Abstract
Background
This study sought to identify, as far as possible, the extent of the specialist children’s nursing workforce in five selected African countries. Strengthening children’s nursing training has been recommended as a primary strategy to reduce the under-five mortality rate in African nations. However, information about the extent of the specialist children’s nursing workforce in this region is not routinely available. Developing an accurate depiction of the specialist children’s nursing workforce is a necessary step towards optimising children’s health service delivery.
Methods
This study used a convergent parallel mixed methods design, incorporating quantitative (surveys) and qualitative (questionnaire and interview) components, to generate data addressing three related questions: how many children’s nurses are believed to be in practice nationally, how many such nurses are recorded on the national nursing register and how many children’s nurses are being produced through training annually.
Results
Data provide insights into reported children’s nursing workforce capacity, training activity and national training output in the five countries. Findings suggest there are approximately 3728 children’s nurses across the five countries in this study, with the majority in South Africa. A total of 16 educational programmes leading to a qualification in paediatric nursing or child health nursing are offered by 10 institutions across the countries in this study, with Kenya, Malawi and Zambia having one institution each and South Africa hosting seven. Data suggest that existing human resources for health information systems do not currently produce adequate information regarding the children’s nursing workforce. Analysis of qualitative data elicited two themes: the role of children’s nurses and their position within health systems, and the capacity of HRH information systems to accurately reflect the specialist children’s nursing workforce.
Conclusion
The data generated provide an initial indication of the size of the children’s nursing workforce in these five countries, as well as an overview of associated training activity. We hope that they can start to inform discussion about what would represent a viable and sustainable regional children’s nursing workforce for the future.
Similar content being viewed by others
Background
Nurses are the backbone of healthcare delivery in Africa, forming the largest part of the professional health workforce [1, 2]. Children aged 0–15 make up between 29 and 48% of the total population in the five countries studied (see Table 2) [3]. Children represent a high proportion of hospital admissions, with neonates in one South African study accounting for 40% of critical care bed occupation [4]. Outcomes for hospitalised children remain poor compared to higher resourced healthcare settings [5].
Strengthening children’s nursing training is recommended as a primary strategy to reduce the under-five mortality rate in African nations [6, 7]. Progress in postgraduate education and training in Africa has resulted in the presence within the workforce of a small cadre of nurses with specialised knowledge and skills relating to the care of sick babies and children, gained through additional qualifications [8]. These specialist children’s nurses are a scarce key resource in a region where more than 100 children per 1000 may die before the age of five [9] and where as many as 80% of nursing posts are vacant in some remote areas [7, 10].
Despite the potential importance of this cadre of nurses, there is a lack of accurate high-quality information about this emerging sector of the nursing workforce. Ideally, health management information systems would already be capable of monitoring the children’s nursing workforce in these countries. The reality is that children’s nurses in Africa are largely invisible to health information systems at the moment. Current data capabilities mean that most systems in lower income countries, including National Health Workforce Accounts, treat the nursing workforce as a single category. The absence of this information currently constrains the planning and creating of a viable and sustainable children’s nursing workforce. Developing an accurate depiction of the specialist registered children’s nursing workforce is a necessary step towards optimising children’s health service delivery and ultimately improving child health. This study sought to provide an initial estimation of the extent of the children’s nursing workforce in five selected African countries, by investigating the numbers of such nurses in practice and the scope of training activity, as a first step towards identifying what would represent a viable and sustainable children’s nursing workforce for the future.
Terminology
The terms used to refer to the category of nurses considered in this study vary throughout the region. The widely understandable plain language description of ‘children’s nurse’ is used throughout this paper to refer to nurses who have undertaken post-basic training leading to a qualification as a specialist paediatric or child health nurse which is registerable with the relevant national nursing council.
Methods
Aim and design
This study aimed to quantify the extent of the children’s nursing workforce in five selected African countries. A convergent parallel mixed methods design was used, incorporating quantitative (surveys) and qualitative (questionnaire and interview) components. The methodology was selected to access both subjective and objective knowledge relating to the children’s nursing workforce, with the intention of maximising understanding and enabling corroboration between sources where existing factual information was known to be scarce [11, 12].
There were two key components of the study. Questionnaire surveys were administered to three groups of participants in order to elicit information about the number of children’s nurses respectively: in practice nationally, recorded on the professional register and being produced through training. Secondly, telephone interviews were scheduled with key informants in the final phase of data collection to supplement the information gathered. Interviewees had prior sight of the draft findings for their country and were asked to engage with the information to highlight inaccuracies or discrepancies and assist with corroboration.
Our study design included asking respondents and interviewees about the existence of recommendations for staffing norms specific to paediatrics. No specific recommendations were identified, and we are not aware of any made by the WHO or major global health organisations in relation to paediatric nurse ratios in LMICs.
Setting and participants
This study extended to five African countries: Kenya, Malawi, Uganda, South Africa and Zambia. These countries were selected because they were believed to be actively training children’s nurses on the basis of knowledge obtained through sectoral engagement by the authors over the preceding 10 years. Documentary review revealed that very little information about the extent of the children’s nursing workforce in these countries was in the public domain. South Africa was the only country for which information relating to the numbers of children’s nurses on the national nursing register was available through published information. Current data capabilities mean that most health information systems in the countries studied, including National Health Workforce Accounts, treat the nursing workforce as a single category. This prior knowledge informed the approach to data collection. Our study design included asking respondents and interviewees about the existence of recommendations for staffing norms specific to paediatrics.
Expert elicitation sampling [13] was used, focusing on respondent characteristics that conferred a high level of familiarity with the children’s nursing workforce and/or access to records and relevant information. Criteria for inclusion were that the individual was a registrar of a national nursing council, the individual was a nursing educator at a training institution in the country or the individual held another leadership position within the national children’s nursing, paediatrics or child health communities. Expert sampling is recommended as an approach in situations where there is a lack of empirical knowledge and where uncertainty may be high [13]. The use of expert sampling was justified in the case of this investigation because of the objectively small size of the children’s nursing workforce in these countries and the lack of existing empirical data.
Two existing sources of information relevant to the question were identified, both of which were specific to South Africa. The record of the Child Nursing Educator Forum Nov. 2016 reported the number of children trained at 7/7 institutions in 2015. A separate study provided the number of children’s nurses trained at 5/7 institutions between 2012 and 2016, as well as information about the nature of this training activity (Chukwu, Shung-King, Sieberhagen, North: Paediatric nurse training activity in South Africa. A short report, forthcoming).
Original data collection was undertaken for Kenya, Malawi, Uganda and Zambia in the form of the questionnaire surveys and interviews described in Table 1. One respondent for each category was also included for South Africa to support consistency and corroboration of existing data. Data from all sources were then combined to provide a complete set of information for 2015, which was the only year for which a full set of data was available. The origins of all data are shown in the text and tables. In total, 15 individuals were invited to participate in the study. A summary of data sources is shown in Table 1.
Analysis and synthesis of data
Analysis of data was driven by the primary goal of this study, which was to identify as far as possible the extent of the children’s nursing workforce in five selected African countries. Quantitative data from questionnaire responses was collated and tabulated in the form of country-level findings. Data from interviews were transcribed by the researcher. An explicit transcription strategy and a consistent approach to coding content supported rigour during analysis [15]. Data derived from the processes described above were integrated or ‘mixed’ during analysis to generate as valid as possible a description of the capacity of the children’s nursing workforce in the five countries.
Ethical approval
The study was approved by the Human Research Ethics Committee of the University of Cape Town (HREC REF: 411/2017).
Results
Findings are presented in relation to reported children’s nursing workforce capacity, training activity and national training output. Analysis of qualitative data elicited two themes: the role of children’s nurses and their position within health systems, and the capacity of HRH information systems to accurately reflect the extent of the specialist children’s nursing workforce.
Reported children’s nursing workforce capacity
The data collected suggest that the combined children’s nursing workforce reported for the five countries in this study totals 3728 nurses. South Africa accounts for around 8/10 of these nurses (3200, 84%). Table 2 presents reported children’s nursing workforce capacity. Data are presented alongside population estimates for babies and children 0–15 years to enable consideration of the numbers of children’s nurses relative to population.
Reported children’s nursing training activity
A total of 16 educational programmes leading to a qualification in paediatric nursing or child health nursing are offered by 10 institutions across the countries in this study, with Kenya, Malawi and Zambia having one institution each and South Africa hosting seven. Table 3 presents data relating to five countries where training is provided, or (in the case of Uganda) was provided until recently. One institution in Uganda was identified by a respondent as possibly offering relevant training, and attempts were made to contact this institution to participate in the survey of Heads of Schools of children’s nursing. No response was received. Private correspondence indicates that this institution is not currently offering training relevant to the purposes of this study, with training having ceased around 2016–2017.
Notwithstanding the cessation of training in Uganda, the data suggest a steady growth in children’s nursing training activity since 2006 overall, measured by the number of programmes being offered. Prior to this, the data suggest that South Africa was the only country in southern Africa training children’s nurses. A total of eight new training programmes were reported to have been established between 2006 and 2016, in Kenya (in 2006 and 2013), Malawi (2010), Zambia (2014) and South Africa (2006, 2009 and 2015).
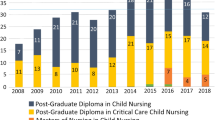
National training output
Examination of the data in Table 4 suggests that a total of 81 children’s nurses were produced through training by Kenya, Malawi and Zambia in 2015 and 191 by South Africa for the same year. South Africa is the region’s largest children’s nursing training provider. Available data show that the number of children’s nurses reported trained at 5 out of 7 South African institutions between 2012 and 2016 equalled 60 (Chukwu, Shung-King, Sieberhagen, North: Paediatric nurse training activity in South Africa. A short report, forthcoming). Based on this, an estimated 179 children’s nurses are produced across South Africa’s seven training institutions on average per year.
Using the survey data obtained, an attempt was made to estimate training output to date for Kenya, Malawi and Zambia. As data were only available for a single year for these countries, the resulting estimations cannot be considered accurate, but are presented in Table 4 for illustrative purposes. Data suggest that by 2015 approximately 397 children’s nurses had been trained since programmes began in these three countries.
Interviews
Interviewees confirmed the plausibility of the information obtained through questionnaires.
Two additional themes were identified.
The role of children’s nurses—perceptions of interviewees
Interviewees were asked to respond to the questions ‘How do children’s nurses contribute to children’s health in your country?’ and ‘Do children’s nurses carry out the same duties and tasks as other categories of nurses?’. They provided insightful descriptions of the role of children’s nurses and the way this category of nurse can contribute within lower resourced healthcare systems.
They contribute greatly in terms of how they are trained and the power to think and do the work they do. They are trained to identify conditions, make plans and commence the initial treatment before the doctor comes in. In Malawi, the ratio of doctors to patients is very low, and the patients are so many. Wherever they are working, these specialist nurses are empowered, through their specialist training…Because of that they are really able to take the lead in managing the children, depending on whichever areas they are in. In outpatients, they are able to triage children and say ‘this child requires quick attention’. They are able to facilitate the management. The delays associated with starting treatment are getting less now. (Nursing leader, Malawi)
The two [children’s] nurses at [name of hospital], they are very good. One is running the whole feeding clinic. (Nursing leader, Uganda)
Specialist children’s nurses should mostly be working at the level of district hospitals. Then you need sub-specialists at regional and tertiary level – the neonatal nurses, and critical care [children’s] nurses. And the role of children’s nurses [at district hospital level] is to be the institutional memory. They are the hearts and brains of a service. (Child health leader, South Africa)
Capacity of information systems—perceptions of interviewees
Interviewees identified the growth of specialisation as having implications for information systems: ‘The growth of specialists is a new demand on the register. In Malawi now we have those doing nursing education, reproductive health, midwifery, community... It’s a different dynamic and we need to respond accordingly, as a country and as a registering board. The recording is done according to qualifications. So if a nurse has a masters in paediatrics, they are recorded as having such. [The register] records the qualification held, but it does not separately record the category of specialists. We are still yet to put up a category of all of the specialists.’ (Nursing leader, Malawi)
The information provided by interviewees concurred with the finding that only South Africa routinely monitors and reports on the size of the registered children’s nursing workforce currently. Even in this case, one interviewee expressed the view that this information is not being used to inform planning: ‘The main focus … is on norms and numbers [of all categories of nurses], it’s not about specialisation.’ (Interview participant, South Africa)
One interviewee suggested that the benefits of information specific to the children’s workforce may not be understood by decision makers due to a lack of understanding of the role: ‘The contribution of the specialist children’s nurses that do exist isn’t always made the most of in the services, they [the services] don’t have that understanding.’ (Interview participant, Uganda)
Existence of polices guiding training
Heads of Schools of Nursing responding to the questionnaire survey and key informants participating in telephone interviews were asked about the existence of national and local policies or training plans determining the provision of children’s nursing training. Very minimal information was elicited. Participants were asked ‘Are there national and local policies or training plans which guide the provision of children’s nursing training in your institution/country?’ Respondents mentioned a total of 11 sources of guidance relevant to the provision of children’s nursing training relating to Malawi, South Africa and Zambia. Of these, four were not possible to identify for review (e.g. ‘the child health policy’). Seven were assessed as not relevant for review (e.g. the document took the form of a specific clinical practice guideline, e.g. Helping Babies Breathe). One item was identified as relevant and was reviewed. This was the South African Nursing Council’s specification of competencies for the category of specialist children’s nurse (South African Nursing Council, 2012). The existence and nature of national policies and strategies guiding the development of the children’s nursing workforce requires further investigation.
Limitations
The lack of response from national nursing councils meant that an important data source intended to enable triangulation was omitted. The information could not be identified through Internet searching of published records of the remaining national nursing councils, either because registers are not available for inspection or because children’s nursing qualifications could not be extracted from published totals. South Africa was the only country for which information relating to the numbers of children’s nurses on the register was available through published information in the public domain.
The decision to collect data relating to training outputs for a single year (2015) was made to reduce the burden on respondents. Confining data to a single year limited the ability to calculate an accurate total for training output, as reported 2015 output may not be typical.
Reliability and validity
No substantial inter-respondent disparities were apparent in respect of the data for any of the five countries. Triangulation through telephone interviews corroborated survey data.
Data were further assessed for internal consistency as follows for each country: (a) estimation of annual output through training based on reports for 2015, (b) multiplication of that figure by the number of years the course(s) have been in operation, and (c) the resulting number should be equal to or less than the number of children’s nurses on the register or reported to be in practice. It is recognised that student numbers may vary year to year in reality.
In the absence of participation by the South African Nursing Council, the reliability of the figure reported for South Africa (3200) was assessed through analysis of the annual reports produced by the South African Nursing Council relating to Additional Qualifications on the Register listed between 2010 and 2016 (3115) (South African Nursing Council, 2010–2016). It was not possible to perform this check for the other countries, either because registers were not available for inspection or because children’s nursing qualifications could not be disaggregated from published totals.
Discussion
The introduction of specialist children’s nurses into these health systems is still at an early stage, and training activity is on a small scale with only South Africa having more than one training centre. Three of the five countries began training children’s nurses less than 5 years ago. It is to be expected therefore that at this stage, the numbers of children’s nurses will be extremely small and inadequate to meet population needs. These limited data, obtained in the absence of reliable official information, identify for the first time a small but growing cohort of specialist children’s nurses within the five countries, supported by relatively recently established training activity in four of the five countries. South Africa has the largest training output, producing 179 children’s nurses per year on average. Average annual training output for the other four countries combined is 81 children’s nurses, meaning that total output across the five countries adds 260 children’s nurses to the workforce on average per year. Given the investment in health workforce development this represents, there is a need to consider how HRH information systems can best support informed decision making.
Investing in developing the children’s nursing workforce
The actions being taken to develop children’s nursing capacity identified through this study suggest that health service decision-makers in these countries believe that, in the context of a widening gap between the growing needs of an expanding child population and the ability of health systems to meet these needs, one justifiable response is to increase the capacity of the children’s nursing workforce. The impact on the wage bill of employing different groups of worker varies considerably. As Scheffler highlights, physicians are expensive, nurses somewhat less so, and lay health workers cheaper still [16]. At the same time, pre-service (basic) training, and by extension post-basic training, has to be seen as a long-term solution as it takes time for specialist nurses to reach their full capacity within the system [17]. In the context of the lower-resourced, demand-stretched healthcare systems considered by this study, the training activity documented represents a strategically significant investment in workforce development.
The composition as well as the size of the health workforce is an important consideration when seeking to manage health workforce shortages, requiring a focus on more than simply ‘strength in numbers’ [16, 18]. Specialist nurses may offer a cost-effective way to maximise the effectiveness of the health workforce in Africa, but intelligent development and deployment of this group of staff requires accurate workforce data to be available. It also requires decision makers to possess a clear strategic vision regarding the contribution of these nurses within a nation’s health system.
It is evident that the number of children’s nurses is extremely small in relation to the extensive child population. Taking Malawi as an example, the ratio of children’s nurses to children aged 0–15 is approximately one nurse per 83 696. Children’s nurses make up 1.9% of nurses on the register in Malawi, compared with 7% of nurses on the register in England [19]. It would be preferable to consider the data in relation to staffing levels and patterns of demand for care in paediatric wards and health facilities, but the ability to estimate workforce needs accurately for specialist nursing cadres in LMICs requires further development.
The envisaged role of children’s nurses in African health systems
Respondents in this small sample were able to articulate very clearly the type of contribution that children’s nurses make within their health systems. There is a need to better understand the rationale and the motivations behind the growth of training activity identified through this study. However, respondents’ comments suggest that children’s nurses in Africa’s health systems perform a wide variety of clinical, professional and organisational leadership roles, some of which have potentially far-reaching impacts on children’s health services and systems. The United Nations high-level commission on health employment and economic growth, with input from the International Council of Nurses, has articulated the need for a comprehensive approach to nursing workforce development, concluding that capacity building efforts must address both quantity and quality by developing nurses’ capacity to practise high-quality care; educate and train other health workers; lead effective teams, organisations and systems; and advocate for health in partnership with others [18].
The roles and contributions described by interviewees align with calls for investment in personal resilience and leadership capacity [20], quality of care and the capacity of clinical leaders to teach, support and manage [21, 22], at the same as increasing staff numbers. This is consistent with the global vision for nursing and midwifery development articulated by the World Health Organization, which sees an appropriately skilled nursing workforce as providing a cost-effective and efficient intersection for inter- and intra-disciplinary health actions, with the nursing workforce amplifying efforts to strengthen healthcare systems [2].
While the WHO’s global strategy points to a need for the nursing workforce to possess the skills and competencies required to serve specific population needs, there remains a need to better define what these skills and competencies are at a regional and country level across the countries in this study.
Monitoring the children’s nursing workforce
Specialist nurses may offer a cost-effective way to maximise the effectiveness of the health workforce in Africa, but intelligent development and deployment of this group of staff is only possible if accurate workforce data is available. Many policies dealing with the nursing workforce tend to assume that all nurses have similar qualifications and that it is efficient to deploy them interchangeably [23].
However, the information generated through this study regarding the extent of the registered children’s nursing workforce suggests that country-level HRH information systems continue to consider the nursing workforce as comprising generalists, with little apparent consideration of specialisation. Recording of the nursing workforce cannot sensibly be approached as though all nurses are generalists.
Limitations
None of the national nursing registries invited to participate in the study provided the information requested about the composition of the registered children’s nursing workforce and the approach to recording. Published information relating to the composition of the registered children’s nursing workforce was available for only one country (South Africa), based on statutory records acknowledged by the national Department of Health as ‘not a true reflection of the numbers of health professionals available for the workforce’ [14]. No attempt was made to establish, in relation to the numbers of children’s nurses reported, how many were active in the workforce and how many of those were working in paediatrics or child health. These questions will form the basis of further research.
The capacity of HRH information systems to monitor the children’s nursing workforce
There are widely acknowledged concerns regarding the capacity of nursing regulatory bodies to monitor and report on the nursing workforce in the countries concerned [6, 24, 25], and the literature suggests that nursing regulatory bodies in Kenya [26] and Uganda [27,28,29] appear to have participated in targeted capacity building interventions focusing on HRH information systems.
The Capacity Project provides an account of the experience of the individuals involved in developing a new HRH information system at Uganda’s national nursing registry, in a vividly descriptive report titled ‘I can now speak boldly’ [28]. The report speaks to feelings of deep responsibility on the part of regulators, a sense of guilt at the inadequacy of systems to respond to the need for information, as well as a wish to improve the situation. When effective systems were successfully implemented, registry staff reported satisfaction and professional pride.
While the reasons for non-participation by nursing regulatory bodies in this study are not known, it is possible that situations similar to the one described above may have influenced the decision of officials not to respond. This suggests that appropriately contextualised collaborative interventions to improve capacity to monitor the specialist registered children’s nursing workforce at country levels could be welcomed.
Conclusions
The efforts directed towards establishing a specialist children’s nursing workforce reported in this study point towards a need for HRH information systems to change in order to provide a sound basis for decisions about workforce composition, workforce development and training plans. The findings of this initial attempt to provide an estimation of the extent of the children’s nursing workforce in five selected African countries suggest that further action is needed to achieve a more finely grained understanding of the state of the specialist children’s nursing workforce, so that this growing population of children’s nurses can be developed and utilised to best effect within Africa’s health systems.
References
Bangdiwala SI, Fonn S, Okoye O, Tollman S. Workforce resources for health in developing countries. Pub Health Res. 2010;32(1):296.
World Health Organization. Global strategic directions for strengthening nursing and midwifery 2016–2020. Geneva: WHO Library; 2016.
World Health Organisation. Atlas of African health statistics 2018: health situation analysis of the African region. Geneva: WHO Library; 2018.
Gillespie R, Kyriacos U, Mayers P. The critical care nursing workforce in Western Cape hospitals-a descriptive survey. S Afr Crit Care J. 2008;22(2):50–6.
Swingler G, Hendricks M, Hall D, Hall S, Sanders D, McKerrow N, Saloojee H, Reid S. Can a new paediatric sub-specialty improve child health in South Africa? S Afr Med J. 2012;102(9):738–9.
CoMMiC. Second triennial report of the Committee on Morbidity and Mortality in Children Under 5 Years (CoMMiC). Pretoria; 2014. Available from: http://www.kznhealth.gov.za/mcwh/2nd-CoMMiC-Triennial-Report-2014.pdf
GHWA task force on scaling up education and training for health workers. Country case study: Malawi’s emergency human resources programme (Report). Geneva: WHO. nd. Available from http://www.who.int/workforcealliance/knowledge/case_studies/CS_Malawi_web_En.pdf.
Coetzee M, McKerrow NH, Chimwaza A, Molyneux E, North N, Sieberhagen S. Building paediatric nurse training capacity for Africa, in Africa. Lancet Glob Health. 2016;4(7):e449–50.
UNICEF. UNICEF global data: global and regional child deaths by cause. New York: UNICEF; 2016. Available from http://data.unicef.org/
USAID. Kenya Health System Assessment (2010). Maryland: Emory; 2010. Available from: https://www.hfgproject.org/wp-content/uploads/2015/02/Kenya-Health-Systems-Assessment-2010.pdf
Creswell JW, Klassen AC, Plano Clark VL, Smith KC. Best practices for mixed methods research in the health sciences, vol. 2013. Bethesda: National Institutes of Health; 2011. p. 541–5.
Johnson RB, Onwuegbuzie AJ, Turner LA. Toward a definition of mixed methods research. J Mix Methods Res. 2007;1(2):112–33.
Palys T. Purposive sampling. In: Given LM, editor. The Sage encyclopaedia of qualitative research methods, vol. 2. Adelaide: SAGE; 2008. p. 697–8.
South Africa Department of Health. HRH strategy for the health sector: 2012/13–2016/17. Pretoria: Department of Health; 2011. Available from: https://www.gov.za/documents/human-resources-health-south-africa-hrh-strategy-health-sector-201213-201617
La Pelle N. Simplifying qualitative data analysis using general purpose software tools. Field Methods. 2004;16(1):85–108.
Scheffler RM, Mahoney CB, Fulton BD, Dal Poz MR, Preker AS. Estimates of health care professional shortages in sub-Saharan Africa by 2015. Health Aff. 2009;28(5):w849–62.
Kinfu Y, Dal Poz MR, Mercer H, Evans DB. The health worker shortage in Africa: are enough physicians and nurses being trained? Bull World Health Organ. 2009;87(3):225–30.
World Health Organisation. Working for health and growth: investing in the health workforce. Report of the high-level commission on health employment and economic growth. Geneva: WHO Press; 2016.
National Health Service of England. NHS workforce statistics - October 2017, provisional statistics (including experimental report on mental health and learning disability workforce up until September 2017). London: NHS; 2017. Available from: https://digital.nhs.uk/data-and-information/publications/statistical/nhs-workforce-statistics/nhs-workforce-statistics-october-2017-provisional-statistics-including-experimental-report-on-mental-health-and-learning-disability-workforce-up-until-september-2017 Accessed 18 Dec 2018
Crisp N, Gawanas B. Scaling up, saving lives: task force for scaling up education and training for health workers. Geneva: Global Health Workforce Alliance; 2008. Available from: http://www.who.int/workforcealliance/documents/Global_HealthFINAL REPORT.pdf
Nakanjako D, Namagala E, Semeere A, Kigozi J, Sempa J, Ddamulira JB, Katamba A, Biraro S, Naikoba S, Mashalla Y, Farquhar C. Global health leadership training in resource-limited settings: a collaborative approach by academic institutions and local health care programs in Uganda. Hum Resour Health. 2015;13(1):87.
Nichols BL, Davis CR, Richardson DR. An integrative review of global nursing workforce issues. Annu Rev Nurs Res. 2010;28(1):113–32.
Uys LR, Klopper HC. What is the ideal ratio of categories of nurses for the South African public health system? S Afr J Sci. 2013;109(5–6):01–4.
Ditlopo P, Blaauw D, Rispel L, Thomas S, Bidwell P. Policy implementation and financial incentives for nurses in South Africa: a case study on the occupation-specific dispensation. Glob Health Action. 2013;6(1):19289.
World Health Organisation Zambia Country Office. WHO Zambia Annual Report 2015. Lusaka: WHO; 2015. Available from: https://afro.who.int/publications/annual-report-2015-who-country-office-zambia
Riley PL, Vindigni SM, Arudo J, Waudo AN, Kamenju A, Ngoya J, Oywer EO, Rakuom CP, Salmon ME, Kelley M, Rogers M. Developing a nursing database system in Kenya. J Healthc Res. 2007;42(3p2):1389–405.
Deussom R, Jaskiewicz W. Using evidence for human resources for health decision-making: an example from Uganda on health workforce recruitment and retention. Washington: IntraHealth; 2014. Report No. 15. Available from: https://www.capacityplus.org/files/resources/using-evidence-human-resources-health-decision-making.pdf
CapacityPlus. Building HR Information Systems: Leading the Way Together in Uganda. Washington: Intrahealth; 2007. Available from: https://www.intrahealth.org/features/voices-capacity-project-building-hr-information-systems%E2%80%94leading-way-together-uganda
The Capacity Project. “I can now speak boldly”: using quality data for health workforce planning in Uganda. Washington: IntraHealth; 2008. Available from: https://www.capacityproject.org/images/stories/Voices/voices_26.pdf
The current situation of children’s nursing training in South Africa: Masters in Public Health dissertation), University of Cape Town. Available from https://open.uct.ac.za/handle/11427/25017
World Bank. (2017). World Bank Health Data Bank estimates based on age/sex distributions of United Nations Population Division’s World Population Prospects. Available from http://data.worldbank.org/indicator/SP.POP.0014.TO.ZS Accessed April 14th 2017
WHO Global Health Workforce Observatory data. (Most recent available year). Available from http://apps.who.int/gho/data/node.main.HWF1?lang=en Accessed Dec. 17th 2018
Acknowledgements
The contributions of the respondents who gave their time and expertise are gratefully acknowledged. Uchenna Chukwu is acknowledged as the originator of the data relating to children’s nursing education programmes in South Africa, as credited in Tables 1 and 2.
Funding
The Child Nurse Practice Development receives funding from Elma Philanthropies, Vitol Foundation, Harry Crossley Foundation and the Children’s Hospital Trust.
Availability of data and materials
All original data created during this research is openly available from https://doi.org/10.5281/zenodo.1476499. This study involved re-analysis of existing data from a postgraduate study that is publicly available from http://hdl.handle.net/11427/25017.
Author information
Authors and Affiliations
Contributions
NN carried out all aspects of the research under the supervision of MC and MS-K. All authors contributed to the conceptualisation and preparation of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Human Research Ethics Committee of the University of Cape Town (HREC REF: 411/2017). Individual consent was provided by all respondents and participants.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
North, N., Shung-King, M. & Coetzee, M. The children’s nursing workforce in Kenya, Malawi, Uganda, South Africa and Zambia: generating an initial indication of the extent of the workforce and training activity. Hum Resour Health 17, 30 (2019). https://doi.org/10.1186/s12960-019-0366-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12960-019-0366-4