Abstract
Background
The contractile response of patients with heart failure (HF) may be assessed by exercise stress echocardiography (ESE)-derived indexes. We sought to test whether ESE parameters are useful to identify the risk of adverse left ventricular (LV) remodeling in patients with chronic HF and reduced or mildly reduced LV ejection fraction (EF).
Methods
We enrolled 155 stabilized patients (age: 62 ± 11 years, 17% female, coronary artery disease 47%) with chronic HF, LV EF ≤50% and LV end-diastolic volume index > 75 ml/m2. All patients underwent a symptom-limited graded bicycle semi-supine ESE, with evaluation of peak stress LV EF, end-systolic pressure-volume relation (ESPVR, i.e. LV elastance) and cardiac power output to LV mass (CPOM). A complete echocardiographic study was performed at baseline and after 6 ± 3 months. Adverse LV remodeling was defined as the association of eccentric LV hypertrophy (LV mass: ≥115 g/m2 for male and ≥ 95 g/m2 for women, and relative wall thickness < 0.32) with an increase in LV end-systolic volume index ≥10% at six months.
Results
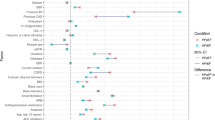
Adverse LV remodeling was detected in 34 (22%) patients. After adjustment for clinical, biochemical and echocardiographic data, peak ESPVR resulted in the most powerful independent predictor of adverse LV remodeling (OR: 12.5 [95% CI 4.5–33]; p < 0.0001) followed by ischemic aetiology (OR: 2.64 [95% 1.04–6.73]; p = 0.04).
Conclusion
In patients with HF and reduced or mildly reduced EF, a compromised ESE-derived peak ESPVR, that reflects impaired LV contractility, resulted to be the most powerful predictor of adverse LV remodeling.
Similar content being viewed by others
Introduction
In patients with left ventricular (LV) dysfunction and reduced ejection fraction (LVEF), transition to heart failure (HF) is often accompanied by progressive LV dilation and changes in ventricular architecture (the so-called LV remodeling) and decline in wall thickness-to-cavity radius, which is referred to as relative wall thickness (RWT), resulting in eccentric LV hypertrophy (LVH) [1]. LV remodeling may occur after myocardial infarction, hemodynamic overload or primary myocardial disease [2,3,4]. Although the etiologies of these disorders are different, they share several pathways that ultimately lead to similar changes in LV size, shape and function [5]. The ensuing development of pathological LVH and LV remodeling may ultimately be associated with a depression of LV performance and the intrinsic contractile state of the myocardium [6].
Stress echocardiography, including dobutamine stress and exercise stress echocardiography (ESE), may endow with additional insights for the evaluation of LV performance and the prediction of changes in LV volumes [7]. Evaluating global myocardial function by stress echocardiography is crucial to distinguish between adaptive or maladaptive LV remodeling in patients with LV systolic dysfunction. The identification of viable tissue relies on the identification of an enhanced contractile response in segments of apparently non-contractile myocardium, usually supplied by stenosed coronary arteries. On the contrary, the assessment of the global pumping capacity during dobutamine challenge or exercise testing is essential to examine the overall ability of the myocardium to comply with the hemodynamic and metabolic needs of the whole body [8, 9]. A number of stress echo studies have been conducted to evaluate the global contractile response of dysfunctional myocardium in patients with HF using different parameters, including changes in LVEF, changes in wall motion score index, changes in end-systolic volume (ESV), cardiac power output-to-mass (CPOM) and the end-systolic pressure-volume relation (ESPVR; i.e. LV elastance) [10,11,12,13,14]. In the present study, we sought to investigate whether the assessment of LV contractile performance during ESE testing may be useful to predict the risk of adverse LV remodeling in patients with HF and reduced or mildly reduced LVEF.
Methods
Patients
This study included a total of 155 outpatients with HF enrolled between 2013 and 2016 at the Cardiac, Thoracic and Vascular Department, University of Pisa, Pisa, Italy. The inclusion criteria comprised LVEF ≤50% and LV end-diastolic volume index (EDVi) > 75 ml/m2. The exclusion criteria were: HF secondary to degenerative valvular heart disease, peripheral artery disease limiting the capability of performing exercise stress test and reduced exercise tolerance attributable to myocardial ischemia or advanced HF (New York Heart Association, NYHA, functional class > III). Of the 168 patients initially selected for the study, 13 were subsequently excluded: six owing to inability to perform the exercise, six due to poor image quality during the exercise test and one due to the occurrence of a second-degree atrioventricular block during exercise. The study patients were clinically stable and under oral treatment. Beta blockers were withheld at least 48 h before the test.
Echocardiography
All patients underwent transthoracic two-dimensional and Doppler echocardiographic examination at baseline, during bicycle semi-supine exercise and after follow-up with commercial equipment using 2nd-harmonic imaging and a 3.5-MHz transducer: Acuson Sequoia C256 (Siemens, Mountain View, California) and iE33 X-matrix(Philips, Einthoven, The Netherlands).
Before exercise and during follow-up, a complete echocardiographic and Doppler examination was performed with the subject in the left lateral supine position. The standard parasternal long-axis view as well as the three standard apical four-chamber, two-chamber and long-axis views were acquired optimising gain setting, sector angle and depth. LV end-diastolic volume (EDV) and ESV were calculated according to the biplane Simpson’s rule. LV ESV index (ESVi) and EDVi were assessed by dividing LV volumes for body surface area. The LV mass index was determined by using the M-mode method according to the Recommendations of the American Society of Echocardiography and the European Association of Cardiovascular Imaging [15]. The LV outflow tract anteroposterior diameter was measured in the parasternal long-axis view and the LV outflow tract area was calculated as πr2 (cm2). The LV stroke distance (cm) was measured tracing the outer edge of the densest (or brightest) portion of the spectral aortic tracing recorded from the apical 5-chamber view, with the PW Doppler sample volume positioned about 5 mm proximal to the aortic valve [16]. Doppler tissue imaging longitudinal velocities were recorded with the sample volume placed at the junction between the septal and lateral LV wall and the mitral annulus in the 4-chamber view and peak early myocardial wave (e’) velocities were measured. The ratio of mitral E peak velocity and averaged e’ velocity (E/e’) was calculated [17]. Patients with a more than mild mitral regurgitation were identified according to the vena contracta method.
Patterns of left ventricular geometry
Allocation of patients into categories of LV geometry was made by reference to the Guidelines for Chamber Quantification: where LVH was assigned for values ≥115 g/m2 for male and ≥ 95 g/m2 for women [15]. A cut-off value for RWT of 0.32 was used to categorize geometric patterns: patients with normal LV mass can have either normal pattern (normal LV mass with RWT ≥ 0.32) or eccentric non-hypertrophied pattern (RWT < 0.32), while patients with increased LV mass can have either non-eccentric (RWT ≥ 0.32) or eccentric (RWT < 0.32) hypertrophy [18].
Definition of adverse LV remodeling
Adverse LV remodeling was defined as the association of eccentric LVH and an increase of LV ESVi [(follow-up LV ESVi – baseline LV ESVi)/baseline LV ESVi] ≥10% [19]. These values were determined via echocardiography during the follow-up period.
Exercise echocardiography
Symptom-limited graded bicycle semi-supine exercise was performed at an initial workload of 20 watts; afterwords, the workload was increased stepwise by 10 watts every two minutes. A 12-lead electrocardiogram and blood pressure (BP) determination were performed at baseline and during the exercise.
At baseline and during each exercise level, Doppler-derived cardiac output at LV outflow tract, heart rate and arterial systolic and diastolic BP (by cuff sphygmomanometer) were measured. Mean BP (MBP) was estimated as follows: diastolic BP + 1/3 (systolic BP – diastolic BP). Stroke volume was calculated as stroke distance times LV outflow tract area and cardiac output (CO) as stroke volume times heart rate.
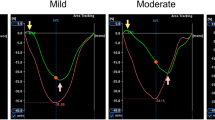
The LV end-systolic pressure (ESP) was obtained as 0.9 x systolic BP (mmHg). The ESVPR or LV elastance (mmHg/ml/m2) was measured as the ratio of the LV ESP to the LV ESV indexed for body surface area [13].
LV cardiac power output (CPO) was calculated as the product of a constant (K1 = 2.22 × 10^-3) with CO (l/min) and MBP (mm Hg). CPOM (W/100 g) was obtained by multiplying CPO by 100 divided by LV mass = K × CO (l/min) × MBP (mmHg) × M− 1 (g); K = 2.22 × 10− 1 [14]. Echocardiographic images were analysed by two independent cardiologists (I.F., N.R.P.), unaware of the identity of the patient. The intra- and inter-observer reproducibility for systolic function parameters at rest and peak exercise in 20 randomly selected patients were good. Concordance between two raters using the Kappa statistic was 0.95 (p < 0.0001).
Statistics
Data are presented as mean ± standard deviation for continuous variables and as percentages for categorical variables. Normality was assessed via the Kolmogorov-Smirnov test.
Continuous variables were compared using paired and independent samples Student t test or Mann-Whitney and Wilcoxon test, as appropriate.
Categorical variables were compared using the Chi-square or Fisher test, as appropriate. Logistic regression was used to explore the determinants of LV diastolic dysfunction. All variables showing a p value < 0.1 at univariate analysis were tested in multivariable models. Stepwise procedure was used to build the multivariate models. The Hosmer-Lemeshow test was used to confirm the goodness-of-fit of multivariable models (p = 0.9). The probability level was p < 0.05 for all the data examined. Data management and analyses were performed using the IBM SPSS Software Package version 17.0.1.
Results
Baseline data of the overall patients’ population (62 ± 11 years; 27, 17% female; 87, 56% previous HF history) and in patients categorised according to the presence of adverse remodeling at follow-up are summarized in Table 1. Exercise-echo data are presented in Table 2. The aetiology was ischemic in 72 (46%). Fourty-seven (30%) patients were in NYHA class I, 65 (42%) in class II and 43 (28%) were in class III.
Adverse LV remodeling was reported in 34 (22%) of the study patients at follow-up. Figure 1 shows the baseline and follow-up variations of LVEF, LV EDVi and LV ESVi. After 6 ± 3 months, LVEF increased from 31% (30–32) to 34% (32–35) (p < 0.0001), LV ESV decreased from 140 ml (133–147) to 132 ml (123–142) (p = 0.01) and LV mass decreased from 146 (140–151) g/m2 to 139 (134–145) g/m2 (p = 0.006). A normal geometric pattern was observed in 8 patients at baseline and in 13 at follow-up, an eccentric non-hypertrophied pattern was reported in 5 at baseline and in 11 at follow-up, a non-eccentric LVH was apparent in 82 at baseline and in 79 at follow-up, while eccentric LVH was present in 60 at baseline and in 52 at follow-up.
Sixty-four of patients exhibited a > 10% reduction in ESVi. Among study patients, 6 underwent percutaneous or surgical correction of functional mitral regurgitation, 3 were submitted to cardiac resynchronization therapy, 2 underwent coronary percutaneous angioplasty and one was revascularized by coronary artery bypass grafting.
Patients with adverse remodeling were prevalently male, presented more advanced NYHA functional class, higher rates of renal dysfunction and moderate to severe mitral regurgitation. Moreover, this group showed higher BNP levels, greater resting and exercise LV volumes, greater LV mass, increased E/e’ratio and more compromised resting and exercise LV EF, peak CPOM and ESPVR.
Univariate and multivariate predictors of adverse LV remodeling are presented in Table 3. By univariate analysis, coronary artery disease, chronic kidney disease, NYHA class, BNP levels, baseline patterns of LV geometry, mitral regurgitation, peak stress LVEF, peak stress LV ESV indexed, peak CPOM and ESPVR were associated to adverse remodeling. In multivariate analysis, peak ESPVR resulted the most powerful independent predictor of adverse LV remodeling (OR: 12.5 [95% CI 4.5–33]; p = < 0.0001), followed by ischemic etiology (OR: 2.64 [95% 1.04–6.73]; p = 0.04).
Discussion
In the present study, conducted in a population of 155 outpatients with HF and reduced or mildly reduced LV EF, we demonstrated that a compromised LV contractility, as reflected by a blunted ESPVR in response to ESE testing, independently predicted adverse LV remodeling as defined by an increased LV mass, RWT < 0.32 and a ≥ 10% increase in LV ESVi.
LV remodeling is usually the result of a progressive process that starts with myocardial damage or excessive LV overload and is very often characterised by the slowly progressive increment of LV volume, increased LV mass and reduced RWT. Since LV overload is initially matched by an adequate growth of cardiac myocytes, the chamber radius is increased, and the wall thickness is increased moderately. To some extent, the initial remodeling may be considered beneficial as the stroke volume may be preserved by augmenting cavity size, but, when the left ventricle further dilates, this adaptive mechanism may progress toward maladaptive remodeling and maladaptive (high-stress) LVH [20,21,22].
The concept that the occurrence of pathological LVH and LV remodeling in patients with LV overload forms a continuum from a compensatory phase to the stage in which exhaustion and myocardial failure prevail is consistent with the work of Meerson [23]. The first stage reflects the initial myocardial damage due to the imposition of the load. The second stage is described as a phase of relatively stable hyperfunction, in which the increased load is compensated by the increase in myocardial mass. The third stage is that of late deterioration and gradual exhaustion. In the latter stage, a progressive decrease of contractile capacity of the entire ventricle is frequently apparent. It would be, therefore, essential to investigate which are the factors that can predict later cavity enlargement and the decline in wall thickness-to-cavity radius or RWT [24].
The importance of changes in LV shape and volume over time has been addressed in some studies. In 1987, White et al. [25] observed that ESVi measured one to two months after thrombolytic therapy for acute myocardial infarction was a powerful predictor of prognosis, providing additional predictive value to LVEF. A continuous relationship between ESVi and both mortality and hospitalisations for worsening HF has been demonstrated in a similar population. LV EDV measured six months after percutaneous coronary intervention for acute myocardial infarction was clearly associated with worse long-term clinical outcome. In particular, an increase of EDV ≥ 20% resulted to be an independent predictor of survival [26].
In an attempt to provide a comprehensive classification, a new categorization capable of including virtually all LV remodeling patterns based on LV volume, mass index and RWT has been proposed [27, 28]. The individual patterns were related to the type of injury or overload, and some of them were closely associated with an adverse outcome, while others appeared to be adaptive or the expression of physiologic response to increased load. Most notably, the term eccentric LVH was applied to patterns with enlarged (dilated) ventricles.
The combination of increased LV mass with the development of eccentric LVH is directly related to deterioration of LV performance. It has been demonstrated that the inability of hypertrophy to keep pace with an abnormally high ventricular wall stress may be responsible for depressed LV function [29]. We hypothesized that ESE-derived parameters of LV performance might be useful in predicting the ensuing cavity enlargement and the decline in wall thickness-to-cavity radius or RWT.
In our study, the results of the ESE testing showed that LV contractility, that is the intrinsic ability of the myocardium to generate force and to shorten independently of changes in loading conditions (afterload and preload), as assessed by the evaluation of echo-derived ESPVR (LV elastance) in response to exercise, can predict subsequent development of adverse LV remodeling. The prognostic value of echo-derived ESVPR at increasing heart rate has been widely demonstrated with either ESE or pharmacological stress echo [30,31,32], but, to our knowledge, this study provides novel information over the relationship between impairment of contractility and the prediction of later adverse LV remodeling.
The transition from a compensated stage of hypertrophy to adverse LV remodeling could be related to the mechanisms by which the inotropic reserve decreases from the initial compensatory phase, albeit the presence of LV dysfunction, to the final stage of exhaustion and progressive deterioration [33]. This form of LVH alters supply-to-demand balance by increasing myocardial oxygen consumption and is often associated with impaired myocardial vascularisation [34], myocyte loss, unfavourable changes in the extracellular matrix composition and fibrosis [35].
The most important study limitation was the reproducibility of LV metrics. As it has been recently pointed out [36], the magnitude of changes of the echocardiographic measures is small enough to fall into the intra- and inter-observer margin of error for these measurements. However, we perform the best of our efforts to guarantee the best reproducibility of the measures by limiting the sources of errors, especially because of the collaborative acquisition and interpretation (I.F., N.R.P., and M.M) of the echocardiographic data both at rest and during exercise, that brought about the intra- and inter-observer variability coefficient for our laboratory within a reasonable range.
Conclusion
A compromised ESE-derived peak ESPVR, that reflects impaired LV contractility, resulted to be the most powerful predictor of adverse LV remodeling, defined on the basis of LV volumes and RWT, in patients with HF with reduced or mildly reduced LVEF.
Abbreviations
- BNP:
-
Brain Natriuretic Peptide
- BP:
-
Blood Pressure
- CO:
-
Cardiac Output
- CPO:
-
Cardiac Power Output
- CPOM:
-
Cardiac Power output-to-mass
- EDV:
-
End-Diastolic Volume
- EDVi:
-
End-Diastolic Volume index
- EF:
-
Ejection Fraction
- ESE:
-
Exercise Stress Echocardiography
- ESP:
-
End-Systolic Pressure
- ESPVR:
-
End-Systolic Pressure Volume Relation
- ESV:
-
End-Systolic Volume
- ESVi:
-
End-Systolic Volume index
- HF:
-
Heart Failure
- LV:
-
Left Ventricular
- LVEF:
-
Left Ventricular Ejection Fraction
- LVH:
-
Left Ventricular Hypertrophy
- MBP:
-
Mean Blood Pressure
- NYHA:
-
New York Heart Association
- RWT:
-
Relative Wall Thickness
References
Gaasch WH, Delorey DE, St. John Sutton MG, Zile MR. Patterns of Structural and Functional Remodeling of the Left Ventricle in Chronic Heart Failure. Am J Cardiol [Internet]. 2008;102(4):459–62. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18678306. [cited 2019 Mar 29].
Pfeffer MA, Braunwald E. Ventricular remodeling after myocardial infarction. Experimental observations and clinical implications. Circulation [Internet]. 1990;81(4):1161–72. Available from: http://www.ncbi.nlm.nih.gov/pubmed/2138525. [cited 2019 Mar 29].
Cohn JN, Ferrari R, Sharpe N. Cardiac remodeling--concepts and clinical implications: a consensus paper from an international forum on cardiac remodeling. Behalf of an International Forum on Cardiac Remodeling. J Am Coll Cardiol [Internet]. 2000 Mar 1 ;35(3):569–82. Available from: http://www.ncbi.nlm.nih.gov/pubmed/10716457. [cited 2019 Mar 29].
Opie LH, Commerford PJ, Gersh BJ, Pfeffer MA. Controversies in ventricular remodelling. Lancet [Internet]. 2006;367(9507):356–67. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16443044. [cited 2019 Mar 29].
Beltrami CA, Finato N, Rocco M, Feruglio GA, Puricelli C, Cigola E, et al. Structural basis of end-stage failure in ischemic cardiomyopathy in humans. Circulation [Internet]. 1994;89(1):151–63. Available from: http://www.ncbi.nlm.nih.gov/pubmed/8281642. [cited 2019 Mar 29].
Katz AM. The “Modern” View of Heart Failure. Circ Hear Fail [Internet]. 2008;1(1):63–71. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19808272. [cited 2019 Mar 29].
Lancellotti P, Pellikka PA, Budts W, Chaudhry FA, Donal E, Dulgheru R, et al. The clinical use of stress echocardiography in non-ischaemic heart disease: recommendations from the European Association of Cardiovascular Imaging and the American Society of Echocardiography. Eur Hear J – Cardiovasc Imaging [Internet]. 2016 Nov 21;17(11):1191–229. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27880640. [cited 2019 Mar 29].
PICANO E, Sicari R. Risk stratification by stress echocardiography: a whiter shade of pale? Eur J Echocardiogr [Internet]. Narnia. 2004;5(3):162–4. Available from: https://academic.oup.com/ehjcimaging/article-lookup/doi/10.1016/j.euje.2004.04.001. [cited 2019 Mar 29].
Picano E, Pellikka PA. Stress echo applications beyond coronary artery disease. Eur Heart J [Internet]. 2014;35(16):1033–40. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24126880. [cited 2019 Mar 29]
Pinamonti B, Perkan A, Di Lenarda A, Gregori D, Sinagra G. Dobutamine echocardiography in idiopathic dilated cardiomyopathy: clinical and prognostic implications. Eur J Heart Fail [Internet]. 2002;4(1):49–61. Available from: http://www.ncbi.nlm.nih.gov/pubmed/11812665. [cited 2019 Mar 29].
Parsai C, Baltabaeva A, Anderson L, Chaparro M, Bijnens B, Sutherland GR. Low-dose dobutamine stress echo to quantify the degree of remodelling after cardiac resynchronization therapy. Eur Heart J [Internet]. 2008;30(8):950–8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19269987. [cited 2019 Mar 29]
Scrutinio D, Napoli V, Passantino A, Ricci A, Lagioia R, Rizzon P. Low-dose dobutamine responsiveness in idiopathic dilated cardiomyopathy: relation to exercise capacity and clinical outcome. Eur Heart J [Internet]. 2000;21(11):927–34. Available from: http://www.ncbi.nlm.nih.gov/pubmed/10806017. [cited 2019 Mar 29].
Bombardini T, Correia MJ, Cicerone C, Agricola E, Ripoli A, Picano E. Force-frequency relationship in the echocardiography laboratory: a noninvasive assessment of Bowditch treppe? J Am Soc Echocardiogr [Internet]. 2003;16(6):646–55. Available from: http://www.ncbi.nlm.nih.gov/pubmed/12778025. [cited 2019 Mar 29].
Dini FL, Mele D, Conti U, Ballo P, Citro R, Menichetti F, et al. Peak Power Output to Left Ventricular Mass: An Index to Predict Ventricular Pumping Performance and Morbidity in Advanced Heart Failure. J Am Soc Echocardiogr [Internet]. 2010;23(12):1259–65. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20889309. [cited 2019 Mar 29].
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, et al. Recommendations for Cardiac Chamber Quantification by Echocardiography in Adults: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr [Internet]. 2015;28(1):1–39.e14. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25559473. [cited 2019 Mar 29].
Quiñones MA, Greenberg BH, Kopelen HA, Koilpillai C, Limacher MC, Shindler DM, et al. Echocardiographic predictors of clinical outcome in patients with left ventricular dysfunction enrolled in the SOLVD registry and trials: significance of left ventricular hypertrophy. Studies of Left Ventricular Dysfunction. J Am Coll Cardiol [Internet]. 2000;35(5):1237–44. Available from: http://www.ncbi.nlm.nih.gov/pubmed/10758966. [cited 2019 Mar 29].
Nagueh SF, Smiseth OA, Appleton CP, Byrd BF, Dokainish H, Edvardsen T, et al. Recommendations for the Evaluation of Left Ventricular Diastolic Function by Echocardiography: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr [Internet]. 2016;29(4):277–314. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27037982. [cited 2019 Mar 29].
Gaasch WH, Zile MR. Left Ventricular Structural Remodeling in Health and Disease. J Am Coll Cardiol [Internet]. 2011;58(17):1733–40. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0735109711028397. [cited 2019 Mar 29].
Farah E, Cogni AL, Minicucci MF, Azevedo PS, Okoshi K, Matsubara BB, et al. Prevalence and predictors of ventricular remodeling after anterior myocardial infarction in the era of modern medical therapy. Med Sci Monit [Internet]. 2012;18(5):CR276-81. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22534706. [cited 2019 Mar 29]
Ross J. Adaptations of the left ventricle to chronic volume overload. Circ Res [Internet]. 1974;35(2):suppl II:64-70. Available from: http://www.ncbi.nlm.nih.gov/pubmed/4276490. [cited 2019 Mar 29].
Konstam MA. “Systolic and diastolic dysfunction” in heart failure? Time for a new paradigm. J Card Fail [Internet]. 2003;9(1):1–3. Available from: http://www.ncbi.nlm.nih.gov/pubmed/12612866. [cited 2019 Mar 29].
Konstam MA, Kramer DG, Patel AR, Maron MS, Udelson JE. Left Ventricular Remodeling in Heart Failure. JACC Cardiovasc Imaging [Internet]. 2011;4(1):98–108. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21232712. [cited 2019 Mar 29].
Meerson FZ. Compensatory Hyperfunction of the Heart and Cardiac Insufficiency. Circ Res [Internet]. Lippincott Williams & Wilkins; 1962;10(3):250–8. Available from: https://www.ahajournals.org/doi/10.1161/01.RES.10.3.250. [cited 2019 Mar 29].
Dini FL, Galeotti GG, Terlizzese G, Fabiani I, Pugliese NR, Rovai I. Left Ventricular Mass and Thickness: Why Does It Matter? Heart Fail Clin [Internet]. Elsevier; 2019;15(2):159–66. Available from: https://www.sciencedirect.com/science/article/pii/S1551713618301259. [cited 2019 Mar 29].
White HD, Norris RM, Brown MA, Brandt PW, Whitlock RM, Wild CJ. Left ventricular end-systolic volume as the major determinant of survival after recovery from myocardial infarction. Circulation [Internet]. 1987;76(1):44–51. Available from: https://www.ahajournals.org/doi/10.1161/01.CIR.76.1.44. [cited 2019 Mar 29].
Bolognese L, Neskovic AN, Parodi G, Cerisano G, Buonamici P, Santoro GM, et al. Left ventricular remodeling after primary coronary angioplasty: patterns of left ventricular dilation and long-term prognostic implications. Circulation [Internet]. 2002 Oct 29;106(18):2351–7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/12403666. [cited 2019 Mar 29].
Pugliese NR, Fabiani I, La Carrubba S, Conte L, Antonini-Canterin F, Colonna P, et al. Classification and Prognostic Evaluation of Left Ventricular Remodeling in Patients With Asymptomatic Heart Failure. Am J Cardiol [Internet]. 2017;119(1):71–7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27776801. [cited 2019 Mar 29].
Fabiani I, Pugliese NR, La Carrubba S, Conte L, Antonini-Canterin F, Colonna P, et al. Incremental prognostic value of a complex left ventricular remodeling classification in asymptomatic for heart failure hypertensive patients. J Am Soc Hypertens [Internet]. 2017;11(7):412–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28619598. [cited 2019 Mar 29].
Dini FL, Capozza P, Donati F, Simioniuc A, Corciu AI, Fontanive P, et al. Patterns of left ventricular remodeling in chronic heart failure: Prevalence and prognostic implications. Am Heart J [Internet]. 2011;161(6):1088–95. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21641355. [cited 2019 Mar 29].
Bombardini T, Agrusta M, Natsvlishvili N, Solimene F, Pap R, Coltorti F, et al. Noninvasive assessment of left ventricular contractility by pacemaker stress echocardiography. Eur J Heart Fail [Internet]. 2005;7(2):173–81. Available from: http://www.ncbi.nlm.nih.gov/pubmed/15701463. [cited 2019 Mar 29].
Bombardini T. Myocardial contractility in the echo lab: molecular, cellular and pathophysiological basis. Cardiovasc Ultrasound [Internet]. 2005;3(1):27. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16150150. [cited 2019 Mar 29].
Grosu A, Bombardini T, Senni M, Duino V, Gori M, Picano E. End-systolic pressure/volume relationship during dobutamine stress echo: a prognostically useful non-invasive index of left ventricular contractility. Eur Heart J [Internet]. 2005;26(22):2404–12. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16105848. [cited 2019 Mar 29].
Sabbah HN, Stein PD, Kono T, Gheorghiade M, Levine TB, Jafri S, et al. A canine model of chronic heart failure produced by multiple sequential coronary microembolizations. Am J Physiol Circ Physiol [Internet]. 1991;260(4):H1379–84. Available from: http://www.ncbi.nlm.nih.gov/pubmed/1826414. [cited 2019 Mar 29].
Dini FL, Ghiadoni L, Conti U, Stea F, Buralli S, Taddei S, et al. Coronary Flow Reserve in Idiopathic Dilated Cardiomyopathy: Relation with Left Ventricular Wall Stress, Natriuretic Peptides, and Endothelial Dysfunction. J Am Soc Echocardiogr [Internet]. 2009;22(4):354–60. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19269783. [cited 2019 Mar 29].
Lavine SJ, Prcevski P, Held AC, Johnson V. Experimental model of chronic global left ventricular dysfunction secondary to left coronary microembolization. J Am Coll Cardiol [Internet]. 1991;18(7):1794–803. Available from: http://www.ncbi.nlm.nih.gov/pubmed/1960332. [cited 2019 Mar 29].
Pellikka PA, She L, Holly TA, Lin G, Varadarajan P, Pai RG, et al. Variability in Ejection Fraction Measured By Echocardiography, Gated Single-Photon Emission Computed Tomography, and Cardiac Magnetic Resonance in Patients With Coronary Artery Disease and Left Ventricular Dysfunction. JAMA Netw Open [Internet]. 2018;1(4):e181456. Available from: http://www.ncbi.nlm.nih.gov/pubmed/30646130. [cited 2019 Mar 29].
Acknowledgements
Not applicable.
Funding
This study was not funded.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
IF, NRP, FLD: Manuscript ideation, Ethical issues, data collection, data analysis. IR, CS: data collection, database completion, critical revision. MM, AdA, RP: critical revision. MMic: data validation; statistical revision. All authors read and approved the final manuscript.
Authors’ informations
Not applicable.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The present study was performed in conformity with the ethical guidelines of the Declaration of Helsinki. The study was approved by the local ethics committee. Written informed consent was obtained from all patients before study inclusion.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Fabiani, I., Pugliese, N.R., Santini, C. et al. The assessment of pressure-volume relationship during exercise stress echocardiography predicts left ventricular remodeling and eccentric hypertrophy in patients with chronic heart failure. Cardiovasc Ultrasound 17, 6 (2019). https://doi.org/10.1186/s12947-019-0157-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12947-019-0157-z