Abstract
Background
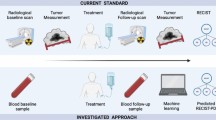
Recently, the concepts of progression due to pre-existing lesions (PPL) and progression due to new metastasis (PNM) have been proposed to differentiate the progression types of treatment-resistant cancers. Previously, the differences between these two progression types did not affect the determination of treatment strategies since both PPL and PNM are classified as progressive disease based on the response evaluation criteria in solid tumors (RECIST) diagnostic criteria. On the other hand, tumor infiltrating lymphocytes (TILs) are effective when used as indicators for monitoring the immune tumor microenvironment (iTME) in the cancer host, and TILs play an important role as biomarkers in predicting prognosis and therapeutic effects. This study focused on the progression types of cancer in patients undergoing eribulin chemotherapy. In addition, the iTME in individuals with PPL and PNM was evaluated using TILs as a marker.
Methods
Of the 52 patients with locally advanced or metastatic breast cancer who underwent chemotherapy with eribulin, 40 remained in the study, and 12 patients were dropout cases. The antitumor effect was evaluated based on the RECIST criteria using version 1.1. TILs were defined as the infiltrating lymphocytes within tumor stroma and were expressed in proportion to the field investigated. In PPL cases, the high-TIL group was considered as type I and the low-TIL group was classified as type II. In PNM cases, the high-TIL group was considered as type III and the low-TIL group was classified as type IV.
Results
In 19 cases, individuals with type I progression had significantly longer progression free survival and overall survival (OS) compared to those with type III progression (p = 0.040, p < 0.001, log-rank). Individuals with type I progression had significantly prolonged survival post progression compared to those with type II progression (p = 0.048, log-rank). A multivariate analysis that validate the effect of OS showed that these were independent factors of good prognosis (p = 0.003; hazard ratio [HR] = 0.065) (p = 0.006; HR = 0.105).
Conclusions
The effects of eribulin chemotherapy suggested that patients with progressive-type breast cancer that proliferates in a good iTME may have a good prognosis.
Similar content being viewed by others
Background
The evaluation of the therapeutic effects of chemotherapy for solid tumors based on the response evaluation criteria in solid tumors (RECIST) plays an important role in determining treatment strategies both in clinical trials and practice [1]. Recently, the concepts of progression due to pre-existing lesions (PPL) and progression due to new metastasis (PNM) have been proposed to differentiate the progression types of treatment-resistant cancers [2, 3]. Previously, the differences between these two progression types did not affect the determination of treatment strategies since both PPL and PNM are classified as progressive disease (PD) based on the RECIST diagnostic criteria. However, to date, it is known that PPL does not involve metastasis but only invasion to the peripheral tissues. In contrast, PNM involves both invasion into the peripheral tissues and metastasis to other organs.
Tumor infiltrating lymphocytes (TILs) are effective when used as indicators for monitoring the immune tumor microenvironment (iTME) in the cancer host, and TILs play an important role as biomarkers in predicting prognosis and therapeutic effects [4,5,6]. The tumor microenvironment (TME) influences tumor survival and growth, infiltration, and metastasis and has been a topic of interest because of its effect on tumor cells. In addition, it has also been considered as a new therapeutic target [7, 8].
Eribulin mesylate (eribulin), as a tubulin inhibitor, has cytocidal effects, and it has unique pharmacological properties that were proven to modulate the TME [9, 10]. In a phase III clinical trial on patients with locally advanced or metastatic breast cancer (MBC), eribulin significantly prolonged the overall survival (OS) of patients with the therapeutic effects of TME [11, 12]. Furthermore, this survival curve showed a characteristic pattern called the delayed separation curve in immune checkpoint inhibitor therapy and immunotherapy, thus emphasizing the effects of eribulin on the iTME.
Therefore, this study focused on the progression types of cancer in patients undergoing eribulin chemotherapy. The purpose of this study is to investigate factors contributing to the extension of OS of eribulin chemotherapy. In addition, the iTME in individuals with PPL and PNM was evaluated using TILs as a marker.
Methods
Patient background
A total of 322 patients with MBC underwent cancer treatment at Osaka City University Hospital from August 2000 to June 2013. In the present study, only 40 patients were included, and 270 patients with other drug therapies (endocrine therapy and other chemotherapeutic regimens) and 12 patients with dropout cases due to surgery or adverse events were excluded (Fig. 1). This data set was also used in previous studies [13, 14].
Consort diagram. A total of 322 patients with MBC underwent cancer treatment at Osaka City University Hospital from August 2000 to June 2013. In the present study, only 40 patients were included, and 270 patients with other drug therapies and 12 patients with dropout cases due to surgery or adverse events were excluded
The median follow-up time was 431 days (range 50–650 days). The objective response rate (ORR), OS, progression free survival (PFS), and survival post progression (SPP) were obtained based on the efficacy of this regimen. The ORR was evaluated by adding the complete response (CR) and partial response (PR). The OS was defined as the period from the start date of treatment to death (daily). The PFS was defined as the period from the start date of treatment to either the earlier date of death or confirmation of PD (daily). The SPP was evaluated daily and defined as the period from the start date of the treatment after PD with eribulin chemotherapy to death. The antitumor effect was evaluated based on the RECIST criteria using version 1.1 [1].
Based on the chemotherapy regimen, which is one course of treatment for 21 days, eribulin (1.4 mg/m2) was intravenously administered on days 1 and 8 [11, 12]. This protocol was repeatedly used until PD was evaluated or it was discontinued due to severe adverse events.
The morphology of the tumor (type of histological tissue and nucleus grade) was identified using hematoxylin and eosin (H.E.) staining. Moreover, the expression of estrogen receptor (ER), progesterone receptor (PgR), human epidermal growth factor receptor 2 (HER2), and Ki67 were immunohistologically evaluated.
Histopathological evaluation
Upon breast cancer diagnosis, TILs were evaluated by measuring the percentage of area occupied by the lymphocytes on the H.E.-stained tumor section using biopsy specimens [15]. The area of stromal TILs surrounding the stained cancer cells was quantitatively measured in each field of view (400×) [13, 16]. The area of the stroma with lymphoplasmacytic infiltration around the invasive tumor cell nests was > 50, > 10–50, ≤ 10%, or absent, and the corresponding scores assigned were 3, 2, 1, or 0, respectively (Additional file 1: Figure S1). TILs were classified as high (score of 2 or higher) and low (score of 1 and 0). TILs were histopathologically evaluated by two professional breast cancer pathologists.
Classification based on progression type and evaluation of TILs
According to the RECIST guideline, PPL is the 20% increase in the sum of the diameters of the target lesions, and taking into consideration the small relative sum obtained in the study, an absolute increase of at least 5 mm was observed. PNM was defined as a lesion identified on a follow-up study in an anatomical location that was not assessed at baseline and is considered as a new lesion that can indicate disease progression [2, 3]. When PPL and PNM were observed at the same time during evaluation, PNM was considered. In PPL cases, the high-TIL group was considered as type I and the low-TIL group was classified as type II. In PNM cases, the high-TIL group was considered as type III and the low-TIL group was classified as type IV.
Statistical analysis
A statistical analysis was performed using the SPSS® version 19.0 statistical software (IBM, Armonk, NY, USA). The association between TILs and other clinicopathologic parameters was analyzed via the Chi square test (or Fisher’s exact test when necessary). The association with PFS, OS, and SPP was analyzed via the Kaplan–Meier plot and log-rank test. Univariate and multivariate hazard ratios (HR) were computed for the study parameters with 95% confidence intervals (CIs) using a Cox proportional hazards model, and a backward stepwise method was used for variable selection in multivariate analyses. A p-value less than 0.05 was considered statistically significant.
Ethics statement
The study design involved a retrospective chart review. An informed consent was obtained from all patients according to the protocol approved by the Ethics Committee of Osaka City University (#926). This research is in accordance with the 2013 Declaration of Helsinki.
Results
Differences in progression types and prognostic analysis
Of the 52 patients with MBC who underwent chemotherapy with eribulin, 40 remained in the study, and 12 patients were excluded. Of which, 7 PNM cases (17.5%) and 33 PPL cases (72.5%) were observed. The PPL group had a significantly longer PFS (p = 0.044, log-rank) and OS (p = 0.017, log-rank) compared to the PNM group (Fig. 2).
TIL expression and differences in progression types
Of the 40 participants, 23 (57.5%) were included in the high-TIL group, and 17 (42.5%) were classified in the low-TIL group. Of the 7 individuals in the PNM group, 4 were classified in the high-TIL group (57.1%), and 3 were included in the low-TIL group (42.9%). Of the 33 participants in the PPL group, 19 were classified in the high-TIL group (57.6%) and 14 were included in the low-TIL group (42.4%). There was no significant difference between clinicopathological parameter and TILs when group was divided by difference of TILs expression (Table 1).
Effects of TIL expression and differences in progression type upon prognosis
In 19 cases, individuals with type I progression had significantly longer PFS compared to those with type III progression (p = 0.040, log-rank) (Fig. 3). Furthermore, individuals with type I progression had significantly longer OS compared to those with type III and type II progression (p < 0.001 and p = 0.047, respectively; log-rank). Individuals with type I progression had significantly prolonged SPP compared to those with type II progression (p = 0.048, log-rank) (Fig. 4). A univariate analysis that validate the effect of OS showed that high ORR and type I progression were considered as factors for a good prognosis (p = 0.006; HR = 0.160) (p = 0.020; HR = 0.221) (Fig. 5). A multivariate analysis also showed that these were independent factors of good prognosis (p = 0.003; HR = 0.065) (p = 0.006; HR = 0.105) (Table 2).
Effects of TIL expression and differences in progression type upon prognosis. In 19 cases, individuals with type I progression had significantly longer PFS compared to those with type III progression (p = 0.040, log-rank) (a). Furthermore, individuals with type I progression had significantly longer OS compared to those with type III and type II progression (p < 0.001 and p = 0.047, respectively; log-rank) (b)
Discussion
Patients with MBC who underwent chemotherapy with eribulin in two international phase III clinical trials (Study 305 [eribulin monotherapy versus physician’s choice of treatment in patients with metastatic breast cancer, EMBRACE] and Study 301) had prolonged OS [11, 12]. Only pertuzumab [17,18,19] and trastuzumab emtansine (T-DM1) [20], other than eribulin, were proven to prolong the OS of individuals with HER2-positive breast cancer. The prolongation of OS due to chemotherapy is challenging in individuals with MBC because of the therapy’s relative biological mildness. However, other treatment options are also available. Although this therapy along with bevacizumab improved PFS, which has a higher response rate, it did not significantly affect OS (E2100, AVADO, RIBBON-1) [21,22,23,24]. Due to this reason, in addition to signal pathway blocking and cytocidal pharmacological actions, the TME is considered important in increasing OS in individuals with MBC who are on chemotherapy. The OS Kaplan–Meier curve in Studies 305 and 301 and the clinical evaluation of pertuzumab and trastuzumab (CLEOPATRA) trial showed a delayed separation curve during immunotherapy, suggesting that tumor immune response may be involved in these chemotherapy regimens [11, 12, 17, 18]. Thus, monitoring iTME through TILs is a key factor in predicting the therapeutic effect of chemotherapy with eribulin.
The TNM classification of tumor factor has conventionally been used as an indicator of cancer prognosis. However, differences in prognosis were found even when the degree of progression was the same. Therefore, the host factors of inflammatory response and nutritional status and TME monitoring as new indicators have been a topic of interest [7, 25,26,27]. That is, cancer progression is determined not only by the characteristics of the cancer cells themselves but also by the interactions between the cancer cells and TME, such as the epithelial–mesenchymal transition (EMT) and immune response [7, 28]. The effect of the immune responses in the TME of cancer host on prognosis and the prediction of the therapeutic effects of chemotherapy have also been reported [5,6,7, 29]. Based on basic research, eribulin has an inhibitory effect on the TME, including EMT suppression and tumor vascular remodeling [9, 10, 30]. Our previous study demonstrated that evaluating TILs before the start of eribulin therapy helped in the prediction of its therapeutic effect in individuals with triple-negative breast cancer [13]. Moreover, this study showed that patients with PPL who have good iTME conditions had a good prognosis.
In contrast, PD in the RECIST diagnostic criteria is classified into PPL and PNM, and individuals with PNM had a poorer prognosis than those with PPL in Studies 305 and 301 [3]. The difference between these two progression types is that PNM involves invasion into peripheral tissues and metastasis to other organs, which explains the course of poor prognosis, whereas the PPL does not involve metastasis but only invasion to peripheral tissues [2, 3].
The study has limitations since it involves a retrospective analysis of a small sample size. However, to the best of our knowledge, this study first investigated the progression types by evaluating the iTME in patients with MBC who undergoing chemotherapy, with an increased OS that was achieved through chemotherapy with eribulin. In the future, differences in progression types should also be considered in clinical practice to determine the best treatment options.
Conclusions
In conclusion, this study showed that patients with PPL who have good iTME conditions had a good prognosis. In brief, the effects of eribulin chemotherapy suggested that patients with progressive-type breast cancer that proliferates in a good TME may have a good prognosis.
Abbreviations
- RECIST:
-
response evaluation criteria in solid tumors
- PPL:
-
progression due to pre-existing lesions
- PNM:
-
progression due to new metastasis
- PD:
-
progressive disease
- TILs:
-
tumor infiltrating lymphocytes
- iTME:
-
immune tumor microenvironment
- TME:
-
tumor microenvironment
- eribulin:
-
eribulin mesylate
- MBC:
-
locally advanced or metastatic breast cancer
- OS:
-
overall survival
- ORR:
-
objective response rate
- PFS:
-
progression free survival
- SPP:
-
survival post progression
- CR:
-
complete response
- PR:
-
partial response
- H.E.:
-
hematoxylin and eosin
- ER:
-
estrogen receptor
- PgR:
-
progesterone receptor
- HER2:
-
human epidermal growth factor receptor 2
- HR:
-
hazard ratio
- CI:
-
confidence interval
- EMBRACE:
-
eribulin monotherapy versus physician’s choice of treatment in patients with metastatic breast cancer
- T-DM1:
-
trastuzumab emtansine
- CLEOPATRA:
-
clinical evaluation of pertuzumab and trastuzumab
- EMT:
-
epithelial–mesenchymal transition
References
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, Dancey J, Arbuck S, Gwyther S, Mooney M, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45(2):228–47.
Litiere S, de Vries EG, Seymour L, Sargent D, Shankar L, Bogaerts J, Committee R. The components of progression as explanatory variables for overall survival in the response evaluation criteria in solid tumours 1.1 database. Eur J Cancer. 2014;50(10):1847–53.
Twelves C, Cortes J, Kaufman PA, Yelle L, Awada A, Binder TA, Olivo M, Song J, O’Shaughnessy JA, Jove M, et al. “New” metastases are associated with a poorer prognosis than growth of pre-existing metastases in patients with metastatic breast cancer treated with chemotherapy. Breast Cancer Res. 2015;17(1):150.
Zitvogel L, Kepp O, Kroemer G. Immune parameters affecting the efficacy of chemotherapeutic regimens. Nat Rev Clin Oncol. 2011;8(3):151–60.
Fridman WH, Pages F, Sautes-Fridman C, Galon J. The immune contexture in human tumours: impact on clinical outcome. Nat Rev Cancer. 2012;12(4):298–306.
Couzin-Frankel J. Breakthrough of the year 2013. Cancer immunotherapy. Science. 2013;342(6165):1432–3.
Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144(5):646–74.
Noman MZ, Messai Y, Muret J, Hasmim M, Chouaib S. Crosstalk between CTC, immune system and hypoxic tumor microenvironment. Cancer Microenviron. 2014;7(3):153–60.
Yoshida T, Ozawa Y, Kimura T, Sato Y, Kuznetsov G, Xu S, Uesugi M, Agoulnik S, Taylor N, Funahashi Y, et al. Eribulin mesilate suppresses experimental metastasis of breast cancer cells by reversing phenotype from epithelial–mesenchymal transition (EMT) to mesenchymal-epithelial transition (MET) states. Br J Cancer. 2014;110(6):1497–505.
Funahashi Y, Okamoto K, Adachi Y, Semba T, Uesugi M, Ozawa Y, Tohyama O, Uehara T, Kimura T, Watanabe H, et al. Eribulin mesylate reduces tumor microenvironment abnormality by vascular remodeling in preclinical human breast cancer models. Cancer Sci. 2014;105(10):1334–42.
Cortes J, O’Shaughnessy J, Loesch D, Blum JL, Vahdat LT, Petrakova K, Chollet P, Manikas A, Dieras V, Delozier T, et al. Eribulin monotherapy versus treatment of physician’s choice in patients with metastatic breast cancer (EMBRACE): a phase 3 open-label randomised study. Lancet. 2011;377(9769):914–23.
Schoffski P, Chawla S, Maki RG, Italiano A, Gelderblom H, Choy E, Grignani G, Camargo V, Bauer S, Rha SY, et al. Eribulin versus dacarbazine in previously treated patients with advanced liposarcoma or leiomyosarcoma: a randomised, open-label, multicentre, phase 3 trial. Lancet. 2016;387(10028):1629–37.
Kashiwagi S, Asano Y, Goto W, Takada K, Takahashi K, Noda S, Takashima T, Onoda N, Tomita S, Ohsawa M, et al. Use of tumor-infiltrating lymphocytes (TILs) to predict the treatment response to eribulin chemotherapy in breast cancer. PLoS ONE. 2017;12(2):e0170634.
Kashiwagi S, Fukushima W, Asano Y, Goto W, Takada K, Noda S, Takashima T, Onoda N, Ohsawa M, Hirakawa K, et al. Identification of predictive markers of the therapeutic effect of eribulin chemotherapy for locally advanced or metastatic breast cancer. BMC Cancer. 2017;17(1):604.
Salgado R, Denkert C, Demaria S, Sirtaine N, Klauschen F, Pruneri G, Wienert S, Van den Eynden G, Baehner FL, Penault-Llorca F, et al. The evaluation of tumor-infiltrating lymphocytes (TILs) in breast cancer: recommendations by an International TILs Working Group 2014. Ann Oncol. 2015;26(2):259–71.
Ono M, Tsuda H, Shimizu C, Yamamoto S, Shibata T, Yamamoto H, Hirata T, Yonemori K, Ando M, Tamura K, et al. Tumor-infiltrating lymphocytes are correlated with response to neoadjuvant chemotherapy in triple-negative breast cancer. Breast Cancer Res Treat. 2012;132(3):793–805.
Baselga J, Cortes J, Kim SB, Im SA, Hegg R, Im YH, Roman L, Pedrini JL, Pienkowski T, Knott A, et al. Pertuzumab plus trastuzumab plus docetaxel for metastatic breast cancer. N Engl J Med. 2012;366(2):109–19.
Baselga J, Cortes J, Im SA, Clark E, Ross G, Kiermaier A, Swain SM. Biomarker analyses in CLEOPATRA: a phase III, placebo-controlled study of pertuzumab in human epidermal growth factor receptor 2-positive, first-line metastatic breast cancer. J Clin Oncol. 2014;32(33):3753–61.
Kawajiri H, Takashima T, Kashiwagi S, Noda S, Onoda N, Hirakawa K. Pertuzumab in combination with trastuzumab and docetaxel for HER2-positive metastatic breast cancer. Expert Rev Anticancer Ther. 2015;15(1):17–26.
Verma S, Miles D, Gianni L, Krop IE, Welslau M, Baselga J, Pegram M, Oh DY, Dieras V, Guardino E, et al. Trastuzumab emtansine for HER2-positive advanced breast cancer. N Engl J Med. 2012;367(19):1783–91.
Rossari JR, Metzger-Filho O, Paesmans M, Saini KS, Gennari A, de Azambuja E, Piccart-Gebhart M. Bevacizumab and breast cancer: a meta-analysis of first-line phase III studies and a critical reappraisal of available evidence. J Oncol. 2012;2012:417673.
Miller K, Wang M, Gralow J, Dickler M, Cobleigh M, Perez EA, Shenkier T, Cella D, Davidson NE. Paclitaxel plus bevacizumab versus paclitaxel alone for metastatic breast cancer. N Engl J Med. 2007;357(26):2666–76.
Miles DW, Chan A, Dirix LY, Cortes J, Pivot X, Tomczak P, Delozier T, Sohn JH, Provencher L, Puglisi F, et al. Phase III study of bevacizumab plus docetaxel compared with placebo plus docetaxel for the first-line treatment of human epidermal growth factor receptor 2-negative metastatic breast cancer. J Clin Oncol. 2010;28(20):3239–47.
Robert NJ, Dieras V, Glaspy J, Brufsky AM, Bondarenko I, Lipatov ON, Perez EA, Yardley DA, Chan SY, Zhou X, et al. RIBBON-1: randomized, double-blind, placebo-controlled, phase III trial of chemotherapy with or without bevacizumab for first-line treatment of human epidermal growth factor receptor 2-negative, locally recurrent or metastatic breast cancer. J Clin Oncol. 2011;29(10):1252–60.
Lu H, Ouyang W, Huang C. Inflammation, a key event in cancer development. Mol Cancer Res. 2006;4(4):221–33.
Toyokawa T, Kubo N, Tamura T, Sakurai K, Amano R, Tanaka H, Muguruma K, Yashiro M, Hirakawa K, Ohira M. The pretreatment controlling nutritional status (CONUT) score is an independent prognostic factor in patients with resectable thoracic esophageal squamous cell carcinoma: results from a retrospective study. BMC Cancer. 2016;16:722.
Shibutani M, Maeda K, Nagahara H, Ohtani H, Sakurai K, Yamazoe A, Kimura K, Toyokawa T, Amano R, Kubo N, et al. Significance of markers of systemic inflammation for predicting survival and chemotherapeutic outcomes and monitoring tumor progression in patients with unresectable metastatic colorectal cancer. Anticancer Res. 2015;35(9):5037–46.
Terry S, Chouaib S. EMT in immuno-resistance. Oncoscience. 2015;2(10):841–2.
Savas P, Salgado R, Denkert C, Sotiriou C, Darcy PK, Smyth MJ, Loi S. Clinical relevance of host immunity in breast cancer: from TILs to the clinic. Nat Rev Clin Oncol. 2016;13(4):228–41.
Ueda S, Saeki T, Takeuchi H, Shigekawa T, Yamane T, Kuji I, Osaki A. In vivo imaging of eribulin-induced reoxygenation in advanced breast cancer patients: a comparison to bevacizumab. Br J Cancer. 2016;114(11):1212–8.
Authors’ contributions
SK participated in the design of the study and drafted the manuscript. GT, YA, WG, KTakad, TM and TT helped with study data collection and manuscript preparation. KTakah, HF and ST helped with study data collection and participated in its design. MOhs helped with pathological diagnosis. KH and MOhi conceived the study, and participated in its design and coordination and helped to draft the manuscript. All authors read and approved the final manuscript.
Acknowledgements
We thank Sayaka Tanaka (STa) (Department of Diagnostic Pathology, Osaka City University Graduate School of Medicine) for helpful advice regarding pathological diagnosis. We thank Yayoi Matsukiyo and Tomomi Okawa (Department of Surgical Oncology, Osaka City University Graduate School of Medicine) for helpful advice regarding data management.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
The datasets supporting the conclusions of this article is included within the article.
Consent for publication
Written informed consent was obtained from all patients.
Ethics approval and consent to participate
Written informed consent was obtained from all subjects. This research conformed to the provisions of the Declaration of Helsinki in 2013. All patients were informed of the investigational nature of this study and provided their written, informed consent. The study protocol was approved by the Ethics Committee of Osaka City University (#926).
Funding
This study was funded by grants from the Japan Society for the Promotion of Science (KAKENHI, Nos. 25461992, 26461957, and 17K10559) to Shinichiro Kashiwagi.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Additional file
Additional file 1: Figure S1.
Region of histopathological TIL evaluation. TILs were measured by examining the occupation ratio of immune cells present in the tumor stroma of hematoxylin and eosin stained specimens at ×400 magnification. Proportional scores of 3, 2, 1, and 0 were given if the area of stroma containing lymphoplasmacytic infiltration around invasive tumor cell nests comprised > 50% (A), > 10–50% (B), ≤ 10% (C), and 0% (D), respectively.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Kashiwagi, S., Tsujio, G., Asano, Y. et al. Study on the progression types of cancer in patients with breast cancer undergoing eribulin chemotherapy and tumor microenvironment. J Transl Med 16, 54 (2018). https://doi.org/10.1186/s12967-018-1443-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12967-018-1443-5