Abstract
Background
Implementing evidence-based management of dyslipidaemia is a challenge worldwide.
Objectives
To understand physician beliefs and behaviour and identify uncertainties in dyslipidaemia management across four world regions.
Methods
Web-based survey of 1758 physicians in Japan, Germany, Colombia and the Philippines who were selected randomly from existing databases. Key inclusion criteria were 1) for cardiologists and diabetes/endocrinology specialists: ≥50 dyslipidaemia patients examined in the last month; 2) for specialists in neurology/neurosurgery/stroke medicine: ≥50 dyslipidaemia patients and ≥ 20 patients with a history of ischaemic stroke examined in the last month; and 3) for specialists in nephrology and general medicine: based at centres with ≥20 beds and ≥ 50 dyslipidaemia patients examined in the last month. The self-report survey covered dyslipidaemia management, target low-density lipoprotein cholesterol (LDL-C) levels in different patient groups, and statin safety. All physicians gave voluntary consent and all data were anonymised. Analysis was solely descriptive.
Results
The survey highlighted key areas of uncertainty in dyslipidaemia management in the four countries. These related to LDL-C targets in different patient groups, the safety of low LDL-C levels, the safety of statins, especially for effects on cognitive, renal and hepatic function and for haemorrhagic stroke risk, and lipid management strategies in patients with chronic kidney disease, including those with concomitant hypertriglyceridaemia.
Conclusions
This survey of physicians in Japan, Germany, Colombia and the Philippines has identified key gaps in knowledge about dyslipidaemia management. These relate to the safety of low LDL-C levels, the safety of statins, and lipid management of chronic kidney disease. The findings from this survey highlight the need for further education to improve the implementation of guideline recommendations for dyslipidaemia management.
Similar content being viewed by others
Introduction
Extensive and robust evidence has established low-density lipoprotein cholesterol (LDL-C) as causal for atherosclerotic cardiovascular disease (ASCVD) [1]. Irrespective of therapeutic strategy, lowering LDL-C levels reduces the risk of ASCVD events, as demonstrated in major cardiovascular outcomes studies in very high-risk patients treated with a statin [2] or non-statin therapy (i.e. ezetimibe or proprotein convertase subtilisin/kexin type 9 [PCSK9] inhibitors) [3,4,5]. The safety of these LDL-lowering therapies has also been demonstrated [2,3,4,5]. Despite this overwhelming body of evidence, controversy persists regarding the role of LDL-C as a cause of ASCVD. Frequent, non-evidence-based assertions published in the media suggest that statins are unsafe and that lowering LDL-C to very low levels is dangerous [6]. There is also uncertainty regarding the veracity of adverse effects of statins, including statin-associated muscle symptoms [7, 8]. Similarly, safety concerns have been raised regarding novel therapies, including the PCSK9 inhibitors [9].
The World Heart Federation has developed a series of ‘roadmaps’ which aim to reduce cardiovascular disease in developing world regions. One of these roadmaps has focused on identifying barriers to effective cholesterol management gaps in knowledge and practice [10]. There is little information, however, regarding the beliefs and behaviour of physicians responsible for managing patients with dyslipidaemia in their routine practice. To address this issue, an online survey was conducted in Japan in 2017 by the Japan Atherosclerosis Society in collaboration with the International Atherosclerosis Society (IAS) to determine the attitudes and practice of physicians responsible for lipid management [11]. Subsequent to this, a second survey in Japan and surveys in Colombia, Germany and the Philippines were conducted by the IAS. These aimed to evaluate cultural differences among physicians in their beliefs and routine practice of managing dyslipidaemia.
Methods
This study was designed as a web-based survey, using an online questionnaire. The project was coordinated by the IAS. The IAS convened a committee, chaired by PB, RS, PL, SY, RDS, AR and UL, which was responsible for developing and implementing the survey in each country.
Physicians were selected randomly from existing databases in each country. In Japan, physician recruitment was conducted by CareNet, Inc., an online Japanese-language medical information service for physicians. All prospective participants were registered members of CareNet, Inc., and received an email introducing the study and inviting them to participate. In Germany, physicians were selected from a market research panel of approximately 17,000 doctors. In Colombia, a local healthcare fieldwork partner recruited physicians via e-mail and telephone. Finally, in the Philippines, physicians were recruited from a database created from an online ‘e-survey’ of internists, cardiologists and vascular specialists attending annual clinical conventions, or by questionnaires distributed at a workshop for cardiologists, and a local chapter convention for internists. In all countries, physicians who met the following criteria were accepted for inclusion in the survey: (i) expertise in cardiology, diabetes or endocrinology and treating ≥50 patients with dyslipidaemia in the previous month; (ii) expertise in neurology, neurosurgery or stroke medicine and treating ≥50 patients with dyslipidaemia and ≥ 20 patients with a history of ischaemic stroke in the previous month; and (iii) expertise in nephrology and general internists based at hospitals with ≥20 beds and treating ≥50 patients with dyslipidaemia in the previous month. All physicians gave voluntary consent before participation.
The study used a self-report web-based survey, which required 15–30 min for completion (Table 1). Briefly, the survey comprised 23 multiple choice questions that aimed to investigate beliefs and behaviour in the management of dyslipidaemia. These included questions relating to the role of LDL-C in ASCVD, target LDL-C levels in different patient groups, safety issues relating to low LDL-C levels and statin use, awareness and management of familial hypercholesterolaemia (FH), and current practice for the management of hypertriglyceridaemia in patients with chronic kidney disease (CKD). Data were anonymised and analysed descriptively by the authors. Categorical data were described as absolute numbers and percentages. No formal statistical analyses comparing different countries or different medical specialties were performed.
Results
A total of 1758 physicians, 508 in Japan, 500 in Germany, 345 in Colombia, and 405 in the Philippines, took part in the survey. Across all four countries, most respondents were either general physicians (33%) or cardiologists (22%) (Table 2). Results are summarised below for findings that show either agreement or uncertainty between countries.
Agreement between countries
There was universal agreement in all four countries (95–99% of respondents) that an elevated LDL-C level is an important cause of coronary disease and ischaemic stroke. Recent efforts aimed at educating clinicians about FH have improved awareness, as > 95% of respondents in all four countries were aware about FH, and between 56% (in the Philippines) and 85% (in Germany) of physicians either treated FH patients or referred them to a specialist centre. Most physicians (81–92%) believed that FH patients were also at increased risk of ischaemic stroke (Fig. 1).
Agreement between physicians in Japan, Germany, Colombia and the Philippines for survey questions relating to familial hypercholesterolaemia and the management of LDL cholesterol in chronic kidney disease (CKD). Abbreviations: ASCVD atherosclerotic cardiovascular disease; LDL low-density lipoprotein
There was also agreement between all four countries that lowering LDL-C reduces the risk of ASCVD events in CKD patients (ranging from 70% of respondents in Germany to 94% in the Philippines) (Fig. 1). Most respondents believed that there was a benefit from using statins at any stage of CKD. Across the countries, between 31% (in Japan) and 61% (in the Philippines) of respondents believed that the statin dose should be reduced in patients with CKD (Fig. 1).
Uncertainty between countries
The survey identified several areas of uncertainty in dyslipidaemia management, both within and across the four countries.
Target LDL-C levels
In people with established coronary heart disease, the target LDL-C level proposed by physicians varied, from 2.48 mmol/L (96 mg/dL) in Japan, 2.22 mmol/L (86 mg/dL) in Germany, 2.10 mmol/L (85 mg/dL) in the Philippines, to 2.07 mmol/L (80 mg/dL) in Colombia. Respondents in three countries believed that the target LDL-C level should be higher in people with diabetes, CKD or peripheral artery disease but without coronary heart disease (2.84 mmol/L [110 mg/dL] in Japan, 2.43 mmol/L [94 mg/dL] in Germany, and 2.25 mmol/L [87 mg/dL] in Colombia). In primary prevention patients without these conditions, the proposed target LDL-C levels were higher, ranging from 3.39 mmol/L (131 mg/dL) in Japan, 3.34 mmol/L (129 mg/dL) in Germany, 2.97 mmol/L (115 mg/dL) in Colombia and 2.72 mmol/L (105 mg/dL) in the Philippines. In Japan, Germany and the Philippines less than half of the respondents, versus 75% in Colombia, used non-high-density lipoprotein cholesterol either to determine global risk or as a therapeutic target.
Management of CKD
Beliefs regarding the target LDL-C level in CKD patients varied between the four countries. In Japan, 67% of respondents believed that the target LDL-C should be < 3.1 mmol/L (120 mg/dL). In the other three countries, between 40% (in the Philippines) and 57% (in Colombia) believed that the target LDL-C should be < 2.6 mmol/L (100 mg/dL), and between 21% (in Germany) and 27% (in Colombia and the Philippines) believed that the target LDL-C should be < 1.8 mmol/L (70 mg/dL). The perceived clinical benefit of treating CKD patients with hypertriglyceridaemia also varied between countries, from 91% in Colombia to 42% in Germany. While the pharmacotherapeutic options for hypertriglyceridaemia in CKD were similar in the four countries (statins, fibrates and omega-3 fatty acids), 30% of physicians in Germany believed that lifestyle modification alone was the most appropriate treatment for CKD.
Safety of low LDL-C levels
About half of the respondents in the four countries had concerns about the safety of low LDL-C levels (≤1.29 mmol/L or ≤ 50 mg/dL) (Table 3). The risk for haemorrhagic stroke with low LDL-C levels was a key concern, although there was also uncertainty (40% of clinicians in Japan and Germany, 38% in Colombia and 44% in the Philippines were uncertain about this issue).
Statin safety
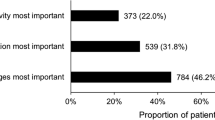
Physicians in all four countries recognised that a small proportion of patients are unable to use statins continuously due to adverse effects. Estimates of the percentage of affected patients varied from < 5% reported by most respondents in Japan, Colombia and the Philippines, to 5–15% reported by half of respondents in Germany. The survey highlighted uncertainty in all four countries regarding the effects of statins on cognitive, renal, and hepatic function (Fig. 2). A substantial proportion of respondents in each of the four countries was uncertain whether statins adversely affect cognitive function (24% in Germany, 26% in Colombia, 36% in the Philippines and 42% in Japan), or renal function (16% in Germany, 8% in Colombia, 13% in the Philippines and 36% in Japan).
Discussion
This survey has identified gaps in knowledge and behaviour amongst physicians managing dyslipidaemia in Japan, Germany, Colombia and the Philippines (Summary figure (Fig. 3)).
It is reassuring that there is almost universal agreement across all four countries regarding the causality of LDL-C in ASCVD. In addition, there is evidence of improvement in FH awareness and care, possibly reflecting a renewed focus from expert consensus groups [12, 13]. This builds on findings from the initial physician survey in Japan, which highlighted underdiagnosis of FH, especially among general practitioners, as an issue [11]. Despite the availability of well-developed evidence-based guidelines for dyslipidaemia management in each country or respective world region, areas of disagreement/uncertainty were identified [14,15,16,17]. These related to the safety of statin therapy, the safety of very low LDL-C levels, and dyslipidaemia management in CKD.
Consistent with the initial survey of physician attitudes in dyslipidaemia management in Japan [11], there were concerns regarding the safety of very low LDL-C levels attained on a statin (with or without other lipid modifying therapy). In the current report, these primarily focus on cognitive and renal function, as well as the risk of haemorrhagic stroke. While there is compelling evidence that a very low level of LDL-C may increase the risk of haemorrhagic stroke [18], especially in Asians [19], it is pertinent that there was no increase in risk at very low LDL-C levels attained by adding ezetimibe [3] or a PCSK9 inhibitor [4, 5] to background statin therapy in major clinical trials. Moreover, the well-documented reduction in the risk of ischaemic stroke in individuals who attain very low LDL-C levels outweighs any possible increase in the risk of a haemorrhagic stroke [2,3,4, 20]. With respect to cognitive adverse effects, the EBBINGHAUS study specifically investigated the effect of very low LDL-C levels using a computerised battery of tests for a range of cognitive domains including episodic and working memory, executive function, psychomotor speed and attention. This study showed no change in cognitive function even at very low LDL-C levels (0.28–0.44 mmol/L or 11–17 mg/dL) attained with the addition of a PCKS9 inhibitor [21]. It should be noted, however, that the duration of treatment with a PCSK9 inhibitor in this trial was relatively short and that longer-term data are still needed. There is no convincing evidence that the use of statins or attainment of a low LDL-C level causes renal dysfunction [2, 8]. Indeed, subgroup analyses from several major studies suggest that statins may have a renoprotective effect which merits further study [22].
Management of dyslipidaemia in CKD patients was another area of uncertainty in all four countries. There was a lack of consensus regarding the perceived need to reduce the statin dose in patients with CKD, the need for different LDL-C target levels depending on the stage of the CKD, as well as the clinical benefit of treating hypertriglyceridaemia in CKD patients.
The authors recognise several limitations relating to the methodology of this survey. First, physicians were recruited to the survey using a variety of approaches, including random selection from existing databases, contact via email and/or telephone, and recruitment from expert-led workshops. Second, the survey was self-report. Another potential source of relates to the distribution of specialties in the countries. Whereas in Japan and Germany there was an equal distribution across all specialties, in both Colombia and the Philippines, about half of all physicians were general physicians (46 and 55%, respectively). Thus, the study findings may have been influenced by differences in the knowledge base between different specialties. Indeed, this was evident in the initial survey conducted in Japan, in which cardiologists were shown to treat LDL-C more aggressively than those in other specialties or in general practice. Results from the PERCRO-DOC survey of more than 1300 randomly selected physicians in Croatia also indicated differences in the approach to cardiovascular prevention between general practitioners and hospital specialists. General practitioners were less likely to refer to guidelines compared with cardiologists and internists [23].
The extent to which the findings from this survey can be extrapolated to other countries is uncertain. Despite this, the results provide several important ‘take-home’ messages for physicians. In all four countries, there are key gaps in beliefs and practice that contribute to a roadblock for treatment of dyslipidaemia in people at high risk of ASCVD [10]. This was also evident in the initial physician survey; while most physicians (~ 80%) believed they treated dyslipidaemia appropriately, only about half (53.3%) knew the LDL-C target for high-risk patients. Moreover, only about half recognised the level at which high-density lipoprotein cholesterol was a marker of increased risk [11]. Similar findings were reported in the PERCRO-DOC survey [23]. Importantly, retrospective analysis of LDL-C goal attainment in more than 4000 outpatients in Italy in a real-world setting showed that less than 10% of patients considered at high or very high risk attained guideline-recommended LDL-C goals [24]. Real-world data derived from the Cegedim Longitudinal Practice Database in Germany, as well as observational findings from 18 countries outside Western Europe, also indicated inadequate use of lipid lowering therapy in high and very high-risk patients [25, 26].
Taken together, these findings highlight the need for educational programmes to increase awareness of the current evidence base supporting dyslipidaemia management. Where evidence is lacking, research is needed to address uncertainties, as well as education to put unresolved issues in perspective. Comparable surveys are also needed in North America, Eastern Europe and the Middle East to extend knowledge and improve dyslipidaemia management across all world regions.
Conclusions
In conclusion, this survey provides a ‘snapshot’ of the beliefs and behaviour of physicians in Japan, Germany, Colombia and the Philippines who are involved in managing patients with dyslipidaemia in their routine practice. The findings highlight key areas of need for further education and research. The results provide a rationale for similar surveys in other countries, as well as follow-up surveys to assess the impact of any educational programmes and activities on these gaps in belief and practice in dyslipidaemia management.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ASCVD:
-
Atherosclerotic cardiovascular disease
- CKD:
-
Chronic kidney disease
- FH:
-
Familial hypercholesterolaemia
- LDL-C:
-
Low-density lipoprotein cholesterol
- PCSK9:
-
Proprotein convertase subtilisin/kexin type 9
References
Ference BA, Ginsberg HN, Graham I, Ray KK, Packard CJ, Bruckert E, et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. Evidence from genetic, epidemiologic, and clinical studies. A consensus statement from the European atherosclerosis society consensus panel. Eur Heart J. 2017;38:2459–72.
Collins R, Reith C, Emberson J, Armitage J, Baigent C, Blackwell L, et al. Interpretation of the evidence for the efficacy and safety of statin therapy. Lancet. 2016;388:2532–61.
Cannon CP, Blazing MA, Giugliano RP, McCagg A, White JA, Theroux P, et al. Ezetimibe added to statin therapy after acute coronary syndromes. N Engl J Med. 2015;372:2387–97.
Sabatine MS, Giugliano RP, Keech AC, Honarpour N, Wiviott SD, Murphy SA, et al. Evolocumab and clinical outcomes in patients with cardiovascular disease. N Engl J Med. 2017;376:1713–22.
Schwartz GG, Steg PG, Szarek M, Bhatt DL, Bittner VA, Diaz R, et al. Alirocumab and cardiovascular outcomes after acute coronary syndrome. N Engl J Med. 2018;379:2097–107.
Nissen SE. Statin denial: an internet-driven cult with deadly consequences. Ann Intern Med. 2017;167:281–2.
Gupta A, Thompson D, Whitehouse A, Collier T, Dahlof B, Poulter N, et al. Adverse events associated with unblinded, but not with blinded, statin therapy in the Anglo-Scandinavian cardiac outcomes trial-lipid-lowering arm (ASCOT-LLA): a randomised double-blind placebo-controlled trial and its non-randomised non-blind extension phase. Lancet. 2017;389:2473–81.
Mach F, Ray KK, Wiklund O, Corsini A, Catapano AL, Bruckert E, et al. Adverse effects of statin therapy: perception vs. the evidence - focus on glucose homeostasis, cognitive, renal and hepatic function, haemorrhagic stroke and cataract. Eur Heart J. 2018;39:2526–39.
Mannarino MR, Sahebkar A, Bianconi V, Serban MC, Banach M, Pirro M. PCSK9 and neurocognitive function: should it be still an issue after FOURIER and EBBINGHAUS results? J Clin Lipidol. 2018;12:1123–32.
Murphy A, Faria-Neto JR, Al-Rasadi K, Blom D, Catapano A, Cuevas A, et al. World heart federation cholesterol roadmap. Glob Heart. 2017;12:179–97.
Yamashita S, Masuda D, Arai H, Matsuzawa Y. Cultural barriers in the treatment of dyslipidemia: a survey of Japanese physician attitudes. J Atheroscler Thromb. 2018;26:154–69.
Nordestgaard BG, Chapman MJ, Humphries SE, Ginsberg HN, Masana L, Descamps OS, et al. Familial hypercholesterolaemia is underdiagnosed and undertreated in the general population: guidance for clinicians to prevent coronary heart disease: consensus statement of the European atherosclerosis society. Eur Heart J. 2013;34:3478–90a.
Santos RD, Gidding SS, Hegele RA, Cuchel MA, Barter PJ, Watts GF, et al. Defining severe familial hypercholesterolaemia and the implications for clinical management: a consensus statement from the international atherosclerosis society severe familial hypercholesterolemia panel. Lancet Diabetes Endocrinol. 2016;4:850–61.
Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L, et al. 2019 ESC/EAS guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J. 2020;41:111–88.
Kinoshita M, Yokote K, Arai H, Iida M, Ishigaki Y, Ishibashi S, et al. Japan atherosclerosis society (JAS) guidelines for prevention of atherosclerotic cardiovascular diseases 2017. J Atheroscler Thromb. 2018;25:846–984.
Herdy AH, Lopez-Jimenez F, Terzic CP, Milani M, Stein R, Carvalho T, et al. South American guidelines for cardiovascular disease prevention and rehabilitation. Arq Bras Cardiol. 2014;103(2 Suppl 1):1–31.
Guerrero AE. 2015 clinical practice guidelines for the Management of Dyslipidemia in the Philippines - executive summary: dyslipidemia guidelines 2015. ASEAN Heart J. 2016;24:7.
Zhang X, Liu J, Wang M, Qi Y, Sun J, Liu J, et al. Twenty-year epidemiologic study on LDL-C levels in relation to the risks of atherosclerotic event, hemorrhagic stroke, and cancer death among young and middle-aged population in China. J Clin Lipidol. 2018;12:1179–89.
Ma C, Gurol ME, Huang Z, Lichtenstein AH, Wang X, Wang Y, et al. Low-density lipoprotein cholesterol and risk of intracerebral hemorrhage: a prospective study. Neurology. 2019;93:e445–e57.
Amarenco P, Kim JS, Labreuche J, Charles H, Abtan J, Béjot Y, et al. A comparison of two LDL cholesterol targets after ischemic stroke. N Engl J Med. 2019. https://doi.org/10.1056/NEJMoa1910355.
Giugliano RP, Mach F, Zavitz K, Kurtz C, Im K, Kanevsky E, et al. Cognitive function in a randomized trial of evolocumab. N Engl J Med. 2017;377:633–43.
Bangalore S, Fayyad R, Hovingh GK, Laskey R, Vogt L, DeMicco DA, et al. Statin and the risk of renal-related serious adverse events: analysis from the IDEAL, TNT, CARDS, ASPEN, SPARCL, and other placebo-controlled trials. Am J Cardiol. 2014;113:2018–20.
Reiner Z, Sonicki Z, Tedeschi-Reiner E. Physicians' perception, knowledge and awareness of cardiovascular risk factors and adherence to prevention guidelines: the PERCRO-DOC survey. Atherosclerosis. 2010;213:598–603.
Presta V, Figliuzzi I, Miceli F, Coluccia R, Fogacci F, Cicero AFG, et al. Achievement of low density lipoprotein (LDL) cholesterol targets in primary and secondary prevention: analysis of a large real practice database in Italy. Atherosclerosis. 2019;285:40–8.
März W, Dippel FW, Theobald K, Gorcyca K, Iorga ŞR, Ansell D. Utilization of lipid-modifying therapy and low-density lipoprotein cholesterol goal attainment in patients at high and very-high cardiovascular risk: real-world evidence from Germany. Atherosclerosis. 2018;268:99–107.
Danchin N, Almahmeed W, Al-Rasadi K, Azuri J, Berrah A, Cuneo CA, et al. Achievement of low-density lipoprotein cholesterol goals in 18 countries outside Western Europe: the international ChoLesterol management practice study (ICLPS). Eur J Prev Cardiol. 2018;25:1087–94.
Acknowledgements
Not applicable.
Funding
This study was supported by an unrestricted grant from Amgen to the International Atherosclerosis Society. In the Philippines, Merck Sharpe & Dome (Philippines) helped in setting up the platform for the questionnaires and the Philippine Lipid and Atherosclerosis Society provided financial support for the survey.
RDS is a recipient of a scholarship from the Conselho Nacional de Pesquisa e Desenvolvimento Tecnologico (CNPq), Brazil, process # 303734/2018–3.
Author information
Authors and Affiliations
Contributions
PJB, RDS and PL conceived the study and analysed the data. All authors were involved in drafting and review of the manuscript. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval was not applicable. All physicians participating in the survey gave voluntary consent and data were fully anonymised.
Consent for publication
Not applicable.
Competing interests
PJB has received honoraria for lectures given for Amgen, Pfizer and Sanofi Regeneron and has been a member of Scientific Advisory Boards for Amgen, Merck, Pfizer and Sanofi Regeneron. SY has received grants or honoraria for lectures from Kowa, Otsuka Pharmaceutical, Shionogi & Co, Bayer Yakuhin, MSD K. K, Takeda, Sanwa Kagaku Kenkyusho Co, Ono Pharmaceutical Company, Astellas Pharma, Daiichi-Sankyo, Mochida, Kaken, Astra Zeneca, Skylight Biotech, Astellas Amgen, Sanofi, Aegerion, and Kyowa Medex. UL has received honoraria for consulting or lectures from Amgen, Bayer, Boehringer, Sanofi/Regeneron. AJR has received honoraria for lectures from Sanofi, Pfizer, AstraZeneca and Valentech and payment for participation in advisory boards from Sanofi and Amgen. RS has received research grant and lecture honorarium from Sanofi, MSD and Pfizer. PL is an unpaid consultant to, or involved in clinical trials for Amgen, AstraZeneca, Esperion Therapeutics, Ionis Pharmaceuticals, Kowa Pharmaceuticals, Novartis, Pfizer, Sanofi-Regeneron XBiotech, Inc. PL is a member of scientific advisory boards for Amgen, Athera biotechnologies, Corvidia Therapeutics, DalCor Pharmaceuticals, IFM Therapeutics, Kowa Pharmaceuticals, Olatec Therapeutics, Medimmune, Novartis and his laboratory has received research funding in the last 2 years from Novartis. YM has received honoraria for consulting or lectures from Teijin Pharma and Kowa. RDS has received honoraria for consulting, speaker activities and or research from Ache, Amgen, Astra Zeneca, Esperion, Kowa, Novo-Nordisk, Merck, MSD, Pfizer, PTC and Sanofi/Regeneron. MDGF and EF have no conflicts to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Barter, P.J., Yamashita, S., Laufs, U. et al. Gaps in beliefs and practice in dyslipidaemia management in Japan, Germany, Colombia and the Philippines: insights from a web-based physician survey. Lipids Health Dis 19, 131 (2020). https://doi.org/10.1186/s12944-020-01265-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12944-020-01265-z