Abstract
Background
Sarcoma patients should be treated in high volume referral sarcoma centers. Compartmental resection is proposed as the best treatment option in retroperitoneal sarcoma patients.
Methods
Institute of Oncology Ljubljana is the only referral sarcoma center in Slovenia. Having a population of 2.1 million poses a unique situation. We manage all sarcoma patients in the country and operate on patients with soft tissue tumors of extremities, trunk, and abdomen. Data for all consecutive patients surgically treated from January 1999 to December 2018 for primary localized retroperitoneal sarcoma was extracted from a prospective surgical database. Data about the incidence of sarcoma patients in Slovenia was extracted from the Cancer Registry of Republic of Slovenia. Clinicopathologic variables and the outcome were analyzed.
Results
In total, 89 patients were included in the study. Median age was 62 years. Dedifferentiated liposarcoma was the most common histology (38.2%). Median tumor size was 21 cm. Compartmental resection was performed in 47.2% (42/89). Postoperative complication grade 3a or higher according to Clavien-Dindo classification had 30.3% (27/89) of patients. The 30-day and 90-day mortality rate was 2.2% and 5.6%. Median follow-up was 62.1 months. Corresponding 5-year overall survival was 67.2%, 5-year disease-specific survival was 72.6%, and 5-year local recurrence-free survival was 81.5%, respectively.
Conclusion
Results from our institution show that referral sarcoma centers may achieve very good results in management of retroperitoneal sarcoma patients, despite not meeting the criteria for high volume hospitals, as long as they have multidisciplinary team, appropriate facilities, and expertise.
Similar content being viewed by others
Background
Surgery is the mainstay of treatment in primary localized retroperitoneal sarcomas (RPS). Compartmental resection offers the best chance for local control and/or potential cure to the patients [1, 2]. This approach comprises an en bloc resection of tumor with kidney, colon, and psoas fascia or muscle. If other adjacent organs are infiltrated, they are resected en bloc as well comprising multivisceral resection. A benefit of preoperative radiotherapy is still under research; thus, it is not routinely recommended. The EORTC 62092 trial (STRASS) failed to demonstrate the benefit of preoperative radiotherapy in abdominal recurrence of RPS [3]. Final results and publications about the STRASS study are awaited. The role of chemotherapy in RPS has not been investigated in a randomized controlled trial. En bloc resections for retroperitoneal tumors have been performed at the Institute of Oncology Ljubljana since 1975 [4, 5]. Primary aim of the study was to analyze the quality of surgery and the outcome of RPS patients treated at our institution in the last two decades. Secondary aim was to analyze the same parameters comparatively for each decade.
Methods
Institutional Review Board (KSOPKR-0020/2020) and Ethical Committee (ERIDEK-0023/2020) approved the study. Clinicopathologic and follow-up data for all consecutive patients surgically treated for primary localized RPS at our institution from January 1999 to December 2018 was extracted from a prospective surgical database. Data about the incidence of sarcoma patients in Slovenia was extracted from the Cancer Registry of Republic of Slovenia.
Primary end point of the study was to investigate the quality of surgery in the last two decades by analyzing surgical resection margins, duration of surgery, blood loss, resection type, complication rates, and 30-day and 90-day postoperative mortality, and to analyze overall survival (OS), disease-specific survival (DSS), and local recurrence-free survival (LRFS). In the analysis of LRFS, deaths without evidence of disease and distant metastases (DM), whichever occurred first, were regarded as competing events. Concomitant local recurrence (LR) and DM were not included in the estimation of LRFS.
Surgical devices of the modern era enable more meticulous hemostasis and shorter operation time. There was also a change of generations of sarcoma surgeons at our institution during this technological development. For those reasons, we decided to investigate the same parameters comparatively for each decade as a secondary end point. The cohort was divided in two groups. Flowchart in Fig. 1 presents the process of patient selection. In the first group were those who underwent surgery in the period from 1999 to 2008, and in the second group those who underwent surgery in the period from 2009 to 2018. All cases were presented at the multidisciplinary sarcoma team (MDT) before treatment.
Clinical characteristics were summarized using frequencies and percentages for categorical variables and median and range for continuous variables. Chi-square test was used to compare categorical variables and t test for continuous variables. Survival curves were estimated by Kaplan-Meier method and compared by the log-rank test. Results were considered statistically significant if two-sided p value < 0.05 was achieved. Statistical analysis was carried out using SPSS version 25.
Results
There were 123 patients operated on for RPS at our institution in the study period. Patients with residual, recurrent, or primary metastatic disease at the referral among them were excluded from the analysis. In total, 89 patients with primary localized RPS were included in the study (Fig. 1). Median age of the patients was 62 years. At the referral, tumor was palpable in half of the cases (49.4%, 44/89) and 43.8% (39/89) of patients lost weight. In 25.8% (23/89), the tumor was coincidental finding. In the entire series, only 3 patients (3.4%) were operated on without the biopsy, 62.9% (56/89) had a fine needle aspiration, 23.6% (21/89) had core needle biopsy, and 10.1% of patients (9/89) had fine needle aspiration and core needle biopsy. Dedifferentiated liposarcoma was the most common histology (38.2%, 34/89). Median tumor size was 21 cm. Macroscopic complete resection (R0/R1) was achieved in all patients with microscopic negative margins in 76.4% (68/89). Compartmental resection was performed in 47.2% (42/89) and was extended into multivisceral resection in half of those cases (23.6%, 21/89). Only 2.2% (2/89) had the tumor removed without en bloc resection of any major organ. Organs were resected as follows: kidney in 57.3% (51/89), colon in 53.9% (48/89), adrenal in 42.7% (38/89), psoas fascia in 30.3% (27/89), psoas muscle in 28.1% (25/89), diaphragm in 20.2% (18/89), spleen and distal pancreas in 10.1% (9/89) each, inferior vena cava in 8.9% (8/89), and liver in 5.6% (5/89) of patients. Median number of resected organs per patient for the whole series was 4. Median hospital stay after surgery was 22 days. Postoperative complication grade 3a or higher according to Clavien-Dindo classification had 30.3% (27/89) of patients. Fifteen (16.9%, 15/89) required reoperation. The 90-day mortality rate was 5.6%. Reasons for reoperation and characteristics of patients who died within 90 days after surgery are summarized in Table 1.
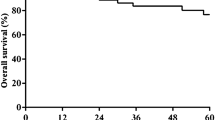
Median follow-up from surgery was 62.1 months. In total, 39 patients died. The corresponding 5-year OS and DSS were 67.2% and 72.6% (Fig. 2). Twenty-five (28.1%) patients developed LR. Fourteen (15.7%) patients had LR only, 3 patients had DM followed by LR, 6 patients had LR followed by DM, and 2 patients had concomitant LR and DM. The corresponding 5-year LRFS was 81.5% (Fig. 3).
By dividing the cohort in two groups, 41 were resected in the first period and 48 in the second. Clinicopathologic characteristics for the entire series and comparison for both periods are presented in Table 2. In the first period, none of the patients died within 90 days after surgery while in the second period 90-day mortality rate was 10.4%. In total, 22 (53.7%) patients from the first and 17 (35.4%) from the second period died. Median follow-up for the first and second period was 95.9 and 46.2 months. The corresponding 5-year OS (Fig. 4) and DSS were 72.8% and 79.6% for patients from the first and 62.9% and 66.4% for patients from the second period. The corresponding 5-year LRFS was 77.3% and 87.8% for the first and second period, respectively (Fig. 5). The differences in OS, DSS, and LRFS between the two periods were not statistically significant.
Nine patients (9.2%, 9/98) diagnosed with primary localized RPS in the study period were not surgically treated because of comorbidities (n = 5), old age (n = 2), irresectability (n = 1), and patient decision (n = 1).
Discussion
Management of sarcoma patients in referral sarcoma centers is organized in different ways. The Sarcoma Policy Checklist was created by European multidisciplinary expert group in 2017 recommending that each country should have at least one designated and accredited center of reference for sarcoma patients and that patients should receive multidisciplinary care delivered by a specialized sarcoma team [6]. Slovenia has a population of 2.1 million. From the referral sarcoma center point of view, this poses a unique situation. Institute of Oncology Ljubljana was established in 1938 and is the only referral sarcoma center in the country. Sarcoma MDT was established in 1975. It currently involves 23 dedicated sarcoma specialists with two specialized sarcoma surgeons, three orthopedic surgeons and a plastic surgeon. At the MDT, we manage all soft tissue and bone sarcoma patients in the country. We are the only institution having facilities for management and treatment. The highest incidence of soft tissue sarcoma patients in Slovenia in the study period was 112, noted in the national registry database in 2015 [7]. According to European Cancer Organisation recommendations, the institution is considered a sarcoma referral center if at least 100 new soft tissue and bone sarcoma patients are treated per year [8]. They also state that sarcoma surgeon should perform at least 2–3 sarcoma operations per month. We operate patients with soft tissue tumors of the extremities, trunk, superficial part of head and neck, retroperitoneum, pelvis, abdominal viscera, and pediatric sarcoma patients at the University Clinical Centre Ljubljana. In total, we perform around 70–80 sarcoma operations per year. Hospital case volume of our institution is about 90 cases per year and surgeon case volume is at least 2 sarcoma operations per month.
Recently, Villano et al. published a multi-institutional analysis of hospital volume-outcome relationship and identified 13 cases of RPS operations per year as a minimum volume threshold for optimal outcome [9]. Institutions meeting this threshold were declared as high volume hospitals (HVH). In our hospital, the average number of resections for primary RPS was 4.5 cases per year in the study period, not meeting the criteria for HVH. However, in the study period, we operated on 28 additional patients with recurrent or residual RPS which are often much more challenging and demanding than the primary ones. Furthermore, factors likely to play a major role in the outcome such as availability of MDT, surgeon case volume and experience, intensive care unit specialists, team for clinical nutrition, interventional radiologists, and others were not accounted for in their analysis. In our hospital, all the expertise mentioned needed for the optimal management of RPS patients is available. Our long-term results are comparable to the largest and most cited series of primary RPS, indicating that lower volume centers may achieve competitive results as long as they have appropriate facilities and expertise. Five-year OS and LRFS for the entire series from our institution were 67.2% and 81.5% and are comparable among other with results of the largest study so far, which included 1007 patients, reported in 2015 from the Transatlantic Retroperitoneal Sarcoma Working Group [10]. Comparison of the outcome data with reports from the literature is shown in Table 3.
Postoperative complication grade 3a or higher according to Clavien-Dindo classification had 30.3% of patients (Table 2) and 2.2% of patients died within 30 days after the operation. These data could be compared to Transatlantic Retroperitoneal Sarcoma Working Group report published by MacNeill et al. in 2018 where the rate of severe postoperative adverse events was 16.4% and 1.8% of patients died in the early postoperative period [19]. Our results are acceptable, but 90-day mortality rate of 10.4% in the second period was, however, high in our series (Table 1). In the future, we are going to try to adopt the enhanced recovery after surgery protocol to try to improve the results.
Finally, in a series of 89 consecutive patients surgically treated for primary localized RPS at our institution in a period of 20 years, 41 were treated in the first and 48 in the second decade. Comparing clinical and pathologic variables and the management of patients between the two periods, we found no major differences. Only variables that significantly differed were median time to treatment and proportion of R0 resection. Median time to treatment was more than twice as long in the second period. Possible reasons that might explain the difference are higher number of patients transferred directly from a local hospital to the Institute for treatment in the first period (26.8% vs 4.2%), higher number of patients having core needle biopsy in the second period (31.3% vs 2.4%), and a trend towards longer preparation for surgery with parenteral nutrition in the second period (11.5 days vs 8.2 days). The proportion of R0 resections in the second period was 85.4% almost 20% higher than in the first period. Possible reason could be a trend to smaller pathologic specimen. There was a trend towards overrepresentation of higher grade and smaller tumors in the second period, higher proportion of neoadjuvant radiotherapy in the second period, and smaller median weight of the specimen in the second period.
Certainly, there are some limitations to the study. The retrospective nature and a long time span of the study could cause potential selection bias. Low number of patients does not allow a large sample size which could affect the results. Nevertheless, the main strength of the study is to emphasize the crucial role of MDT and sarcoma surgeon in management of sarcoma patients.
In conclusion, our institution fulfills the criteria for a sarcoma referral center representing a low volume center for RPS patients. However, membership in the Transatlantic Australasian Retroperitoneal Sarcoma Working Group gives us the opportunity for education, international collaboration, research, and better understanding of the natural history of RPS in the effort for optimal treatment of RPS patients.
Conclusion
We are aware that HVH offer best chances for the optimal treatment to RPS patients, but results from our institution show that referral sarcoma centers may achieve very good results in management of these patients, despite not meeting the criteria for HVH, as long as they have MDT, appropriate facilities, and expertise.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- RPS:
-
Retroperitoneal sarcoma
- OS:
-
Overall survival
- DSS:
-
Disease-specific survival
- LRFS:
-
Local recurrence-free survival
- DM:
-
Distant metastases
- LR:
-
Local recurrence
- MDT:
-
Multidisciplinary team
- HVH:
-
High volume hospital
References
Bonvalot S, Rivoire M, Castaing M, Stoeckle A, Le Cesne A, Blay JY. Primary retroperitoneal sarcomas: a multivariate analysis of surgical factors associated with local control. J Clin Oncol. 2009; https://doi.org/10.1200/JCO.2008.18.0802.
Gronchi A, Lo Vullo S, Fiore M, Mussi C, Stacchiotti S, Collini P, et al. Aggressive surgical policies in a retrospectively reviewed single-institution case series of retroperitoneal soft tissue sarcoma patients. J Clin Oncol. 2009; https://doi.org/10.1200/JCO.2008.17.8871.
Bonvalot S, Gronchi A, Le Pechoux S, Swallow CJ, Strauss DC, Meeus P, et al. STRASS (EORTC 62092): A phase III randomized study of preoperative radiotherapy plus surgery versus surgery alone for patients with retroperitoneal sarcoma. J Clin Oncol. 2019; https://doi.org/10.1200/JCO.2019.37.15.
Erzen D, Sencar M, Novak J. Retroperitoneal sarcoma: 25 years of experience with aggressive surgical treatment at the Institute of Oncology. Ljubljana. J Surg Oncol. 2005; https://doi.org/10.1002/jso.20265.
Erzen D, Novak J, Spiler M, Sencar M. Aggressive surgical treatment of retroperitoneal sarcoma: long-term experience of a single institution. Surg Technol Int. 2007;16:97–106.
Kasper B, Lecointe-Artzner L, Wait S, Boldon S, Wilson R, Gronchi A, et al. Working to improve the management of sarcoma patients across Europe: a policy checklist. BMC Cancer. 2018; https://doi.org/10.1186/s12885-018-4320-y.
Zadnik V. Cancer in Slovenia 2015. Ljubljana: Institute of Oncology Ljubljana, Epidemiology and Cancer registry, Cancer Registry of Republic Slovenia; 2018.
Andritsch E, Beishon M, Bielack S, Bonvalot S, Casali P, Crul M, et al. ECCO essential requirements for quality cancer care: soft tissue sarcoma in adults and bone sarcoma. Crit Rev Oncol: A critical review. 2017; https://doi.org/10.1016/j.critrevonc.2016.12.002.
Villano AM, Zeymo A, Chan KS, Shara N, Al-Refaie WB. Identifying the minimum volume threshold for retroperitoneal soft tissue sarcoma resection: merging national data with consensus expert opinion. J Am Coll Surg. 2019; https://doi.org/10.1016/j.jamcollsurg.2019.09.013.
Gronchi A, Strauss DC, Miceli R, Bonvalot S, Swallow CJ, Hohenberger P, et al. Variability in patterns of recurrence after resection of primary retroperitoneal sarcoma (RPS). Ann Surg. 2016; https://doi.org/10.1097/sla.0000000000001447.
Kilkenny JW, Bland KI, Copeland EM. Retroperitoneal sarcoma: The University of Florida experience. J Am Coll Surg. 1996;182:329–39.
Lewis JJ, Leung D, Woodruff JM, Brennan MF. Retroperitoneal soft-tissue sarcoma: analysis of 500 patients treated and followed at a single institution. Ann Surg. 1998; https://doi.org/10.1097/00000658-199809000-00008.
Stoeckle E, Coindre JM, Bonvalot S, Kantor G, Terrier P, Bonichon F, et al. Prognostic factors in retroperitoneal sarcoma: a multivariate analysis of a series of 165 patients of the French Cancer Center Federation Sarcoma Group. Cancer. 2001; https://doi.org/10.1002/1097-0142(20010715)92:2<359:AID-CNCR1331>3.0.CO;2-Y.
Ferrario T, Karakousis CP. Retroperitoneal sarcomas: grade and survival. Arch Surg. 2003; https://doi.org/10.1001/archsurg.138.3.248.
Hassan I, Park SZ, Donohue JH, et al. Operative management of primary retroperitoneal sarcomas: a reappraisal of an institutional experience. Ann Surg. 2004; https://doi.org/10.1097/01.sla.0000108670.31446.54.
van Dalen T, Plooij JM, van Coevorden F, van Geel AN, Hoekstra HJ, Albus-Lutter C, et al. Long-term prognosis of primary retroperitoneal soft tissue sarcoma. Eur J Surg Oncol. 2007; https://doi.org/10.1016/j.ejso.2006.09.020.
Strauss DC, Hayes AJ, Thway K, Moskovic EC, Fisher C, Thomas JM. Surgical management of primary retroperitoneal sarcoma. Br J Surg. 2010; https://doi.org/10.1002/bjs.6994.
Toulmonde M, Bonvalot S, Méeus P, Stoeckle E, Riou O, Isambert N, et al. Retroperitoneal sarcomas: patterns of care at diagnosis, prognostic factors and focus on main histological subtypes: A multicenter analysis of the French Sarcoma Group. Ann Oncol. 2014; https://doi.org/10.1093/annonc/mdt577.
MacNeill A, Gronchi A, Miceli R, Bonvalot S, Swallow CJ, Hohenberger P, et al. Postoperative morbidity after radical resection of primary retroperitoneal sarcoma. Ann Surg. 2018; https://doi.org/10.1097/SLA.0000000000002250.
Acknowledgements
The authors gratefully acknowledge Mrs. Tina Žagar, PhD., from the Department of Epidemiology and Cancer Registry at the Institute of Oncology Ljubljana for providing data from cancer registry.
Funding
Nothing to declare.
Author information
Authors and Affiliations
Contributions
All authors helped in study design, interpreted, and critically revised the previous versions of the manuscript. MN collected part of the data and was a major contributor in writing the manuscript. AP performed the statistical analysis, interpreted the statistical data, and wrote part of the manuscript. MKP was the editor, MA created the tables, and DE collected major part of the data. All authors read and approved this version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Institutional Review Board (KSOPKR-0020/2020) and Ethical Committee (ERIDEK-0023/2020).
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Novak, M., Perhavec, A., Kerin Povšič, M. et al. Primary localized retroperitoneal sarcomas: report from Slovenian sarcoma referral center. World J Surg Onc 18, 277 (2020). https://doi.org/10.1186/s12957-020-02038-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12957-020-02038-9