gastric, and small intestine tissue in anumbilical polyp, causing persistent umbilical discharge in a 2 year old child – a rare case report. J Evol Med Dent Sci. 2013;2:447–51.
Park E, Kim H, Jung KW, Chung JH. Heterotopic pancreas in omphalomesenteric duct remnant results in persistent umbilical discharge. Korean J Pathol. 2014;48(4):323–6.
Moore TC. Omphalomesenteric duct malformations. Semin Pediatr Surg. 1996;5(2):116–23.
Song DE, Kwon Y, Kim KR, Oh ST, Kim JS. Adenocarcinoma arising in gastric heterotopic pancreas: a case report. J Korean Med Sci. 2004;19(1):145–8.
Bromberg SH, Camilo Neto C, Borges AF, Franco MI, França LC, Yamaguchi N. Pancreatic heterotopias: clinicopathological analysis of 18 patients. Rev Col Bras Cir. 2010;37(6):413–9.
Heinrich H. Ein Beitrag zur Histologie dessogen. Akzessorischen Pankreas Virchows Arch. 1909;198:392–401.
Rimal D, Thapa SR, Munasinghe N, Chitre VV. Symptomatic gastric heterotopic pancreas: clinical presentation and review of the literature. Int J Surg. 2008;6(6):e52–4.
Nakaoa T, Yanoh K, Itoh A. Aberrant pancreas in Japan. Review of the literature and report of 12 surgical cases. Med J Osaka Univ. 1980;30(3–4):57–63.
Acknowledgements
Not applicable.
Funding
Not applicable.
Availability of data and materials
Not applicable.
Author information
Authors and Affiliations
Contributions
ZZ collected clinical and pathological information of the case, and was a major contributor in writing the manuscript. KS provided clinical information. SM was the reporting pathologist of the case, conceived the study, critically reviewed the manuscript draft and is corresponding author. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent for publication of their clinical details was obtained from the parent of the patient. A copy of the consent form is available for review by the Editor of this journal.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Zhao, Z., Sim, C.K. & Mantoo, S. Heterotopic pancreas in the omphalomesenteric duct remnant in a 9-month-old girl: a case report and literature review. Diagn Pathol 12, 49 (2017). https://doi.org/10.1186/s13000-017-0643-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13000-017-0643-2