Abstract
Background
Host genetic factors such as MBL2 gene polymorphisms cause defects in the polymerization of MBL protein and result in a functional deficiency and/or in low serum levels that can influence susceptibility to various viral infections. The aim of this study was to estimate the frequency of alleles, genotypes and haplotypes related to -550, -221 and exon 1 polymorphisms of the MBL2 gene and investigate their association with HHV-8 in people living with HIV/AIDS (PLWHA), as well as the impacts on CD4 cell count and HIV viral load in HIV/HHV-8 coinfected and HIV monoinfected patients.
Results
A cross sectional study in PLWHA, with and without HHV-8 infection, exploring associations between different factors, was performed in the outpatient infectious and parasitic diseases clinic at a referral hospital. Genomic DNA extractions from leukocytes were performed using a commercial Wizard® Genomic DNA Purification kit (Promega, Madison, WI). The promoter region (-550 and -221) was genotyped with the TaqMan system (Applied TaqMan Biosystems® genotyping Assays), and the structural region (exon1) was genotyped with Express Sybr Greener Supermix kit (Invitrogen, USA). In total, 124 HIV/HHV-8 coinfected and 213 HIV monoinfected patients were analysed. Median TCD4 counts were significantly lower in HIV/HHV-8 coinfected patients, whereas the mean of the first and last viral load of HIV did not present significant difference. There was no difference in frequency between the LL, YY and AA genotypes between the HIV/HHV-8 coinfected or HIV monoinfected patients. However, in a multivariate analysis, coinfected patients with the intermediate expression haplotype of the MBL2 gene had an odds ratio of 3.1-fold (CI = 1.2–7.6) of their last CD4 cell count being below 350 cells/mm3. Among the coinfected individuals, four developed KS and presented the intermediate expression MBL haplotype, with three being HYA/LXA and one being LYA/LYO.
Conclusions
Host genetic factors, such as -550, -221 and exon 1 polymorphisms, can be related to the may modify coinfections and/or to the development clinical manifestations caused by HHV-8, especially in HIV/HHV-8 coinfected patients who present the intermediate expression haplotypes of MBL.
Similar content being viewed by others
Background
Human herpesvirus 8 (HHV-8) is associated with all forms of Kaposi’s sarcoma (KS), being the necessary aetiological agent but insufficient alone for the development of this disease [1, 2]. Therefore, other factors such as host genetic polymorphisms may influence the development of clinical manifestations caused by HHV8. The prevalence of HHV-8 varies according to geographic regions and sub-populations, but after the human immunodeficiency virus (HIV) epidemic, the incidence of KS increased drastically compared to HIV-negative individuals, being one of the commonest cancers in people living with HIV (PLWHA) [3,4,5,6]. These coinfected patients have a more aggressive clinical course and progression to death [3,4,5,6].
The host’s innate and adaptive immune responses have a key role in the control of HHV-8 infection and the early stages of KS development [7,8,9]. Mannose-binding lectin (MBL) is a protein of the innate immune system that binds with high affinity to mannose or other carbohydrates that may be present on the surface of the pathogens. MBL can mediate phagocytosis by macrophages, and when associated with serine protease (MASP), it activates the complement system by the lectin pathway in an antibody-independent mechanism [10, 11].
The protein expression of MBL is determined genetically, and the serum concentration is directly related to mutations in the structural region of the MBL2 gene (exon 1) and in other polymorphic sites in the promoter region (-550 and -221). These three loci are closely related, and the allelic combinations of these regions result in different haplotypes that can cause defects in the polymerization of the molecule resulting in a functional deficiency and/or in low serum levels of MBL [12,13,14,15,16]. Thus, these polymorphisms have been associated with susceptibility or resistance to viral infections or the development of clinical manifestations and were studied in patients with hepatitis C virus, hepatitis B virus, human papillomavirus, Epstein-Barr virus, and dengue virus [17,18,19,20,21,22,23,24,25,26,27].
The progression of the disease caused by HIV infection is characterized by a decline in TCD4 cell count and an increase in viral load, leading to patient death in the absence of antiretroviral therapy [28]. Thus, some studies suggest that in HIV/HHV-8 coinfection, severe depletion or inactivation of T cells and HIV replication may be important factors in the clinical evolution of HHV-8 infection and the development of KS [4, 29,30,31].
However, host genetic factors such as MBL2 gene polymorphisms can control HIV/HHV-8 coinfection and influence on HHV-8 infection in PLWHA and/or the clinical evolution of coinfected individuals. The aim of this study was to estimate the frequency of alleles, genotypes and haplotypes related to -550, -221 and exon 1 polymorphisms of the MBL2 gene in HIV/HHV-8 coinfected and HIV monoinfected patients. In addition, we also explored associations of these gene variants with TCD4 cell count and HIV viral load in both groups.
Methodology
Study population
This is a cross section of PLWHA, with and without HHV-8 infection, in which patients’ demographic and laboratory variable data were originally described by Cahú et al. [32] in a research on the HIV/HHV-8 coinfection prevalence in 500 PLWHA, reporting 143 HIV/HHV-8 coinfected and 357 HIV monoinfected. Of this total, we randomly selected 124 HIV/HHV-8 coinfected and 213 HIV monoinfected patients, by the statistical program Epi Info version 7.1.5 (CDC, Atlanta, GA, USA), who were followed up by the doctors from the outpatient clinic Infectious and Parasitic Diseases in the Clinical Hospital of the Federal University of Pernambuco. This sample size was calculated using the same software, with the 99.9% confidence interval, with study power of 80%, prevalence of exposure to gene polymorphism MBL2 of 17%. At the time of initial measurement all patients were on ART and there were no patients with KS, as evaluated in the medical records and through an interview with the patient. This research was approved by the ethics committee and the institutional review board of the Federal University of Pernambuco under case number 22428813.5.0000.5208.
DNA extraction and genotyping
Genomic DNA was extracted from leukocytes isolated from whole blood in anticoagulant solution (EDTA) using a commercial kit Wizard® Genomic DNA Purification (Promega, Madison, WI) following the manufacturer’s instructions. After extraction, all samples were measured to determine the concentration and the degree of purity of DNA using the Thermo Scientific NanoDrop 2000 spectrophotometer. All samples were diluted to the DNA concentration required for each reaction.
The promoter region (-550 and -221) was genotyped using the TaqMan system (Applied Biosystems® Genotyping Assays TaqMan), and the structural region (exon 1) genotyping was performed using the Express Sybr Greener Supermix kit (Invitrogen, USA). The melting temperature (melting temperature assay, MTA) and the melting curve profiles were obtained using the decoupling device software. The detection of polymorphisms in the codons -550, -221 and the exon 1 MBL2 gene was performed using the Rotor Gene 6000 (Corbett Research, Sydney, Australia). The three allelic variants of the MBL2 gene in codon positions 52, 54, and 57 in exon-1 were designated ‘O’, and the wild-type allele was designated ‘A’, as previously described in several studies [21, 27, 33, 34], the sequences of the primers and probes used are described in Table 1.
MBL2 gene haplotypes according to the grouping of the genotypes
The genotypes of the promoter region (-550 H/L and -221 Y/X) were grouped into the genotype of the structural region (exon 1 A/O) and categorized according to the haplotypes. We considered high expression haplotypes to be LYA/LYA, HYA/HYA and HYA/LYA. Intermediate expression haplotypes to be HYA/HXA, HYA/HYO, HYA/LXA, HYA/LYO, LXA/LXA, LYA/LXA and LYA/LYO. Low expression haplotypes to be HYO/HYO, LYO/LYO and HYO/LYO, according to some studies [27, 34, 35].
Statistical analysis
For the statistical analysis, we used Epi Info version 7.1.5 (CDC, Atlanta, GA, USA) and Rstudio version 1.0.143 (Northern Ave, Boston, MA) and considered values of p < 0.05 as statistically significant. Additionally, the values of the odds ratios (ORs) and confidence intervals (95% CIs) were used for each respective value of p. Categorical variables were analysed Chi-square test (χ2) or Fisher’s exact test, while continuous variables were analysed using Mann–Whitney and Kruskal–Wallis tests. To verify if the population was in Hardy–Weinberg equilibrium and for the construction of the haplotypical combination, we used the programme Arlequin version 3.11 (Institute of Ecology and Evolution, University of Bern).
Results
In total, 337 samples of PLWHA were analysed, of which 124 were HIV/HHV-8 coinfected, and 213 were HIV monoinfected patients. Table 2 shows the frequency of the sociodemographic variables distributed between coinfected and monoinfected patients.
Table 3 shows the median values of the clinical variables analysed in coinfected and monoinfected patients.
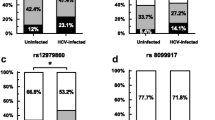
The frequencies of the alleles, genotypes and haplotypes related to -550, -221 and exon 1 polymorphisms of the MBL2 gene are shown in Table 4. According to the Hardy–Weinberg test, the groups were balanced.
The frequency of haplotypes according to expression in coinfected and monoinfected patients is described in Table 5.
Table 6 shows the frequencies of viral load of HIV and TCD4 counts according to high, intermediate and low expression levels of MBL in coinfected and monoinfected patients.
The variable last TCD4 count in coinfected patients with intermediate expression haplotype remained associated following the final model in the multivariate analysis, as is shown in Table 7 with the adjusted odds ratio (OR) and confidence intervals (95% CI).
Among the coinfected, four developed KS during the clinical course of HIV/HHV-8 coinfection and all were characterized as intermediate expression haplotypes, three were HYA/LXA and one LYA/LYO.
Discussion
The pathogenesis of HIV/HHV-8 coinfection is complex and can be influenced by viral factors; for example, HIV induces the HHV-8 lytic cycle through the activation of the RTA protein and the TAT protein, and HHV-8 interferes with HIV replication by regulating the LTR by LANA antigen [36,37,38,39,40]. However, host genetic factors such as MBL2 gene polymorphisms may also influence factors as diverse as susceptibility to HHV-8 infection, as well as impact on important factors such as HIV viral load and TCD4 counts.
The results of our research showed that the median of the first TCD4 cell count was lower in coinfected patients than monoinfected patients with a statistically significant difference. However, another study has shown that HHV-8 has little influence on HIV progression in initially asymptomatic individuals, with little repercussion in TCD4 cell count [41]. Nonetheless, considering that our study was a cross section of PLWHA, with or without HHV-8 infection, it was not possible to identify the moment of HHV-8 seroconversion, because ours was not an observational cohort study. Highlighting the importance of more specific studies with HIV/HHV-8 coinfected patients.
The median of the last TCD4 count was not statistically significant between the coinfected and monoinfected patients, corroborating with some previous studies [38, 39]. Additionally, another study did not find an association between coinfection in PLWHA with KS and the last TCD4 count [42]. The absence of an association in PLWHA with and without KS may suggest that factors other than TCD4 influence the pathogenesis of HIV/HHV-8 coinfection. Similarly, the median values of the first and last HIV viral load did not present statistically significant differences between the groups. However, the coinfected patients had a median value of the first viral load two times higher, however did not present statistically significant differences.
Some studies have shown that the order and timing of HIV and HHV-8 infection may have prognostic implications and that the incidence of KS is higher in people with HHV-8 seroconversion following HIV infection [3, 38, 43,44,45]. In the present study, the time of HIV infection as well as the time from diagnosis to the initiation of antiretroviral therapy (ART) was lower in coinfected patients, although not statistically significant. This corroborates a study that evaluated the time of seroconversion for HHV-8 and did not find an association between HHV-8 infection and HIV disease progression the time of diagnosis and the need to use ART [38], suggesting that HHV-8 does not accelerate the need to use ART.
The importance of the host genetic factors such as MBL2 gene polymorphisms and its association with infections has been studied for several viruses [17,18,19,20,21, 25,26,27]. In this study, the frequency of the alleles, genotypes and haplotypes of -550, -221 and exon 1 polymorphisms of the MBL2 gene had no association with HHV-8 infection in PLWHA. However, it is important to highlight there is very little research in this area to compare our results.
One study evaluated the -550, -221 and exon 1 polymorphisms in PLWHA and found an association between the LX/LX genotype and low expression haplotypes with HIV infection when compared with blood donors. However, the authors reported that the study population was composed of PLWHA of European ethnicity and suggested that individuals of this origin may be more susceptible to HIV infection [46]. Nonetheless, a study of Zimbabweans in South Africa found no association of these polymorphisms with HIV infection when compared to uninfected individuals [47]. Most of the individuals evaluated in the present study declared themselves mulattos, which may have contributed to the non-association with HHV-8 infection in PLWHA. The absence of an association may be related to the ethnic groups of Northeast Brazil, which have a combined mixture of the genomes of Africans, Europeans and Native Americans [48,49,50].
Simultaneous analysis of the -550, -221 and exon 1 polymorphisms can provide more complete information on the role of polymorphisms in infections since the concentrations of MBL may vary depending on the combinations of the structural and promoter polymorphisms [12,13,14]. According to Vallinoto et al. [51], these polymorphisms may be genetic markers associated with a better response in HIV-infected individuals using older antiretroviral therapy regimens. When exon 1 polymorphism was studied in isolation, the presence of the A allele was associated with the reduction of HIV viral load and the improvement of the TCD4 count in PLWHA [51]. The high expression haplotype HY, referring to codons -550 and -221, was associated with a decrease in viral load and an increase in TCD4 counts during the clinical course of monoinfected HIV patients [52].
In contrast, the -550, -221 and exon 1 polymorphisms were studied simultaneously in PLWHA and showed no impact on viral load or TCD4 count [53], and they were also not associated with viral load, TCD4 count, disease progression, or survival of a population of PLWHA from Africa who was not under antiretroviral therapy [28]. However, the present study simultaneously evaluated the three main polymorphisms of the MBL2 gene and the high, intermediate and low expression haplotypes and found an association between the HIV/HHV-8 coinfected patients who had the intermediate expression haplotype with TCD4 count when compared with patients monoinfected by HIV.
Considering the ability of MBL to bind to the HIV-1 gp120 glycoprotein and mediating phagocytosis or activating the complement system [54,55,56], our results demonstrate that coinfected patients who present the intermediate expression haplotype of MBL2 gene may have the last TCD4 count < 350 cells/mm3. It is important to note that among the coinfected patients, the four who developed KS also had intermediate expression MBL haplotypes, three with HYA/LXA and one with LYA/LYO, suggesting that these haplotypes may interfere with the clinic development of SK in HIV/HHV-8 coinfected patients. It should also be emphasized that none of the coinfected patients who presented the high expression haplotypes of MBL2 gene developed KS during clinical follow-up.
The role of MBL2 gene polymorphisms is still a subject that needs to be further studied both in HHV-8 infected and HIV/HHV-8 coinfected patients, mainly in other populations of regions endemic to HHV-8, due to the importance of MBL protein in the innate immune system. Host genetic factors such as -550, -221 and exon 1 polymorphisms cause defects in the polymerization of MBL protein, resulting in a functional deficiency and/or in low serum levels of this protein that can influence the individual susceptibility to various viral infections. Therefore, these polymorphisms can be related to the coinfection and/or to the development clinical manifestations caused by HHV-8, as the KS, especially in HIV/HHV-8 coinfected patients who present the intermediate expression haplotypes of MBL.
References
Gantt S, Casper C. Human herpesvirus 8-associated neoplasms: the roles of viral replication and antiviral treatment. Curr Opin Infect Dis. 2011;24:295–301.
Goncalves PH, Ziegelbauer J, Uldrick TS, Yarchoan R. Kaposi sarcoma herpesvirus-associated cancers and related diseases. Curr Opin HIV AIDS. 2017;12:47–56.
Rohner E, Wyss N, Trelle S, Mbulaiteye SM, Egger M, Novak U, et al. HHV-8 seroprevalence: a global view. Syst Rev. 2014;3:1–7.
Dittmer DP, Damania B. Kaposi sarcoma—associated herpesvirus: immunobiology, oncogenesis, and therapy. J Clin Investig. 2016;126:3165–75.
Broccolo F, Din CT, Viganò MG, Rutigliano T, Esposito S, Lusso P, et al. HHV-8 DNA replication correlates with the clinical status in AIDS-related Kaposi’s sarcoma. J Clin Virol. 2016;78:47–52.
Paoli PDE, Carbone A. Kaposi’s sarcoma herpesvirus: twenty years after its discovery. Eur Rev Med Pharmacol Sci. 2016;20:1288–94.
Laurent C, Meggetto F, Brousset P. Human herpesvirus 8 infections in patients with immunodeficiencies. Hum Pathol. 2008;39:983–93.
Aresté C, Blackbourn DJ. Modulation of the immune system by Kaposi’s sarcoma-associated herpesvirus. Trends Microbiol. 2009;17:119–29.
Lee H-R, Amatya R, Jung JU. Multi-step regulation of innate immune signaling by Kaposi’s sarcoma-associated herpesvirus. Virus Res. 2015;209:39–44.
Brulois K, Jung JU. Interplay between Kaposi’s sarcoma-associated herpesvirus and the innate immune system. Cytokine Growth Factor Rev. 2014;25:597–609.
Mason CP, Tarr AW. Human lectins and their roles in viral infections. Molecules. 2015;20:2229–71.
Eisen DP, Minchinton RM. Impact of mannose-binding lectin on susceptibility to infectious diseases. Clin Infect Dis. 2003;37:1496–505.
Worthley DL, Bardy PG, Mullighan CG. Mannose-binding lectin: biology and clinical implications. Intern Med J. 2005;35:548–55.
Ip WK, Takahashi K, Ezekowitz RA, Stuart LM. Mannose-binding lectin and innate immunity. Immunol Rev. 2009;230:9–21.
Hartz A, Pagel J, Humberg A, Preuss M, Schreiter L, Rupp J, et al. The association of mannose-binding lectin 2 polymorphisms with outcome in very low birth weight infants. PLoS ONE. 2017;12(5):e0178032.
Bautista-Rodriguez C, Launes C, Jordan I, Andres M, Arias MT, Lozano F, et al. Mannose-binding lectin-deficient genotypes as a risk factor of pneumococcal meningitis in infants. PLoS ONE. 2017;12(5):e0178377.
Guimaraes V, Guimaraes R, Brandao L, Baldez da Silva MFPT, Milanese M, Segat L, et al. Association between MBL2 gene functional polymorphisms and high-risk human papillomavirus infection in Brazilian women. Hum Immunol. 2008;69:273–8.
Alves Pedroso ML, Boldt ABW, Pereira-Ferrari L, Steffensen R, Strauss E, Jensenius JC, et al. Mannan-binding lectin MBL2 gene polymorphism in chronic hepatitis C: association with the severity of liver fibrosis and response to interferon therapy. Clin Exp Immunol. 2008;152:258–64.
Seppänen M, Lokki M-L, Lappalainen M, Hiltunen-Back E, Rovio AT, Kares S, et al. Mannose-binding lectin 2 gene polymorphism in recurrent herpes simplex virus 2 infection. Hum Immunol. 2009;70:218–21.
Friborg JT, Jarrett RF, Koch A, Garred P, Freeland JML, Andersen A, et al. Mannose-binding lectin genotypes and susceptibility to epstein-barr virus infection in infancy. Clin Vaccine Immunol. 2010;17:1484–7.
Halla MC, do Carmo RF, Silva Vasconcelos LR, Pereira LB, Moura P, de Siqueira ERF, et al. Association of hepatitis C virus infection and liver fibrosis severity with the variants alleles of MBL2 gene in a Brazilian population. Hum Immunol. 2010;71:883–7.
Brudner M, Karpel M, Lear C, Chen L, Yantosca LM, Scully C, et al. Lectin-dependent enhancement of Ebola virus infection via soluble and transmembrane C-type lectin receptors. PLoS ONE. 2013;8(4):e60838.
Egli A, Schäfer J, Osthoff M, Thiel S, Mikkelsen C, Rauch A, et al. Low levels of Mannan-binding lectin or ficolins are not associated with an increased risk of cytomegalovirus disease in HIV-infected patients. PLoS ONE. 2013;8(1):e51983.
Xu H, Zhao M, Wan T, Song G, He J, Chen Z. Association between Mannose-binding lectin gene polymorphisms and hepatitis B virus infection: a meta-analysis. PLoS ONE. 2013;8(10):e75371.
Yanagisawa K, Ogawa Y, Uchiumi H, Gohda F, Mawatari M, Ishizaki T, et al. Gene polymorphisms of mannose-binding lectin confer susceptibility to Pneumocystis pneumonia in HIV-infected patients. J Infect Chemother. 2015;21:769–75.
Erdemir G, Ozkan TB, Ozgur T, Budak F, Kilic SS, Onay H. Mannose-binding lectin gene polymorphism and chronic hepatitis B infection in children. Saudi J Gastroenterol. 2015;21:84–9.
Figueiredo GG, Cezar RD, Freire NM, Teixeira VG, Baptista P, Cordeiro M, et al. Mannose-binding lectin gene (MBL2) polymorphisms related to the mannose-binding lectin low levels are associated to dengue disease severity. Hum Immunol. 2016;77:571–5.
Zinyama-Gutsire RBL, Chasela C, Kallestrup P, Rusakaniko S, Christiansen M, Ngara B, et al. HIV-1 disease progression and survival in an adult population in Zimbabwe: Is there an effect of the Mannose binding lectin deficiency? Omics J Integr Biol. 2015;19:542–52.
Casper C. New approaches to the treatment of human herpesvirus 8-associated disease. Rev Med Virol. 2008;18:321–9.
Dow DE, Cunningham CK, Buchanan AM. A review of human herpesvirus 8, the Kaposi’s sarcoma-associated herpesvirus, in the pediatric population. J Pediatr Infect Dis Soc. 2014;3:66–76.
Munawwar A, Singh S. Human herpesviruses as copathogens of HIV infection, their role in HIV transmission, and disease progression. J Lab Physicians. 2016;8:5.
de Oliveira Mendes Cahú GG, Morais VMS, Lopes TRR, da Silva DM, Tozetto-Mendoza TR, Pannuti CS, et al. Prevalence of human herpesvirus 8 infection in people living with HIV/AIDS in Pernambuco, Brazil. J Med Virol. 2016;88:2016–20.
Hladnik U, Braida L, Boniotto M, Pirulli D, Gerin F, Amoroso A, et al. Single-tube genotyping of MBL-2 polymorphisms using melting temperature analysis. Clin Exp Med. 2002;2:105–8.
Vasconcelos LRS, Fonseca JPL, do Carmo RF, de Mendonça TF, Pereira VRA, Lucena-Silva N, et al. Mannose-binding lectin serum levels in patients with leprosy are influenced by age and MBL2 genotypes. Int J Infect Dis. 2011;15:551–7.
Garred P, Larsen F, Madsen HO, Koch C. Mannose-binding lectin deficiency—revisited. Mol Immunol. 2003;40:73–84.
Varthakavi V, Smith RM, Deng H, Sun R, Spearman P. Human immunodeficiency virus type-1 activates lytic cycle replication of Kaposi’s sarcoma-associated herpesvirus through induction of KSHV Rta. Virology. 2002;297:270–80.
Zeng Y, Zhang X, Huang Z, Cheng L, Yao S, Qin D, et al. Intracellular Tat of human immunodeficiency virus type 1 activates lytic cycle replication of Kaposi’s sarcoma-associated herpesvirus: role of JAK/STAT signaling. J Virol. 2007;81:2401–17.
Batista MD, Ferreira S, Sauer MM, Tomiyama H, Giret MTM, Pannuti CS, et al. High human herpesvirus 8 (HHV-8) prevalence, clinical correlates and high incidence among recently HIV-1-infected subjects in São Paulo, Brazil. PLoS ONE. 2009;4:2–6.
Hesamizadeh K, Keyvani H, Bokharaei-Salim F, Monavari SH, Esghaei M, Jahanbakhsh Sefidi F. Molecular epidemiology of Kaposi’s sarcoma-associated herpes virus, and risk Factors in HIV-infected patients in Tehran, 2014. Iran Red Crescent Med J. 2016;18:e32603.
Begré L, Rohner E, Mbulaiteye SM, Egger M, Bohlius J. Is human herpesvirus 8 infection more common in men than in women? Int J Cancer. 2016;139:776–83.
Ait-Arkoub Z, Robert-Visse C, Calvez V, Costagliola D, Autran B, Candotti D, et al. No influence of human herpesvirus 8 infection on the progression of HIV-1 infection in initially asymptomatic patients. AIDS. 2003;17:1394–6.
Tozetto-Mendoza TR, Ibrahim KY, Tateno AF, de Oliveira CM, Sumita LM, Sanchez MCA, et al. Genotypic distribution of HHV-8 in AIDS individuals without and with Kaposi sarcoma. Medicine. 2016;95:e5291.
Renwick N, Halaby T, Weverling GJ, Dukers NH, Simpson GR, Coutinho RA, et al. Seroconversion for human herpesvirus 8 during HIV infection is highly predictive of Kaposi’s sarcoma. Aids. 1998;12:2481–8.
Jacobson LP, Jenkins FJ, Springer G, Munoz A, Shah KV, Phair J, et al. Interaction of human immunodeficiency virus type 1 and human herpesvirus type 8 infections on the incidence of Kaposi’s sarcoma. J Infect Dis. 2000;181:1940–9.
Volkow P, Jacquemin B, Zinser JW, Prez-Padilla R. Revisión histórica del sarcoma de Kaposi en la era pre-TARAA (terapia antirretroviral altamente activa): evolución con diferentes esquemas de quimioterapia y remisión con el uso de ganciclovir. Gac Med Mex. 2016;152:96–102.
da Silva GK, Guimarães R, Mattevi VS, Lazzaretti RK, Sprinz E, Kuhmmer R, et al. The role of mannose-binding lectin gene polymorphisms in susceptibility to HIV-1 infection in southern Brazilian patients. Aids. 2011;25:411–8.
Zinyama-Gutsire R, Chasela C, Madsen HO, Rusakaniko S, Kallestrup P, Christiansen M, et al. Role of mannose-binding lectin deficiency in HIV-1 and schistosoma infections in a rural adult population in Zimbabwe. PLoS ONE. 2015;10:1–23.
Alves-Silva J, da Silva Santos M, Guimarães PEM, Ferreira ACS, Bandelt H-J, Pena SDJ, et al. The ancestry of Brazilian mtDNA lineages. Am J Hum Genet. 2000;67:444–61.
Da Cruz HLA, Da Silva RC, Segat L, De Carvalho MSZMG, Brandão LAC, Guimarães RL, et al. MBL2 gene polymorphisms and susceptibility to tuberculosis in a northeastern Brazilian population. Infect Genet Evol. 2013;19:323–9.
Sandoval JR, Madsen HO, De Stefano G, Descailleaux-Dulanto J, Velazquez-Reinoso M, Pique C, et al. Extreme high prevalence of a defective mannose-binding lectin (MBL2) genotype in native South American West Andean populations. PLoS ONE. 2014;9(10):e108943.
Vallinoto ACR, Menezes-Costa MR, Alves AEM, Machado LFA, Azevedo VN, De Souza LLB, et al. Mannose-binding lectin gene polymorphism and its impact on human immunodeficiency virus 1 infection. Mol Immunol. 2006;43:1358–62.
Vallinoto AC, Muto NA, Alves AE, Machado LF, Azevedo VN, Souza LL, et al. Characterization of polymorphisms in the mannose-binding lectin gene promoter among human immunodeficiency virus 1 infected subjects. Mem Inst Oswaldo Cruz. 2008;103:645–9.
Catano G, Agan BK, Kulkarni H, Telles V, Marconi VC, Dolan MJ, et al. Independent effects of genetic variations in mannose-binding lectin influence the course of HIV disease: the advantage of heterozygosity for coding mutations. J Infect Dis. 2008;198:72–80.
Ji X, Gewurz H, Spear GT. Mannose binding lectin (MBL) and HIV. Mol Immunol. 2005;42:145–52.
Eisen S, Dzwonek A, Klein NJ. Mannose-binding lectin in HIV infection. Future Virol. 2008;3:225–33.
Teodorof C, Divakar S, Soontornniyomkij B, Achim CL, Kaul M, Singh KK. Intracellular mannose binding lectin mediates subcellular trafficking of HIV-1 gp120 in neurons. Neurobiol Dis. 2014;69:54–64.
Authors’ contributions
VMSM designed the study, did all the experimental work, analyzed the data statistically, interpretation the data and drafted the manuscript. ELSL participated in the genetic experiments and revised the manuscript critically for genetic content. GGOMC collected the samples and acquired data. TRRL collected the samples, acquired data and revised the manuscript critically. JPG acquired data and revised the manuscript. MTCM revised the manuscript critically for genetic content. MRCDC obtained the funding and revised the manuscript critically for important intellectual content. All the authors read and approved the final manuscript.
Acknowledgements
The authors thank all patients who accepted to participate this research and technical support from the Virology Laboratory of the Tropical Medicine Institute (LIM-52-IMT) of the University of São Paulo for the realization of HHV-8 serology.
Competing interests
The authors declare that they have no competing interests.
Ethical approval
The research protocol was approved by the Research Ethics Committee of the Federal University of Pernambuco (Number: 22428813.5.0000.5208).
Funding
The authors received no specific funding for this work.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
de Morais, V.M.S., de Lima, E.L.S., Cahú, G.G.d.M. et al. MBL2 gene polymorphisms in HHV-8 infection in people living with HIV/AIDS. Retrovirology 15, 75 (2018). https://doi.org/10.1186/s12977-018-0456-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12977-018-0456-8