Abstract
Background
Component-resolved diagnosis (CRD) allows to identify single molecular allergen components, and constitutes a routine practice in many allergy units. However, skin prick test (SPT) remains the technique of choice in many otorhinolaryngology departments, thus increasing the risk of using inadequate immunotherapies in patients with respiratory allergies. This study aimed to compare sensitization profiles determined by SPT and CRD in patients with respiratory allergy, and to explore the relationship between sensitization and type and severity of the respiratory disease.
Methods
Cross-sectional, multicenter study of patients admitted to the Otorhinolaryngology Department due to symptoms of respiratory allergy. Extracts from various house dust mites, pollens, and molds were tested by SPT, whereas IgE against the corresponding antigens were measured by CRD.
Results
The analysis included 101 patients. The sensitization profile obtained by SPT had low agreement with that of CRD, particularly to dust mite allergens (Dermatophagoides sp.) and pollens (Plantago lanceolata, Olea europaea, and Cupressus sempervirens). While SPT did not show any significant relationship between sensitization and type/severity of the respiratory disease, CRD allowed to associate Der p 1, Der f 1 and Lep d 2 sensitizations with asthma, and Der p 2, Der f 2 and Lep d 2 sensitizations with more severe symptoms of allergic rhinitis.
Conclusions
Compared with SPT, CRD enables to describe a more accurate sensitization profile and to identify associations between symptoms and specific antigens. The routine use of CRD in an otorhinolaryngology setting may benefit the management of patients with respiratory allergy.
Trial registration IB 3108/15 (Retrospectively registered)
Similar content being viewed by others
Background
Respiratory allergies, particularly allergic rhinitis and asthma, are amongst the most common allergies in industrialized areas. They constitute a major public health and economic problem worldwide because of their prevalence, morbidity, and impact on quality of life [1,2,3]. Of all allergens that can elicit respiratory allergic reactions, grass pollen and house dust mites have been identified as the most prevalent [4, 5]. However, many patients are sensitized to various allergic sources, either as a result of multiple allergic responses or due to the presence of cross-reactants or panallergens [6]. This phenomenon often hinders the correct identification of the allergen source, which may ultimately lead to an inadequate diagnosis or treatment of the allergic disease [7,8,9].
The diagnosis of allergic diseases has been traditionally based on patient anamnesis, supported by skin prick test (SPT) and/or the identification of serum IgE in whole allergen extracts. Both methods are suitable for detecting reactivity against allergen extracts but fail to identify the specific disease-eliciting molecules. The development of the component-resolved diagnosis (CRD), also known as molecular diagnosis, has allowed to identify single molecular allergen components responsible for sensitization [10]. This feature, which allows to distinguish symptom-eliciting allergens from those attributable to cross-reactivity, has become particularly relevant since the advent of allergen-specific immunotherapy [10,11,12]. While CRD has been increasingly established as routine practice in many allergy units, SPT remains the technique of choice in many otorhinolaryngology departments because of its lower cost, thus increasing the risk of using inadequate immunotherapies in patients with respiratory allergies [7, 13].
Subjects living in areas with high allergy burden (e.g., Mediterranean countries) are more prone to sensitizations to minor allergens; therefore, these areas often show a higher prevalence of polysensitized patients. In this scenario, the identification of disease-eliciting molecules provided by CRD becomes even more relevant in terms of using accurate immunotherapies. In this cross-sectional study, we compared sensitization profiles determined by SPT and CRD in patients with respiratory allergy from a Mediterranean area and explored the relationship between sensitization and type and severity of the respiratory disease.
Methods
Study design and patients
This was a cross-sectional study of consecutive patients admitted to the otorhinolaryngology department of three hospitals in the Balearic Islands (Spain) due to symptoms of respiratory allergy between October 2012 and November 2013. The inclusion was restricted to patients of both sexes, aged between 7 and 60 years, who had been living in the same area for at least 5 years, had experienced symptoms of a respiratory allergic disease (i.e., rhinitis, asthma or both) for at least 2 years and had a positive reaction to an allergen as determined by SPT. Patients who received immunotherapy within 5 years prior to admission or who had no diagnostic tests performed were excluded from the dataset.
Variables and endpoints
Demographic and clinical characteristics included age, sex, time from symptoms onset to diagnosis, type of respiratory allergic disease (rhinitis, asthma or rhinitis with concomitant asthma), frequency of symptoms (perennial or seasonal), and severity of the allergic disease, which was rated as mild or moderate-to-severe, based on the Spanish guidelines on the management of asthma (GEMA) [14, 15] and allergic rhinitis with impact on asthma (ARIA) [16]. Other clinical data included concomitant food allergies, and personal and/or family history of allergy. Allergen sensitization was determined using both SPT and CRD. Patients sensitized to more than one extract (SPT) or to specific IgE of more than one species (CRD) were considered polysensitized.
Skin prick test, performed according to the European Academy of Allergy and Clinical Immunology guidelines [17], was considered positive if wheals and flares were observed within 15 min, and wheal mean diameter was ≥ 3 mm. The following extracts were tested by SPT: House dust mites Dermatophagoides pteronyssinus, Dermatophagoides farinae, and Lepidoglyphus destructor; pollens Olea europaea, Artemisia vulgaris, Plantago lanceolata, Platanus hispanica, Parietaria judaica, Salsola kali, Cupressus sempervirens, and grass mixture; molds Alternaria alternata. Panallergen profilins, polcalcins, non-specific lipid transfer proteins (nsLTPs), and tropomyosins were also analyzed. Histamine and saline solution were used as positive and negative controls, respectively. Allergen extracts were provided by ALK-Abelló, S.A. (Madrid, Spain).
Allergen-specific IgE was quantified using chemiluminescent acridinium on the ADVIA Centaur platform (Bayer HealthCare LLC, Diagnostics Division, Tarrytown, NY, USA) as described by Petersen et al. [18]. CRD was considered positive when binding values exceeded 0.35 kU/L. The CRD analysis screened the presence of specific IgE against the following molecules: Der p 1 and 2, Der f 1 and 2, and Lep d 2; Ole e 1 and 9, Art v 1, Pla l 1, Phl p 1 and 5, Pla a 1 and 2, Par j 2, Sal k 1, Cup s 1;Alt a 1; Pho d 2, Che a 3, Pru p 3, Der p 10, and Pen a 1.
Statistics
Quantitative variables are described as mean and standard deviation (SD) or as median and interquartile range (IQR), whereas categorical variables are presented as frequencies and percentages. Differences between groups (according to type and severity of the disease, frequency of symptoms, diagnostic method) were analyzed using the Fisher exact test or the non-parametric Wilcoxon test. Concordance between SPT and CRD methods was assessed by Cohen’s kappa coefficient (κ). Associations between demographic and clinical factors and the most prevalent sensitizations were determined by logistic regression analyses, with age, time from onset of symptoms to diagnosis, type and severity of the disease and concomitant food allergies as the independent variables. The threshold for statistical significance was established at a two-sided alpha value of 0.05. All statistical analyses were performed using the SAS 9.3 software.
Results
Characteristics of study patients
The analysis included 101 patients, whose demographic and clinical characteristics are summarized in Table 1. Time from onset of respiratory symptoms to diagnosis ranged from 1 to 30 years, with no differences regarding the frequency of symptoms: the mean (SD) for patients with perennial and seasonal symptoms was 7.7 (6.6) and 10.6 (8.0) years, respectively (p = 0.092). The most common allergic disease was rhinitis alone, followed by rhinitis with asthma. Asthma alone was present only in two patients (2%); therefore, for subsequent analyses, these patients were included in a group encompassing all patients with asthma, either alone or with concomitant rhinitis.
Sensitization profile
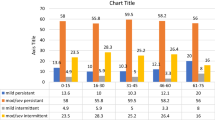
Table 2 shows the sensitization profiles obtained with each diagnostic method. Most prevalent sensitizations, present in more than 20% of patients, were to D. pteronyssinus (Der p 1 and 2), D. farinae (Der f 1 and 2), L. destructor (Lep d 2), Olea europaea (Ole e 1), and Phleum pratense (Phl p 1) allergens. The percentage of sensitized patients was significantly higher with SPT than CRD for Der p 1 and 2, Der f 1 and 2, Lep d 2, Ole e 1, Pla l 1, and Sal k 1. However, Alt a 1 and Pru p 3 showed a lower percentage of sensitized subjects when SPT was used compared with CRD. Overall, 91 (93.8%) and 72 (79.1%) patients were polysensitized according to SPT and CRD tests, respectively. The results regarding the quantitative determination of allergen-specific IgE are summarized in Additional file 1: Table S1.
Cohen’s kappa of SPT vs. CRD for allergens with significant differences in the sensitization profile revealed low agreement between both diagnosis methods: κ = 0.12 (95% CI − 0.10, 0.35) for D. pteronyssinus vs. Der p 1 and 2; κ = − 0.05 (95% CI − 0.12, 0.01) for D. farinae vs. Der f 1 and 2;κ = 0.05 (95% CI − 0.08, 0.19) for L. destructor vs. Lep d 2; κ = − 0.01 (95% CI − 0.20, 0.17) for O. europaea vs. Ole e 1 and 9; and κ = 0.07 (95% CI − 0.09, 0.23) for P. lanceolata vs. Pla l 1 and 2. Cohen’s kappa could not be determined for Sal k 1 and Alt a 1.
Association between allergens and diseases
Table 3 summarizes the association between allergen sensitizations and type of respiratory allergic disease. SPT did not reveal significant associations, except for the extract of P. lanceolata, the sensitization to which was more frequent in patients with rhinitis than those with asthma (with or without concomitant rhinitis). On the other hand, sensitization to house dust mite allergens Der p 1, Der f 1 and Lep d 2 were significantly more frequent in patients with asthma (with or without concomitant rhinitis) compared to patients with rhinitis alone (Table 3).
When analyzing disease severity regarding sensitization to specific molecules, sensitization to Der p 2, Der f 2, and Lep d 2 appeared to be associated with moderate-to-severe rhinitis (Table 4). This trend was not observed in the corresponding primary antigens of Dermatophagoides sp. Der p 1 and Der f 1.
Demographic and clinical factors influencing sensitization
The results of the multivariate analysis to predict sensitization to each of the most prevalent antigens based on clinical and demographic characteristics are summarized in Table 5. The analysis failed to yield a multivariate model to predict sensitization to plant antigens Ole e 1 and Phl p 1. On the other hand, either the type or severity of the disease significantly contributed to sensitization toall house dust mite allergens included in the analysis (Table 5).
Discussion
In this cross-sectional study, we found that the sensitization profile of patients with respiratory allergy obtained by the traditional SPT has low agreement with that of CRD, particularly to dust mite allergens and pollens, such as P. lanceolata, O. europaea, and C. sempervirens. Furthermore, whereas SPT failed to reflect a significant relationship between sensitization and type/severity of the respiratory disease, CRD allowed to identify Der p 1, Der f 1 and Lep d 2 as antigens more frequently associated with asthma, and Der p 2, Der f 2 and Lep d 2 as antigens associated with more severe symptoms in patients with allergic rhinitis.
The low agreement between SPT and CRD observed in our analysis is consistent with that reported by previous authors [19, 20]. One of the major consequences of inconsistency in sensitization profiles is the inaccurate prescription of immunotherapy for patients with respiratory symptoms. In this regard, some authors have observed that the choice of immunotherapy may vary in about 55% of cases after comparing SPT and CRD sensitization profiles [7, 13] and that respondent rates increase when immunotherapy is used based on CRD results [9]. In this study, the number of sensitizations diagnosed by CRD was generally lower than those identified by SPT, being P. lanceolata the allergen that showed the greater difference (prevalence was 80% lower with CRD than with SPT). This finding was in line with that reported by Orovitg et al. [20]. and confirms Pla l 1 as a minor allergen eliciting respiratory allergic diseases in Mediterranean areas. Although this significant difference in sensitization to P. lanceolata could be attributed to the presence of panallergens (e.g., profilin), the small number of patients sensitized to panallergens in our study prevented further analyses in this regard. Other pollens with a strong presence in Mediterranean areas, such as Olea sp. [21], followed the same trend, albeit in a lesser extent. Of note, the differences between SPT and CRD for Olea sp. pollens found in our cohort were similar than those reported by previous authors in areas with higher prevalence of these pollens [20, 22]. Unlike plant antigens, the proportion of patients sensitized to LTPs (Pru p 3) and A. alternata were higher with CRD than SPT. Although our analysis does not allow us to draw strong conclusions in this regard, the cross-reactivity described for Art v 3 and Pru p 3 may have contributed to this observation [20].
The association between sensitization to specific allergens and the occurrence of respiratory diseases such as asthma and rhinitis has motivated the use of immunotherapy in those patients [23, 24]. In fact, allergen-specific immunotherapy is currently the only causal treatment for allergic rhinitis that can reduce its symptoms and the need for medical therapies [25]. However, in routine clinical practice, these therapies are often based on SPT diagnoses, assuming sensitization to main allergens. In our cohort, sensitization profiles determined by SPT did not reveal significant a relationship between sensitization and either the type of respiratory allergy or symptom severity. Conversely, CRD allowed to associate sensitizations to Der p 1, Der f 1 and Lep d 2 with asthma (with or without concomitant rhinitis), and sensitizations to Der p 2, Der f 2 and Lep d 2 with moderate-to-severe diseases in patients with rhinitis. Consistently with this finding, the multivariate analysis showed that the type of disease significantly contributed to sensitization to group 1 (Der p 1 and Der f 1) house dust mite allergens, whereas the severity of the disease significantly influenced sensitization to group 2 (Der p 2 and Der f 2) house dust mite allergens; sensitization to Lep d 2 was associated with both the type and severity of the disease. Similar relationships have been reported between various pollens and the type of respiratory disease [22, 26, 27]; however, to our knowledge, this is the first study showing a relationship between disease type/severity and house dust mite allergens. Although evidence regarding these specific relationships is still weak, consistent findings that specific antigens are associated with clinical characteristics of the respiratory disease strengthen the importance of using CRD to assess the sensitization profile of patients with respiratory allergy.
The main limitation of our study was its cross-sectional design, which restricted data collection to a particular period of the year for each patient, thus losing sight of changes in sensitization profiles caused by variations in antigen prevalence throughout the seasons. Although most patients in our cohort had perennial symptoms (and, therefore, were expected to show consistent sensitization profiles throughout the year), sensitization to pollens has a high seasonal variability in our area [21]. Another limitation of our results was the low prevalence of panallergens found in our study cohort. The presence of these allergens, which is commonly higher in other studies [20, 22, 27], has been considered a key benefit of CRD and may increase the differences between the two types of diagnosis.
Conclusions
Our results emphasize the limitations of SPT to determine sensitization profiles of patients with respiratory allergy in an otorhinolaryngology setting. Although the relationship between symptoms and specific antigens is still poorly understood, the ability of CRD to depict more accurate sensitization profiles and identify candidates to symptom-triggering antigens indicates that the routine use of CRD in this setting may provide remarkable benefits for the management of patients with respiratory allergy. The assessment of the cost-effectiveness of this approach in future studies is warranted.
Abbreviations
- CRD:
-
component-resolved diagnosis
- nsLTPs:
-
non-specific lipid transfer proteins
- SPT:
-
skin prick test
References
Dahl R, Andersen PS, Chivato T, Valovirta E, de Monchy J. National prevalence of respiratory allergic disorders. Respir Med. 2004;98:398–403. https://doi.org/10.1016/j.rmed.2003.11.015.
Simoens S. The cost-effectiveness of immunotherapy for respiratory allergy: a review. Allergy Eur J Allergy Clin Immunol. 2012;67:1087–105. https://doi.org/10.1111/j.1398-9995.2012.02861.x.
Meltzer EO, Bukstein DA. The economic impact of allergic rhinitis and current guidelines for treatment. Ann Allergy Asthma Immunol Off Publ Am Coll Allergy Asthma Immunol. 2011;106:S12–6. https://doi.org/10.1016/j.anai.2010.10.014.
Bousquet PJ, Burbach G, Heinzerling LM, Edenharter G, Bachert C, Bindslev-Jensen C, et al. GA2LEN skin test study III: minimum battery of test inhalent allergens needed in epidemiological studies in patients. Allergy Eur J Allergy Clin Immunol. 2009;64:1656–62. https://doi.org/10.1111/j.1398-9995.2009.02169.x.
Roberts G, Peckitt C, Northstone K, Strachan D, Lack G, Henderson J, et al. Relationship between aeroallergen and food allergen sensitization in childhood. Clin Exp Allergy J Br Soc Allergy Clin Immunol. 2005;35:933–40. https://doi.org/10.1111/j.1365-2222.2005.02280.x.
Ferreira F, Wolf M, Wallner M. Molecular approach to allergy diagnosis and therapy. Yonsei Med J. 2014;55:839–52. https://doi.org/10.3349/ymj.2014.55.4.839.
Sastre J, Landivar ME, Ruiz-García M, Andregnette-Rosigno MV, Mahillo I. How molecular diagnosis can change allergen-specific immunotherapy prescription in a complex pollen area. Allergy Eur J Allergy Clin Immunol. 2012;67:709–11. https://doi.org/10.1111/j.1398-9995.2012.02808.x.
Letrán A, Espinazo M, Moreno F. Measurement of IgE to pollen allergen components is helpful in selecting patients for immunotherapy. Ann Allergy Asthma Immunol. 2013;111:295–7. https://doi.org/10.1016/j.anai.2013.07.005.
Lepage-Nefkens I, Van der Maas M, Rijnen M, Hermansson L. A cost-effectiveness model evaluating component-resolved diagnosis (Crd) versus standard testing method (Skin Prick Testing (Spt)) in the diagnosis and treatment of allergic rhinitis in the Netherlands. Value Health. 2015;18:A359. https://doi.org/10.1016/j.jval.2015.09.689.
Kazemi-Shirazi L, Niederberger V, Linhart B, Lidholm J, Kraft D, Valenta R. Recombinant marker allergens: diagnostic gatekeepers for the treatment of allergy. Int Arch Allergy Immunol. 2002;127:259–68. https://doi.org/10.1159/000057742.
Melioli G, Passalacqua G, Canonica GW, Baena-Cagnani CE, Matricardi P. Component-resolved diagnosis in pediatric allergic rhinoconjunctivitis and asthma. Curr Opin Allergy Clin Immunol. 2013;13:446–51. https://doi.org/10.1097/ACI.0b013e32836274d8.
Van Gasse AL, Mangodt EA, Faber M, Sabato V, Bridts CH, Ebo DG. Molecular allergy diagnosis: status anno 2015. Clin Chim Acta Int J Clin Chem. 2015;444:54–61. https://doi.org/10.1016/j.cca.2015.02.012.
Letrán A, Espinazo M, Moreno F. Measurement of IgE to pollen allergen components is helpful in selecting patients for immunotherapy. Ann Allergy Asthma Immunol Off Publ Am Coll Allergy Asthma Immunol. 2013;111:295–7. https://doi.org/10.1016/j.anai.2013.07.005.
Caballero Martínez F, Plaza V, Quirce Gancedo S, Fernández Benítez M, Gómez Ruiz F, López Viña A, et al. External assessment of the GEMA2009 recommendations by a multidisciplinary expert panel on asthma. Arch Bronconeumol. 2010;46:411–9. https://doi.org/10.1016/j.arbres.2010.05.004.
Executive Committee GEMA 2009. GEMA 2009 (Spanish guideline on the management of asthma). J Investig Allergol Clin Immunol. 2010;20(Suppl 1):1–59.
Bousquet J, Schünemann HJ, Samolinski B, Demoly P, Baena-Cagnani CE, Bachert C, et al. Allergic rhinitis and its impact on asthma (ARIA): achievements in 10 years and future needs. J Allergy Clin Immunol. 2012;130:1049–62. https://doi.org/10.1016/j.jaci.2012.07.053.
Dreborg S. Skin testing. The safety of skin tests and the information obtained from using different methods and concentrations of allergen. Allergy. 1993;48:473–5.
Petersen AB, Gudmann P, Milvang-Grønager P, Mørkeberg R, Bøgestrand S, Linneberg A, et al. Performance evaluation of a specific IgE assay developed for the ADVIA centaur immunoassay system. Clin Biochem. 2004;37:882–92. https://doi.org/10.1016/j.clinbiochem.2004.06.010.
Lizaso MT, García BE, Tabar AI, Lasa E, Echechipía S, Lvarez MJ, et al. Comparison of conventional and component-resolved diagnostics by two different methods (Advia-Centaur/Microarray-ISAC) in pollen allergy. Ann Allergy Asthma Immunol. 2011;107:35–41. https://doi.org/10.1016/j.anai.2011.03.017.
Orovitg A, Guardia P, Barber D, de la Torre F, Rodríguez R, Villalba M, et al. Enhanced diagnosis of pollen allergy using specific immunoglobulin E determination to detect major allergens and panallergens. J Investig Allergol Clin Immunol. 2011;21:253–9.
Boi M, Llorens L. Annual pollen spectrum in the air of Palma de Mallorca (Balearic Islands, Spain). Aerobiologia. 2013;29:385–97. https://doi.org/10.1007/s10453-013-9288-0.
Barber D, de la Torre F, Feo F, Florido F, Guardia P, Moreno C, et al. Understanding patient sensitization profiles in complex pollen areas: a molecular epidemiological study. Allergy. 2008;63:1550–8. https://doi.org/10.1111/j.1398-9995.2008.01807.x.
Pfaar O, Demoly P, Gerth van Wijk R, Bonini S, Bousquet J, Canonica GW, et al. Recommendations for the standardization of clinical outcomes used in allergen immunotherapy trials for allergic rhinoconjunctivitis: an EAACI position paper. Allergy. 2014;69:854–67. https://doi.org/10.1111/all.12383.
Wahn U. Preventing new sensitization and asthma onset by allergen immunotherapy: the current evidence. Curr Opin Allergy Clin Immunol. 2017;17:443–6. https://doi.org/10.1097/ACI.0000000000000399.
Petalas K, Durham SR. Allergen immunotherapy for allergic rhinitis. Rhinology. 2013;51:99–110. https://doi.org/10.4193/Rhino12.086.
Cipriani F, Mastrorilli C, Tripodi S, Ricci G, Perna S, Panetta V, et al. Diagnostic relevance of IgE sensitization profiles to eight recombinant Phleum pratense molecules. Allergy. 2018;73:673–82. https://doi.org/10.1111/all.13338.
Segura N, Abos T, Compaired JA, Compés E, Guallar I, Morales M, et al. Influence of profilin on sensitisation profiles determined by cutaneous tests and IgE to major allergens in polysensitised patients. Clin Transl Allergy. 2016;6:23. https://doi.org/10.1186/s13601-016-0114-y.
Authors’ contributions
GTP conceived and designed the study, performed the analysis, interpreted the data, and was a major contributor in writing the manuscript. All authors participated in data collection, and thoroughly revised the various drafts of the manuscript. All authors read and approved the final manuscript.
Acknowledgements
The authors would like to thank Fernando de la Torre for thoroughly revising the manuscript text, and BioClever2005 S.L. for providing statistical and medical writing support.
This was a cross-sectional study of consecutive patients admitted to the otorhinolaryngology department of three hospitals in the Balearic Islands (Spain) due to symptoms of respiratory allergy between October 2012 and November 2013.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The study protocol was approved by the independent Ethics Committee of the Balearic Islands. All patients signed an informed consent to participate in this study.
Funding
The study was partially funded by ALK-abelló S.A., who afforded the statistical support.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Additional file
Additional file 1: Table S1.
Quantitative determination of allergen-specific IgE.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Til-Pérez, G., Carnevale, C., Sarría-Echegaray, P.L. et al. Sensitization profile in patients with respiratory allergic diseases: differences between conventional and molecular diagnosis (a cross-sectional study). Clin Mol Allergy 17, 8 (2019). https://doi.org/10.1186/s12948-019-0112-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12948-019-0112-4