Abstract
Background
HIV-associated neurocognitive disorder (HAND) remains common, despite antiretroviral therapy (ART). HIV dysregulates iron metabolism, but cerebrospinal fluid (CSF) levels of iron and iron-transport proteins in HIV-infected (HIV+) persons are largely unknown. The objectives of this study were to characterize CSF iron-related biomarkers in HIV+ adults and explore their relationships to known predictors of HAND.
Methods
We quantified total iron, transferrin and heavy-chain (H)-ferritin by immunoassay in CSF sampled by lumbar puncture in 403 HIV+ participants in a multi-center, observational study and evaluated biomarker associations with demographic and HIV-related correlates of HAND [e.g., age, sex, self-reported race/ethnicity, ART, and detectable plasma virus and CSF viral load (VL)] by multivariable regression. In a subset (N = 110) with existing CSF: serum albumin (QAlb) measurements, QAlb and comorbidity severity were also included as covariates to account for variability in the blood–CSF-barrier.
Results
Among 403 individuals (median age 43 years, 19% women, 56% non-Whites, median nadir CD4+ T cell count 180 cells/µL, 46% with undetectable plasma virus), men had 25% higher CSF transferrin (median 18.1 vs. 14.5 µg/mL), and 71% higher H-ferritin (median 2.9 vs. 1.7 ng/mL) than women (both p-values ≤0.01). CSF iron was 41% higher in self-reported Hispanics and 27% higher in (non-Hispanic) Whites than in (non-Hispanic) Blacks (median 5.2 and 4.7 µg/dL in Hispanics and Whites, respectively, vs. 3.7 µg/dL in Blacks, both p ≤ 0.01); these findings persisted after adjustment for age, sex, and HIV-specific factors. Median H-ferritin was 25% higher (p < 0.05), and transferrin 14% higher (p = 0.06), in Whites than Blacks. Transferrin and H-ferritin were 33 and 50% higher, respectively, in older (age > 50 years) than in younger persons (age ≤ 35 years; both p < 0.01), but these findings lost statistical significance in subset analyses that adjusted for QAlb and comorbidity. After these additional adjustments, associations were observed for CSF iron and transferrin with race/ethnicity as well as CSF VL, for transferrin with sex and ART, and for H-ferritin with plasma virus detectability and significant comorbidity (all p < 0.05).
Conclusions
CSF iron biomarkers are associated with demographic factors, ART, and CSF VL in HIV+ adults. Future studies should investigate a role for CNS iron dysregulation, to which an altered blood-CSF barrier may contribute, in HAND.
Similar content being viewed by others
Background
HIV affects an estimated 40 million people worldwide [1], and owing to the success of combination antiretroviral therapy (ART) in suppressing viral replication, this population is aging [2–4]. An increasing number of chronic disease complications, such as HIV-associated neurocognitive disorders (HAND), are therefore the focus of current efforts to improve quality of life for HIV-infected (HIV+) individuals. HAND remains disturbingly common despite ART, for reasons that are only partially understood, occurring in 30–60% of unselected HIV+ persons, even when the virus is undetectable [5, 6]. Intensive research has suggested many possible mechanisms and etiologies for HAND, including persistent low-level immune activation and inflammation within the central nervous system (CNS) [4, 7, 8], comorbid conditions [9], and accelerated aging [10], but few of these mechanisms are directly actionable, and effective interventions remain elusive. Risk factors for HAND include the nadir CD4+ T-cell count, indicating the depth of immunosuppression achieved during the course of HIV disease, older age at seroconversion, anemia, delay in initiating ART, and the presence of HIV RNA in the CSF and plasma, as well as comorbidity [11–14]. Anemia is prevalent in HIV infection, even when the virus is undetectable during successful ART, and it has been consistently associated with increased morbidity and mortality in HIV infection in retrospective and prospective studies [15]. In addition, the possibility that CNS toxicity due to ART contributes to HAND remains a matter of debate; certain antiretroviral drugs such as zidovudine (ZDV) have well-described effects on iron transport and frequently cause anemia, and others may exhibit neurotoxicity [14, 16, 17]. Female sex appears also to be associated with higher susceptibility to HAND, but women have been underrepresented in prior HIV studies, and factors unrelated to HIV infection may also explain this finding [18–20]. Finally, HIV+ persons of Hispanic ethnicity experience an increased risk of neurocognitive decline, possibly due in part to reduced or delayed access to health care [13, 18, 21–23].
Iron homeostasis is essential for normal brain function: iron is required for the synthesis of monoamine neurotransmitters, for mitochondrial function, myelin synthesis, and the catalytic function of a large number of metabolic enzymes [4, 24]. Alterations in brain iron content and distribution (e.g., excess iron deposition) have long been associated with complex neurodegenerative disorders such as Parkinson’s disease, Alzheimer’s disease, and amyotrophic lateral sclerosis (ALS) [25]. Neurocognitive impairment has also been reported in the restless leg syndrome (RLS), in which brain iron deficiency contributes to dopaminergic dysfunction within the brain [26]. It has been challenging to determine the extent to which iron plays a pathogenic as opposed to a bystander role in these conditions, but evidence is accumulating in favor of the former [27–30]. An extensive literature has established that peripheral iron deficiency also leads to reduced cognitive performance and behavioral disturbances, which in children and adolescents may be long-lasting and not fully reversible upon iron repletion [31–33]. Despite the known importance of iron to brain health, iron and iron transport proteins in the CSF have been measured only anecdotally in small numbers of HIV-negative persons with specific neurodegenerative conditions, or in healthy controls [34–38]. CNS iron homeostasis has not been adequately investigated in HIV+ individuals with or without HAND, either by measurement of iron or iron-related biomarkers in CSF, or indirectly, by iron-sensitive neuroimaging [4, 39, 40].
Transferrin, the chief iron-transporter in the circulation, binds and transports ferric iron in a soluble, nonreactive state to metabolically active cells throughout the body, whereupon transferrin-bound iron is internalized by receptor-mediated endocytosis [41]. Transferrin is synthesized and secreted by the choroid plexus and is also produced by oligodendrocytes; it is the chief mode of delivery of iron to neurons [42]. Ferritin, the principal intracellular iron-storage molecule in tissues, is frequently elevated in HIV+ persons, possibly reflecting a prolonged acute-phase inflammatory response [43, 44]. Ferritin comprises varying proportions of heavy (iron-avid) and light (relatively iron-poor) chains (H- and L-ferritin, respectively), depending on the tissue of origin. H-ferritin is the predominant form in the CNS, and it delivers iron to oligodendrocytes via the Tim-2 receptor [45, 46]. Iron delivery by H-ferritin to other cell types has also been suggested [47]. Serum ferritin levels generally rise, and transferrin levels fall, with increasing systemic iron stores; the reverse changes occur in functionally iron-deficient states [41, 43]. Both transferrin and H-ferritin can be influenced by inflammatory stimuli, such as infection or comorbid conditions [48, 49]. The synthesis, transport, and regulation of iron, transferrin, and ferritin within the CNS are incompletely understood and the subject of ongoing investigation [24] In contrast to many other serum proteins, levels of these iron-related proteins in CSF have often been reported not to correlate with those in the peripheral circulation, and the brain is well buffered against systemic iron deficiency or excess [50]. Although a number of studies have examined peripheral (serum or plasma) iron biomarkers in HIV infection as a factor in disease outcomes [51–54], CSF levels of iron, transferrin, and H-ferritin remain inadequately characterized from an epidemiological perspective [55, 56].
Serum is the most convenient source for routine, noninvasive testing of iron parameters, but the CSF is more likely to provide an accurate reflection of iron transport in the CNS. There is also considerable precedent for the use of CSF biomarkers as surrogate markers of iron metabolism and/or neuronal injury in the brain [57–59]. Recent studies have documented selective prioritization and partitioning of iron across different tissues in the anemic state, for example, and thus, blood indices may not reflect CNS iron depletion [60, 61]. Another advantage of CSF as the biological medium for estimating CNS iron status is that CSF is sequestered behind both the blood–brain barrier (BBB) and blood–CSF barrier. This isolation from the periphery permits measurement of iron and iron-management proteins at least in part derived from or in equilibrium with the brain parenchyma and specific to the CNS, potentially reflecting unique aspects of iron transport within that compartment.
It is of interest to evaluate associations of known predictors of neurocognitive decline in HIV infection with levels of CSF iron and iron-transport proteins, because such associations would suggest a possible novel role for dysregulation of iron metabolism or iron transport pathways in the pathogenesis of HAND that might be targeted therapeutically. Analogous approaches have proven instructive in achieving a better understanding of other chronic disease phenotypes linked to inflammation, such as cancer [62]. The purpose of this study was therefore to quantify, for the first time, iron and biomarkers of iron transport in the CSF of HIV+ persons and systematically evaluate their relationships to host factors such as age, sex, ethnicity or ancestry, and key HIV disease-related factors like ART (including ZDV use) and the presence and quantity of CSF virus.
Methods
Patient selection and CSF sampling
The CNS HIV Antiretroviral Therapy Effects Research (CHARTER) Study is an observational, prospective cohort study that enrolled ambulatory, HIV+ adults at six large U.S. Medical Centers in the U.S., including Johns Hopkins University School of Medicine (Baltimore, MD, USA), the University of California (San Diego, CA, USA), University of Texas Medical Branch (Galveston, TX, USA), Washington University School of Medicine (Saint Louis, MO, USA), University of Washington (Seattle, WA, USA), and the Icahn School of Medicine of Mount Sinai (New York, NY, USA). CHARTER was designed specifically to evaluate neurological outcomes in HIV+ individuals; hence, all participants underwent detailed neuromedical, neuropsychological, and cognitive evaluations at baseline and 6-month follow-up visits, as previously described [7]. Comorbid conditions were categorized upon careful assessment as minimal, mild or moderate, or severe by expert clinicians [6, 63].
Participants in this study of CSF iron biomarkers were selected based on availability of at least 1.0 mL of CSF at both baseline (N = 403) and 6-month (N = 100) follow-up visits. Individuals with comorbid conditions deemed by expert clinicians to be severe (conditions such as traumatic brain injury with prolonged loss of consciousness, recent stroke, or a history of developmental delay) were excluded, and the remainder were classified as having minimal or mild-moderate comorbidity following extensive chart review [6]. Basic demographic information (e.g., age, sex, self-reported race/ethnicity) and HIV disease characteristics [e.g., ART, nadir CD4+ T-cell count, and HIV RNA concentrations (viral load, VL) in plasma and CSF] were determined at the baseline visit during structured in-person interviews, when CSF was first sampled, as described in detail previously [13]. Non-Hispanic Whites of European ancestry are henceforth referred to as “Whites” and non-Hispanic Blacks, as “Blacks”, to distinguish them from self-reported Hispanic individuals. Nine study participants reported their race/ethnicity as “Other” and were too few in number for subgroup analyses; therefore, race-stratified analyses included only self-reported Black, White, and Hispanic study participants.
All CHARTER study participants provided written informed consent for the study, and the CHARTER study adheres to the ethical principles set forth in the Declaration of Helsinki. The present study was also approved by the institutional review boards of all participating institutions.
CSF iron quantification
Iron content within the CSF was evaluated using the Quantichrom iron assay (BioAssay Systems, Hayward, CA, USA) and the manufacturer’s protocol. Briefly, 50 μL of standards or patient CSF samples were mixed with 200 μL Quantichrom Working Reagent in a 96-well plate (in duplicate) and incubated at room temperature for 40 min. The iron concentration in experimental samples was determined by comparison of the optical density at 590 nm with the standard curve.
CSF transferrin quantification
Transferrin content within sampled CSF was determined by enzyme-linked immunosorbent assay (Human Transferrin ELISA kit (ab108902) (Abcam, Cambridge, MA, USA) performed according to the manufacturer’s protocol. After the CSF was collected and centrifuged, the samples (in duplicate) were diluted 1:1000 with mix diluent. Briefly, transferrin standard or diluted CSF sample (50 μL) was added to each well and the solution was incubated for 2 h. Following incubation, the plate was washed five times with 200 μL of 1× Wash Buffer. Following the wash step, 1× Biotinylated transferrin antibody (50 μL) was added to each well and the solution was incubated for 1 h. The plate was washed again as described above. 1× SP Conjugate (50 μL) was added to each well and the solution was incubated for 30 min. The microplate was washed again as described above. Chromogen substrate (50 μL) was added to each well and the solution was incubated for 12 min. Stop solution (50 μL) was added to each well and the absorbance was read immediately on a microplate reader at 450 nm. Transferrin concentration was then determined by comparison to the standard curve.
CSF H-ferritin quantification
The H-ferritin content of CSF was determined by an enzyme-linked immunosorbent assay (Human H-ferritin ELISA kit, Abnova, Taipei, Taiwan) performed according to the supplier’s instructions. Briefly, 20 µL of standards, subject samples (in duplicate), and controls were combined with 100 µL of enzyme conjugate reagent. The solution was mixed for 30 s and incubated at room temperature for 45 min. The incubation mixture was removed and the plate was rinsed five times with distilled water. The TMB Reagent (100 µL) was added into each well, the solution was mixed for 10 s, and the solution was incubated at room temperature in the dark for 20 min. Stop Solution (100 µL) was added to each well and the solution was mixed for 30 s. The ferritin concentration in the experimental samples was determined by comparison of the optical density at 450 nm with the standard curve within 15 min.
Serum iron biomarker measurement
Iron, ferritin, and transferrin were also quantified in serum using routine, commercially available, automated assays in a subset of study participants (N = 11) who had sufficient serum available at the 6-month follow-up visit. Circulating ferritin, which consists primarily of the L subunit, was quantified by electrochemiluminescence assay (“ECLIA”), using a biotinylated, monoclonal ferritin-specific antibody and a ruthenium-labeled monoclonal ferritin antibody to form a sandwich complex. Upon addition of streptavidin-coated microparticles, chemiluminescence emission was measured by a photomultiplier (Roche e411 immunoassay analyzer, Roche Diagnostics, Indianapolis, IN, USA) and ferritin concentration determined from a standard curve. Serum iron and transferrin were measured on a Roche c311 automated chemistry analyzer (Roche Diagnostics, Indianapolis, IN, USA), iron by a colorimetric method based on the FerroZine reaction (without deproteinization), which captures unbound and transferrin-bound iron, and transferrin by immunoturbidimetry [64].
Functional integrity of the blood–CSF barrier
As a measure of the integrity of the blood–CSF barrier, CSF and matched serum levels of albumin were quantified by the nephelometric method (Dade Behring BNII, Deerfield, IL, USA) in CHARTER study subjects, 110 of whom participated in this study, and the ratio of CSF to serum albumin (CSF: serum albumin ratio, or QAlb) was calculated as QAlb = albumin(CSF)/albumin(serum) [65]. Individuals with matched CSF and serum albumin measurements from multiple visits were assigned a mean value for QAlb.
Statistical analyses
The Wilcoxon rank sum test was used to determine univariate differences in CSF iron, H-ferritin, and transferrin levels among HIV-infected individuals by demographic and clinical characteristics or factors. Spearman’s rho values were determined for correlation between CSF iron biomarkers at baseline or at 6-months, and between CSF and corresponding serum biomarker levels at the 6-month visit in the subset with matched measurements. Unadjusted and adjusted analyses of association were performed after taking the natural logarithm of biomarker values to enforce normality, in order to fulfill the assumptions of linear regression.
Associations of each CSF biomarker with age, sex, and race/ethnicity (dichotomized as Blacks compared with Whites, Whites compared with Hispanics, or Blacks compared with Hispanics), and clinical HIV disease characteristics were individually evaluated in multivariable regression models. Clinical disease factors that were evaluated included: VL in plasma and CSF and presence or absence of detectable plasma or CSF virus, estimated duration of HIV infection (months), ART (on vs. off therapy at the time of blood sampling), current ZDV use (yes/no), nadir CD4+ T-cell count, AIDS status (yes/no), hemoglobin level, anemia status (yes/no), current alcohol use (yes/no), and comorbidity (minimal vs. mild-to-moderate). Hemoglobin, anemia status, and alcohol use showed no relationship to CSF iron biomarkers in univariate analyses and were therefore not included in models to optimize power. Regression models for iron, transferrin, and H-ferritin are presented with partial or full covariate adjustment. For CSF iron, models included the following covariates: (1) age, sex, and race/ethnicity (partial adjustment), or all of the covariates listed in (1) as well as ART (on vs. off), current ZDV use (yes vs. no), plasma VL detectability (yes vs. no), and CSF VL (full adjustment). Covariates in partially adjusted models of transferrin and H-ferritin included age, sex, race/ethnicity, and ZDV use; ART, plasma VL detectability and CSF VL were added to fully adjusted models. Beta-coefficients and their 95% Confidence Intervals were estimated for associations, and two-sided p-values were determined. Following analyses in the entire study sample of 403 individuals, similar analyses with additional adjustment for mean QAlb were performed in the 110 individuals who had this data. All analyses were performed using STATA statistical software v10.0.
Results
CSF iron-related biomarkers in CHARTER study participants
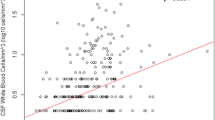
Characteristics of the CHARTER study population at baseline are summarized in Table 1. Median CSF iron levels in this sample were 3.1 µg/dL (interquartile range or IQR 1.6–5.7 µg/dL); median transferrin levels were 17.2 µg/mL (IQR 10.3–27.6 µg/mL), and median H-ferritin levels were 2.7 ng/mL (IQR 1.4–4.2). In order to characterize demographic differences in CSF iron-related biomarkers in HIV+ persons, we measured CSF iron, transferrin, and H-ferritin in 403 cryopreserved CSF samples from CHARTER study participants collected at baseline and in 100 of the same persons at 6 months of follow-up. Within individuals, CSF iron, transferrin and ferritin levels measured at the baseline visit were correlated with levels of the same biomarkers measured at the 6-month visit (all p < 0.01, see Additional file 1: Figure S1 and Additional file 2: Table S1). Correlations between different iron-related biomarkers at baseline, and the same correlations at 6 months are shown in Fig. 1. CSF iron levels were weakly correlated with CSF transferrin and H-ferritin levels at baseline and 6 months (Spearman’s rho = 0.12 and 0.24 at baseline, and rho = 0.28 and 0.24 at 6 months, respectively, all p-values <0.05). Transferrin levels in CSF were modestly correlated with H-ferritin levels at baseline (rho = 0.37, p < 0.05), but not at 6 months. Age, sex, and ZDV use did not differ between study participants sampled at baseline and 6-months. As shown in Table 2 and Fig. 2, CSF transferrin and H-ferritin levels differed significantly between men and women in the study in univariate analyses (median transferrin levels in men at the baseline visit were 18.1 vs. 14.5 µg/mL, p < 0.05; median H-ferritin levels were 2.9 vs. 1.7 ng/mL, p = 1.4 × 10−5). Significant sex differences in CSF iron content were not observed.
In order to better explore age-related differences in CSF iron measures, we evaluated CSF iron, transferrin, and H-ferritin levels in non-contiguous age groups of younger (≤35 years) and older HIV+ adults (>50 years of age) from the CHARTER Study. As shown in Table 3 and Fig. 3, 134 study participants were included in this comparison, which was not adjusted for other HIV-related or demographic factors. CSF transferrin and H-ferritin levels were significantly higher in older than in younger individuals in this study population (both p-values <0.01), but CSF total iron content did not differ significantly between these groups.
Since there is evidence of genetic differences among population subgroups with regard to iron metabolism [66], we also compared levels of CSF iron, transferrin, and H-ferritin between self-reported HIV+ White, Black, and Hispanic study participants and were able to discern ancestry-related differences. As shown in Table 4 and Fig. 4, differences in CSF transferrin levels did not attain statistical significance between any of these subgroups in unadjusted analyses, although self-identified Whites tended to have higher CSF transferrin levels than Blacks (p = 0.057). CSF H-ferritin levels were significantly lower in Blacks than in Whites (p < 0.05) in this HIV+ sample, however, and total iron CSF iron levels were also significantly lower in Blacks compared to either Whites or Hispanics (p = 0.002 and p = 0.013, respectively).
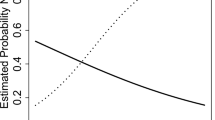
In unadjusted analyses (data not shown), CSF iron was not associated with any HIV disease-related variables, but CSF transferrin was associated with CSF VL and current ZDV use (both p-values <0.05) and tended to be higher in Whites than in Blacks (p = 0.05); CSF H-ferritin levels showed a borderline association with plasma VL detectability (p = 0.06) and current ZDV use (p = 0.05). In order to estimate the degree of association between CSF iron biomarkers and demographic or HIV-related factors while accounting for possible confounding by these factors, some of which promote inflammation, multivariable-adjusted linear regression analyses were conducted, using natural-log-transformed biomarker values to enforce normality. These results are shown in Table 5. CSF iron levels remained significantly associated with self-reported ancestry: iron levels were higher in Whites and Hispanics than in Blacks. CSF iron levels were not significantly related to plasma or CSF VL or virus detectability, current use of ART or ZDV, age, or sex in adjusted models. CSF transferrin associations with age (positive) and sex (lower levels in women, β = −0.225 [95% CI −0.445 to 0.006], p < 0.05) persisted following adjustment, but the association with ancestry lost significance. With regard to HIV-related factors, CSF transferrin levels remained negatively associated with ZDV use (β = −0.254 [95% CI −0.467, −0.040], p = 0.03) and increased with CSF VL (β = 0.297 [95% CI 0.145, 0.450], p < 0.01). H-ferritin levels in the CSF also remained positively associated with age and negatively associated with female sex after multivariable adjustment. Study participants with detectable plasma virus had lower CSF ferritin levels (β = −0.242 [95% CI −0.449, −0.035], p = 0.02), and those who were currently on ZDV also tended to have lower levels (β = −0.196 [95% CI −0.413, 0.021], p = 0.07); the association of transferrin with plasma VL detectability, though in the same direction, was non-significant. Higher H-ferritin levels were associated with increasing CSF VL (β = 0.142 [95% CI −0.002, 0.286], p = 0.05). Neither CSF transferrin nor H-ferritin was significantly related to race/ethnicity in multivariable-adjusted analyses. Estimates of association with age, sex, and ancestry did not appreciably change for any biomarker with full adjustment, including HIV disease factors.
In the subset of individuals in this study who had available QAlb data (N = 110), similar multivariable regression analyses were performed. In these models, QAlb as well as comorbidity were included as additional covariates to adjust for likely changes in the functional integrity of the blood-CSF barrier that occur with age as well as HIV infection, and for comorbidity-related inflammation, which can influence iron biomarkers [14]. These models are summarized in Table 6. Higher CSF iron was again significantly associated with race/ethnicity (β = 0.732, p = 0.02; higher iron in Hispanics and Whites than in Blacks), as well as with plasma virus detectability (β = 0.611, p = 0.05) but lower CSF VL (β = −0.511, p = 0.03). Higher transferrin levels were associated with male sex (β = −0.389, p = 0.03), non-White race/ethnicity (β = −0.100, p = 0.057, and being on ART (β = 0.801, p = 0.03), but not with comorbidity; the associations with age and ZDV use lost significance. Finally, levels of H-ferritin in CSF were significantly higher among subjects with clinically mild-to-moderate comorbidity (β = 0.416, p = 0.03) and when plasma virus was undetectable (β = −0.407, p = 0.03); CSF VL, age, and gender were no longer significant factors, though the direction of the point estimate for age remained the same. Associations for all iron biomarkers with blood–CSF barrier integrity (mean QAlb) were statistically significant with the exception of H-ferritin (p-value = 0.07). None of the CSF iron biomarkers was associated with nadir CD4+ T-cell count, hemoglobin level, or anemia (data not shown).
Iron and biomarkers of iron transport were quantified in serum in 11 individuals with available serum as well as measured CSF biomarkers at 6 months, and we evaluated correlations of iron, ferritin and transferrin levels in serum to levels of the same analytes in CSF (Additional file 3: Table S2); the methods of quantification were the same. No significant correlations were observed between levels of any of these biomarkers in CSF and their corresponding serum values.
Discussion
This represents the first large study to systematically quantify levels of iron and the two major iron-transport proteins, transferrin and (H)-ferritin, in the CSF of HIV+ persons and to evaluate their associations with known predictors of neurocognitive impairment in this population. Due to the invasive nature of lumbar puncture, published data for CSF iron biomarkers have been scarce even in HIV-negative individuals, in whom data are available only in small numbers of individuals with specific disorders and at different stages of neurodegenerative disease [36, 37, 67–69]. Hence, normal variations of these biomarkers in healthy persons are also not well documented in the literature [38, 67, 70]. Our findings in over 400 clinically well-characterized HIV+ individuals demonstrate that CSF iron and transferrin are independently associated with demographic factors (race/ethnicity and/or sex) and HIV-disease-specific factors (plasma virus detectability, ART, and/or CSF VL), while CSF H-ferritin is related to comorbidity and virus detectability in plasma. Interestingly, observed differences in CSF iron by self-reported race/ethnicity parallel known differences in the risk of neurocognitive decline in HIV+ adults, with the highest levels occurring in persons of Hispanic ethnicity who also appear to be at increased risk of HAND [13]. This study provides the only available estimates of the range and degree of variability of iron biomarkers in HIV + CSF currently available, and the observed relationships to known risk factors for HAND are hypothesis-generating with regard to the potential role of iron dyshomeostasis in HIV-associated neurocognitive decline.
Both nonhuman primate and human studies have shown that systemic iron deficiency and anemia have lasting impact on brain iron homeostasis and neuronal health, influencing memory and cognition [32, 60, 71–73]. In Alzheimer’s disease and ALS, both peripheral and CSF iron biomarker profiles suggest disruption of iron homeostasis with concomitant inflammation within the brain [28, 30, 34, 35]. The situation in HIV infection may be similar, with neuroinflammation due to HIV-activated macrophage–monocytes migrating across a damaged BBB triggering a reduction in iron bioavailability in the CNS that may promote neurocognitive decline. Accumulating evidence for systemic changes in iron transport by HIV [54, 74, 75], mediated at least in part by the iron-regulatory hormone hepcidin, and appearance of the virus in the CNS within days of acute infection, suggest that HIV-mediated iron dysregulation may also occur in the CNS. HIV does not infect neurons, but the virus has been shown to infect perivascular macrophages, microglia, and other supporting cells within the CNS, some of which play central roles in regulating brain iron content and distribution [4, 24, 50]. HIV infection of macrophages has also been shown to downregulate expression of the MHC-class I-like iron-regulatory protein Hfe on the macrophage cell surface via the actions of viral proteins, thereby increasing macrophage iron content to benefit viral replication [76].
In the present study, higher CSF iron content tended to be associated with detectable virus in the plasma but with lower CSF VL, when adjusting for the QAlb, a measure reflecting variability in integrity of the blood–CSF barrier. This apparent discordance suggests that either (1) more iron fails to cross the CSF–brain barrier when HIV levels in the brain or CSF are low, leading to higher levels in the CSF, or (2) higher amounts of virus in the brain or CSF are associated with greater extraction of iron from the CSF, because HIV requires iron for its replication [77]. The significantly lower CSF transferrin levels among persons of Hispanic ethnicity and non-Hispanic Whites compared to Blacks after adjustment for QAlb were also in accord with the corresponding observed CSF iron differences. Even when accounting for the effects of ZDV, an antiretroviral drug that can affect iron transport, ART was independently associated with higher CSF transferrin, raising the possibility that other commonly used antiretroviral drugs may impact transferrin levels in the CNS, possibly by inducing a functionally iron-deficient state. Initiation of ART has been temporally linked to an increase in soluble transferrin receptors, a sensitive indicator of tissue iron deficiency [78, 79]. Other mechanisms by which functional iron deficiency might be induced in the CNS during HIV infection are the depletion of cellular iron due to active viral replication and/or chronic inflammation in the brain that results in iron entrapment within supporting cells that normally deliver iron, or iron deficiency of these cells themselves [24, 76, 80]. Indeed, higher CSF VL was associated in our analyses with higher CSF transferrin levels, with and without QAlb adjustment. Interestingly, HIV+ individuals are at increased risk of RLS, a condition associated with iron deficiency in the brain [81, 82].
Although men are known to have significantly higher systemic iron stores than pre-menopausal women, differences in CSF levels of iron, transferrin, or H-ferritin levels have not been documented, and they may have clinical relevance [83]. Women were observed to have significantly lower levels of both transferrin and H-ferritin before QAlb adjustment; this association persisted following adjustment only for transferrin, and the direction of the estimate remained the same for H-ferritin although significance was lost. That higher H-ferritin levels were associated with undetectable plasma virus but a higher quantity of CSF virus suggests that induction of H-ferritin in the CNS may be a physiological (cytoprotective) response to viral compartmentalization and replication in the CNS. HIV-induced oxidative stress is manifested by upregulation of heme-oxygenase-1 in the brain [84], and the ferroxidase activity of H-ferritin has recently been shown to mediate the antioxidant activity of heme oxygenase-1 [85]. Due to its high metabolic demands, the brain also requires a steady supply of iron in non-reactive form, for energy production as well as myelin and neurotransmitter synthesis [61, 86–88]. Todorich et al. [46] previously identified H-ferritin as an important source of iron for oligodendrocytes, and although the origin of CSF iron, H-ferritin, and transferrin cannot be established in this type of study, it is possible that both proteins are upregulated in persons with suppressed viremia in an attempt to preserve iron delivery to oligodendrocytes, other supporting cells of the CNS, and neurons. Indeed, HIV infection is associated with decreased amounts of myelin or loss of myelin integrity [89–91]. One neuroimaging study that used modern, iron-sensitive techniques reported possible decreases in brain iron in HIV-infected individuals [40], and studies using diffusion tensor imaging or other modalities have consistently revealed white matter damage [40, 83]. It is not surprising that CSF H-ferritin levels were also associated with more clinically significant comorbidity, as comorbidity has emerged as a powerful predictor of neurocognitive decline and is a common correlate of chronic inflammation in HIV+ persons [92]. Mechanisms other than inflammation may also explain increases in H-ferritin in CSF, including HIV-induced changes in autophagy or even ferritinophagy [93, 94]. Finally, associations with age, a strong risk factor for HAND, with both CSF transferrin and H-ferritin were pronounced before adjusting for QAlb but lost significance after this adjustment; this begs the question whether the loss of iron regulation (or the loss of compartmentalization of iron) in the CSF due to age- or HIV-related damage to the blood–CSF barrier may in part mediate age-related neurocognitive decline.
Levels of CSF iron biomarkers in this HIV+ population were not dramatically different from levels previously reported in small numbers of healthy individuals, but the different assay methods used complicate any comparisons: CSF ferritin levels in this study were lower than levels in individuals either with or without RLS that were reported by Mizuno et al. and they were also lower than levels observed in chronic demyelinating disorders like chronic progressive multiple sclerosis [37, 38, 67]. Assays for total ferritin, rather than H-ferritin, may also have been used in previous studies. As with other intracellular microorganisms, the manipulation of cellular iron homeostasis by HIV to benefit its own replication may eventually result in altered brain iron balance (either functional iron deficiency, or iron excess in specific brain regions, or a combination of these). Significant changes in total CSF iron biomarker levels may or may not accurately reflect these regional changes. CSF iron, transferrin and ferritin did not appear to be correlated with their respective serum levels in 11 individuals with visit-matched CSF and serum samples, but the small size of the sample with both sets of measurements precludes firm conclusions. While possibly due to insufficient power, the absence of significant correlations supports the concept that levels of iron and iron transporters in the CNS are actively regulated and do not merely reflect passive influx from the circulation; this view is entirely consistent with prior studies [50]. Differences in serum and CSF assays used for iron-biomarker quantification and the fact that H-ferritin was measured in CSF, while the L subunit (iron-poor form) of ferritin predominates in serum, could also account for these differences. Relatively little is known about mechanisms controlling total or H-ferritin levels in either compartment [95].
We acknowledge the limitations of this study, including its cross-sectional design, which limits interpretation, the lack of an HIV-negative comparison group, and absence of matched serum iron biomarker data for most participants. Moderately correlated, within-individual values of iron, transferrin and H-ferritin obtained at baseline and 6 months in 100 of the study participants, however, support the use of single CSF biomarker measurements for our analyses and favor their stability in HIV+ persons over short periods of time. Regarding the lack of HIV-negative controls, we would stress that our objective was not to determine the impact of HIV on CSF iron biomarker levels, but to ascertain their associations with key demographic, HIV disease- and treatment-related predictors of neurocognitive decline, since measures of HAND are often imprecise and fluctuate in individuals over time [4]. Better knowledge of iron biomarker variability and associations with these other host factors will facilitate the design of future studies and inform the precision of predictive models. Longitudinal follow-up studies with measurements of biomarkers at more than one time-point in individual disease trajectories will be needed to clarify the temporal sequence of iron dysregulation after HIV infection, although such studies may be challenging due to the invasive nature of CSF sampling. This study provides a systematic assessment of the demographic and disease-related factors associated with CSF iron biomarker levels in HIV+ persons, laying the foundation for studies that specifically evaluate whether changes in these iron-related measures promote the development of HAND.
Conclusions
In HIV+ adults, CSF levels of iron and major biomarkers of iron-transport are independently associated with sex, self-reported race/ethnicity, ART, plasma virus detectability and/or CSF VL. Associations of CSF iron biomarkers with age, which disappeared following adjustment for a measure of blood-CSF barrier function, suggests the possibility that age- or HIV-related declines in the integrity of the blood-CSF barrier may contribute to changes in CNS iron balance as HIV+ individuals age. Furthermore, this study raises the intriguing possibility that consistent correlates of HAND such as race/ethnicity, ART, and HIV RNA in the CSF, may be linked to HAND in part via changes in CNS iron homeostasis. Additional studies, preferably including longitudinal samples and a higher number of participants over 50 years of age, as well as matched HIV-negative controls, are needed to further investigate these questions.
Abbreviations
- CSF:
-
cerebrospinal fluid
- ART:
-
antiretroviral therapy
- HAND:
-
HIV-associated neurocognitive disorder
- CNS:
-
central nervous system
- HIV+:
-
HIV-infected
- ZDV:
-
zidovudine
- ALS:
-
amyotrophic lateral sclerosis
- RLS:
-
restless leg syndrome
- BBB:
-
blood–brain barrier
- VL:
-
viral load (HIV RNA concentration)
- CHARTER:
-
CNS HIV antiretroviral therapy effects research (study)
- IQR:
-
interquartile range
- QAlb :
-
CSF to serum albumin ratio
References
(UNAIDS) J.U.N.P.o.H.A., global report: UNAIDS report on the global AIDS epidemic; 2012.
Mateen FJ, Mills EJ. Aging and HIV-related cognitive loss. JAMA. 2012;308:349–50.
Wing EJ. HIV and aging. Int J Infect Dis. 2016;53:61–8.
Kallianpur AR, Levine AJ. Host genetic factors predisposing to HIV-associated neurocognitive disorder. Curr HIV/AIDS Rep. 2014;11:336–52.
So-Armah KA, Chang J, Alcorn C, Lo Re V, Baker JV, Tracy R, et al. HIV infection, antiretroviral therapy initiation and longitudinal changes in biomarkers of organ function. Curr HIV Res. 2014;12:50–9.
Heaton RK, Clifford DB, Franklin DR Jr, Woods SP, Ake C, Vaida F, CHARTER Group, et al. HIV-associated neurocognitive disorders persist in the era of potent antiretroviral therapy: CHARTER Study. Neurology. 2010;75:2087–96.
Heaton RK, Franklin DR, Ellis RJ, McCutchan JA, Letendre SL, Leblanc S, CHARTER Group, HNRC Group, et al. HIV-associated neurocognitive disorders before and during the era of combination antiretroviral therapy: differences in rates, nature, and predictors. J Neurovirol. 2011;17:3–16.
Angelovich TA, Hearps AC, Maisa A, Martin GE, Lichtfuss GF, Cheng WJ, et al. Viremic and virologically suppressed hiv infection increases age-related changes to monocyte activation equivalent to 12 and 4 years of aging respectively. J Acquir Immune Defic Syndr. 2015;69:11–7.
Tedaldi EM, Minniti NL, Fischer T. HIV-associated neurocognitive disorders: the relationship of HIV infection with physical and social comorbidities. Biomed Res Int. 2015;2015:641913.
Horvath S, Levine AJ. HIV-1 infection accelerates age according to the epigenetic clock. J Infect Dis. 2015;212:1563–73.
Ellis RJ, Badiee J, Vaida F, Letendre S, Heaton RK, Clifford D, CHARTER Group, et al. CD4 nadir is a predictor of HIV neurocognitive impairment in the era of combination antiretroviral therapy. AIDS. 2011;25:1747–51.
McArthur JC, Hoover DR, Bacellar H, Miller EN, Cohen BA, Becker JT, et al. Dementia in AIDS patients: incidence and risk factors. Multicenter AIDS Cohort Study. Neurology. 1993;43:2245–52.
Heaton RK, Franklin DR Jr, Deutsch R, Letendre S, Ellis RJ, Casaletto K, CHARTER Group, et al. Neurocognitive change in the era of HIV combination antiretroviral therapy: the longitudinal CHARTER study. Clin Infect Dis. 2015;60:473–80.
Kallianpur AR, Wang Q, Jia P, Hulgan T, Zhao Z, Letendre SL, CHARTER Study Group, et al. Anemia and red blood cell indices predict HIV-associated neurocognitive impairment in the highly active antiretroviral therapy era. J Infect Dis. 2016;213:1065–73.
Redig AJ, Berliner N. Pathogenesis and clinical implications of HIV-related anemia in 2013. Hematol Am Soc Hematol Educ Progr. 2013;2013:377–81.
Bozzi A, Brisdelli F, D’Alessandro AM, D’Andrea G, Lizzi AR, Rinaldi AC, et al. Effects of AZT on cellular iron homeostasis. Biometals. 2004;17:443–50.
D’Andrea G, Brisdelli F, Bozzi A. AZT: an old drug with new perspectives. Curr Clin Pharmacol. 2008;3:20–37.
Maki PM, Martin-Thormeyer E. HIV, cognition and women. Neuropsychol Rev. 2009;19:204–14.
Royal W 3rd, Cherner M, Burdo TH, Umlauf A, Letendre SL, Jumare J, et al. Associations between cognition, gender and monocyte activation among HIV infected individuals in Nigeria. PLoS ONE. 2016;11:e0147182.
Hestad KA, Menon JA, Silalukey-Ngoma M, Franklin DR Jr, Imasiku ML, Kalima K, et al. Sex differences in neuropsychological performance as an effect of human immunodeficiency virus infection: a pilot study in Zambia, Africa. J Nerv Ment Dis. 2012;200:336–42.
Hulgan T, Samuels DC, Bush W, Ellis RJ, Letendre SL, Heaton RK, CHARTER Group, et al. Mitochondrial DNA haplogroups and neurocognitive impairment during HIV infection. Clin Infect Dis. 2015;61:1476–84.
Marquine MJ, Sakamoto M, Dufour C, Rooney A, Fazeli P, Umlauf A, et al. HNRP Group. The impact of ethnicity/race on the association between the Veterans Aging Cohort Study (VACS) index and neurocognitive function among HIV-infected persons. J Neurovirol. 2016;22:442–54.
Mindt MR, Miranda C, Arentoft A, Byrd D, Monzones J, Fuentes A, et al. Aging and HIV/AIDS: neurocognitive implications for older HIV-positive Latina/o adults. Behav Med. 2014;40:116–23.
Duck KA, Connor JR. Iron uptake and transport across physiological barriers. Biometals. 2016;29:573–91.
Hadzhieva M, Kirches E, Mawrin C. Review: iron metabolism and the role of iron in neurodegenerative disorders. Neuropathol Appl Neurobiol. 2014;40:240–57.
Galbiati A, Marelli S, Giora E, Zucconi M, Oldani A, Ferini-Strambi L. Neurocognitive function in patients with idiopathic restless legs syndrome before and after treatment with dopamine-agonist. Int J Psychophysiol. 2015;95:304–9.
Pichler I, Del Greco MF, Gögele M, Lill CM, Bertram L, Do CB, et al. Serum iron levels and the risk of Parkinson disease: a Mendelian randomization study. PLoS Med. 2013;10:e1001462.
Crespo ÂC, Silva B, Marques L, Marcelino E, Maruta C, Costa S, et al. Genetic and biochemical markers in patients with Alzheimer’s disease support a concerted systemic iron homeostasis dysregulation. Neurobiol Aging. 2014;35:777–85.
Bandyopadhyay S, Rogers JT. Alzheimer’s disease therapeutics targeted to the control of amyloid precursor protein translation: maintenance of brain iron homeostasis. Biochem Pharmacol. 2014;88:486–94.
Ayton S, Faux NG, Bush AI. Alzheimer’s disease neuroimaging initiative ferritin levels in the cerebrospinal fluid predict Alzheimer’s disease outcomes and are regulated by APOE. Nat Commun. 2015;6:6760.
Scott SP, Murray-Kolb LE. Iron status Is associated with performance on executive functioning tasks in nonanemic young women. J Nutr. 2016;146:30–7.
Lozoff B, Smith JB, Kaciroti N, Clark KM, Guevara S, Jimenez E. Functional significance of early-life iron deficiency: outcomes at 25 years. J Pediatr. 2013;163:1260–6.
Berglund SK, Westrup B, Hägglöf B, Hernell O, Domellöf M. Effects of iron supplementation of LBW infants on cognition and behavior at 3 years. Pediatrics. 2013;131:47–55.
Khalil M, Riedlbauer B, Langkammer C, Enzinger C, Ropele S, Stojakovic T, et al. Cerebrospinal fluid transferrin levels are reduced in patients with early multiple sclerosis. Mult Scler J. 2014;20(12):1569–77.
Mitchell RM, Simmons Z, Beard JL, Stephens HE, Connor JR. Plasma biomarkers associated with ALS and their relationship to iron homeostasis. Muscle Nerve. 2010;42:95–103.
Mizuno S, Mihara T, Miyaoka T, Inagaki T, Horiguchi J. CSF iron, ferritin and transferrin levels in restless legs syndrome. J Sleep Res. 2005;14:43–7.
Earley CJ, Connor JR, Beard JL, Malecki EA, Epstein DK, Allen RP. Abnormalities in CSF concentrations of ferritin and transferrin in restless legs syndrome. Neurology. 2000;54:1698–700.
LeVine SM, Lynch SG, Ou CN, Wulser MJ, Tam E, Boo N. Ferritin, transferrin and iron concentrations in the cerebrospinal fluid of multiple sclerosis patients. Brain Res. 1999;821:511–5.
Simpson IA, Ponnuru P, Klinger ME, Myers RL, Devraj K, Coe CL, et al. A novel model for brain iron uptake: introducing the concept of regulation. J Cereb Blood Flow Metab. 2015;35:48–57.
Granziera C, Daducci A, Simioni S, Cavassini M, Roche A, Meskaldji D, et al. Micro-structural brain alterations in aviremic HIV+ patients with minor neurocognitive disorders: a multi-contrast study at high field. PLoS ONE. 2013;8:e72547.
Gkouvatsos K, Papanikolaou G, Pantopoulos K. Regulation of iron transport and the role of transferrin. Biochim Biophys Acta. 1820;2012:188–202.
Leitner DF, Connor JR. Functional roles of transferrin in the brain. Biochim Biophys Acta. 2012;1820:393–402.
Arosio P, Ingrassia R, Cavadini P. Ferritins: a family of molecules for iron storage, antioxidation and more. Biochim Biophys Acta. 2009;1790:589–99.
Feelders RA, Vreugdenhil G, Eggermont AM, Kuiper-Kramer PA, van Eijk HG, Swaak AJ. Regulation of iron metabolism in the acute-phase response: interferon gamma and tumour necrosis factor alpha induce hypoferraemia, ferritin production and a decrease in circulating transferrin receptors in cancer patients. Eur J Clin Invest. 1998;28:520–7.
Todorich B, Zhang X, Slagle-Webb B, Seaman WE, Connor JR. Tim-2 is the receptor for H-ferritin on oligodendrocytes. J Neurochem. 2008;107:1495–505.
Todorich B, Zhang X, Connor JR. H-ferritin is the major source of iron for oligodendrocytes. Glia. 2011;59:927–35.
Fisher J, Devraj K, Ingram J, Slagle-Webb B, Madhankumar AB, Liu X, Klinger M, Simpson IA, Connor JR. Ferritin: a novel mechanism for delivery of iron to the brain and other organs. Am J Physiol Cell Physiol. 2007;293:C641–9.
Ritchie RF, Palomaki GE, Neveux LM, Navolotskaia O. Reference distributions for the negative acute-phase proteins, albumin, transferrin, and transthyretin: a comparison of a large cohort to the world’s literature. J Clin Lab Anal. 1999;13:280–6.
Kushner I. The phenomenon of the acute phase response. Ann NY Acad Sci. 1982;389:39–48.
Singh N, Haldar S, Tripathi AK, Horback K, Wong J, Sharma D, et al. Brain iron homeostasis: from molecular mechanisms to clinical significance and therapeutic opportunities. Antioxid Redox Signal. 2014;20:1324–63.
Fuchs D, Zangerle R, Artner-Dworzak E, Weiss G, Fritsch P, Tilz GP, et al. Association between immune activation, changes of iron metabolism and anaemia in patients with HIV infection. Eur J Haematol. 1993;50:90–4.
Pugliese A, Gennero L, Pescarmona GP, Beccattini M, Morra E, Orofino G, et al. Serum citrate levels, haptoglobin haplotypes and transferrin receptor (CD71) in patients with HIV-1 infection. Infection. 2002;30:86–9.
Salomé MA, Grotto HZ. Human immunodeficiency virus-related anemia of chronic disease: relationship to hematologic, immune, and iron metabolism parameters, and lack of association with serum interferon-gamma levels. AIDS Patient Care STDS. 2002;16:361–5.
Armitage AE, Stacey AR, Giannoulatou E, Marshall E, Sturges P, Chatha K, et al. Distinct patterns of hepcidin and iron regulation during HIV-1, HBV, and HCV infections. Proc Natl Acad Sci USA. 2014;111:12187–92.
Perrella O, Finelli L, Munno I, Perrella A, Soscia E, Carrieri PB. Cerebrospinal fluid ferritin in human immunodeficiency virus infection: a marker of neurologic involvement? J Infect Dis. 1993;168:1079–80.
Deisenhammer F, Miller RF, Brink NS, Harrison MJ, Thompson EJ. Cerebrospinal fluid ferritin in HIV infected patients with acute neurological episodes. Genitourin Med. 1997;73:181–3.
Lleó A, Cavedo E, Parnetti L, Vanderstichele H, Herukka SK, Andreasen N, et al. Cerebrospinal fluid biomarkers in trials for Alzheimer and Parkinson diseases. Nat Rev Neurol. 2015;11:41–55.
Dickens AM, Anthony DC, Deutsch R, Mielke MM, Claridge TD, Grant I, et al. Cerebrospinal fluid metabolomics implicate bioenergetic adaptation as a neural mechanism regulating shifts in cognitive states of HIV-infected patients. AIDS. 2015;29:559–69.
Tarawneh R, Head D, Allison S, Buckles V, Fagan AM, Ladenson JH, et al. Cerebrospinal fluid markers of neurodegeneration and rates of brain atrophy in early Alzheimer disease. JAMA Neurol. 2015;72:656–65.
Patton SM, Coe CL, Lubach GR, Connor JR. Quantitative proteomic analyses of cerebrospinal fluid using iTRAQ in a primate model of iron deficiency anemia. Dev Neurosci. 2012;34:354–65.
Hyacinthe C, De Deurwaerdere P, Thiollier T, Li Q, Bezard E, Ghorayeb I. Blood withdrawal affects iron store dynamics in primates with consequences on monoaminergic system function. Neuroscience. 2015;290:621–35.
Clendenen TV, Koenig KL, Arslan AA, Lukanova A, Berrino F, Gu Y, et al. Factors associated with inflammation markers, a cross-sectional analysis. Cytokine. 2011;56:769–78.
Antinori A, Arendt G, Becker JT, Brew BJ, Byrd DA, Cherner M, et al. Updated research nosology for HIV-associated neurocognitive disorders. Neurology. 2007;69:1789–99.
Burtis C, Ashwood E, Bruns D, editors. Tietz textbook of clinical chemistry and molecular diagnostics. Elsevier Saunders: St. Louis; 2012.
de Almeida SM, Rotta I, Ribeiro CE, Smith D, Wang R, Iudicello J, Potter M, Vaida F, Letendre S, Ellis RJ, HNRC Group. Blood–CSF barrier and compartmentalization of CNS cellular immune response in HIV infection. J Neuroimmunol. 2016;301:41–8.
Gichohi-Wainaina WN, Tanaka T, Towers GW, Verhoef H, Veenemans J, Talsma EF, et al. Associations between common variants in iron-related genes with haematological traits in populations of African Ancestry. PLoS ONE. 2016;11:e0157996.
Hozumi I, Hasegawa T, Honda A, Ozawa K, Hayashi Y, Hashimoto K, et al. Patterns of levels of biological metals in CSF differ among neurodegenerative diseases. J Neurol Sci. 2011;303:95–9.
Clardy SL, Earley CJ, Allen RP, Beard JL, Connor JR. Ferritin subunits in CSF are decreased in restless legs syndrome. J Lab Clin Med. 2006;147:67–73.
Clardy SL, Wang X, Boyer PJ, Earley CJ, Allen RP, Connor JR. Is ferroportin-hepcidin signaling altered in restless legs syndrome? J Neurol Sci. 2006;247:173–9.
Earley CJ, Connor JR, Beard JL, Clardy SL, Allen RP. Ferritin levels in the cerebrospinal fluid and restless legs syndrome: effects of different clinical phenotypes. Sleep. 2005;28:1069–75.
Congdon EL, Westerlund A, Algarin CR, Peirano PD, Gregas M, Lozoff B, et al. Iron deficiency in infancy is associated with altered neural correlates of recognition memory at 10 years. J Pediatr. 2012;160:1027–33.
Doom JR, Georgieff MK. Striking while the iron is hot: understanding the biological and neurodevelopmental effects of iron deficiency to optimize intervention in early childhood. Curr Pediatr Rep. 2014;2:291–8.
Lozoff B, Beard J, Connor J, Barbara F, Georgieff M, Schallert T. Long-lasting neural and behavioral effects of iron deficiency in infancy. Nutr Rev. 2006;64(Suppl (5 Pt 2)):34–43.
Minchella PA, Armitage AE, Darboe B, Jallow MW, Drakesmith H, Jaye A, et al. Elevated hepcidin is part of a complex relation that links mortality with iron homeostasis and anemia in men and women with HIV infection. J Nutr. 2015;145:1194–201.
Chang HC, Bayeva M, Taiwo B, Palella FJ Jr, Hope TJ, Ardehali H. Short communication: high cellular iron levels are associated with increased HIV infection and replication. AIDS Res Hum Retroviruses. 2015;31:305–12.
Drakesmith H, Chen N, Ledermann H, Screaton G, Townsend A, Xu XN. HIV-1 Nef down-regulates the hemochromatosis protein HFE, manipulating cellular iron homeostasis. Proc Natl Acad Sci USA. 2005;102:11017–22.
Skjørringe T, Møller LB, Moos T. Impairment of interrelated iron- and copper homeostatic mechanisms in brain contributes to the pathogenesis of neurodegenerative disorders. Front Pharmacol. 2012;3:169.
Speeckaert MM, Speeckaert R, Delanghe JR. Biological and clinical aspects of soluble transferrin receptor. Crit Rev Clin Lab Sci. 2010;47(5–6):213–28.
Flax VL, Adair LS, Allen LH, Shahab-Ferdows S, Hampel D, Chasela CS, Teqha G, Daza EJ, Corbett A, Davis NL, Kamwendo D, Kourtis AP, van der Horst CM, Jamieson DM, Bengley ME, BAN Study Team. Plasma microniutrient concentrations are altered by antiretroviral therapy and lipid-based nutrient supplements in lactating HIV-infected Malawian women. J Nutr. 2015;145:1950–7.
Ganz T, Nemeth E. Iron balance and the role of hepcidin in chronic kidney disease. Semin Neprhol. 2016;36:87–93.
Happe S, Kundmüller L, Reichelt D, Husstedt IW, Evers S. Comorbidity of restless legs syndrome and HIV infection. J Neurol. 2007;254:1401–6.
Provini F, Chiaro G. Neuroimaging in restless legs syndrome. Sleep Med Clin. 2015;10:215–26.
Meyers DG. The iron hypothesis—does iron cause atherosclerosis? Clin Cardiol. 1996;19:925–9.
Gill AJ, Kovacsics CE, Vance PJ, Collman RG, Kolson DL. Induction of heme oxygenase-1 deficiency and associated glutamate-mediated neurotoxicity is a highly conserved HIV phenotype of chronic macrophage infection that is resistant to antiretroviral therapy. J Virol. 2015;89:10656–67.
Cheng HT, Yen CJ, Chang CC, Huang KT, Chen KH, Zhang RY, Lee PY, MIaw SC, Huang JW, Chiang CK, Wu KD, Hung KY. Ferritin heavy chain mediates the protective effect of heme oxygenase-1 against oxidative stress. Biochim Biophys Acta. 2015;1850:2506–17.
Earley CJ, Connor J, Garcia-Borreguero D, Jenner P, Winkelman J, Zee PC, et al. Altered brain iron homeostasis and dopaminergic function in restless legs syndrome (Willis–Ekbom disease). Sleep Med. 2014;15:1288–301.
Kim J, Wessling-Resnick M. Iron and mechanisms of emotional behavior. J Nutr Biochem. 2014;25:1101–7.
Ortancil O, Sanli A, Eryuksel R, Basaran A, Ankarali H. Association between serum ferritin level and fibromyalgia syndrome. Eur J Clin Nutr. 2010;64(308–12):78.
Fennema-Notestine C, Ellis RJ, Archibald SL, Jernigan TL, Letendre SL, Notestine RJ, CHARTER Group, et al. Increases in brain white matter abnormalities and subcortical gray matter are linked to CD4 recovery in HIV infection. J Neurovirol. 2013;19:393–401.
Li J, Wu G, Wen Z, Zhang J, Lei H, Gui X, et al. White Matter Development is Potentially Influenced in Adolescents with Vertically Transmitted HIV Infections: a Tract-Based Spatial Statistics Study. AJNR Am J Neuroradiol. 2015;36:2163–9.
Hoare J, Fouche JP, Spottiswoode B, Donald K, Philipps N, Bezuidenhout H, et al. A diffusion tensor imaging and neurocognitive study of HIV-positive children who are HAART-naive “slow progressors”. J Neurovirol. 2012;18:205–12.
Clifford DB. HIV-associated neurocognitive disorder. Curr Opin Infect Dis. 2017;30:117–22.
Campbell GR, Rawat P, Bruckman RS, Spector SA. Human Immunodeficiency Virus type 1 Nef inhibits autophagy through transcription factor EB sequestration. PLoS Pathog. 2015;11:e1005018.
Biasiotto G, Di Lorenzo D, Archetti S, Zanella I. Iron and neurodegeneration: is ferritinophagy the link? Mol Neurobiol. 2016;53:5542–74.
Wang W, Knovich MA, Coffman LG, Torti FM, Torti SV. Serum ferritin: past, present and future. Biochim Biophys Acta. 2010;1800:760–9.
Authors’ contributions
Specific contributions to this manuscript were as follows: SP performed all CSF iron, transferrin and ferritin measurements at the bench and drafted the manuscript; QW and PJ performed multivariable regression analyses; ZZ supervised all analyses and commented on the manuscript; JC assisted in study design, supervised biomarker measurement in his laboratory, and provided helpful comments on the manuscript; TH assisted in data interpretation and commented on the manuscript; RE and SL assisted in selection of CSF samples and commented on the manuscript; DF assisted in sample selection and coordinated sample shipments; WB and DC provided helpful comments on the manuscript; HK assisted in analyses and development of figures for the revised manuscript; JI helped to acquire CSF and serum albumin data and provided this quality-controlled dataset for analyses; AK conceived, designed, and implemented the study, revised the manuscript, and performed some of the statistical analyses. IG was Principal Investigator of the parent CHARTER study that provided data and samples for these analyses. Both TH and AK funded the study. Authors SP and AK contributed equally to this work. All authors read and approved the final manuscript.
Acknowledgements
The authors gratefully acknowledge the many CHARTER study participants who provided CSF and clinical data for this study, as well as the support of all CHARTER study investigators and sites.
CHARTER is affiliated with the University of California, San Diego; Johns Hopkins University; the Icahn School of Medicine of Mount Sinai; University of Texas Medical Branch, Galveston; University of Washington, Seattle; Washington University, Saint Louis, and it is headquartered at the University of California, San Diego.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
All data generated or analyzed during this study are included in this published article and its Additional files 1, 2 and 3.
Ethics approval and consent to participate
CHARTER is has been continuously approved by the Institutional Review Boards of all participating institutions listed in the Methods. All CHARTER study participants provided written informed consent for the study, and the CHARTER Study adheres to the ethical principles set forth in the Declaration of Helsinki.
Funding
NIH R01 MH095621 and Supplemental Award NIH MH095621 04S1 (to A.R.K. and T.H.).
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Additional files
12987_2017_58_MOESM1_ESM.docx
Additional file 1: Figure S1. Scatter plots of iron biomarker values in CSF at baseline (N=403) and 6 months (N=100). P-values shown are for corresponding Spearman correlations.
12987_2017_58_MOESM2_ESM.docx
Additional file 2: Table S1. Iron biomarker values for CHARTER study participants at baseline and 6-months. Units of measurement: (CSF) iron, µg/dL; transferrin, µg/mL; ferritin, ng/mL.
12987_2017_58_MOESM3_ESM.docx
Additional file 3. Visit-matched (6-month) CSF and serum iron biomarker values for 11 CHARTER study participants. Units of measurement: (CSF) iron, µg/dL; transferrin, µg/mL; ferritin, ng/mL; (Serum) iron, µg/dL; transferrin, mg/dL; ferritin, ng/mL.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Patton, S.M., Wang, Q., Hulgan, T. et al. Cerebrospinal fluid (CSF) biomarkers of iron status are associated with CSF viral load, antiretroviral therapy, and demographic factors in HIV-infected adults. Fluids Barriers CNS 14, 11 (2017). https://doi.org/10.1186/s12987-017-0058-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12987-017-0058-1