Abstract
Background
Over the years, the scope of outcomes assessment in chronic obstructive pulmonary disease (COPD) has broadened, allowing for the evaluation of various patient-reported outcomes (PROs). As it still remains unclear whether and to what extent PROs mirror the exercise performance of patients with COPD, the current study aimed to assess the association between different exercise test outcomes and PROs, before and after pulmonary rehabilitation (PR).
Methods
Correlations between PROs used to describe health-related quality of life (HRQoL), mood status, level of care dependency and dyspnea in patients with COPD and commonly used laboratory- and field-based exercise test outcomes were evaluated in 518 individuals with COPD attending PR.
Results
Overall, correlations between PROs and exercise test outcomes at baseline were statistically significant. The correlation between modified Medical Research Council (mMRC) dyspnea score and 6-min walking distance (6MWD) was strongest (ρ:-0.65; p<0.001). HRQoL related PROs showed weak correlations with exercise outcomes at baseline. Moderate correlations were found between St George’s Respiratory Questionnaire total score and 6MWD (r:-0.53; p<0.001) and maximal workload achieved during cardiopulmonary exercise testing (ρ:-0.48; p<0.001); and between Clinical COPD Questionnaire (CCQ) total score and 6MWD (r:-0.48; p<0.001) and maximal workload (ρ:-0.43; p<0.001). When significant, correlations between changes in exercise test outcomes and changes in PROs after PR were generally very weak or weak. The highest correlation was found between changes in CCQ total score and changes in 6MWD (ρ: − 0.36; p<0.001).
Conclusions
PROs and exercise test outcomes, although significantly correlated with each other, assess different disease features in patients with COPD. Individual PROs need to be supported by additional functional measurements whenever possible, in order to get a more detailed insight in the effectiveness of a PR program.
Trial registration
Netherlands Trial Register (NL3263/NTR3416). Registered 2 May 2012.
Similar content being viewed by others
Background
Patients with chronic obstructive pulmonary disease (COPD), a highly-prevalent chronic lung disease, frequently suffer from symptoms of dyspnea, exercise intolerance, an impaired mood status and a reduced health status [1,2,3]. These features are typically weakly related to the degree of lung function impairment [4]. Therefore, the use of additional assessments such as exercise tests and patient-reported outcomes (PROs) has been advocated [3, 5, 6]. Appraisal of these extra-pulmonary features is necessary to better understand the patients’ daily needs or problems, to identify possible treatable traits for integrated COPD care programs, and to evaluate its efficacy [7].
Several laboratory- and field-based exercise tests can be performed to measure exercise performance, which is typically affected in patients with COPD [3, 8], due to a downward spiral of dyspnea, disability and physical inactivity [9]. Important aspects from the patient’s perspective like health-related quality of life (HRQoL), dyspnea, anxiety, depression, and the level of care dependency, all of which have a direct impact on daily life [10], are measured using PROs.
Punekar and colleagues systematically reviewed the strength of the available evidence supporting correlations between the outcomes of different exercise tests and PROs most commonly used to assess HRQoL and dyspnea [11]. They concluded that only a limited amount of studies have focused on the correlations between exercise test outcomes and PROs in patients with COPD. The available evidence indicates a very weak to moderate negative correlation between 6-min walking distance (6MWD) and HRQoL, measured with the St. George’s Respiratory Questionnaire (SGRQ). The relationship between PROs for dyspnea and 6MWD showed contrasting results, with both moderate to strong positive and negative correlations being reported [11]. So, it still remains unclear whether and to what extent PROs mirror the exercise performance of patients with COPD. It seems reasonable to hypothesize that other exercise test outcomes than 6MWD may be stronger correlated with different PROs. For example, disease-specific questionnaires like the Clinical COPD Questionnaire (CCQ) and the COPD Assessment Test (CAT) focus more on functional impairments and symptoms related to COPD and may therefore be more closely associated with exercise test outcomes in patients with COPD.
Pulmonary rehabilitation (PR) reduces dyspnea, increases exercise capacity, and improves HRQoL in individuals with COPD [6]. Exercise training is a major component of PR and therefore exercise test outcomes are consistently used to assess the individual patient’s response to PR [12,13,14,15,16,17]. Nevertheless, improvements in exercise performance after PR do not necessarily lead to a concurrent decrease in symptoms in patients with COPD and vice versa [18]. Therefore, the question remains whether changes in exercise test outcomes after PR translate into changes in disease-specific PROs.
In this observational study, we aimed to assess the association between different exercise test outcomes and PROs most commonly used to describe HRQoL, anxiety, depression and disease-specific symptoms, such as dyspnea, in patients with COPD before and after PR. A priori, we hypothesized that the correlation between PROs for dyspnea and HRQoL and exercise test outcomes would be statistically significant, but that there would be no strong or very strong association. Furthermore, it was expected that improvements in exercise test outcomes after PR showed weak correlations with changes in PROs in patients with COPD.
Methods
Study design and participants
The current study is a retrospective analysis of the ‘COPD, Health status and Comorbidities’ (Chance) study, Netherlands Trial Register NTR3416 [19]. The Medical Ethical Committee of the Maastricht University Medical Centre+ (MEC 11–3-070) approved this trial, which conformed to the ‘Declaration of Helsinki’ as amended most recently by the 64th WMA General Assembly, Fortaleza, Brazil, October 2013 [20]. The Medical Research Involving Human Subjects Act (WMO) does not apply for the secondary analysis of the Chance study. Therefore, an additional official approval of this secondary analysis by the Medical Ethical Committee is not required (MEC letter 2019–0987).
Patients with mild to very severe COPD were recruited before the start of a comprehensive PR program at CIRO in Horn, The Netherlands [21]. Patients between the age of 40 and 85 years with a diagnosis of COPD according to GOLD guidelines [22] were eligible. The protocol and part of the results of the Chance-study have been published before [1, 4, 10, 15, 19, 23,24,25,26]. All patients gave written informed consent prior to inclusion in the study.
PR program
PR took place inpatient (8 weeks, 5 sessions per week; total of 40 sessions) or outpatient (8 weeks, 3 sessions per week, followed by 8 weeks, 2 sessions per week; total of 40 sessions), in line with the 2013 American Thoracic Society & European Respiratory Society Statement [4]. Extensive pre- and post-PR assessments were performed, as described before [19].
Measurements
Demographics, body mass index (BMI), body composition (fat-free mass index) [27], smoking history were assessed, as part of standard care. Lung function was determined with standardized spirometry equipment of Masterlab (CareFusion, Hoechberg, Germany) [28].
To evaluate HRQoL, three disease-specific PROs, the CAT (range 0–40 points) [29], the CCQ (range 0–6 points) [30] and the COPD-specific version of the SGRQ (range 0–100 points) [31] were assessed in all participants. Mood status was measured with the Hospital Anxiety and Depression scale (HADS; range 0–21 points) [32]. Higher scores are equivalent to a decreased HRQoL and/or increase in symptoms of anxiety or depression, respectively. The mMRC dyspnea scale was used to establish functional impairment due to dyspnea [33]. The level of care dependency was determined at baseline with the Care Dependency Scale (CDS; range 15–75 points) with a lower score representing a higher level of care dependency [34].
The 6-min walking test (6MWT) [35], cardiopulmonary exercise test (CPET; only at baseline) [36] were used to assess exercise capacity. Exercise tolerance was determined as cycle endurance time (CET) during the constant work rate cycle test (CWRT) [37]. Functional mobility was measured with the Timed ‘Up and Go’ (TUG) test [15, 17]. Isokinetic quadriceps muscle function (i.e. strength and endurance/total work) was determined using a Biodex System 4 Pro (Biodex Medical Systems Inc., New York, USA) [38].
Statistical analyses
Analyses were performed using SPSS software (statistical package for the social sciences) for Windows (version 25.0). Results are presented as mean and standard deviation (SD), median and interquartile range (IQR), and/or proportions, as appropriate. Continuous variables were tested for normality. Differences at baseline between completers and non-completers were analyzed using independent samples T-tests or Mann-Whitney U tests. Correlations between PROs and exercise test outcomes were analyzed using Scatter plots and Pearson’s or Spearman’s correlations, as appropriate. The strength of correlations has been classified according to British Medical Journal guidelines, which regard significant correlation coefficients of 0–0.19 as very weak, 0.2–0.39 as weak, 0.4–0.59 as moderate, 0.6–0.79 as strong, and 0.8–1 as very strong [39]. A priori, the level of significance was set at ≤0.01.
Results
A total of 518 patients (55.6% male, age 64.1 ± 9.1 years) volunteered to participate and attended the pre-PR assessment. The mean baseline 6MWD was 424 ± 124 m and 25.1% of the patients had a 6MWD below 350 m [40] and in 74.7% of the patients, quadriceps muscle strength was less than 80% of the predicted value [41]. The PROs showed a high degree of dyspnea (80.7% with mMRC dyspnea grade of two or higher) [22], anxiety (34.8% with ≥10 points) [32], depression (33.4% with ≥10 points) [32], care dependency (28.5% with CDS total score of ≤68 points) [25], and an impaired HRQoL (81.9% with a SGRQ total score of ≥44 points; 75.0% with a CAT total score of ≥18 points; 76.7% CCQ total score of ≥1.9 points) [22]. Baseline characteristics, exercise test outcomes and PROs at baseline are presented in Table 1.
Correlations between exercise test outcomes and PROs at baseline
Overall, correlations between PROs and exercise test outcomes at baseline were statistically significant (Table 2). Of these, the correlation between mMRC score and 6MWD was the strongest (ρ: −0.65; p<0.001), which is visually presented in Fig. 1. A moderate correlation was found between mMRC score and CPET maximum workload (Wmax; ρ: −0.54; p<0.001), CPET peak oxygen uptake (VO2peak; ρ: −0.40; p<0.001), TUG time (ρ: 0.49; p<0.001), quadriceps total work (ρ: −0.43; p<0.001), respectively.
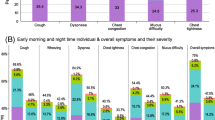
HRQoL PROs showed weak correlations with exercise outcomes at baseline. Moderate correlations were only found between SGRQ-C and 6MWD (r: −0.53; p<0.001) and CPET maximum workload (ρ: −0.48; p<0.001) and between CCQ and 6MWD (r: −0.48; p<0.001) and CPET maximum workload (ρ: −0.43; p<0.001). See Fig. 2 for a scatter plot illustrating the relationship between HRQoL PROs and 6MWD. CDS score was significantly correlated with all exercise test outcomes, with correlations ranging from 0.24 (CWRT cycle endurance time) to 0.50 (6MWD). Both HADS-D and HADS-A showed non-significant or very weak to weak correlations with all exercise test outcomes.
Left: Association between the SGRQ-C score (a), CAT score (b), CCQ score (c), and the 6MWD. Right: association between the change in SGRQ-C score (d), CAT score (e), CCQ score (f), and the change in 6MWD after PR. On the X-axis the MCID of 30 m for the 6MWT [42] is marked, on the Y-axis the MCIDs for SGRQ-C (−4.0), CAT (−2.0) and CCQ score (−0.4) are marked [10, 43]. MCID, minimal clinically important difference
Correlations between changes in exercise test outcomes and changes in PROs after PR
Four hundred nineteen patients completed the PR program. Completers and non-completers were comparable with respect to baseline characteristics (Table 1). Only the amount of current smokers was significantly higher in the non-completer group (p<0.001). All PROs and exercise test outcomes changed significantly after PR (Table S1). When significant, correlations between changes in exercise test outcomes and changes in PROs were generally very weak or weak. The highest correlation, being classified as weak, was found between ΔCCQ and Δ6MWD (ρ: −0.36; p<0.001; Fig. 2). Changes in other HRQoL PROs demonstrated similar association with changes in exercise test outcomes (Table 3). Changes in quadriceps peak muscle strength were not correlated with changes in any of the PROs.
Discussion
This study demonstrates that PROs and exercise test outcomes are associated to some extent in patients with mild to very severe COPD, but, in general, these correlations are weak to moderate. A strong relationship was merely found between the severity of dyspnea (mMRC) and distance covered in the 6MWT at baseline. In the current study, dyspnea tended to indicate at least moderate negative correlations with exercise test outcomes at baseline, suggesting that exercise performance decreases as dyspnea scores increase. However, these associations attenuated considerably or even became non-significant once the changes in dyspnea were correlated with changes in exercise test outcomes following PR, indicating that an improvement in exercise performance after PR does not necessarily imply that self-reported breathlessness decreases concurrently, like shown before [18]. As a side remark, it is important to note that correlations between changes in parameters are always lower than cross-sectional correlations. After all, the measurement error is included twice (pre vs. post) in the analysis, which always results in a weaker signal [44].
While the mMRC-scale is a unidimensional method to quantify only dyspnea, there are several multidimensional disease-specific PROs, which assess not only dyspnea but also other symptoms and perceived HRQoL in COPD [1]. Of these HRQoL PROs (CAT, CCQ, SGRQ), their association with exercise test outcomes was weak to moderate, indicating that no single exercise test accurately reflects HRQoL (or the other way around), proving that HRQoL is indeed a multi-dimensional concept that includes domains related to physical, mental, emotional, and social functioning. Overall, these results support the findings by Punekar et al. [11] who showed that generally there was a very weak to moderate negative correlation between the 6MWD and the SGRQ.
While guidelines on the diagnosis and treatment of COPD have intensively stated that the assessment of disease severity is substantially improved by using functional criteria [22], such as exercise capacity, the current study demonstrates that the variance in PROs can only be partially explained by attributes related to exercise performance. So, despite the fact that PROs for HRQoL, dyspnea, anxiety, depression and the level of care dependency are crucial when evaluating the disease severity and effectiveness of a treatment in COPD, it is justified to conclude that these PROs assess features not measured by exercise tests. Consequently, if we solely use a few outcome measures (for example, walking distance or HRQoL) to evaluate performance after PR, the clinical complexity and multidimensional aspect of PR in patients with COPD appears to be ignored [18].
In our study, the 6MWD showed the strongest relationship with important clinical PROs, underlining the fact that the 6MWT indeed seems to play a key role in evaluating functional exercise capacity [14]. Since the 6MWT is self-paced, test outcomes are likely to be affected by a patient’s mental and emotional status [3].
Limitations
Patients were solely recruited in a specialized PR centre, resulting in a selected group of COPD patients. This should be considered when applying results to other COPD samples. Furthermore, by quantifying the associated exercise limitation, a mMRC-score of 4 reflects the most disabled COPD patients who are not always able to perform a symptom-limited CPET, as a result of their dyspnea. In the current study, patients unable to perform a CPET and, concurrently, a CWRT were automatically excluded from the correlation analysis, since they did not present any values for both exercise tests, possibly affecting the correlation coefficients.
Conclusions
In conclusion, we have found that patient-reported outcomes and exercise test outcomes, although significantly correlated with each other, assess different disease features in patients with COPD. Therefore, it can be stated that relevant features from the patient’s perspective like HRQoL, anxiety, depression, and the level of care dependency are not an accurate reflection of a patient’s exercise capacity. The only exception to this seems to be dyspnea, the only PRO that tended to imply at least moderate association with exercise test outcomes. We would like to highlight the complexity of evaluating the effectiveness of a personalized PR program, in which we note that changes in PROs and changes in exercise test outcomes correlate poorly. Indeed, improvements in exercise capacity obtained after PR do not necessarily result in alterations in PROs in patients with COPD. Individual PROs need to be supported by additional functional measurements whenever possible, in order to get a more detailed insight in the effectiveness of a PR program.
Availability of data and materials
The datasets generated during and/or analyzed during the current study are available from the Board of Directors of CIRO on reasonable request and following the CIRO’s data request policy.
Abbreviations
- 6MWD:
-
Six-minute Walking Distance
- 6MWT:
-
Six-minute Walking Test
- BMI:
-
Body Mass Index
- CAT:
-
COPD Assessment Test
- CCQ:
-
Clinical COPD Questionnaire
- CDS:
-
Care Dependency Scale
- COPD:
-
Chronic Obstructive Pulmonary Disease
- CPET:
-
Cardiopulmonary Exercise Test
- CWRT :
-
Constant Work Rate (cycle) Test
- FEV1 :
-
Forced Expiratory Volume in One Second
- HADS:
-
Hospital Anxiety and Depression Scale
- HRQoL:
-
Health-Related Quality of Life
- IQR :
-
Interquartile Range
- mMRC:
-
modified Medical Research Council
- MEC:
-
Medical Ethics Committee
- PR:
-
Pulmonary Rehabilitation
- PRO:
-
Patient-reported Outcome
- SD:
-
Standard Deviation
- SGRQ-C :
-
St George’s Respiratory Questionnaire (COPD-specific version)
- TUG :
-
Timed Up and Go
- VO2peak :
-
Peak Oxygen Uptake
- Wmax :
-
Maximal Workload
- WMO:
-
Medical Research Involving Human Subjects Act
References
Smid DE, Spruit MA, Houben-Wilke S, Muris JWM, Rohde GGU, Wouters EFM, Franssen FME. Burden of COPD in patients treated in different care settings in the Netherlands. Respir Med. 2016;118:76–83.
Spruit MA, Pennings HJ, Janssen PP, Does JD, Scroyen S, Akkermans MA, Mostert R, Wouters EF. Extra-pulmonary features in COPD patients entering rehabilitation after stratification for MRC dyspnea grade. Respir Med. 2007;101:2454–63.
Spruit MA, Watkins ML, Edwards LD, Vestbo J, Calverley PM, Pinto-Plata V, Celli BR, Tal-Singer R, Wouters EF, Evaluation of CLtIPSEsi. Determinants of poor 6-min walking distance in patients with COPD: the ECLIPSE cohort. Respir Med. 2010;104:849–57.
Augustin IML, Spruit MA, Houben-Wilke S, Franssen FME, Vanfleteren L, Gaffron S, Janssen DJA, Wouters EFM. The respiratory physiome: clustering based on a comprehensive lung function assessment in patients with COPD. PLoS One. 2018;13:e0201593.
Agusti A, Calverley PM, Celli B, Coxson HO, Edwards LD, Lomas DA, MacNee W, Miller BE, Rennard S, Silverman EK, et al. Characterisation of COPD heterogeneity in the ECLIPSE cohort. Respir Res. 2010;11:122.
Spruit MA, Singh SJ, Garvey C, ZuWallack R, Nici L, Rochester C, Hill K, Holland AE, Lareau SC, Man WD, et al. An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. 2013;188:e13–64.
Wouters EF, Augustin IM. COPD health-care delivery: a holistic and dynamic approach is needed. Lancet Respir Med. 2016;4:e30–1.
Buekers J, Aerts JM, Theunis J, Houben-Wilke S, Franssen FME, Uszko-Lencer N, Wouters EFM, Simons S, De Boever P, Spruit MA. Kinetic analyses as a tool to examine physiological exercise responses in a large sample of patients with COPD. J Appl Physiol (1985). 2020;128(4):813–821.
Ramon MA, Ter Riet G, Carsin AE, Gimeno-Santos E, Agusti A, Anto JM, Donaire-Gonzalez D, Ferrer J, Rodriguez E, Rodriguez-Roisin R, et al. The dyspnoea-inactivity vicious circle in COPD: development and external validation of a conceptual model. Eur Respir J. 2018;52.
Smid DE, Franssen FM, Houben-Wilke S, Vanfleteren LE, Janssen DJ, Wouters EF, Spruit MA. Responsiveness and MCID estimates for CAT, CCQ, and HADS in patients with COPD undergoing pulmonary rehabilitation: a prospective analysis. J Am Med Dir Assoc. 2017;18:53–8.
Punekar YS, Riley JH, Lloyd E, Driessen M, Singh SJ. Systematic review of the association between exercise tests and patient-reported outcomes in patients with chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2017;12:2487–506.
Andrianopoulos V, Wagers SS, Groenen MT, Vanfleteren LE, Franssen FM, Smeenk FW, Vogiatzis I, Wouters EF, Spruit MA, Network CR. Characteristics and determinants of endurance cycle ergometry and six-minute walk distance in patients with COPD. BMC Pulm Med. 2014;14:97.
Burtin C, Franssen FME, Spruit MA. Should resistance training be targeted to a specific subgroup of patients with non-small cell lung cancer? - reply. Respirology. 2017;22:1474.
Holland AE, Spruit MA, Troosters T, Puhan MA, Pepin V, Saey D, McCormack MC, Carlin BW, Sciurba FC, Pitta F, et al. An official European Respiratory Society/American Thoracic Society technical standard: field walking tests in chronic respiratory disease. Eur Respir J. 2014;44:1428–46.
Mesquita R, Wilke S, Smid DE, Janssen DJ, Franssen FM, Probst VS, Wouters EF, Muris JW, Pitta F, Spruit MA. Measurement properties of the Timed Up & Go test in patients with COPD. Chron Respir Dis. 2016;13(4):344–352.
Singh SJ, Puhan MA, Andrianopoulos V, Hernandes NA, Mitchell KE, Hill CJ, Lee AL, Camillo CA, Troosters T, Spruit MA, et al. An official systematic review of the European Respiratory Society/American Thoracic Society: measurement properties of field walking tests in chronic respiratory disease. Eur Respir J. 2014;44:1447–78.
Mesquita R, Janssen DJ, Wouters EF, Schols JM, Pitta F, Spruit MA. Within-day test-retest reliability of the timed up & go test in patients with advanced chronic organ failure. Arch Phys Med Rehabil. 2013;94:2131–8.
Spruit MA, Augustin IM, Vanfleteren LE, Janssen DJ, Gaffron S, Pennings HJ, Smeenk F, Pieters W, van den Bergh JJ, Michels AJ, et al. Differential response to pulmonary rehabilitation in COPD: multidimensional profiling. Eur Respir J. 2015;46:1625–35.
Smid DE, Wilke S, Jones PW, Muris JW, Wouters EF, Franssen FM, Spruit MA. Impact of cardiovascular comorbidities on COPD assessment test (CAT) and its responsiveness to pulmonary rehabilitation in patients with moderate to very severe COPD: protocol of the chance study. BMJ Open. 2015;5:e007536.
WMA. World Medical Association Declaration of Helsinki: Ethical Principles for Medical Research Involving Human SubjectsWorld Medical Association Declaration of HelsinkiSpecial Communication. JAMA. 2013;310:2191–4.
Spruit MA, Vanderhoven-Augustin I, Janssen PP, Wouters EF. Integration of pulmonary rehabilitation in COPD. Lancet. 2008;371:12–3.
Global Strategy For The Diagnosis, Management, and Prevention of Chronic, Obstructive Pulmonary Disease, 2019 report [www.goldcopd.com].
Augustin IML, Wouters EFM, Houben-Wilke S, Gaffron S, Janssen DJA, Franssen FME, Spruit MA. Comprehensive lung function assessment Does not allow to infer response to pulmonary rehabilitation in patients with COPD. J Clin Med. 2018;8.
Houben-Wilke S, Spruit MA, Uszko-Lencer N, Otkinska G, Vanfleteren L, Jones PW, Wouters EFM, Franssen FME. Echocardiographic abnormalities and their impact on health status in patients with COPD referred for pulmonary rehabilitation. Respirology. 2017;22:928–34.
Janssen DJ, Wilke S, Smid DE, Franssen FM, Augustin IM, Wouters EF, Spruit MA. Relationship between pulmonary rehabilitation and care dependency in COPD. Thorax. 2016;71:1054–6.
Mesquita R, Franssen FM, Houben-Wilke S, Uszko-Lencer NH, Vanfleteren LE, Goertz YM, Pitta F, Wouters EF, Spruit MA. What is the impact of impaired left ventricular ejection fraction in COPD after adjusting for confounders? Int J Cardiol. 2016;225:365–70.
Moon JR, Stout JR, Smith-Ryan AE, Kendall KL, Fukuda DH, Cramer JT, Moon SE. Tracking fat-free mass changes in elderly men and women using single-frequency bioimpedance and dual-energy X-ray absorptiometry: a four-compartment model comparison. Eur J Clin Nutr. 2013;67(Suppl 1):S40–6.
Munnik P, Zanen P, Lammers JW. A comparison of lung function equipment with emphasis on interchangeability and methods. Physiol Meas. 2006;27:445–55.
Jones PW. COPD assessment test --rationale, development, validation and performance. COPD. 2013;10:269–71.
van der Molen T, Willemse BW, Schokker S, ten Hacken NH, Postma DS, Juniper EF. Development, validity and responsiveness of the clinical COPD questionnaire. Health Qual Life Outcomes. 2003;1:13.
Meguro M, Barley EA, Spencer S, Jones PW. Development and validation of an improved, COPD-specific version of the St. George Respiratory Questionnaire. Chest. 2007;132:456–63.
Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–70.
Mahler DA, Wells CK. Evaluation of clinical methods for rating dyspnea. Chest. 1988;93:580–6.
Janssen DJ, Wouters EF, Schols JM, Spruit MA. Care dependency independently predicts two-year survival in outpatients with advanced chronic organ failure. J Am Med Dir Assoc. 2013;14:194–8.
Hernandes NA, Wouters EF, Meijer K, Annegarn J, Pitta F, Spruit MA. Reproducibility of 6-minute walking test in patients with COPD. Eur Respir J. 2011;38:261–7.
ATS/ACCP. ATS/ACCP Statement on cardiopulmonary exercise testing. Am J Respir Crit Care Med. 2003;167:211–77.
van’t Hul A, Gosselink R, Kwakkel G. Constant-load cycle endurance performance: test-retest reliability and validity in patients with COPD. J Cardpulm Rehabil. 2003;23:143–50.
Franssen FM, Broekhuizen R, Janssen PP, Wouters EF, Schols AM. Limb muscle dysfunction in COPD: effects of muscle wasting and exercise training. Med Sci Sports Exerc. 2005;37:2–9.
Correlation and Regression [https://www.bmj.com/about-bmj/resources-readers/publications/statistics-square-one/11-correlation-and-regression].
Spruit MA, Polkey MI, Celli B, Edwards LD, Watkins ML, Pinto-Plata V, Vestbo J, Calverley PM, Tal-Singer R, Agusti A, et al. Predicting outcomes from 6-minute walk distance in chronic obstructive pulmonary disease. J Am Med Dir Assoc. 2012;13:291–7.
Seymour JM, Spruit MA, Hopkinson NS, Natanek SA, Man WD, Jackson A, Gosker HR, Schols AM, Moxham J, Polkey MI, Wouters EF. The prevalence of quadriceps weakness in COPD and the relationship with disease severity. Eur Respir J. 2010;36:81–8.
Polkey MI, Spruit MA, Edwards LD, Watkins ML, Pinto-Plata V, Vestbo J, Calverley PM, Tal-Singer R, Agusti A, Bakke PS, et al. Six-minute-walk test in chronic obstructive pulmonary disease: minimal clinically important difference for death or hospitalization. Am J Respir Crit Care Med. 2013;187:382–6.
Jones PW. St. George's respiratory questionnaire: MCID. Copd. 2005;2:75–9.
Bland JM, Altman DG. Measurement error and correlation coefficients. Bmj. 1996;313:41–2.
Acknowledgements
The authors would like to thank Professor W. Derave (Ghent University) and Dr. P. Klijn (Merem Hilversum) for their input and collaboration within the BASES-consortium, in the context of which the current manuscript was written.
Funding
The BASES project is supported by the Lung Foundation Netherlands (#5.1.18.232). The Chance project was supported by the Lung Foundation Netherlands (#3.4.10.015) and GlaxoSmithKline (SCO115406).
Author information
Authors and Affiliations
Consortia
Contributions
Drafting of the manuscript, RM, FMEF, MAS. Conception and design of the original study, SH-W, DJAJ, MAS. Acquisition and analysis of data, SH-W, DJAJ, MAS. Analysis and interpretation of data, RM, FMEF, MAS. Editing manuscript, AAFS, SH-W, DJAJ, CB, HWHH, BB, EFMW. All authors critically revised the article and gave final approval of this version to be submitted.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The COPD, health status and co-morbidities (Chance) study was approved by the local ethics committee of Maastricht University Medical Centre+, The Netherlands (MEC 11–3-070). All patients gave written informed consent.
Consent for publication
Not applicable.
Competing interests
DJAJ reports personal fees from Boehringer Ingelheim, personal fees from Novartis, personal fees from Astra Zeneca, outside the submitted work; FMEF reports grants and personal fees from AstraZeneca, personal fees from Boehringer Ingelheim, personal fees from Chiesi, personal fees from GlaxoSmithKline, grants and personal fees from Novartis, personal fees from TEVA, outside the submitted work; BB reports personal fees from AstraZeneca, personal fees from Boehringer Ingelheim bv, outside the submitted work; EFMW reports personal fees from Nycomed, personal fees from Boehringer Ingelheim BV, grants and personal fees from AstraZeneca, grants and personal fees from GlaxoSmithKline, personal fees from Novartis, personal fees from Chiesi, outside the submitted work; MAS reports grants from Lung Foundation Netherlands, grants from GlaxoSmithKline Netherlands, during the conduct of the study. RM, AAFS, SH-W, CB and HWHH have nothing to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1: Table S1.
Changes in PROs and exercise test outcomes after PR.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Meys, R., Stoffels, A.A.F., Houben-Wilke, S. et al. Association between patient-reported outcomes and exercise test outcomes in patients with COPD before and after pulmonary rehabilitation. Health Qual Life Outcomes 18, 300 (2020). https://doi.org/10.1186/s12955-020-01505-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12955-020-01505-x