Abstract
Background
Despite exercising in cool environments, ice hockey players exhibit several dehydration risk factors. Individualized fluid plans (IFPs) are designed to mitigate dehydration by matching an individual’s sweat loss in order to optimize physiological systems and performance.
Methods
A randomized control trial was used to examine IFP versus ad libitum fluid ingestion on hydration in 11 male minor professional ice hockey players (mean age = 24.4 ± 2.6 years, height = 183.0 ± 4.6 cm, weight = 92.9 ± 7.8 kg). Following baseline measures over 2 practices, participants were randomly assigned to either control (CON) or intervention (INT) for 10 additional practices. CON participants were provided water and/or carbohydrate electrolyte beverage to drink ad libitum. INT participants were instructed to consume water and an electrolyte-enhanced carbohydrate electrolyte beverage to match sweat and sodium losses. Urine specific gravity, urine color, and percent body mass change characterized hydration status. Total fluid consumed during practice was assessed.
Results
INT consumed significantly more fluid than CON (1180.8 ± 579.0 ml vs. 788.6 ± 399.7 ml, p = 0.002). However, CON participants replaced only 25.4 ± 12.9% of their fluid needs and INT 35.8 ± 17.5%. Mean percent body mass loss was not significantly different between groups and overall indicated minimal dehydration (<1.2% loss). Pre-practice urine specific gravity indicated CON and INT began hypohydrated (mean = 1.024 ± 0.007 and 1.024 ± 0.006, respectively) and experienced dehydration during practice (post = 1.026 ± 0.006 and 1.027 ± 0.005, respectively, p < 0.001). Urine color increased pre- to post-practice for CON (5 ± 2 to 6 ± 1, p < 0.001) and INT (5 ± 1 to 6 ± 1, p < 0.001).
Conclusions
Participants consistently reported to practice hypohydrated. Ad libitum fluid intake was not significantly different than IFP on hydration status. Based on urine measures, both methods were unsuccessful in preventing dehydration during practice, suggesting practice-only hydration is inadequate to maintain euhydration in this population when beginning hypohydrated.
Similar content being viewed by others
Background
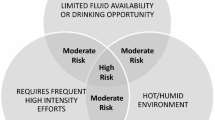
Ice hockey is a fast-paced, equipment-intensive sport played in a cold environment. Athletes perform high intensity, short duration bouts of quick accelerations and decelerations with changes in direction during on-ice shifts lasting 45–90 s [1]. Players rely on both anaerobic force production and aerobic efficiency [2]. It is estimated that players’ on-ice oxygen consumption reaches 80% of their \( \dot{\mathrm{V}} \)O2max [3]. This type of high intensity exercise increases plasma lactate concentrations, which correlates with increased plasma osmolality and plasma sodium concentration [4] and is known to increase vasopressin [5]. In response to these physiological changes, individuals will voluntarily take in more water after intense exercise [6]. Voluntarily consuming more fluid during exercise can be complicated by factors such as fluid availability, rest time, and other sport dynamics [7]. Further, during intense exercise gastric emptying slows down, causing fluid that is consumed to remain in the stomach [8]. An individual may then limit voluntary intake due to gastrointestinal discomfort. Inadequate fluid consumption, leading to hypohydration, will limit the amount of fluid available to maintain physiological function (e.g. heart rate and blood pressure) during exercise.
The equipment and cold environment in ice hockey also influences hydration in athletes. The protective equipment required in ice hockey increases core body temperature, sweat loss, and plasma lactate; thus, resulting in decreased power output and compromising fluid balance [9, 10]. Athletes in cool environments are often unable to replace enough fluid to counter sweat losses [9, 11,12,13]. In part, this is due to a blunted thirst response seen with moderate-intense (70% \( \dot{\mathrm{V}} \)O2max) exercise [14]. Individuals reduce the amount of fluid they consume, resulting in voluntary dehydration. Additional confounding factors for fluid intake in the cold include cold-induced diuresis and an increase in insensible sweat and respiratory fluid loss [15, 16].
In contrast to voluntary dehydration, some individuals consume more fluid than necessary and gain weight by the end of exercise, even in the cold [14]. To discourage excessive or inadequate fluid consumption, the American College of Sports Medicine and National Athletic Trainers’ Association recommend individualized fluid plans (IFPs) [7, 17]. IFPs use an individual’s distinct sweat rate to guide adequate fluid replacement during exercise and maintain euhydration. There is some speculation to how 2% body mass (BM) loss may impact an individual’s health and performance, with some evidence that there is no detriment to performance [8, 18] and others showing aerobic and anaerobic impairment [19, 20]. Regardless, it is generally recommended to maintain less than 2% loss from pre- to post-exercise [7, 17]. In clinical settings, 2% loss may not represent 2% from a euhydrated baseline BM. For instance, an athlete beginning practice hypohydrated who loses 2% during practice is at a larger deficit by post-practice. This is an important consideration because many ice hockey players begin activity hypohydrated [11,12,13, 21, 22].
The environmental conditions, complex physical demands, and protective equipment associated with ice hockey heightens the importance of proper hydration to maintain health and performance. Most research examining hydration in ice hockey is limited to 1–4 days [11, 12, 22] and utilizes junior and collegiate players [9, 11,12,13]. Often, fluid intake did not match sweat rate, resulting in dehydration [9, 11, 12, 22]. Existing literature on the effects of matching fluid consumption to sweat rate is primarily in controlled laboratory settings [8, 18]. Field studies investigating the effectiveness of IFPs versus ad libitum are limited [21, 23] and have not included sweat sodium concentration ([Na+]). The purpose of this study was two-fold: 1) to implement and determine efficacy of IFPs vs ad libitum fluid consumption in the field setting of an ice hockey team and 2) to examine fluid and electrolyte balance in minor professional ice hockey players across multiple practices. We hypothesized that providing IFPs would improve pre- and post-practice hydration measures compared to ad libitum. We also hypothesized that players in the ad libitum group would report to practices hypohydrated and remain hypohydrated at post-exercise.
Methods
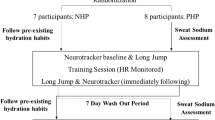
We utilized a randomized controlled design to compare 2 experimental conditions: control (CON) and intervention (INT) on hydration status. Our main outcome measures were urine specific gravity (Usg), urine color (Ucol), urine sodium concentration ([Na+]), urine potassium concentration ([K+]), and percent body mass change (%BM). We also assessed fluid volume (Fvol) and sodium ingestion. Data collection occurred at 10 practices over 3 months during the middle of the hockey season (November – January) to avoid pre-season physiological changes and allow rosters to be set. To minimize game effects and differences in practice intensity, no data collection was scheduled on days immediately before or after a game.
Participants
Twenty-one male minor professional ice hockey players consented to participate. We experienced attrition due to trades, call-ups, and voluntary cessation, yielding 11 participants. Three participants had incomplete data; therefore, we conducted analysis on a total of 8 participants (2 forwards, 4 defensemen, and 2 goalies; mean age = 24.4 ± 2.6 years, height = 183.0 ± 4.6 cm, weight = 92.9 ± 7.8 kg, and body fat = 14.0 ± 3.8%). Participants were required to be in good general health. Participants were free of cardiovascular, respiratory, and metabolic disorders; fluid and electrolyte balance disorders; and gastrointestinal and swallowing disorders. Prior to participation, participants signed an informed consent form approved by the Institutional Review Board at the University of South Carolina (#HSA4821). Participants were asked to maintain normal levels of physical activity, maintain a normal state of hydration, and avoid changes in caffeine consumption and dehydration-inducing substances (e.g., alcohol) during the course of this study.
Baseline measures were assessed over 2 practices. Participants’ pre- and post-practice BM, Usg, Ucol, and urine [Na+] and [K+] were measured. Practice sweat [Na+] and sweat rate were also measured. At the end of baseline, participants were randomly assigned to one of the 2 conditions (CON or INT). Total Fvol consumed was measured during practice by providing individual water bottles identifiable by the player’s assigned team number. To minimize crossover between participants and non-participants, participants’ bottles were a different color and located separately from non-participants’ bottles.
The CON condition required participants maintain normal hydration habits (i.e., drinking ad libitum) during practice. Participants received either one water (W), one commercially available carbohydrate-electrolyte beverage (CEB; Powerade, The Coca-Cola Company, Atlanta, GA) or one of each, depending on individual preference. CON participants were not aware of their individual needs (based on sweat rate and [Na+]) or the INT participants’ fluid needs.
Each INT participant was provided individualized recommendations regarding Fvol to consume per hour of practice that corresponded to his baseline sweat rate and sweat [Na+]. The INT group received one bottle with W and one electrolyte-enhanced CEB (E-CEB). For example, if a participant’s baseline sweat rate = 2 L/h and his sweat [Na+] = 1000 mg/L/h, an E-CEB was made to match the sodium loss. The E-CEB contained a measured amount of commercially available electrolyte mixture (Gatorlytes, Gatorade Company, Inc., Chicago, IL; sodium = 780 mg/packet) combined with the CEB (sodium = 150 mg/L). In the example, the participant would be given 1 L of CEB mixed with 1 Gatorlyte packet for a total of 930 mg of sodium. He would also be provided 1 L of water. Prior to practice starting, the player was verbally recommended to consume both bottles of fluid during practice and within 1 h (average practice length). To minimize interference during practice, no verbal instructions were given to players during practice. Participants were allowed to consume more than recommended. All bottles were continuously checked throughout practice and refilled, as necessary, with a pre-measured fluid amount. Fluid remaining in bottles at the end of practice was measured using a graduated cylinder and recorded. Samples were taken from each CEB to determine beverage [Na+]. Sodium concentration was corrected for participant’s ingested Fvol to determine total sodium ingested.
Instruments and protocols
Hydration indices
Hydration status was characterized using a Ucol chart (Human Kinetics, Champaign, IL), Usg (refractometer model REF 312, Atago Company Ltd., Tokyo, Japan), and %BM (Tanita TBF-300A, Tanita Corporation, Tokyo, Japan). Dehydration was defined as >1% BM loss from pre-practice weight, a Usg ≥ 1.020, and/or Ucol shade ≥4 [7].
Electrolytes
Sweat and urine electrolytes were assessed using ion-selective electrode analysis (EasyLyte® Na+/K+ electrolyte analyzer, Medica, Bedford, MA). Normal urine [Na+] was defined as 40–220 mmol/L and normal urine [K+] as 25–120 mmol/L. Participants were considered to be in a state of sodium conservation when urine [Na+] < 40 mmol/L.
Sweat
Prior to the participant dressing for practice, a sweat patch was applied to the forearm. Researchers wore rubber gloves, cleaned the forearm area with alcohol and placed a 3 × 3 sterile gauze pad on the area. The gauze pad was held in place with a water resistant clear adhesive patch (SEAL-TIGHT® Shower Patch™). Immediately after practice, researchers removed patches and sweat was squeezed into a 2 ml microtube, closed, placed on ice, and set aside to be analyzed.
Environment
Temperature and relative humidity were monitored with an environmental monitor (QuestTemp-34, QuestTechnology, Oconomowoc, WI) to determine practice arena environment.
Body composition
On two occasions, once at baseline (November) and once at the end of the data collection (January), body fat % was calculated using a 7-site (i.e., chest, mid-axillary, triceps, subscapular, abdomen, suprailiac, and thigh) skin fold procedure with Lange skinfold calipers (Beta Tehnology Inc., Cambridge, MD).
Statistical analysis
We used IBM SPSS 22 (IBM, Inc., Chicago, IL) for all analyses with a significance level of p < 0.05. Descriptive statistics were calculated for all dependent measures. A 2 (condition) × 9 (practice days) repeated measures ANOVA was utilized to determine changes in dependent measures. Day 2 was excluded due to a team function preventing post-practice data collection. One-way ANOVAs and paired sample t-tests were used to determine differences in demographics, baseline measures, hydration and electrolytes, Fvol, and sodium consumed between and within CON and INT. Due to missing data, only 7 practice days were used to analyze urine [Na+] and [K+]. Post-hoc power analysis using recommended versus actual Fvol and pre- to post-Usg indicated a statistical power > 0.70.
Results
There were no significant differences in age, baseline height, weight, or body fat % between groups (Table 1). Body mass and body fat % did not significantly change from baseline to the end of the data collection period (3 months). Mean practice time for 10 days = 68.4 ± 14.8 min (range = 50–78 min). Mean arena temperature = 12.6 °C and relative humidity = 47%. Baseline mean sweat rate (3.4 ± 1.4 L/h) and sweat [Na+] (63.1 ± 17.1 mmol/L; 145.0 ± 39.3 mg/L) were not significantly different between conditions. Sweat rate and [Na+] did not significantly differ during practices between CON (2.1 ± 0.5 L/h and 54.3 ± 22.3 mmol/L) and INT (2.5 ± 0.9 L/h and 70.2 ± 19.5 mmol/L).
On average, the INT maintained <1% BM loss during practice and there was no significant difference from CON (Table 2). Mean Usg and Ucol indicated participants in both groups were hypohydrated before practice and experienced significant dehydration during practice (Table 2). There were no significant differences between CON and INT Usg at pre- or post-practices for any days.
Overall mean total fluid, CEB, and sodium intake was significantly higher in the INT (Table 3). Both CON and INT consumed significantly less fluid and sodium than recommended based on sweat rate and [Na+] (Table 3). CON participants replaced 25.4 ± 12.9% of their fluid needs and INT 35.8 ± 17.5%. Looking at individual data, no participant consumed fluid or sodium on any practice day matching recommended intake. When corrected for BM, fluid was consumed at a rate of 7.5 ml/kg/h for CON and 11.0 ml/kg/h for INT.
Urine [Na+] did not significantly change from pre- to post-practice for CON or INT and there was no significant differences between conditions (Table 2). In the INT, participants reported 23% of the time with a urine [Na+] < 40 mmol/L (mean = 23.2 ± 2.5 mmol/L) and 24% ended practice in a similar state (18.9 ± 14.6 mmol/L). Similar results were found for the CON, with 26% reporting with a low urine [Na+] at pre-practice (29.5 ± 7.6 mmol/L) and 31% at post-practice (27.4 ± 9.0 mmol/L). Post-practice urine [K+] was significantly greater than pre- for both conditions (Table 2). Only once (4% of the time) did an INT participant arrive to practice with urine [K+] < 25 mmol/L (22.2 mmol/L), compared to18.5% of the time in the CON (17.1 ± 5.6 mmol/L). No participant had low urine [K+] post practice. High urine [K+] (>120 mmol/L) occurred 16% of the time within CON (156.2 ± 19.1 mmol/L) and 12.5% in INT (164.0 ± 44.7 mmol/L).
Three of four CON participants regularly consumed only W during practice. These 3 participants had significantly higher sweat [Na+] than the fourth CON participant (136.4 ± 13.7 versus 53.7 mmol/L, t(2) = 17.3, p = 0.003, d = −6.0) and more frequently their urine [Na+] was <40 mmol/L (31% versus 14%). Despite consuming an E-CEB, the 2 INT participants with higher sweat [Na+] most frequently had urine [Na+] < 40 mmol/L (33%) compared to the other 2 INT participants (0.8%).
Discussion
We assessed fluid and sodium balance in minor professional ice hockey players and examined these variables after implementing IFPs. We found players reported to practice hypohydrated and experienced negative fluid and sodium balance during practice. Once players in the INT group were informed of their IFP, participants consumed more fluids and electrolytes than the players drinking ad libitum. Despite increased fluid ingestion, there were no significant differences between conditions for hydration and sodium measures. Based on urinary hydration measures, the IFP was unsuccessful in offsetting fluid loss during ice hockey practice. Further, IFP participants were unable to consume the recommended Fvol.
Fluid and sodium balance
Despite playing in cool environments, ice hockey players are susceptible to dehydration [9, 11,12,13, 22], increased core temperature [9], and sodium depletion [11,12,13]. Our mean sweat rates were higher than collegiate (0.8 L/h) [9] and elite junior ice hockey players (1.5 ± 0.1 L/h and 1.8 ± 0.1 L/h) [12, 13] yet similar to professional athletes in warmer environments [24, 25]. Similarly, our participants’ mean sweat [Na+] was comparable to other ice hockey studies and professional football [11,12,13, 24]. Despite the higher sweat rates, we observed BM losses similar to collegiate practices (−1.1%) [9], juniors practice (−0.8%) [12], and a juniors game (−1.3%) [11]. In order to maximize performance and maintain health, it is advisable to develop a hydration strategy to limit fluid losses to less than 2%.
We did not expect to find our IFP participants repeatedly arriving to practice hypohydrated. However, our results are consistent with previous ice hockey studies [11, 12, 22] as well as other sports [24]. Pre-exercise Usg has not correlated with ad libitum fluid consumption during activity [11], having very little effect on hydration-related hormonal and vascular responses during exercise when fluid is available [26]. In other words, athletes observed in training and competition do not tend to consume more fluids when beginning exercise hypohydrated. It is important to note using %BM calculations as the only hydration measure may not accurately portray an individual’s fluid balance and can underestimate actual hypohydration level. This concept is reflected in our study, and supported by Cleary et al. [21], where participants experienced <2%BM loss with an IFP, but frequently began practice hypohydrated and experienced significant dehydration during activity. To prevent dehydrating during activity and chronic hypohydration, athletes need individualized hydration monitoring and fluid replacement recommendations that extend beyond practice only.
Urine electrolyte excretion can vary depending on diet. Although we were unable to determine dietary influences, the frequency of low urine [Na+] among those only consuming water and those with higher sweat [Na+] suggests these individuals were often in a state of sodium conservation. This is supported by the increase in urine [K+] from pre- to post-practice. There are few field studies examining urine electrolytes, but our results are consistent with professional American football players completing 2-a-day practices in hot environments [27]. It is possible the elevated post-practice potassium was a result of potassium leaking from working and/or damaged muscle during intense exercise. However, to maintain electrolyte balance, increased urine potassium often accompanies decreased urine sodium as the kidneys use sodium to retain water during hypohydration [28]. In addition to matching sweat rates, individuals with high sodium losses or low sodium intake (e.g., low-sodium diet) receive more specific sodium recommendations that can come with an IFP.
Individualized fluid plans
Voluntary dehydration commonly occurs in athletes [9, 11,12,13] despite unlimited access to water. Individuals who plan to purposefully consume more fluid during exercise increase ad libitum consumption compared to those without purposeful intentions [29]. Using a similar theoretical approach, we informed INT participants on individual baseline data and gave target Fvol to meet during practice. This is in contrast to adolescent volleyball players provided metered IFPs to match fluid loss [21] and runners provided designated water stations with specific fluid requirements throughout a 20-km race [23]. Though fluid consumption increased, to our surprise, IFP participants continued to experience dehydration, suggesting inadequate fluid absorption during practice. The two most significant factors affecting fluid absorption rate and availability are gastric emptying and intestinal absorption [30]. Some INT participants were provided E-CEBs to match higher sweat [Na+], which increased beverage [Na+] and osmolarity. Research has shown gastric emptying is not affected by CEB [Na+] or osmolarity [31]. Therefore, it is unlikely beverage composition attenuated fluid absorption and negatively affected post-practice hydration measures.
Two factors that may have hindered fluid absorption are practice length and intensity. Mean practice length in the present study was similar to Palmer et al. [12], but shorter than other hockey studies [9, 13]. During a 60 min cycling time-trial in which participants replaced 100% of sweat losses, of the ingested 1.5 L, 0.3 L remained in the stomach and 0.2 L was urinated out following exercise. Only 1.02 L was available for fluid replacement [8]. If gastric emptying was slowed due to the high practice intensity, our participants may have voluntarily limited fluid consumption in fear of causing gastrointestinal discomfort. Ingesting fluid volumes, even water, matching 100% sweat loss may induce feelings of fullness and bloating [18]. We believe the short practice length and high intensity made it difficult for participants to absorb and utilize some of the ingested fluid, and may partially explain the similar post-practice hydration measures between groups.
Limitations and future research
A unique aspect of our study is the cross-sectional look at mid-season hydration rather than a one day snap shot or several days over one week. Unfortunately, because of this approach we experienced high participant attrition over the 3 months. Though similar to previous research [10], our sample size is a limitation. The higher mean baseline sweat rate compared to mean practice sweat rates is likely due to the conditioning activity at the end of practices earlier in the season compared to practices later in the season. Using a one-site local sweat patch is a limitation because of the tendency to overestimate sweat [Na+]. Whole-body wash down is a more valid technique to assess sweat [Na+]. Using urine [Na+] and [K+] only allows for generalizations on electrolyte balance. Measuring plasma electrolytes and fluid regulatory hormones (e.g., aldosterone) is optimal, but collecting blood samples was impractical in this field setting. Measuring plasma volume or osmolality would provide a more accurate indication of hydration status. However, one time urine collection (i.e., pre-practice) to determine hydration status, although less valid, is a common, practical tool for clinicians. We did not encourage participants to void urine upon waking and prior to coming to practice. Morning Usg measures are often skewed high. Obtaining a subsequent urine sample would provide a more accurate Usg measure. Practices occurred mid-morning and we assume some participants voided before coming to practice. The purpose of this study was to examine an IFP during practice; therefore, we did not provide participants with recommendations for post-practice hydration to attenuate losses. Only examining hydration and fluid during practice limited our ability to identify daily nutritional factors that may positively or negatively affect hydration in this population. Future research should consider dietary analysis and 24 h urine collection to better describe these individual’s hydration state. We did not formally measure gastrointestinal discomfort. No participant reported emesis or gastrointestinal distress during the IFP. However, a number of participants verbally reported during baseline testing that they generally did not consume CEB during practice due to gastrointestinal symptoms (i.e., fullness and bloating). Future studies are warranted to examine gastrointestinal distress with IFPs. Finally, we did not control for individual exercise intensity during practice, which may have affected Fvol.
Interestingly, one participant in the INT group, a goalie, reported a history of exercise associated muscle cramps, dehydration, and fatigue during long games, particularly in arenas in the Southeast. Individual results from this participant showed he had the highest sweat rate, sweat [Na+], fluid ingestion and frequently lower urine [Na+] compared to any other participant. Research should continue to examine risk factors (e.g., equipment, environment, travel, etc.) and symptoms of fluid and thermoregulatory imbalance in ice hockey players.
Conclusions
Our primary purpose was to determine if an IFP would improve hydration status compared to ad libitum fluid intake among male, minor professional ice hockey players. Despite increased fluid intake and attenuated BM loss, IFPs did not improve hydration status during mid-season ice hockey practices. When developing IFPs, clinicians should consider individuals completing a short, high intense activity may be unable to consume enough fluid to match losses. Since participants reported to practice hypohydrated, it is likely daily hydration behaviors were inadequate to maintain fluid balance and not influenced by the IFP. Members of the sports medicine team should monitor hydration status and educate ice hockey players on proper pre- and post-activity hydration to maintain daily fluid balance and limit negative dehydration induced performance and health effects during activity.
Abbreviations
- BM:
-
Body mass
- CEB:
-
Carbohydrate electrolyte beverage
- CON:
-
Control
- E-CEB:
-
Electrolyte enhanced carbohydrate electrolyte beverage
- Fvol:
-
Fluid volume
- IFP:
-
Individual fluid plans
- INT:
-
Intervention
- Ucol:
-
urine color
- Usg:
-
urine specific gravity
- \( \dot{\mathrm{V}} \)O2max :
-
maximum volume of oxygen consumed
- W:
-
water
References
Cox MH, Miles DS, Verde TJ, Rhodes EC. Applied physiology of ice hockey. Sports Med. 1995;19(3):184–201.
Montgomery DL. Physiology of ice hockey. Sports Med. 1988;5:99–126.
Paterson DH, Cunningham DA, Penny DS, Lefcoe M, Sangal S. Heart rate telemetry and estimated energy metabolism in minor league ice hockey. Can J Appl Sport Sci. 1977;2:71–5.
Nose H, Takamata A, MG W, et al. Water and electrolyte balance in the vascular space during graded-exercise in humans. J Appl Physiol. 1991;70:2757–62.
Hew-Butler T, Noakes TD, Soldin SJ, Verbalis JG. Acute changes in endocrine and fluid balance markers during high-intensity, steady-state, and prolonged endurance running: unexpected increases in oxytocin and brain natriuretic peptide during exercise. Eur J Endocrinol. 2008;159(6):729–37. doi:10.1530/EJE-08-0064.
Mears SA, Shirreffs SM. The effects of high-intensity intermittent exercise compared with continuous exercise on voluntary water ingestion. Int J Sport Nutr Exerc Metab. 2013;23:488–97.
Casa DJ, Armstrong LE, Hillman SK, et al. National Athletic Trainers’ Association Position Statement: fluid replacement for athletes. J Athl Train. 2000;35(2):212–24.
Robinson TA, Hawley JA, Palmer GS, et al. Water ingestion does not improve 1-h cycling performance in moderate ambient temperatures. Eur J Appl Physiol. 1995;71:153–60.
Batchelder BC, Krause BA, Seegmiller JG, Starkey CA. Gastrointestinal temperature increases and hypohydration exists after collegiate men's ice hockey participation. J Strength Cond Res. 2010;24(1):68–73. doi:10.1519/JSC.0b013e3181c49114.
Noonan B, Mack G, Stachenfeld N. The effects of hockey protective equipment on high-intensity intermittent exercise. Med Sci Sports Exerc. 2007;39(8):1327–35. doi:10.1249/mss.0b013e3180619644.
Logan-Sprenger HM, Palmer MS, Spriet LL. Estimated fluid and sodium balance and drink preferences in elite male junior players during an ice hockey game. Appl Physiol Nutr Metab. 2011;36(1):145–52. doi:10.1139/H10-098.
Palmer MS, Spriet LL. Sweat rate, salt loss, and fluid intake during an intense on-ice practice in elite Canadian male junior hockey players. Appl Physiol Nutr Metab. 2008;33(2):263–71. doi:10.1139/H08-011.
Palmer MS, Logan HM, Spriet LL. On-ice sweat rate, voluntary fluid intake, and sodium balance during practice in male junior ice hockey players drinking water or a carbohydrate-electrolyte solution. Appl Physiol Nutr Metab. 2010;35(3):328–35. doi:10.1139/H10-027.
Mears SA, Shirreffs SM. Voluntary water intake during and following moderate exercise in the cold. Int J Sport Nutr Exerc Metab. 2014;24(1):47–58. doi:10.1123/ijsnem.2013-0034.
Fruend BJ, Sawka MN. Influence of cold stress on human fluid balance. Washington: National Academy of Science; 1995.
Kenefick RW, Hazzard MP, Mahood NV, Castellani JW. Thirst sensations and AVP responses at rest and during exercise-cold exposure. Med Sci Sports Exerc. 2004;36(9):1528–34. doi:10.1249/01.mss.0000139901.63911.75.
Armstrong LE, Casa DJ. Millard-Stafford M, Moran DS, Pyne SW, Roberts WO. American College of Sports Medicine position stand. Exertional heat illness during training and competition. Med Sci Sports Exerc. 2007;39(3):556–72. doi:10.1249/MSS.0b013e31802fa199.
McConell GK, Stephens TJ, Canny BJ. Fluid ingestion does not influence intense 1-h exercise performance in a mild environment. Med Sci Sports Exerc. 1999;31(3):386–92.
Walsh RM, Noakes TD, Hawley JA, Dennis SC. Impaired high-intensity cycling performance time at low levels of dehydration. Int J Sports Med. 1994;15(7):392–8. doi:10.1055/s-2007-1021076.
Maxwell NS, Gardner F, Nimmo MA. Intermittent running: muscle metabolism in the heat and effect of hypohydration. Med Sci Sports Exerc. 1999;31(5):675–83.
Cleary MA, Hetzler RK, Wasson D, Wages JJ, Stickley C, Kimura IF. Hydration behaviors before and after an educational and prescribed hydration intervention in adolescent athletes. J Athl Train. 2012;47(3):273–81. doi:10.4085/1062-6050-47.3.05.
Ozolina L, Pontaga I, Kisis I. Amateur and professional ice hockey player hydration status and urine specific gravity values before and after training in winter conditions. Lase J Sport Sci. 2014;5(2):55–63.
Lopez RM, Casa DJ, Jensen KA, et al. Comparison of two fluid replacement protocols during a 20-km trail running race in the heat. J Strength Cond Res. 2016;30(9):2609–16. doi:10.1519/JSC.0000000000001359.
Ozgunen KT, Kurdak SS, Maughan RJ, et al. Effect of hot environmental conditions on physical activity patterns and temperature response of football players. Scand J Med Sci Sports. 2010;20(Suppl 3):140–7. doi:10.1111/j.1600-0838.2010.01219.x.
Godek SF, Peduzzi C, Burkholder R, Condon S, Dorshimer G, Bartolozzi AR. Sweat rates, sweat sodium concentrations, and sodium losses in 3 groups of professional football players. J Athl Train. 2010;45(4):364–71. doi:10.4085/1062-6050-45.4.364.
Brandenberger G, Candas V, Follenius M, Kahn JM. The influence of the initial state of hydration on endocrine responses to exercise in the heat. Eur J Appl Physiol. 1989;58:674–9.
Godek SF, Godek JJ, Bartolozzi AR. Hydration status in college football players during consecutive days of twice-a-day preseason practices. Am J Sports Med. 2005;33(6):843–51. doi:10.1177/0363546504270999.
McArdle WD, Katch FI, Katch VL. Exercise Physiology: Energy, Nutrition, and Human Performance. Fifth ed. Baltimore: Lippincott Williams & Wilkins; 2001.
Hagger MS, Montasem A. Implementing intentions to drink a carbohydrate-electrolyte solution during exercise. J Sport Sci. 2009;27(9):963–74. doi:10.1080/02640410902998262.
Maughan RJ. Fluid and electrolyte loss and replacement in exercise. J Sport Sci. 1991;9:117–42. doi:10.1080/02640419108729870.
Gisolfi CV, Lambert GP, Summers RW. Intestinal fluid absorption during exercise: role of sport drink osmolality and [Na+]. Med Sci Sports Exerc. 2001;33(6):907–15.
Acknowledgements
We would like to thank the head coach, athletic trainer, and other team personnel for their assistance and support throughout this study. We are extremely grateful to the players for their time and patience as participants.
Funding
This study was funded by internal funds obtained by TTM at the University of South Carolina.
Availability of data and materials
The datasets used for this study are available from the corresponding author (DE) on a case by case basis.
Author information
Authors and Affiliations
Contributions
All authors contributed to the development of the study, analysis of data, and read and approved the final manuscript. DE, CE and TL collected data. DE and CE were major contributors to writing the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Institutional Review Board at the University of South Carolina (#HSA4821). All participants read and signed an approved informed consent form prior to participation.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Emerson, D.M., Torres-McGehee, T.M., Emerson, C.C. et al. Individual fluid plans versus ad libitum on hydration status in minor professional ice hockey players. J Int Soc Sports Nutr 14, 25 (2017). https://doi.org/10.1186/s12970-017-0183-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12970-017-0183-x