Abstract
Background
In pregnancy, reduction of HIV plasma viral load (pVL) for the prevention of vertical transmission is time-constrained. The study primary objective is to investigate factors associated with faster initial HIV RNA half-life decay when combination antiretroviral treatment (cART) is initiated in pregnancy.
Methods
This was a multicentre, retrospective, observational study, conducted in south England, United Kingdom, between August 2001 and February 2018. Data were extracted from case notes of eligible women initiating cART during the index pregnancy. Anonymised data were collated and analysed centrally. Regression analyses were conducted to determine factors associated with faster HIV RNA half-life decay in the first 14 days after commencing cART (first-phase), and with achieving an undetectable maternal pVL by 36 weeks’ gestation. We then assessed whether HIV- and obstetric- related parameters differed by antiretroviral third agent class and whether the proportions of women with undetectable pVL at 36 weeks’ gestation and at delivery differed by antiretroviral third agent class.
Results
Baseline pVL was the only independent factor associated with faster first-phase HIV RNA half-life decay on commencing cART. Lower pVL on day 14 after starting cART was associated with an increased likelihood of achieving an undetectable pVL by 36 weeks’ gestation. Integrase inhibitor-based cART was associated with a faster first-phase HIV RNA half-life decay on commencing cART. Overall, 73% and 85% of women had an undetectable pVL at 36 weeks’ gestation and at delivery respectively, with no significant difference by antiretroviral third agent class.
Conclusions
Only high baseline pVL independently contributed to a faster rate of first-phase viral half-life decay. pVL at 14 days after initiating cART allows early identification of treatment failure. In the first 14 days after initiating cART in pregnancy, integrase inhibitor-based cART reduced maternal pVL faster than protease inhibitor- and non-nucleoside reverse transcriptase-based cART. While our study findings support INSTI use when initiated in pregnancy especially when initiated at later gestations and in those with higher baseline pVL, other non-INSTI based cART with more data on safety in pregnancy also performed well.
Similar content being viewed by others
Background
In the UK, opt-out antenatal HIV-1/2 (hereafter referred to as HIV) screening, combination antiretroviral treatment (cART) and infant formula feeding have successfully reduced rates of vertical transmission of HIV from 25% in 1993 [1], to the present national rate of < 0.5% [2,3,4]. In recent years, the majority of pregnant women living with HIV (WLWH) in the UK conceive on cART and maintain HIV suppression throughout pregnancy [4]. However, as recently as 2015–2016, 30% of pregnant WLWH in the UK were still initiating cART during pregnancy [5].
Guidance regarding the timing of cART initiation and the class of compounds used during pregnancy has evolved over the study period and continue to vary between guidelines [6,7,8,9]. British HIV Association (BHIVA) guidelines recommend that if maternal plasma viral load (pVL) is > 100,000 copies/mL and/or CD4+ count is < 200 cells/µL, cART should be initiated within the first trimester, and that all women should have commenced cART by 24 weeks’ gestation [10]. Women presenting with untreated HIV beyond 28 weeks’ gestation should initiate cART immediately, and if pVL is > 100,000 copies/mL, a three- or four-drug regimen including raltegravir or dolutegravir is recommended. Read et al. demonstrated that delaying the initiation of cART beyond 26.3 weeks’ gestation when baseline pVL is < 10,000 copies/mL, or beyond 20.4 weeks’ gestation when baseline pVL is > 100,000 copies/mL, was associated with a reduced likelihood of achieving pVL < 50 copies/mL by delivery [11].
The rationale behind recommending the initiation of integrase strand transferase inhibitor (INSTI)-based cART, especially later in pregnancy, is the presumption that a more rapid reduction in maternal pVL will result in a higher chance of having an undetectable maternal pVL by delivery, with subsequent lower rates of perinatal HIV acquisition. Maternal viral burden is a strong predictor of perinatal HIV transmission, with a vertical transmission risk of 63% when untreated maternal pVL is > 100,000 copies/mL during pregnancy and at delivery [12], compared to 0.1% when maternal pVL is < 50 copies/mL on cART [2]. The risk of vertical transmission increases with shorter periods on cART prior to delivery: 3.5% with > 16 weeks of cART and 9% in women who initiate cART < 4 weeks prior to delivery [13]. However, the reductions in HIV vertical transmission are only partly explained by reductions in maternal pVL: firstly, in ACTG 076, maternal pVL at delivery in women initiating zidovudine monotherapy during pregnancy was only 0.24 log10 HIV RNA copies/mL lower than in the placebo group, but HIV vertical transmission reduced by 67% in the zidovudine group [14, 15]. Secondly, a single-dose of nevirapine administered at the onset of labour was capable of reducing HIV vertical transmission by nearly 50% [16] compared to zidovudine monotherapy initiated during labour. Given these findings, the reduction in vertical transmission in WLWH on cART during pregnancy can be considered to be the result of both treatment as prevention and infant peri-exposure prophylaxis.
Observational studies suggest that in the absence of cART and in exclusively formula-fed babies, two-thirds of HIV vertical transmissions occur during the intrapartum period [17]. However, in the cART era, 80% of HIV vertical transmission is thought to occur during the later stages of the antepartum period, prior to the onset of labour [18]. For women with untreated HIV infection, strategies that rapidly suppress maternal pVL during pregnancy are desirable, although the evidence that this directly translates into fewer HIV vertical transmissions is not yet available.
Modelling and clinical studies have demonstrated that when three or more antiretroviral drugs are initiated, a rapid exponential decline in pVL occurs in the first 6–14 days [19, 20], followed by a slower, second phase exponential decline, before pVL suppression [19, 21]. Choice of cART has been shown to affect time to viral suppression, notably with INSTI-based regimens achieving viral suppression significantly faster than other drug classes [22, 23].
The primary aim of our study was to investigate the factors associated with a faster first-phase plasma HIV RNA decay in women initiating cART during pregnancy. Secondary aims included investigating factors associated with an increased likelihood of having an undetectable pVL by 36 weeks’ gestation (given that in the UK, recommendations for mode of delivery are guided by maternal pVL at 36 weeks’ gestation [10] and investigating differences in HIV- and obstetric-related parameters when stratified by antiretroviral third agent class.
Methods
Study setting and ethical considerations
We conducted a retrospective case note review of all women initiating cART in pregnancy at HIV tertiary centres in south England, United Kingdom. The overall study was conducted between August 2001 and February 2018 to avoid bias, but the actual start dates varied according to site. All data were obtained as part of routine clinical care, anonymised at site, and then collated centrally for analysis. As per the National Research Ethics Service guidelines [24], additional patient consent and ethical approval were not required.
Eligibility criteria
Inclusion criteria were any woman commencing or re-commencing cART during the index pregnancy with a quantifiable pVL at baseline, and further evaluation on day 14 (± 3 days) following cART initiation. Subjects were excluded if poor adherence to cART was reported by either the subject or clinician.
Data collection
Clinical data collected included baseline demographics, HIV-specific parameters (cART history, CD4+ T cell count and pVL during index pregnancy) and obstetric and infant specific information (estimated due date and actual delivery date). Aggregate level data on infant HIV infection status (where available) was provided by the National Surveillance of HIV in Pregnancy and Childhood [25].
Outcome measures
The primary outcome was first-phase plasma HIV RNA half-life decay rate, 14 days after commencing cART. First phase HIV RNA half-life decay (T/2) was calculated using the formula: n × log10 0.5/log10 (VL1/VLBL), where n = number of days to VL1; VL1 = plasma HIV RNA load measured 14 days following the initiation of cART and VLBL = plasma HIV RNA load measured prior to the initiation of cART. T/2 was only calculated where VL1 was quantifiable. In a secondary analysis, when VL1 was reported as < 50 or < 20 HIV RNA copies/mL at day 14, a value of 49 or 19 HIV RNA copies/mL were imputed respectively, to enable an estimation of the slowest first phase T/2 in these women. Secondary outcomes were time taken to achieve undetectable maternal pVL (lower than the limits of quantification) and proportion of women with an undetectable pVL by 36 weeks’ gestation and by delivery. Subjects who did not achieve an undetectable pVL were censored at delivery.
Statistical analyses
Descriptive statistics summarised variables using median (interquartile range) and total (percentage). For the purposes of this study, the impact of the three dual nucleos(t)ide reverse transcriptase inhibitors (NRTIs) used were considered equal. In subjects on quadruple therapy comprising dual NRTIs, an INSTI and a protease inhibitor (PI), T/2 was presumed to reflect the INSTI component.
Maternal pVL of < 50 copies/mL were regarded as undetectable, including those measured between 20 and 49 copies/mL. All quantifiable pVL ≥ 20 copies/mL were included when calculating T/2. Time taken to achieve an undetectable pVL was calculated assuming that the date an undetectable pVL was achieved was the mid-point between the last detectable and first undetectable pVL.
Regression analysis was performed to investigate factors associated with faster T/2 (linear regression analysis) and with having an undetectable pVL at 36 weeks’ gestation (logistic regression analysis). Kruskall-Wallis test was used to assess whether HIV- and obstetric- related parameters differed by antiretroviral third agent class. Mann–Whitney test (with Bonferroni correction) was then used to compare the parameters between antiretroviral third agent class. Fisher’s exact test was used to assess whether the proportions of women with undetectable pVL at 36 weeks’ gestation and at delivery differed by antiretroviral third agent class. All statistical analyses were conducted using SPSS version 24 (IBM Corp, Armonk, NY, US). Statistical significance was defined as < 0.05 throughout.
Results
Of the 221 pregnant women at 11 participating HIV centres who initiated cART during the index pregnancy and had sufficient data for analysis, 192 had a detectable pVL after 14 days therapy. 29 women had VL1 < 50 copies/mL and are described separately.
Baseline characteristics
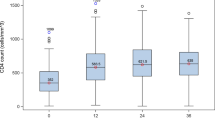
Baseline characteristics of the 192 women included in the main analysis are described in Table 1. 83.3% were Black African/Caribbean, 98.5% identified heterosexual intercourse as their route of HIV acquisition, 63.5% were cART-naïve and median CD4+ count prior to initiating cART (baseline) was 339 cells/µL (Table 1). 126 (65.6%) had pre-cART (baseline) plasma HIV RNA < 30,000 copies/mL, 37 (19.3%) between 30,000 and 100,000 HIV RNA copies/mL and 29 (15.1%) had baseline plasma HIV RNA > 100,000 copies/mL. 91% of women commenced cART before 28 weeks’ gestation: 181 (94.3%) women initiated a dual NRTI backbone plus a third agent, 11 (5.7%) initiated abacavir, lamivudine and zidovudine (ABC/3TC/AZT) (Table 1) and seven (3.6%) initiated quadruple cART. Amongst the 192 women included in the main analysis, pVL fell by a median of 1.8 log10 HIV RNA copies/mL 14 days after initiating cART, and median T/2 was 2.5 days (Table 1).
Factors associated with first-phase plasma HIV RNA half-life decay
Univariate linear regression analysis demonstrated that lower baseline CD4+ T-cell count, higher VLBL and INSTI-based cART were associated with faster viral decay (shorter T/2) (Table 2). However, in multivariable regression analysis, only higher VLBL remained independently associated with shorter T/2 (− 0.61 days per 1 log10 plasma HIV RNA higher, p < 0.001) (Table 2).
Factors associated with having an undetectable maternal plasma viral load at 36 weeks’ gestation
In multivariate logistic regression analysis, the following factors were associated with a higher probability of having an undetectable maternal pVL by 36 weeks’ gestation: lower maternal pVL 14 days after initiating cART (odds ratio (OR) 0.05, 95% confidence interval (CI) 0.01, 0.19) and earlier gestational age when cART was initiated (OR 0.66, 95% CI 0.58, 0.76) (Table 3).
Differences in HIV- and obstetric-related parameters when stratified according to antiretroviral third agent class
T/2 was significantly shorter in women commenced on INSTIs compared to those commenced on PIs, non-nucleoside reverse transcriptase inhibitor (NNRTIs), and ABC/3TC/AZT (p < 0.001, p < 0.001 and p = 0.03, respectively) (Table 4). T/2 was significantly longer in women commenced on PIs compared to NNRTIs, p = 0.03 (Table 4).
Women who initiated an INSTI had significantly higher VLBL compared to women initiating PIs and ABC/3TC/AZT (p < 0.001 and p < 0.001, respectively), while women commenced on ABC/3TC/AZT had significantly lower VLBL and higher baseline CD4 + counts compared to women commenced on PIs and NNRTIs (Table 4). Women who initiated NNRTIs had lower baseline CD4 compared to women initiated on PIs. While there was no statistically significant difference in the gestational age at which cART was commenced when stratified according to the three-third agent antiretroviral classes and ABC/3TC/AZT (Table 4), higher VLBL was significantly associated with earlier gestational age when cART was initiated, p = 0.02.
Between the four groups, the overall time to an undetectable pVL was numerically shorter in women commenced on INSTIs, but statistically only approached significance when comparing women initiating INSTIs (27.5 days) and NNRTIs (51.5 days), p = 0.05 (Table 4).
An undetectable pVL was seen in 72.9% of all women by 36 weeks gestational age with broadly similar rates across the three antiretroviral third agent classes: PIs 72.0%, NNRTIs 65.6% and INSTIs 76.5% (Table 4). 164 (85.4%) women had an undetectable pVL by delivery: PIs 85.6%, NNRTIs 75.0% and INSTIs 94.1% (Table 4). All women who initiated ABC/3TC/AZT had undetectable pVL at both 36 weeks’ gestation and delivery. Statistically, the proportions of women with undetectable pVL at 36 weeks’ gestation and at delivery did not differ significantly by antiretroviral third agent class (p = 0.13 and p = 0.17, respectively).
Women with pVL < 50 copies/mL at day 14 following cART initiation
Baseline characteristics for the 29 women with VL1 < 50 copies/mL were broadly similar to the 192 women included in the main analysis (Table 1). However, this cohort of 29 women had significantly higher baseline CD4+ count (p = 0.001), lower VLBL (p < 0.001), a higher proportion with Hepatitis B co-infection (p = 0.007), and all women had VLBL < 30,000 copies/mL. The longest estimated T/2 in this cohort of 29 women was similar to the T/2 seen in the subgroup of women included in the main analysis with VLBL < 30,000 copies/mL, p = 0.354.
Infant HIV infection rates
Infant HIV infection status was established for 171/221. All 171/221 infants were negative by molecular HIV testing at birth. For the remaining 50/221, infection status was not available. Although data on infant HIV peri-exposure prophylaxis were not available, each centre managed infants according to the contemporaneous version of the BHIVA guidelines on the management of HIV infection in pregnancy.
Discussion
In this study, higher baseline plasma viral load (VLBL) was the sole independent predictor of faster first-phase HIV RNA decay. Secondly, lower maternal pVL 14 days after cART initiation and earlier gestational age when cART was initiated independently predicted a higher likelihood of having an undetectable maternal pVL at 36 weeks’ gestation.
Overall, women in this cohort experienced a median 1.8 log10 copies/mL decline in pVL 14 days after initiating cART, with the shortest T/2 and thus, largest HIV RNA decline seen in women on INSTIs (despite small numbers of women on INSTIs), in keeping with the DolPHIN-1 (Dolutegravir in pregnant HIV mothers and their neonates) [26] study results demonstrating superior virological responses with dolutegravir-based cART compared to efavirenz-based cART when initiated in late pregnancy in low and middle-income settings. This strengthens the recommendation for assessing response to cART at this early stage and emphasises that clinicians and patients should expect around a 99% reduction in maternal pVL after 2 weeks of cART. Less convincing reductions in pVL at day 14, regardless of third agent in the cART regime, should be a cause for concern. Current BHIVA guidelines recommending all women should have started cART by 24 weeks’ gestation are based on the results published by Read et al. [11]. However, it is important to note that cART regimens in this study only included PIs, NNRTIs and ABC/3TC/AZT and did not include INSTI-based cART. Given the faster rate of HIV RNA declines in women on INSTIs as demonstrated in our study and other published data [26], the latest gestational age before which women on INSTI-based cART should have commenced cART will need to be explored in future studies.
Excluding ABC/3TC/AZT due to small subject numbers, only 66–77% of women on PIs, NNRTIs and INSTIs had undetectable pVL at 36 weeks’ gestation, when obstetric delivery plans are usually finalised. Of these women, those on INSTIs had the highest proportion of undetectable pVL by delivery and a shorter time to an undetectable pVL, despite starting with significantly higher VLBL, mirroring the findings seen in randomised trials of cART initiation during pregnancy performed in low and middle-income countries (DolPHIN-2 study [27]: dolutegravir versus efavirenz-based cART and the National Institute of Child Health and Human Development P1081 study [28]: raltegravir versus efavirenz-based cART). At present, INSTIs are considered the preferred antiretroviral third agent for women presenting late in pregnancy, yet in our study cohort, gestational age when cART was initiated was numerically earlier with INSTIs than with the other classes, reflecting the recommendation to initiate cART earlier in women with high baseline pVL. Over 90% of women in our study initiated cART before 28 weeks’ gestation but the low overall maternal CD4+ counts prior to initiating cART indicates that many of these women were presenting late in the course of their HIV infection.
While the small number of women who initiated ABC/3TC/AZT in pregnancy all had an undetectable pVL at delivery, they had lower VLBL and higher CD4+ counts than women who initiated PIs and NNRTIs, consistent with a targeted approach for initiating ABC/3TC/AZT. The results seen in this subgroup of women should therefore not be extrapolated to women with higher VLBL and lower baseline CD4+ counts.
Limitations of our study include the small number of subject initiating INSTIs, preventing statistical analysis of the clinical effects between the individual INSTI agents, and the long data collection period, meaning that data were collected and analysed for antiretroviral drugs that are now rarely used or commenced in the UK. While the exclusion of subjects with poor adherence reported by either the subject or clinician was necessary to enable the accurate calculation of the first-phase HIV RNA half-life decay during treatment, this may have led to inadvertent subject selection bias. Recent modelling studies have since suggested that on INSTI-based cART regimens, the original first phase T/2 described may be replaced by a split first phase (phase 1a and 1b), followed by the second phase which starts at a lower plasma viral load than the start of the second phase with PI and NNRTIs [29]. We were unable to explore this concept in our study.
The findings of this observational study support the use of INSTIs when initiating cART in pregnancy, especially in women presenting later in pregnancy and/or with higher VLBL on the basis of achieving rapid reductions in pVL and an undetectable viral load at delivery. However, it is important to note that non-INSTI-based regimens also performed well. Whilst awaiting further data on the higher incidence (0.3%) of neural tube defects in infants born to women conceiving on dolutegravir [30], there may well be a decrease in the use of dolutegravir, and possibly INSTIs as a whole, especially when initiating cART in the first trimester of pregnancy. In the meantime, other third agent antiretroviral drugs with more data on safety and efficacy in pregnancy that perform well in pregnancy are likely to be used in preference.
Conclusions
Higher baseline maternal pVL was the sole independent factor associated with faster HIV RNA decay 14 days after cART initiation. Lower maternal pVL 14 days after initiating cART, but not lower baseline maternal pVL, was associated with a higher chance of having an undetectable maternal pVL at 36 weeks’ gestation.
Availability of data and materials
The datasets generated and analysed during the current study are not publicly available but are available from the corresponding author upon reasonable request.
Abbreviations
- ABC/3TC/AZT:
-
Abacavir/lamivudine/zidovudine
- BHIVA:
-
British HIV Association
- cART:
-
Combination antiretroviral treatment
- DolPHIN study:
-
Dolutegravir in pregnant HIV mothers and their neonates study
- INSTI:
-
Integrase strand transferase inhibitor
- NRTIs:
-
Nucleos(t)ide reverse transcriptase inhibitors
- NNRTIs:
-
Non-nucleoside reverse transcriptase inhibitors
- PIs:
-
Protease inhibitors
- pVL:
-
Plasma viral load
- T/2:
-
First phase HIV RNA half-life decay
- VL1 :
-
Plasma HIV RNA load measured 14 days following the initiation of cART
- VLBL :
-
Plasma HIV RNA load measured prior to the initiation of cART
- WLWH:
-
Women living with HIV
References
Duong T, Ades AE, Gibb DM, Tookey PA, Masters J. Vertical transmission rates for HIV in the British Isles: estimates based on surveillance data. BMJ. 1999;319(7219):1227–9.
Townsend CL, Cortina-Borja M, Peckham CS, de Ruiter A, Lyall H, Tookey PA. Low rates of mother-to-child transmission of HIV following effective pregnancy interventions in the United Kingdom and Ireland, 2000–2006. AIDS. 2008;22(8):973–81.
Townsend CL, Byrne L, Cortina-Borja M, Thorne C, De Ruiter A, Lyall H, et al. Earlier initiation of ART and further decline in mother-to-child HIV transmission rates, 2000–2011. AIDS. 2014;28(7):1049–57.
Peters H, Francis K, Sconza R, Horn A, Peckham CS, Tookey PA, et al. UK mother-to-child HIV transmission rates continue to decline: 2012-2014. Clin Infect Dis. 2017;64(4):527–8.
Peters H, Francis K, Horn A, Thorne C. Successes and emerging challenges in prevention of vertical HIV transmission in the UK & Ireland. 2019; https://www.ucl.ac.uk/nshpc/sites/nshpc/files/peters_successes_and_challenges_pmtct.pdf.
European AIDS Clinical Society. European AIDS Clinical Society (EACS) Guidelines. Version 9. 2017;72. http://www.eacsociety.org/guidelines/eacs-guidelines/eacs-guidelines.html.
US Department of Health and Human Services. Recommendations for the Use of Antiretroviral Drugs in Pregnant Women with HIV Infection and Interventions to Reduce Perinatal HIV Transmission in the United States. AIDSinfo. 2017.
Money D, Tulloch K, Boucoiran I, Caddy S, Yudin MH, Allen V, et al. Guidelines for the care of pregnant women living with HIV and interventions to reduce perinatal transmission: executive summary. J Obstet Gynaecol Canada. 2014;36(8):721–34.
Organization WH. Rapid advice: use of antiretroviral drugs for treating pregnant women and preventing HIV infection in infants. Geneva: WHO; 2009.
Gilleece Y, et al. British HIV Association guidelines for the management of HIV in pregnancy and postpartum 2018. HIV Med. 2019;20:s2–85. https://doi.org/10.1111/hiv.12720.
Read PJ, Mandalia S, Khan P, Harrisson U, Naftalin C, Gilleece Y, et al. When should HAART be initiated in pregnancy to achieve an undetectable HIV viral load by delivery? AIDS. 2012;26(9):1095–103.
Garcia PM, Kalish LA, Pitt J, Minkoff H, Quinn TC, Burchett SK, et al. Maternal levels of plasma human immunodeficiency virus type 1 RNA and the risk of perinatal transmission. N Engl J Med. 1999;341(6):394–402.
Hoffman RM, Black V, Technau K, van der Merwe KJ, Currier J, Coovadia A, et al. Effects of highly active antiretroviral therapy duration and regimen on risk for mother-to-child transmission of HIV in Johannesburg, South Africa. J Acquir Immune Defic Syndr. 2010;54(1):35–41. http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=2880466&tool=pmcentrez&rendertype=abstract.
Sperling RS. Maternal viral load, zidovudine treatment, and the risk of transmission of human immunodeficiency virus type 1 from mother to infant. Stud Fam Plann. 2006;335(22):1621–9.
Connor EM, Sperling RS, Gelber R, Kiselev P, Scott G, O’Sullivan MJ, et al. Reduction of maternal-infant transmission of human immunodeficiency virus type 1 with zidovudine treatment. Pediatric AIDS Clinical Trials Group Protocol 076 Study Group. N Engl J Med. 1994;331(18):1173–80.
Guay LA, Musoke P, Fleming T, Bagenda D, Allen M, Nakabiito C, et al. Intrapartum and neonatal single-dose nevirapine compared with zidovudine for prevention of mother-to-child transmission of HIV-1 in Kampala, Uganda: hIVNET 012 randomised trial. Lancet. 1999;354(9181):795–802.
Rouzioux C, Costagliola D, Burgard M, Blanche S, Mayaux MJ, Griscelli C, et al. Estimated Timing of Mother-to-Child Human Immunodeficiency Virus Type 1 (HIV-1) Transmission by Use of a Markov Model. Am J Epidemiol [Internet]. 1995;142(12):1330–7. http://aje.oxfordjournals.org/content/142/12/1330.abstract?maxtoshow = &HITS = 10&hits = 10&RESULTFORMAT = &author1 = Rouzioux%252C + C%253B + &andorexacttitle = and&andorexacttitleabs = and&andorexactfulltext = and&searchid = 1&FIRSTINDEX = 0&fdate = 1/1/1995&tdate = 12/31/1995&res.
Magder LS, Mofenson L, Paul ME, Zorrilla CD, Blattner WA, Tuomala RE, et al. Risk factors for in utero and intrapartum transmission of HIV. J Acquir Immune Defic Syndr. 2005;38(1):87–95.
Perelson AS, Essunger P, Cao Y, Vesanen M, Hurley A, Saksela K, et al. Decay characteristics of HIV-1-infected compartments during combination therapy. Nature. 1997;387(6629):188–91.
Stephan C, Baldauf HM, Barry J, Giordano FA, Bartholomae CC, Haberl A, et al. Impact of raltegravir on HIV-1 RNA and DNA forms following initiation of antiretroviral therapy in treatment-naive patients. J Antimicrob Chemother. 2014;69(10):2809–18.
Ding AA, Wu H. Relationships between antiviral treatment effects and biphasic viral decay rates in modeling HIV dynamics. Math Biosci. 1999;160(1):63–82.
Hoenigl M, Chaillon A, Moore DJ, Morris SR, Mehta SR, Gianella S, et al. Rapid HIV viral load suppression in those initiating antiretroviral therapy at first visit after HIV diagnosis. Sci Rep. 2016;6(1):1–5.
Lennox JL, DeJesus E, Lazzarin A, Pollard RB, Madruga JVR, Berger DS, et al. Safety and efficacy of raltegravir-based versus efavirenz-based combination therapy in treatment-naive patients with HIV-1 infection: a multicentre, double-blind randomised controlled trial. Lancet. 2009;374(9692):796–806.
Do I need NHS Ethics approval? [Internet]. [cited 2019 Sep 23]. Available from: http://www.hra-decisiontools.org.uk/ethics/.
National Surveillance of HIV in Pregnancy and Childhood - UCL - London’s Global University. https://www.ucl.ac.uk/nshpc/.
Waitt C, Orrell C, Walimbwa S, Singh Y, Kintu K, Simmons B, et al. Safety and pharmacokinetics of dolutegravir in pregnant mothers with HIV infection and their neonates: a randomised trial (DolPHIN-1 study). PLoS Med. 2019;16(9):e1002895.
Kintu K, Malaba TR, Nakibuka J, Papamichael C, Colbers A, Byrne K, et al. Dolutegravir versus efavirenz in women starting HIV therapy in late pregnancy (DolPHIN-2): an open-label, randomised controlled trial. Lancet HIV. 2020;7:e332–9.
João EC, Morrison RL, Shapiro DE, Chakhtoura N, Gouvèa MIS, de Lourdes BTM, et al. Raltegravir versus efavirenz in antiretroviral-naive pregnant women living with HIV (NICHD P1081): an open-label, randomised, controlled, phase 4 trial. Lancet HIV. 2020;7(5):e322–31.
Cardozo EF, Andrade A, Mellors JW, Kuritzkes DR, Perelson AS, Ribeiro RM. Treatment with integrase inhibitor suggests a new interpretation of HIV RNA decay curves that reveals a subset of cells with slow integration. PLoS Pathog. 2017;13(7):e1006478.
Zash R, Holmes L, Diseko M, Jacobson DL, Brummel S, Mayondi G, et al. Neural-tube defects and antiretroviral treatment regimens in Botswana. N Engl J Med. 2019;381(9):827–40.
Acknowledgements
Department of Genitourinary Medicine & HIV, Queen Elizabeth Hospital, London, UK: Judith Russell; Department of Genitourinary Medicine & HIV, Central Middlesex Hospital, London, UK: Siobhan Murphy, Paola Hafner; Statistical Advisory Service, Imperial College London: Joseph Eliahoo.
Funding
None.
Author information
Authors and Affiliations
Consortia
Contributions
GPT conceptualised the design of the study; JA and GPT designed the study data collection proforma; JA, HP, KF, YG, FPF, REG, SP, MP, BCW, RS, SR, DAH, SC, LS, RM, AH, AVN, MR and GPT had major roles in the acquisition of the data; JA and GPT performed the statistical analysis; JA and GPT interpreted the data results; JA and GPT drafted and revised the initial manuscript; all authors contributed and revised the manuscript for intellectual content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Alagaratnam, J., Peters, H., Francis, K. et al. An observational study of initial HIV RNA decay following initiation of combination antiretroviral treatment during pregnancy. AIDS Res Ther 17, 41 (2020). https://doi.org/10.1186/s12981-020-00297-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12981-020-00297-w