Abstract
Aim
To systematically review currently available cardiac shock-wave therapy (CSWT) studies in humans and perform meta-analysis regarding anti-anginal efficacy of CSWT.
Methods
The Cochrane Controlled Trials Register, Medline, Medscape, Research Gate, Science Direct, and Web of Science databases were explored. In total 39 studies evaluating the efficacy of CSWT in patients with stable angina were identified including single arm, non- and randomized trials. Information on study design, subject’s characteristics, clinical data and endpoints were obtained. Assessment of publication risk of bias was performed and heterogeneity across the studies was calculated by using random effects model.
Results
Totally, 1189 patients were included in 39 reviewed studies, with 1006 patients treated with CSWT. The largest patient sample of single arm study consisted of 111 patients. All selected studies demonstrated significant improvement in subjective measures of angina symptoms and/or quality of life, in the majority of studies left ventricular function and myocardial perfusion improved. In 12 controlled studies with 483 patients included (183 controls) angina class, Seattle Angina Questionnaire (SAQ) score, nitrates consumption were significantly improved after the treatment.
In 593 participants across 22 studies the exercise capacity was significantly improved after CSWT, as compared with the baseline values (in meta-analysis standardized mean difference SMD = −0.74; 95% CI, −0.97 to −0.5; p < 0.001).
Conclusions
Systematic review of CSWT studies in stable coronary artery disease (CAD) demonstrated consistent improvement of clinical variables. Meta-analysis showed a moderate improvement of exercise capacity.
Overall, CSWT is a promising non-invasive option for patients with end-stage CAD, but evidence is limited to small sample single-center studies. Multi-center adequately powered randomised double blind studies are warranted.
Similar content being viewed by others
Background
A substantial number of patients suffer from disabling angina despite having undergone invasive treatment methods and continuation on optimal medical treatment (OMT) [1]. Such condition is defined as a refractory angina (RFA) [2]. In many cases, stable coronary artery disease (CAD) becomes too diffuse and extensive to be treated by traditional revascularization methods. The annual mortality rate of RFA in recent studies is in the range of 3–4% [3, 4].
Several new alternative treatment methods of RFA are being investigated. A number of studies showed that transmyocardial [5] and percutaneous myocardial laser revascularization [6, 7], spinal cord stimulation [8] and stem cell therapy [9–11] may reduce angina symptoms and improve exercise capacity, myocardial perfusion and function. Nevertheless, these treatment modalities are invasive, quite expensive or still at a preclinical stage.
Enhanced external counter-pulsation is a non-invasive option suggested for CAD patients. However, the recent studies were inconclusive and found no or small differences between test and control groups with respect to change in angina or exercise duration [12, 13].
Ultrasound-guided cardiac shock wave (SW) therapy is another promising non-invasive modality in patients with stable CAD. Experimental studies showed that SW might induce shear stress to endothelial cells and produce complex cascade of short- and long-term reactions leading to angiogenesis [14, 15]. The observed immediate increase in blood flow due to local vasodilation and the formation of new capillaries in the treated tissue [16–18] has led to its application in cardiovascular medicine. Since 1999 [19], cardiac shock-wave therapy (CSWT) as a tool for the management of RFA has been investigated in a considerable number of clinical studies.
Our aim was to systematically review and analyse currently available data from CSWT studies in humans and perform meta-analysis regarding efficacy of CSWT on exercise capacity.
Materials and methods
Inclusion criteria, search strategy, methods of data collection and analysis were elaborated in a protocol.
Data sources
We searched for articles evaluating the efficacy of CSWT in CAD patients from the following medical bibliographic databases: Cochrane Controlled Trials Register, Medline, Medscape, Research Gate, Science Direct, Web of Science (from 1999 to April of 2016), and Google Web. Publications were selected by pre-defined criteria and reviewed by two authors (GB, ES) following PRISMA statement [20]. Disagreements were discussed with other author (JC). The search terms included coronary artery disease, ischemic heart disease, refractory angina treatment, stable angina treatment combined with extracorporeal cardiac shock wave therapy, myocardial shock wave therapy, extracorporeal myocardial revascularisation. We also searched for references in review articles and abstracts.
Study selection criteria
In order to be included, trials had to assess the treatment with CSWT of CAD patients, written in English. Selected studies included patients with stable CAD proven by coronary angiography or computed tomography angiography, not amenable to revascularization, angina class II-IV (Canadian Cardiology Society, CCS), despite OMT, and documented stress induced myocardial ischemia. Trials investigating combination of CSWT with stem cell therapy were not included.
Data extraction
Information on 1) study design (including study type, method of randomization and blinding of patients, study personnel and outcome assessors), 2) sample size and patients characteristics (including age, sex), 3) intervention strategies (including treatments schedule, follow up duration), 4) outcome measures (including (short-acting nitrates consumption per week, CCS angina class and New York Heart Association [NYHA] functional class, Seattle Angina Questionnaire (SAQ) scores, and parameters of the functional tests as exercise duration, workload, global and regional left ventricular [LV] function, myocardial perfusion) were extracted into Microsoft Excel (Microsoft, Seattle, Wash., USA) spread sheets.
Statistical analysis
Variables were presented as mean value ± standard deviation (SD) for continuous data with normal distribution and as median with interquartile range (IQR: Q1, Q3) for data not normally distributed, whereas categorical variables were expressed as number (%).
Assessment of risk of bias randomized trials was performed in accordance with the Cochrane Collaboration tool [21] and was based on information on concealment of allocation and random sequence generation, blinding of participants and personnel, incomplete outcome data and selective reporting. For risk of bias assessments the low/unclear/high scale was used.
The effect sizes used in each study are presented as standardized mean difference (SMD) with 95% confidence interval (CI) to allow for combination of different measurements of exercise capacity. In line with Cohen's classification [22], effect sizes were divided into trivial (Cohen's d ≤0.2), small (<0.5), moderate (<0.8), and large (>0.8).
Heterogeneity was assessed by using the chi-square test for heterogeneity and the I2 statistic to determine the proportion of variation attributable to heterogeneity among studies. Values of I2 considered as low (<25%), moderate (25–50%) and high (>50%) heterogeneity. Meta-analysis results are presented as forest plots. Random effects model according to Der Simonian-Laird was used to verify the significant evidence of heterogeneity between the results of studies. Publication bias was estimated by drawing funnel plot. The analysis was performed using RevMan 5.3 software (Copenhagen, The Nordic Cochrane Centre) [23].
Results
Study characteristics and patient population
From 590 identified publications after exclusion of irrelevant, experimental, animal and non-English studies 39 studies were selected for review following the PRISMA statement [20] (Fig. 1, Table 1); their common characteristics are summarized in Table 2.
In total, 1189 patients were included with 1006 patients treated with CSWT (483 patients underwent CSWT in controlled studies), 183 patients entered control groups. The mean age of patients was 66 ± 6.7 years, 80.8% were men. Study sample size was from 8 to 111 patients; duration of follow up lasted from 1 to 72 months.
No procedure related adverse events and good treatment tolerance were reported.
Studies did not include patients with acute coronary syndromes at least 3 months before enrolment, recent revascularization and thrombus in the left ventricle.
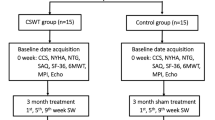
In most studies the treatment protocol consisted of nine sessions conducted over a 9-week period with three treatment series performed on the 1st, 5th and 9th week. Shock waves were applied to targeted area of myocardial ischemia detected by imaging stress tests. Wang showed that a modified regimen of nine treatment sessions within 1 month had similar therapeutic effect, as compared to the standard treatment protocol [24]; only a standard treatment group from this study was included in meta-analysis in order to reduce possible heterogeneity.
Risk of bias and quality assessment of controlled studies is shown in Table 3.
Cardiac shock wave therapy effect on clinical variables
All selected studies demonstrated positive effect of CSWT on clinical variables (results of controlled studies are shown in Table 4). In CSWT patients CCS angina scale (31 studies) and NYHA class (13 studies) have reduced by 1 (1, 1) and 1 (0, 1), respectively, compared with the baseline values. The frequency of weekly nitroglycerine use declined from 40 to 75% (in 16 related studies).
Meta-analysis of cardiac shock wave therapy effect on exercise capacity
Two studies investigating ischemic heart failure population were excluded from meta-analysis [25, 26].
From remaining 37 studies only 22 studies provided data suitable to be included in meta-analysis to evaluate the impact of CSWT on the parameters of exercise tolerance (mean and standard deviation or standard error of mean values, both baseline and post procedure), (Fig. 2, Table 5).
Across 22 contributing studies (596 participants) the exercise capacity was significantly improved after CSWT, as compared with the baseline values (SMD = −0.74; 95% CI, −0.97 to −0.5; p < 0.001, I2 = 70%, Fig. 2); mean follow up period made 8 months (range 1–72 months).
In order to explain heterogeneity, we performed sensitivity analysis by removing from analysis one of the studies at a time. Overall effect changed to −0.61, 95% CI (−0.78 to −0.44), p < 0.001 when excluding study of Zhao L. et al. (2015) and to −0.77, 95% CI (−1.01 to −0.52), p < 0.001 when excluding study of Prinz C. et al (2013).
Funnel plot analysis was performed in order to evaluate publication bias (Fig. 3). The funnel plot graph was asymmetrical and three outliers were identified representing studies of Caspari, Gutersohn and Zhao group. Without these studies heterogeneity decreased to I2 = 0%, p = 0.57 with SMD = −0.54; 95% CI, −0.66 to −0.42; p < 0.001.
Funnel plot of the meta-analysis. The standardized mean difference (SMD) on the x-axis is plotted against the standard error (SE) of the log(SMD) on the y-axis. A symmetrical distribution of studies indicates the absence of publication bias. An asymmetrical distribution with, for example, relatively more smaller studies with a positive result (in the lower right part of the plot) would suggest the presence of publication bias
Interestingly, in uncontrolled studies treatment effect was smaller than in controlled studies (SMD -0.59 (−0.81, −0.36) vs −0.93 (−1.44, −0.42)).
Cardiac shock wave therapy effect on left ventricular function
Figures 4 and 5 demonstrate changes of rest left ventricular (LV) function by echocardiography and magnetic resonance imaging (MRI), respectively. Changes of LV end diastolic diameter are shown in Fig. 6. Seven studies demonstrated significant LV function improvement due to CSWT, while in eight studies no statistically significant changes were found.
Cardiac shock wave therapy effect on myocardial perfusion
During SPECT significant improvement of myocardial perfusion was demonstrated in 27 of 32 studies, during PET in two of four studies. Beneficial changes of myocardial perfusion were associated with increase of LVEF in seven of 13 studies with modest effect of 3.58% (2.0, 4.57). Cassar et al. [27] compared segments that were treated with CSW and those that were not, and found that after 4 months of follow–up the progression of ischemic burden of untreated segments was significantly greater.
Cardiac shock wave therapy effect on angiogenesis markers
Angiogenesis markers were assessed in four studies. Increased VEGF concentration was revealed after CSWT [28–30]. Kikuchi et al. found that the number of circulating progenitor cells (CD 34+/KDR+ and CD 34+/KDR+/c-kit+) in peripheral blood remained unchanged [31]. Cai et al. observed significant increase in the number of circulating progenitor cells (CD45low/CD34+/VEGFR2) in peripheral blood [30].
Generation of shock waves and cardiac shock wave treatment
Shock waves (SW) belong to acoustic waves that can be transmitted through a liquid medium and focused with a precision of several millimetres to any intended treatment area inside the body.
In CAD patients, SW can be delivered to the border of the ischemic area to potentially induce neovascularization from the healthy area to the ischemic zone. Shock waves can be generated by discharge of a high-voltage spark under water or electromagnetic impulse. CSWT is performed using a SW generator system coupled with a cardiac ultrasound imaging system that is traditionally used to target the treatment to area with previously documented ischemia (Fig. 7). SW are delivered via a special applicator through the anatomical acoustic window to the treatment area under electrocardiographic R-wave gating. For optimal therapy, the treatment area is divided into target zones corresponding to the size of the focal zone of the SW applicator (Fig. 7).
The methodology of cardiac shock wave therapy. a Shock wave generator system (Medispec, Germantown, MD, USA) and cardiac imaging system (Vivid i, GE Healthcare, Horten, Norway). b Shock wave focal zone alignment: Position of the sub-segment on the 2-dimensional image determined by X and Y coordinates (1). The shockwave applicator position is identically adjusted along X- and Y-axes corresponding to the X and Y coordinates of the ultrasound image (2)
Discussion
Clinical research in intriguing CSWT field continues since 1999, and several new trials are being published every year. The aim of this study was to summarize the results and also to evaluate the quality of currently accumulated evidence on the efficacy of CSWT on CAD treatment. This systematic review expands previously published analysis [32] by including 23 recent studies, and confirms the beneficial effects of CSWT in a larger pooled sample size of patients with stable CAD. The strength of this paper is a systematic character of review, an inclusion in meta-analysis studies with single clinical indication and a uniform treatment protocol, and assessment of bias risk in randomised trials.
In contrast to our study, recently published meta-analysis of Wang and co-authors covered only a limited period of publications, from 2010 to 2014, and included not only English but also Chinese articles [33]. As a result, our work presents the largest contemporary review of human CSWT trials incorporating all the research period.
Like in the previous analyses the majority of detected trials are relatively small, single centre, single arm, some of them insufficiently report methodology and results. In order to avoid substantial heterogeneity and publication bias reported by Wang, we excluded from meta-analysis studies, which targeted at different population of ischemic heart failure, and also non-English articles as potentially producing more beneficial results. Our study focused on the stable CAD patients and confirmed consistent positive anti-anginal effect of CSWT.
In medical field high-energy extracorporeal shock wave therapy (ESWT) was introduced more than 30 years ago as a treatment option for urinary tract stones [34]. ESWT has changed the treatment of urinary calculi, and even today it remains the primary treatment in most non-complicated cases [35]. ESWT has also been applied in biliary tract [36], pancreatic [37] and salivary stones treatment [38]. Low energy ESWT has regenerative features and has been developed as a treatment standard for a variety of orthopedic and soft tissue diseases [39], including wound healing in diabetic patients [40]. Furthermore, shockwaves have been used for treatment chronic pelvic pain syndrome [41] and erectile dysfunction. The observed immediate increase in blood flow due to local vasodilatation and the formation of new capillaries in the treated tissue [16, 17] has led to one of its more promising application in cardiovascular medicine as a possible treatment for patients with stable angina.
The mechanism of CSWT action is multifactorial. SW induces tissue cavitation, leading to a variety of biochemical effects, including shear stress on cell membranes [42], an increase in nitric oxide synthesis [43–46], an up-regulation of vascular endothelial growth factor (VEGF), [14], acceleration of bone marrow cell differentiation into endothelial cells [47], an increase of the amount of circulating endothelial progenitor cells [15]. Thus, CSWT may enhance angiogenesis, reduce inflammatory response, oxidative stress, cellular apoptosis and fibrosis [14, 47, 48]. It is presumed that these mechanisms demonstrated in experimental settings could be translated into clinical effects of improvement of symptoms and myocardial perfusion in CAD patients.
Our review and meta-analysis show that in the majority of published CSWT studies, nitroglycerine consumption and angina frequency decreases, CCS, SAQ scores and NYHA class improves, myocardial perfusion and exercise capacity increases significantly. Most benefits could be observed as early as in the first month, suggesting the contribution of an early local vasodilating effect of SW. Those beneficial effects persisted during the 1-year of follow up, probably related to angiogenesis and other tissue reactions [49, 50].
Total exercise capacity is one of the most important variables used to assess efficacy of any anti-anginal treatment. We evaluated data from randomized clinical studies along with several non-controlled studies of good quality, though certain extent of heterogeneity is not avoided. Our meta-analysis of 596 participants suggests at least a moderate improving effect of CSWT on exercise tolerance.
However, most of the studies included in the review and meta-analysis are single-centre and uncontrolled, making the likelihood of bias towards larger intervention effect substantial. Different methodological quality, inadequate design or unbalanced analysis compels cautious interpretation of the real CSWT effect. Moreover, Wang assessment of methodology confirms our findings that quality of published controlled trials methodology was low [33]. The majority of the randomised studies were evaluated as having high risk if bias in terms of attribution, sample size calculation, blinding of participants and outcome assessment.
Despite very well tolerance, virtually absence of side effects, considerable symptomatic effect and non-invasive nature of CSWT it has not been widely put into practice. This may be associated with the need of special average cost equipment, particular skills of ultrasound scanning and CSWT application, and with the significant time consumption for the whole therapy course as well. Therefore, CSWT can be considered not as a substitutive but as adjunct therapy in case of limited efficacy of optimal medical treatment.
It seems that the tentative phase of this novel treatment lasted enough, and still there is a lack of high quality evidence. This warrants to perform adequately powered double blind, randomized, placebo controlled study in patients with CAD. Currently appropriately designed multicentre study is ongoing with the aim to confirm the additional improvement of exercise tolerance due to CSWT (NCT02339454).
Conclusions
Systematic review of CSWT studies in stable CAD demonstrated a clinically significant improvement of clinical variables including angina class and quality of life, as well as positive changes in LV function and perfusion. Meta-analysis showed moderate improvement in exercise capacity. Overall, CSWT is a potentially effective new non-invasive option for patients with CAD, but evidence is limited to small low/moderate quality single-centre studies. Multicentre adequately powered randomised double blind studies are warranted.
Abbreviations
- CAD:
-
Coronary artery disease
- CCS:
-
Canadian Cardiology Society
- CI:
-
Confidence interval
- CSWT:
-
Cardiac shock wave therapy
- LV:
-
Left ventricular
- LVEF:
-
Left ventricular ejection fraction
- MRI:
-
Magnetic resonance imaging
- NYHA:
-
New York Heart Association
- OMT:
-
Optimal medical treatment
- PET:
-
Positron emission tomography
- RFA:
-
Refractory angina
- SAQ:
-
Seattle Angina Questionnaire
- SMD:
-
Standardized mean difference
- SPECT:
-
Single photon emission computed tomography
- SW:
-
Shock waves
- VEGF:
-
Vascular endothelial growth factor
References
Williams B, Menon M, Satran D, Hayward D, Hodges JS, Burke MN, et al. Patients with coronary artery disease not amenable to traditional revascularization: prevalence and 3-year mortality. Catheter Cardiovasc Interv. 2010;75:886–91.
McGillion M, Arthur H, Cook A, Carroll SL, Victor JC, L’allier PL, et al. Management of patients with refractory angina: Canadian Cardiovascular Society/Canadian Pain Society Joint Guidelines. Can J Cardiol. 2012;28:S20–41.
Henry TD. A new option for the “no-option” patient with refractory angina? Catheter Cardiovasc Interv. 2009;74:395–7.
Henry TD, Satran D, Hodges JS, Johnson RK, Poulose AK, Campbell AR, et al. Long-term survival in patients with refractory angina. Eur Heart J. 2013;34:2683–8.
Briones E, Lacalle JR, Marin I. Transmyocardial laser revascularization versus medical therapy for refractory angina. Cohrane Database Syst Rev. 2009;1, CD003712.
Oesterele SN, Sanborn TA, Ali N, Resar J, Ramee SR, Heuser R, et al. Percutaneus transmyocardial laser revascularization for severe angina: the PACIFIC randomized trial. Potential class improvement from intramyocardial channels. Lancet. 2000;356:1705–10.
Salem M, Rotevatn S, Nordrehaug JE. Long-term results following percutaneous myocardial laser therapy. Coron Artery Dis. 2006;17:385–90.
Taylor RS, De Vries J, Bucher E, Dejongste MJ. Spinal cord stimulation in the treatment of refrctory angina: systematic review and metaanalysis of randomised controlled trials. BMC Cardiovasc Disord. 2009;9:13.
Van Ramshorst J, Bax JJ, Sl B, Dibbets-Schneider P, Roes SD, Stokkel MP, et al. Intramyocardial bone marrow cell injection for chronic myocardial ischemia: a randomised controlled trial. JAMA. 2009;301:1997–2004.
Assmus B, Schachinger V, Teupe C, Britten M, Lehmann R, Döbert N, et al. Transplantation of Progenitor Cells and Regeneration Enhancement in Acute Myocardial Infarction (TOPCARE-AMI). Circulation. 2002;106:3009–17.
Wollert KC, Meyer GP, Lotz J, Ringes-Lichtenberg S, Lippolt P, Breidenbach C, et al. Intracoronary autologous bone-marrow cell transfer after myocardial infarction: the BOOST randomised controlled clinical trial. Lancet. 2004;364:141–8.
Loh PH, Cleland JG, Louis AA, Kennard ED, Cook JF, Caplin JL, et al. Enhanced external counterpulsation in the treatment of chronic refractory angina: A long-term follow-up outcome from the international enhanced external counterpulsation patient registry. ClinCardiol. 2008;31:159–64.
Kumar A, Aronow WS, Vadnerkar A, Sindhu P, Mittal S, Kasliwal RR, et al. Effect of enhanced external counterpulsation on clinical symptoms, quality of life, 6-min walking distance, and echocardiographic measurements of left ventricular systolic and diastolic function after 35 days of treatment and at 1-year follow up in 47 patients with chronic refractory angina pectoris. Am J Ther. 2009;16:116–8.
Nishida T, Shimokawa H, Oi K, Tatewaki H, Uwatoku T, Abe K, et al. Extracorporeal cardiac shock wave therapy markedly ameliorates ischemia-induced myocardial dysfunction in pigs in vivo. Circulation. 2004;110:3055–61.
Fu M, Sun CK, Lin YC, Wang CJ, Wu CJ, Ko SF, et al. Extracorporeal shock wave therapy reverses ischemia-related left ventricular dysfunction and remodeling: molecular-cellular and functional assessment. PLoS One. 2011;6, e24342.
Young SR, Dyson M. The effect of therapeutic ultrasound on angiogenesis. Ultrasound Med Biol. 1990;16:261–9.
Wang CJ, Huang HY, Pai CH. Shock wave-enhanced neovascularization at the tendon-bone junction: an experiment in dogs. J Foot Ankle Surg. 2002;41:16–22.
Song J, Qi M, Kaul S, Price RJ. Stimulation of arteriogenesis in skeletal muscle by microbuble destruction with ultrasound. Circulation. 2002;106:1550–5.
Caspari GH, Erbel R. Revascularization with extracorporeal shock wave therapy: first clinical results. Circulation. 1999;100 Suppl 18:84–9.
Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. Preferred reporting items for systematic reviews and meta- analyses: the PRISMA statement. PLoS Med. 2009;6(7), e1000097. doi:10.1371/journal.pmed.1000097.
Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman A, on behalf of Cochrane Bias Methods Group; Cochrane Statistical Methods Group, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomized trials. BMJ. 2011;343:d5928.
Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. New Jersey: Lawrence Erlbaum; 1988. p. 567.
2014 Review Manager (RevMan) [Computer program]. Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration. http://community.cochrane.org/tools/review-production-tools/revman-5/about.
Wang Y, Guo T, Ma T, Cai H, Tao S, Peng Y, et al. A modified regimen of extracorporeal cardiac shock wave therapy for treatment of coronary artery disease. Cardiovasc Ultrasound. 2012;10:35.
Vasyuk Y, Hadzegova A, Shkolnik E, Kopeleva M, Krikunova O, Iouchtchouk E, et al. Initial clinical experience with extracorporeal shock wave therapy in treatment of ischemic heart failure. Congest Heart Fail. 2010;16:226–30.
Peng YZ, Guo T, Yang P, Yang HW, Zhou P, Wang Y, et al. Effects of extracorporeal cardiac shock wave therapy in patients with ischemic heart failure. Zhonghua Xin Xue Guan Bing Za Zhi. 2012;40:141–6.
Cassar A, Prasad M, Rodriguez-Porcel M, Reeder GS, Karia D, DeMaria AN, et al. Safety and efficacy of extracorporeal shock wave myocardial revascularization therapy for refractory angina pectoris. Mayo Clin Proc. 2014;89:346–54.
Takayama T, Saito S, Hirayama A, Honye J, Chiku M, Yoda T, et al. Investigation into effectiveness of Shock Wave treatment for Angina Pectoris patients post-bypass surgery. Eur Heart J. 2008;29:200.
Gabrusenko S, Malakhov V, Shitov V, Sankova A, Sergienko V, Masenko V, et al. An experience of the use of a curative metod of cardiac shock wave therapy in patients with ischemic heart disease. Kardiologiya. 2013;53:20–6.
Cai HY, Li L, Guo T, Wang Y, Ma TK, Xiao JM, et al. Cardiac shockwave therapy improves myocardial function in patients with refractory coronary artery disease by promoting VEGF and IL-8 secretion to mediate the proliferation of endothelial progenitor cells. Exp Ther Med. 2015;10:2410–6.
Kikuchi Y, Ito K, Ito Y, Shiroto T, Tsuburaya R, Aizawa K, et al. Double-blind and placebo-controlled study of the effectiveness and safety of extracorporeal cardiac shock wave therapy for severe angina pectoris. Circ J. 2010;74:589–91.
Ruiz-Garcia J, Lerman A. Cardiac shock-wave therapy in the treatment of refractive angina pectoris. Interv Cardiol. 2011;3(2):191-201.
Wang J, Zhou C, Liu L, Pan X, Guo T. Clinical effect of cardiac shock wave therapy on patients with ischemic heart disease: a systematic review and meta-analysis. Eur J Clin Invest. 2015;45(12):1270–85.
Chaussy C, Brendel W, Schmiedt E. Extracorporeally induced destruction of kidney stones by shock waves. Lancet. 1980;2:1265–8.
Turk C, Knoll T, Petrik A, Sarica K, Skolarikos A, Straub M, Seitz C. European Association of Urology, Guidelines on Urolithiasis. 2015. p. 1–71.
Tandan M, Reddy DN, Santosh D, Reddy V, Koppuju V, Lakhtakia S, et al. Extracorporeal shock wave lithotripsy of large difficult common bile duct stones: efficacy and analysis of factors that favour stone fragmentation. J Gastroenterol Hepatol. 2009;24:1370–4.
Parsi MA, Stevens T, Lopez R, Vargo JJ. Extracorporeal shock wave lithotripsy for prevention of recurrent pancreatitis caused by obstructive pancreatic stones. Pancreas. 2010;39:153–5.
Capaccio P, Torreta S, Pignataro L. Extracorporeal lithotripsy techniques for salivary stones. Otorungol Clin North Am. 2009;42:1139–59.
Zelle BA, Gollwitzer H, Zlowodzki M, Buhren V. Extracorporeal shock wave therapy:current evidence. J Orthop Trauma. 2010;24 Suppl 1:S66–70.
Wang CJ, Cheng JH, Kuo YR, Schaden W, Mittermayr R. Extracorporeal shockwave therapy in diabetic foot ulcers. Int J Surg. 2015. doi:10.1016/j.ijsu.2015.06.024.
Vahdatpour B, Alizadeh F, Moayednia A, Emadi M, Khorami MH, Haghdani S. Efficacy of extracorporeal shock wave therapy for the treatment of chronic pelvic pain syndrome: a randomized, controlled trial. ISRN Urology. 2013:972601. doi:10.1155/2013/972601..
Maisonhaute E, Prado C, White PC, Compton RG. Surface acoustic cavitation understood via nanosecond electrochemistry. Part III: shear stress in ultrasonic cleaning. Ultrason Sonochem. 2002;9:297–303.
Ito Y, Ito K, Shiroto T, Tsuburaya YGJ, Takeda M, et al. Cardiac shock wave therapy ameliorates left ventricular remodeling after myocardial ischemia-reperfusion injury in pigs in vivo. Coron Artery Dis. 2010;21:304–11.
Gotte G, Amelio E, Russo S, Marlinghaus E, Musci G, Suzuki H. Short-time non-enzmatic nitric oxide synthesis from L-arginine and hydrogen peroxide induced by shock waves treatment. FEBS Lett. 2002;520:153–5.
Mariotto S, Cavalieri E, Amelio E, Ciampa AR, de Prati AC, Marlinghaus E, et al. Extracorporeal shock waves: from lithotripsy to anti-inflamatory action by NO production. Nitric Oxide. 2005;12:89–96.
Mariotto S, de Prati AC, Cavalieri E, Amelio E, Marlinghaus E, Suzuki H. Extracorporeal shock wave therapy in inflammatory diseases: molecular mechanism that triggers anti-inflammatory action. Curr Med Chem. 2009;16:2366–72.
Yip JK, Chang LT, Sun CK, Youssef AA, Sheu JJ, Wang CJ. Shock wave therapy applied to rat bone marrow-derived mononuclear cells enhances formation of cells stained positive for CD31 and vascular endothelial growth factor. Circ J. 2008;72:150–6.
Ciampa AR, de Prati AC, Amelio E, Cavalieri E, Persichini T, Colasanti M, et al. Nitric oxide mediates anti-inflammatory action of extracorporeal shock waves. FEBS Lett. 2005;579:6839–45.
Kaller M, Faber L, Bogunovic N, Horstkotte D, Burchert W, Lindner O. Cardiac shock wave therapy and myocardial perfusion in severe coronary artery disease. Clin Res Cardiol. 2015;104(10):843–9.
Zuoziene G, Laucevicius A, Leibowitz D. Extracorporeal shockwave myocardial revascularization improves clinical symptoms and left ventricular function in patients with refractory angina. Coron Artery Dis. 2012;23:62–7.
Gutersohn A, Caspari G, Erbel R. Cardiac shock wave therapy: new option for endstage cardiovascular disease. Atherosclerosis Suppl. 2003;4(2):3P-0626.
Gutersohn A, Caspari G, Erbel R. Autoangiogenesis induced by Cardiac Shock Wave Therapy (CSWT) increases perfusion and exersice tolerance in endstage CAD patients with refractory angina. Presented at the 69th Annual Scientific Meeting of the Japanese Circulation Society 2005.
Gutersohn A, Caspari G, Erbel R. Short and long term clinical improvement in patients with refractory angina using Cardiac Shock Wave Therapy (CSWT). Presented at the ACC 2006.
Fukumoto Y, Ito A, Uwatoku T, Matoba T, Kishi T, Takeshita A, et al. Extracorporeal cardiac shock wave therapy ameliorates myocardial ischemia in patients with severe coronary artery disease. Coron Artery Dis. 2006;17(1):63–70.
Lyadov K, Uvarov A. Cardiac shock-wave therapy: First Experience. Presented at the 6th Mediterranean congress of PRM. 2006;181–2.
Naber C, Ebralidze T, Lammers S, Hakim G, Erbel R. Non invasive cardiac angiogenesis shock wave therapy increases perfusion and exercise tolerance in endstage CAD patients. Eur J Heart Fail. 2007;7:71.
Khattab A, Brodersen B, Schuermann-Kuchenbrandt D, Beurich H, Tölg R, Geist V, et al. Extracorporeal cardiac shock wave therapy: First experience in the everyday practice for treatment of chronic refractory angina pectoris. Int J Cardiol. 2007;121(1):84–5.
Naber C, Lammers S, Lind T, Müller N, Hakim G, Erbel R. Safety and efficacy of extracorporeal low energy shockwave application for the treatment of refractory angina pectoris and myocardial ischemia in patients with end-stage coronary artery disease. Medispec. 2008;1–16.
Wang Y, Guo T, Cai HY, Ma TK, Tao SM, Sun S, et al. Cardiac shock wave therapy reduces angina and improves myocardial function in patients with refractory coronary artery disease. Clin Cardiol. 2010;33:693–9.
Faber L, Lindner O, Prinz C, Fricke E, Hering D, Burchert W, et al. Echo-guided extracorporeal shock wave therapy for refractory angina improves regional myocardial blood flow as assessed by PET imaging. J Am Coll Cardiol. 2010;55(10A):A120.
Vainer J, Habets J, Lousberg A, Brans B, Schalla S, Waltenberger J. Cardiac shockwave therapy in patients with end-stage coronary artery disease and chronic refractory angina pectoris – mid term results. Eur Heart J. 2010;31(Abstract Supplement):198.
Alunni G, D’amico M, Meynet I, Andriani M, Giraudi E, Giorgi M, et al. A new treatment for patients with refractory angina: extracorporeal shockwave myocardial revascularization. Eur Heart J. 2011;32(Abstract Supplement):575.
Vainer J, Habets J, De Pont C, Lousberg A, Schalla S, Brans B, et al. Extracorporeal shockwave myocardial revascularization therapy (ESMR): an alternative for patients with end-stage coronary artery disease and chronic refractory angina pectoris? Eur Heart J. 2012;33(Abstract Supplement):782.
Alunni G, Meynet I, D’Amico M, Garrone P, Checco L, Marra S. Extracorporeal shockwave myocardial revascularization: a promising therapy for refractory angina. Cardiology. 2013;126 Suppl 2:390.
Zuoziene G. Evaluation of myocardium revascularization y cardiac shock wave therapy applying multimodal image analysis. Summary of doctoral dissertation. Vilnius University, 2013
Prinz C, Faber L, Lindner O, Bogunovic N, Hering D, Burchert D, et al. Echo-guided extracorporeal shock wave therapy for refractory angina improves regional myocardial blood flow as assessed by PET imaging. Eur Heart J. 2013;34 suppl 1:4007.
Faber L, Prinz C, Lindner O, Bogunovic N, Hering D, Burchert D, et al. Echo-guided extracorporeal shock wave therapy for refractory angina improves regional left ventricular function along with myocardial blood flow. Eur Heart J. 2014;35(Abstract Supplement):658.
Prasad M, Wan Ahmad WA, Sukmawan R, Magsombol EB, Cassar A, Vinshtok J, et al. Extracorporeal shockwave myocardial therapy is efficacious in improving symptoms in patients with refractory angina pectoris – a multicenter study. Coron Artery Dis. 2015;26:194–200.
Liu BY, Li WC, Zhang RS, Chen CX, Yao ZM, He Q. Application of extracorporeal cardiac shock wave therapy in treating coronary heart disease in the elderly. J Am Geriatr Soc. 2015;63:S408.
Vainer J, Habets JHM, Schalla S, Lousberg AHP, dePont CDJM, Voo SA, et al. Cardiac shockwave therapy in patients with chronic refractory angina pectoris. Neth Heart J. 2016;24:343–9.
Kazmi WH, Rasheed SZ, Ahmed S, Saadat M, Altaf S, Samad A. Noninvasive therapy for the management of patients with advanced coronary artery disease. Coron Artery Dis. 2012;23:549–54.
Alunni G, Marra S, Meynet I, D’amico M, Elisa P, Fanelli A, et al. The beneficial effect of extracorporeal shockwave myocardial revascularization in patients with refractory angina. Cardiovasc Revasc Med. 2015;16:6–11.
Nirala S, Wang Y, Peng YZ, Yang P, Guo T. Cardiac shock wave therapy shows better outcomes in the coronary artery disease patients in a long term. Eur Rev Med Pharmacol Sci. 2016;20:330–8.
Zhao L, Yang P, Tang Y, Li R, Peng Y, Wang Y, et al. Effect of cardiac shock wave therapy on the microvolt T wave alternans of patients with coronary artery disease. Int J Clin Exp Med. 2015;8:16463–71.
Schmid JP, Capoferri M, Schepis T, Siegrist P, Schroeder V, Kaufmann P, et al. Extracorporeal shock wave for therapy of refractory angina pectoris: the shock trial. Presented at the American College of Cardiology 55th Annual Scientific Session 2006.
Yang P, Peng Y, Guo T, Wang Y, Cai H, Zhou P. A clinical study of the extracorporeal cardiac shock wave therapy for coronary artery disease. Heart. 2012;98 Suppl 2:E163–4.
Leibowitz D, Weiss AT, Rott D, Durst R, Lotan C. The efficacy of cardiac shock wave therapy in the treatment of refractory angina: a pilot prospective, randomized, double-blind trial. Int J Cardiol. 2013;167:3033–4.
Schmid JP, Capoferri, Wahl A, Eshtehardi P, Hess OM. Cardiac shock wave therapy for chronic refractory angina pectoris. a prospective placebo-controlled randomized trial. Cardiovasc Ther. 2013;31:e1–6.
Yang P, Guo T, Wang W, Peng YZ, Wang Y, Zhou P, et al. Randomized and double-blind controlled clinical trial of extracorporeal cardiac shock wave therapy for coronary heart disease. Heart Vessels. 2013;28:284–91.
Acknowledgements
Not applicable.
Funding
No funding.
Availability of data and material
The datasets used and/ or analysed during the current study are available from the corresponding author on reasonable request.
Author’s contributions
GB participated in conception and design creation, collection and interpretation of data, drafting the manuscript. ES participated in conception and design creation, collection and interpretation of data, drafting the manuscript and revising it critically for important intellectual content and final approval of the manuscript submission. JC participated in conception and design creation, collection and interpretation of data, drafting the manuscript and revising it critically for important intellectual content. GZ participated in analysis and interpretation of data, drafting the manuscript. IB participated in analysis and interpretation of data, drafting the manuscript. BP participated in analysis and interpretation of data, drafting the manuscript. PS participated in analysis and interpretation of data, drafting the manuscript. AL participated in conception and design creation, analysis and interpretation of data, drafting the manuscript and revising it critically for important intellectual content and final approval of the manuscript submission. AL participated in analysis and interpretation of data, drafting the manuscript and revising it critically for important intellectual content and final approval of the manuscript submission. All authors read and approved the final manuscript.
Competing interests
GB has received investigator fees from Sanofi and Janssen Research; has received travel fee from Servier; has received research support from Medispec (applicators for study NCT02339454). ES has received consulting fee and research support from Medispec (applicators for study NCT02339454); has received speaker fee from Servier, GE Healthcare; has received investigator fees from Servier and Bayer. JC is a member of advisory board for Novartis; has received investigator fees from Amgen and Servier; has received research support from Medispec (applicators for study NCT02339454). GZ has received travel fee from Servier; has received research support from Medispec for Cardiac Shock wave study. IB has received investigator fee from Bioventrix. BP is a member of steering committee for Novartis and Janssen Research; has received speaker fees from Remedica, Astra Zeneca, Pfizer, Bayer and Beohringer -Ingelheim. PS has no competing interest. AL is a member of steering committee for Servier and Sanofi; has received research support from Medispec for Cardiac Shock wave study. AL has no competing interest.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Not applicable.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Burneikaitė, G., Shkolnik, E., Čelutkienė, J. et al. Cardiac shock-wave therapy in the treatment of coronary artery disease: systematic review and meta-analysis. Cardiovasc Ultrasound 15, 11 (2017). https://doi.org/10.1186/s12947-017-0102-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12947-017-0102-y