Abstract
Background
Acute high level carbon monoxide (CO) exposure can cause immediate cardio-respiratory arrest in anyone, but the effects of lower level exposures in susceptible persons are less well known. The percentage of CO-bound hemoglobin in blood (carboxyhemoglobin; COHb) is a marker of exposure and potential health outcomes. Indoor air quality guidelines developed by the World Health Organization and Health Canada, among others, are set so that CO exposure does not lead to COHb levels above 2.0%, a target based on experimental evidence on toxicodynamic relationships between COHb and cardiac performance among persons with cardiovascular disease (CVD). The guidelines do not consider the role of pathophysiological influences on toxicokinetic relationships. Physiological deficits that contribute to increased CO uptake, decreased CO elimination, and increased COHb formation can alter relationships between CO exposures and resulting COHb levels, and consequently, the severity of outcomes. Following three fatalities attributed to CO in a long-term care facility (LTCF), we queried whether pathologies other than CVD could alter CO-COHb relationships. Our primary objective was to inform susceptibility-specific modeling that accounts for physiological deficits that may alter CO-COHb relationships, ultimately to better inform CO management in LTCFs.
Methods
We reviewed experimental studies investigating relationships between CO, COHb, and outcomes related to health or physiological outcomes among healthy persons, persons with CVD, and six additional physiologically susceptible groups considered relevant to LTCF residents: persons with chronic obstructive pulmonary disease (COPD), anemia, cerebrovascular disease (CBD), heart failure, multiple co-morbidities, and persons of older age (≥ 60 years).
Results
We identified 54 studies published since 1946. Six studies investigated toxicokinetics among healthy persons, and the remaining investigated toxicodynamics, mainly among healthy persons and persons with CVD. We identified one study each of CO dynamics in persons with COPD, anemia and persons of older age, and no studies of persons with CBD, heart failure, or multiple co-morbidities. Considerable heterogeneity existed for exposure scenarios and outcomes investigated.
Conclusions
Limited experimental human evidence on the effects of physiological deficits relevant to CO kinetics exists to support indoor air CO guidelines. Both experimentation and modeling are needed to assess how physiological deficits influence the CO-COHb relationship, particularly at sub-acute exposures relevant to indoor environments. Such evidence would better inform indoor air quality guidelines and CO management in indoor settings where susceptible groups are housed.
Similar content being viewed by others
Background
Carbon monoxide is a colorless, odorless and tasteless gas produced from the incomplete combustion of carbon-containing fuels such as natural gas, oil, and wood. Common indoor sources include poorly maintained or improperly vented appliances such as furnaces, fireplaces, and gas stoves [1, 2]. Tobacco smoke and vehicles left idling in attached garages or near open windows and building air intakes also contribute to indoor concentrations [1, 2]. Intentional and unintentional indoor CO exposure is linked to substantial burden of disease world-wide [3,4,5].
Carbon monoxide toxicity is primarily mediated through hypoxic pathways, whereby CO molecules displace oxygen (O2) and bind to hemoglobin to form carboxyhemolgobin (COHb) [1, 6]. The concentration of COHb increases with concentration and duration of exposure. The increased presence of COHb in the blood and the resultant leftward shift in the O2 dissociation curve reduces O2 transport to and transfer at tissue sites. Other heme-containing molecules, such as myoglobin, are similarly affected [2, 7]. Organs with the highest metabolic demand, such as the heart and brain, are most sensitive to CO-induced tissue hypoxia. Less is known about non-hypoxic pathways of CO toxicity [1]. Among other direct effects, CO has been shown to activate immunological responses by interfering with nitric oxide (NO) production [8]. Clinical symptoms associated with the hypoxic effects of mild exposures are typically non-specific, and can include headache, nausea, and dizziness, while severe exposures, also called CO poisonings, can result in disorientation, unconsciousness, and cardio-respiratory arrest [1, 7]. Persons with cardiovascular (CVD) are considered most sensitive to CO exposure.
We undertook a review of indoor air guidelines for CO and their relevance to indoor settings that house susceptible persons following a CO poisoning incident that led to the evacuation and treatment of 24 occupants from one wing of a long-term care facility in Saskatchewan, Canada. Three of the evacuated residents died within a month of the incident. All three were elderly, with pre-existing co-morbidities, and CO was listed as a contributing factor in each death [9]. A power company technician was called to the facility on the morning of December 26, 2010, after several occupants reported experiencing headaches, dizziness and nausea overnight and throughout the previous day [10]. The technician measured CO concentrations of 63 ppm in the affected wing, triggering an evacuation. An investigation of the facility revealed the source to be a faulty boiler that had emitted CO into the ventilation system, which was then distributed to occupied spaces in the affected wing [10]. Carbon monoxide detectors were not required in the facility at the time of the incident and there were no specific provincial or municipal regulations requiring their use. Based on the data collected by the power company technician, which may underestimate true exposures since the facility was ventilated prior to their collection, we assume that concentrations in the facility would not have triggered CO detectors, which are designed to alarm at CO levels considered to be immediately hazardous to health [11]. This incident shows the serious consequences of indoor CO exposure among susceptible persons, even at levels below those that may be considered immediately hazardous.
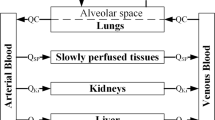
The World Health Organization (WHO) recommends that indoor air not exceed CO concentrations of 86 ppm, 30 ppm, 9 ppm, and 6 ppm for exposure periods of 15-min, 1-h, 8-h and 24-h, respectively. These guidelines are intended for use in settings such as homes, offices, schools, public buildings, and health care facilities [1]. Health Canada recommends that CO levels of 25 ppm and 10 ppm not be exceeded over periods of 1-h and 24-h, respectively, in guidelines intended for residential settings [12]. Similar methodologies were used to set WHO and Health Canada guidelines. Both guidelines are set so that short and long term exposures do not lead to COHb levels above 2.0%. Derived from controlled human exposure studies, this maximum acceptable level is based on observed changes in exercise electrocardiograms in subjects with ischemic heart disease. Both sets of guidelines also used the Coburn-Forster-Kane (CFK) equation to model CO-COHb relationships. This non-linear equation uses physiological parameters that influence CO uptake and elimination and COHb formation, such as the diffusing capacity of the lungs, alveolar ventilation rate, blood volume, and partial pressure of O2 in the pulmonary capillaries [1, 12, 13]. Health Canada’s guidelines were based on an adapted CFK model that includes additional parameters to account for CO in alveoli and CO-bound heme proteins in extravascular spaces [14]. All modeling scenarios were based on physiological parameters relevant to healthy adults, and as such, the setting of both WHO and Health Canada guidelines did not consider the role of physiological deficits on CO-COHb relationships.
We hypothesized that six groups in particular may be at increased risk of adverse effects: persons with COPD, anemia, cerebrovascular disease (CBD), heart failure, multiple co-morbidities, and persons of older age (≥ 60 years). COPD is characterized by lower diffusion capacity, greater alveolar dead space, and a higher degree of air trapping, all of which can decrease CO elimination [1, 6]. Additionally, persons with COPD may have secondary polycythemia [15], which can increase endogenous CO production. Persons with anemia have lower hemoglobin concentrations, which leads to less O2 binding to hemoglobin and therefore, lower blood O2 content. Additionally, persons with hemolytic anemia have higher baseline COHb levels due to higher rates of endogenous CO production that result from increased heme catabolism [1, 6, 16], and persons with sickle cell anemia may have increased alveolar dead space due to impaired pulmonary capillary perfusion [17]; both conditions would increase sensitivity to CO. Finally, decreased diffusing capacity, arterial degeneration and other circulatory changes among persons with heart failure, cerebrovascular (CBV) disease, persons of older age, and/or multiple co-morbidities can lead to lower baseline O2 content, and in some cases, a reduced capacity to vasodilate in response to increasing CO exposures [1, 6, 18,19,20]. The objective of this review was to investigate evidence on the kinetics of COHb formation as a joint function of CO exposure and altered uptake, distribution, and elimination of CO and O2 in these groups, as well as in healthy persons and persons with CVD.
Methods
We reviewed experimental studies in humans investigating relationships among CO, COHb, and outcomes in healthy persons, persons with CVD, and six additional susceptible groups: persons with COPD, anemia, CBD, heart failure, multiple co-morbidities, and persons of older age (≥ 60 years). Our intention was to capture all potential susceptibilities relevant to persons residing in long term care facilities. We selected susceptible groups based on (i) initial review of the rationale for indoor air quality guidelines for CO developed by the World Health Organization [1] and Health Canada [12], and ambient air quality criteria for CO developed by the U.S. Environmental Protection Agency [6], and (ii) expert consultation [21]. Our main objective was to review studies investigating CO-COHb relationships, but to capture all relevant information, we also reviewed studies investigating CO-COHb-outcome or COHb-outcome relationships. An outcome was considered to be any measured variable that could act as a surrogate for CO-related morbidity or mortality, including exercise duration, increases to cardiac output or heart rate, and cognitive effects. We identified articles though EBSCOhost (to access MEDLINE, CINAHL, PsycINFO, Biomedical Reference Collection, and Academic Search Complete), Ovid (to access Elsevier Science Direct, Evidence Based Medicine, SAGE journals online, and Cochrane Database of Systematic Reviews), and Google Scholar (to access books, book chapters, older articles, and articles from journals not indexed through major database platforms). We used broad keywords: “carboxyhemoglobin” or “carboxyhaemoglobin” and “carbon monoxide”.
The search was restricted to English language articles using an experimental study design. No date restrictions were imposed. We reviewed abstracts of studies to exclude those involving the investigation of smoking- or occupationally-related CO exposures. Additional research studies were identified by reviewing article bibliographies. The search was completed in March 2017.
Results
Our search identified 2394 articles, of which 54 were retained, after the removal of duplicates, implementation of inclusion/exclusion criteria, and manual review of abstracts (Fig. 1). All of the studies were published between 1946 and 2016. Only ten studies were published since 2000, with the majority (27) having been published between 1970 and 1990. Most studies involved healthy adults, predominantly young males (31) [22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50], and persons with cardiovascular disease (20) [51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70]. One study was conducted among persons with COPD [71], one was conducted among persons with disease-related anemia [72], and one among healthy older persons (aged ≥60 years) [73]. We found no studies conducted among persons with CBD, heart failure, or multiple co-morbidities.
Six studies investigated CO-COHb relationships [23, 27, 35, 36, 41, 42]. All of the studies were controlled exposure studies where subjects were exposed to a known CO concentration over a given time period, and the resulting COHb levels were measured during and/or after the exposure period. Exposures varied from 12 ppm for 48-h to 6683 ppm for 3–7 min. All studies but one included only healthy males ranging from 20 to 42 years [23, 27, 36, 41, 42]. Hauck and Neuberger [35] included a 10-year old female subject, in addition to three male subjects aged 22–36 years. Individual clinical and exercise-related factors that might have impacted COHb formation were not assessed or received little attention in all of these studies. In the earliest study, Forbes et al. [23] reported that CO uptake increased with physical work and duration of exposure. The remaining five studies evaluated the CFK equation against measured COHb levels [27, 35, 36, 41, 42].
Forty-nine studies investigated CO dynamics to understand the relationships between COHb concentrations and specific outcomes. One study ([36]) investigated both CO-COHb and COHb-outcome relationships. All but two studies used a double-blind crossover design where subjects were exposed to filtered air to establish low baseline COHb levels, followed by exposure scenarios corresponding to those required to reach target COHb levels of interest. Scenarios typically involved high exposures over short periods (e.g 7500 ppm for 1 min) or lower exposures over longer periods (e.g. 36 ppm over 4 h). In most studies, no rationale was provided for the exposure scenario or target COHb level of interest. Additionally, the focus of the studies was on observation of the effects of the target COHb levels, and no studies reported the duration of effects. Two studies used non-controlled exposures [47, 53]. Thomassen et al. [47] exposed seven subjects sitting in a tent to CO generated from a camp stove. Continuous CO measurements were collected throughout the 2-h study period and venous blood samples were collected every 15-min. Aronow et al. [53] investigated outcomes after subjects were exposed to freeway air while sitting in a car for 2 h; mean (standard deviation) CO concentrations were 47 (8) ppm, compared with scenarios where subjects were exposed to filtered air for 2 h [53].
The exposure scenarios differed greatly among the subject groups studied. Table 1 summarizes CO in air levels and durations, and resulting mean COHb levels for studies investigating toxicokinetic and toxicodynamic relationships. Differences in study design, including the exposure scenarios investigated, small sample sizes, as well as lack of reporting of baseline COHb levels limit comparisons of findings between studies, however, some comparisons are possible. Five studies investigated CO exposures of 100 pm CO for 1-h. Three of these studies were conducted among subjects with CVD (n = 24, 30, 41) [59, 63, 65], one was conducted among healthy subjects (10) [31], and one among subjects with COPD (n = 10) [71]. The mean change in COHb from baseline to post-exposure was highest in a study conducted in subjects with COPD (2.6%), compared with healthy subjects (2.3%) and in subjects with CVD (1.5, 2.1, and 2.4% for the three studies). Additionally, two studies which were conducted among subjects with CVD (n = 15) [58] and anemia [72] investigated CO exposures of 50 ppm for 1-h, (n = 10). The mean change in COHb was higher in the study conducted in subjects with anemia (1.2%) compared with that conducted in subjects with CVD (0.9%).
The outcome measures studied also varied by clinical population. In healthy subjects, outcome measures included exercise performance, cardiac function (e.g. changes to cardiac output, heart rate, and electrocardiogram tests), respiratory response (e.g. lung capacity, minute ventilation), and nervous system response (e.g. cognitive function, behavioral impairments). For subjects with CVD, the most commonly assessed outcome was exercise-induced angina. Exercise performance was the only outcome investigated in subjects with COPD and anemia, and cognitive function was the only outcome investigated in older persons (Table 2). The lowest level for which any effect was observed was at 2%. At this level, a decrease in mean length of time to a threshold ischemic ST-segment change and decreased time to onset of angina was observed among persons with ischemic heart disease. The relationship between COHb levels > 2% COHb and outcomes were investigated for our additional groups of interest.
Discussion
We reviewed evidence from 54 peer-reviewed experimental studies in humans investigating relationships between CO concentrations in air, COHb levels, and outcomes among healthy persons, those with CVD, and an additional six susceptible groups. Few studies have investigated the toxicokinetics of CO. Only six of the 54 studies identified in our search measured the relationship between CO exposure and COHb formation, and all six involved healthy participants. Since the objective of five of the six studies was to compare COHb levels predicted by the CFK model with measured levels following controlled exposures, few physiological parameters important to CO-COHb relationships were investigated. As for toxicodynamic studies, limited between-study comparison of CO-COHb levels is possible, taking into account pathophysiology. A higher mean increase in COHb from baseline to post-exposure was reported in a study of persons with COPD, compared with four studies of healthy persons or persons with CVD, at an equivalent CO exposure of 100 ppm for 1-h. Similarly, a higher mean increase in COHb was reported in a study of persons with anemia compared with a study of persons with CVD, at an equivalent CO exposure of 50 ppm for 1-h. Although findings from these studies cannot be directly compared for several reasons, including differing baseline COHb levels, the lack of subject-level data, and small sample sizes, the limited evidence does suggest that higher COHb levels may occur among some groups, likely due to underlying pathology, compared with healthy persons (or persons with CVD) at equivalent CO exposures. As we hypothesized, specific physiological deficits such as increased air trapping and greater alveolar dead space may increase CO absorption, decrease CO elimination, and/or increase COHb formation. Currently, WHO and Health Canada do not consider differences in toxicokinetics between susceptible groups in setting CO guidelines for indoor air, and instead assume that CO-COHb relationships estimated based on parameters reflecting those of healthy adults are representative of the entire population. These limited findings suggest that this may not be the case, and highlight the need for more evidence on CO-COHb relationships in susceptible groups.
Although experimental studies can allow for direct measure of CO-COHb relationships, there are limitations to the evidence these studies can provide. It is unethical to expose people to harmful CO levels, particularly over long periods of time. Additionally, it may not be appropriate to extrapolate findings on acute exposures to guidelines intended to protect persons from the effects of longer-term CO exposures, such as those intended for 24-h periods. An alternative to experimentation is the use of models that predict CO-COHb relationships. The use of models based on physiological deficits relevant to this relationship over a range of exposure scenarios can allow for a fuller understanding of CO-related susceptibility. Several empirical and mechanistic models have been developed to estimate the uptake and distribution of CO [74], including the widely used CFK equation [13, 75]. Other researchers have adapted the CFK equation to include additional physiological parameters in an attempt to more precisely predict CO-COHb relationships. An example is the setting Health Canada guidelines, which use an adapted CFK equation that incorporates parameters to account for CO in alveoli and CO-bound heme proteins in extravascular spaces [14]. Fewer studies, however, have attempted to model the effects of specific physiological deficits on CO-COHb relationships [76]. Benignus and Coleman 2010 [76] used a whole-body physiological model, which uses a form of the CFK equation, to simulate effects of CO on exercise duration among healthy persons and those with vascular disease at different exercise levels. Stenosis of the left heart arterial supply was introduced to simulate IHD, and stenosis of the cerebral arteries to simulate reductions in brain flow. For simulations involving IHD, the authors reported that the largest reductions in exercise duration were seen with the lowest severity of ischemia and COHb concentrations. For simulations involving reduced brain blood flow, a non-threshold effect on brain metabolism was seen for any increase in COHb levels when blood flow was reduced by more than 50%. In their Qualitative Risk and Exposure Assessment for Carbon Monoxide [77], the U.S. EPA used the CFK equation to model COHb levels in a simulated urban population with coronary heart disease. The population was assumed to be exposed to CO concentrations equivalent to the 8-h ambient CO standard of 9 ppm. The COHb levels in this population were estimated using a haemoglobin distribution relevant to the general population as well as an “anemic haemoglobin distribution” that was reflective of persons with anemia [77]. The percentage of the population with daily maximum COHb levels at or above 2% increased from 5.3% to 8.2% when the anemic haemoglobin distribution was used [77]. Modelling exercises such as these can be used to provide an understanding of how various sub-populations are affected under different CO exposure scenarios, which would not be possible with experimentation alone. Epidemiologic evidence can also inform our understanding of CO on susceptible persons, but must be interpreted with caution. Limited evidence suggests associations between 1 and 6 day ambient CO concentrations and increased emergency admissions for persons with COPD and sickle cell anemia [78,79,80,81]. However, recent studies have also suggested that low level ambient CO exposures, typically below 5 ppm, may be protective of some respiratory effects [82, 83]. More research is needed to assess how sub-acute and chronic CO exposures may affect these groups, including the mechanisms underlying these effects.
The majority of the studies (92%) we accessed attempted to characterize COHb-outcome relationships, predominantly among healthy persons. It is well characterized that the lowest COHb level at which an effect is seen is 2%. However, the degree to which severity of disease impacts this relationship has not been investigated. Additionally, equivalent sensitive outcomes, such as changes in ECG readings, have not been investigated in groups outside of those with CVD, making it difficult to compare CO sensitivity between potentially susceptible groups. The lack of data on CO effects among persons with multiple co-morbidities is also important, considering that individuals may have several conditions that potentially increase their overall susceptibility to CO. For example, persons with COPD are also likely to have CVD [84] and to a lesser degree, anemia [85]. The existing literature is also limited in other ways. While many studies reported mean COHb levels before and after CO exposures among all study subjects, few provided statistics on the distribution of COHb levels, including standard deviations around the mean, ranges, or subject-specific data. As noted earlier, study subjects consisted mainly of young healthy males, and where female and/or older subjects were included, reporting of results was insufficient to allow for examination of the role of sex or age on COHb-outcome relationships. Finally, much of the existing literature was published over 20 years ago. Improvements in measurement techniques have most likely led to more accurate CO and COHb measurements over time, and values reported in older studies are likely less reliable.
This review was conducted following a CO incident that was associated with three deaths in a long term care facility. Provincial or municipal regulations requiring CO detectors in Canadian health care facilities did not exist at the time of the incident. CO detector use has been shown to reduce CO poisonings in homes [86,87,88], and extending their use to other indoor settings would be beneficial, particularly where susceptible occupants are housed. However, CO detectors are only intended to prevent acute exposures at levels judged immediately hazardous to health, and therefore, it would be advantageous to consider ways to prevent low level exposures through comprehensive CO management programs based on education, prevention, and monitoring. In Canada as elsewhere, certified CO detectors are approved to alarm at levels considerably higher than those recommended by indoor air guidelines. Alarms are triggered when a peak value of 400 ppm is reached within 4–15 min, 150 ppm is reached within 15–50 min and when approximately 70 ppm is reached within 1–4 h [11]. These values are considered equivalent to an attained 10% COHb level, which is considerably higher than the 2% level used to derive guideline values. Certification and use of more sensitive detectors that both display and alarm at CO concentrations in the lower range would allow for better protection of the health of susceptible occupants.
Conclusions
Our review of the experimental literature found that few studies have examined CO-COHb relationships, and in general, persons with COPD, anemia, CBD, heart failure, persons of older age, as well as those with multiple co-morbidities have largely been overlooked in the experimental CO research. Indoor air guidelines, which are largely based on limited experimental research on CO toxicodynamics, do not take into account the potential impacts of physiological deficits that alter CO uptake and elimination as well as COHb formation. Susceptibility-specific toxicokinetic modelling is needed to better understand how CO-COHb relationships differ among susceptible groups. This information in turn, can better inform indoor air guidelines as well as CO management practices in indoor settings where susceptible persons are housed.
Abbreviations
- CBD:
-
Cerebrovascular disease
- CFK:
-
Coburn-Forster-Kane
- CO:
-
Carbon monoxide
- COHb:
-
Carboxyhemologbin
- COPD:
-
Chronic obstructive pulmonary disease
- CVD:
-
Cardiovascular disease
- IHD:
-
Ischemic heart disease
- O2 :
-
Oxygen
- WHO:
-
World Health Organization
References
World Health Organization. WHO guidelines for indoor air quality: selected pollutants. Geneva: WHO; 2010. http://www.euro.who.int/__data/assets/pdf_file/0009/128169/e94535.pdf.
Raub JA, Mathieu-Nolf M, Hampson NB, Thom SR. Carbon monoxide poisoning -- a public health perspective. Toxicology. 2000;145(1):1–14. https://doi.org/10.1016/s0300-483x(99)00217-6.
Lavigne E, Weichenthal S, Wong J, Smith-Doiron M, Dugandzic R, Kosatsky T. Mortality and hospital admission rates for unintentional nonfire-related carbon monoxide poisoning across Canada: a trend analysis. CMAJ Open. 2015;3(2):E223–30. https://doi.org/10.9778/cmajo.20140122.
Braubach M, Algoet A, Beaton M, Lauriou S, Heroux ME, Krzyzanowski M. Mortality associated with exposure to carbon monoxide in WHO European member states. Indoor Air. 2013;23(2):115–25. https://doi.org/10.1111/ina.%2012007.
Bronstein A, Clower JH, Iqbal S, Yip FY, Martin CA, Chang A, Wolkin AF, Bell J. Carbon monoxide exposures, United States, 2000-2009. Mor Mortal Wkly Rep CDC Surveill Summ. 2011;60(30):1014–7.
U.S. Environmental Protection Agency. Air quality criteria for carbon monoxide. 2000. https://cfpub.epa.gov/ncea/risk/recordisplay.cfm?deid=18163.
Agency for Toxic Substances and Drug Registry. Toxicological profile for carbon monoxide. Atlanta, GA: U.S. Department of Health and Human Services; 2012. https://www.atsdr.cdc.gov/toxprofiles/tp.asp?id=1145&tid=253
Rose JJ, Wang L, McTiernan C, Shiva C, Tejero J, Gladwin M. Carbon monoxide poisoning: pathogenesis, management, and future directions of therapy. Am J Respir Crit Care Med. 2017;195(5):596–606. https://doi.org/10.1164/rccm.201606-1275CI.
Saskatoon Health Region. Review of carbon monoxide exposure in St Mary’s Villa long term care facility Humboldt, Saskatchewan, December 26, 2010. Regina, SK: Saskatoon Health Region; 2011.
Saskatoon Health Region. Epidemiological analysis of residents of St. Mary's Villa, Humboldt, October 3–2010 - February 26, 2011. Regina, SK: Saskatoon Health Region; 2011.
Canadian Standards Association. CSA 6.19–01. Residential carbon monoxide alarming devices. 2001.
Health Canada. Residential indoor air quality guideline: carbon monoxide. Ottawa, ON: Health Canada; 2010. http://www.hc-sc.gc.ca/ewh-semt/pubs/air/carbon_mono/index-eng.php.
Coburn RF, Forster RE, Kane PB. Considerations of the physiological variables that determine the blood carboxyhemoglobin concentration in man. J Clin Invest. 1965;44(11):1899–910.
Gosselin NH, Brunet RC, Carrier G. Determination of carboxyhaemoglobin in humans following low-level exposures to carbon monoxide. Inhal Toxicol. 2009;21(13):1077–91. https://doi.org/10.3109/08958370902744848.
Kent BD, Mitchell PD, McNicholas WT. Hypoxemia in patients with COPD: cause, effects, and disease progression. Int J Chronic Obstr. 2011;6:199–208. https://doi.org/10.2147/COPD.S10611.
Sears DA, Udden MM, Thomas LJ. Carboxyhemoglobin levels in patients with sickle-cell anemia: relationship to hemolytic and vasoocclusive severity. Am J Med Sci. 2001;322(6):345–8.
Pianosi P, D'Souza SJ, Esseltine DW, Charge TD, Coates AL. Ventilation and gas exchange during exercise in sickle cell anemia. Am Rev Respir Dis. 1991;143(2):226–30.
Strait JB, Lakatta EG. Aging-associated cardiovascular changes and their relationship to heart failure. Heart Fail Clin. 2012;8(1):143–64. https://doi.org/10.1016/j.hfc.2011.08.011.
Morosin M, Vignati C, Novi A, Salvioni E, Veglia F, Alimento M, Merli G, Sciomer S, Sinagra G, Agostoni P. The alveolar to arterial oxygen partial pressure difference is associated with pulmonary diffusing capacity in heart failure patients. Respir Physiol Neurobiol. 2016;233:1–6. https://doi.org/10.1016/j.resp.2016.06.004.
Kee KK. Increased dead space ventilation mediates reduced exercise capacity in systolic heart failure. Am J Respir Crit Care Med. 2016;193(11):1292–300. https://doi.org/10.1164/rccm.201508-1555OC.
National Collaborating Centre for Environmental Health. Carbon monoxide monitoring in long term care facilities and hospitals. Carbon Monoxide Monitoring in Long Term Care Facilities and Hospitals: Experts Group Meeting. Vancouver, BC: National Collaborating Centre for Environmental Health; 2013. http://www.ncceh.ca/content/carbon-monoxide-monitoring-long-term-care-facilities-and-hospitals. Accessed 20 Feb 2017.
Pitts GC, Pace N. The effect of blood carboxyhemoglobin concentration on hypoxia tolerance. Am J Phys. 1947;148(1):139–51.
Forbes W, Sargent F, Roughton F. The rate of carbon monoxide uptake by normal men. Am J Phys. 1945;143(4):594–608.
Schulte JH. Effects of mild carbon monoxide intoxication. Arch Environ Health. 1963;7:524–30.
Chevalier RB, Krumholz RA, Ross JC. Reaction of nonsmokers to carbon monoxide inhalation. Cardiopulmonary responses at rest and during exercise. JAMA. 1966;198(10):1061–4.
Beard RR, Wertheim GA. Behavioral impairment associated with small doses of carbon monoxide. Am J Public Health Nations Health. 1967;57(11):2012–22.
Peterson JE, Stewart RD. Absorption and elimination of carbon monoxide by inactive young men. Arch Environ Health. 1970;21(2):165–71.
Stewart RD, Peterson JE, Baretta ED, Bachand RT, Hosko MJ, Herrmann AA. Experimental human exposure to carbon monoxide. Arch Environ Health. 1970;21(2):154–64.
Parving HH. The effect of hypoxia and carbon monoxide exposure on plasma volume and capillary permeability to albumin. Scand J Clin Lab Invest. 1972;30(1):49–56.
Vogel JA, Gleser MA, Wheeler RC, Whitten BK. Carbon monoxide and physical work capacity. Arch Environ Health. 1972;24(3):198–203.
Aronow WS, Cassidy J. Effect of carbon monoxide on maximal treadmill exercise. A study in normal persons. Ann Intern Med. 1975;83(4):496–9.
Horvath SM, Raven PB, Dahms TE, Gray DJ. Maximal aerobic capacity at different levels of carboxyhemoglobin. J Appl Physiol. 1975;38(2):300–3.
Davies DM, Smith DJ. Electrocardiographic changes in healthy men during continuous low-level carbon monoxide exposure. Environ Res. 1979;21(1):197–206. https://doi.org/10.1016/0013-9351(80)90022-5.
Putz VR. The effects of carbon monoxide on dual-task performance. Hum Factors. 1979;21(1):13–24.
Hauck H, Neuberger M. Carbon monoxide uptake and the resulting carboxyhemoglobin in man. Eur J Appl Physiol. 1984;53(2):186–90.
Tikuisis P, Buick F, Kane DM. Percent carboxyhemoglobin in resting humans exposed repeatedly to 1,500 and 7,500 ppm CO. J Appl Physiol. 1987;63(2):820–7.
Bunnell DE, Horvath SM. Interactive effects of physical work and carbon monoxide on cognitive task performance. Aviat Space Environ Med. 1988;59(12):1133–8.
Bunnell DE, Horvath SM. Interactive effects of heat, physical work, and CO exposure on metabolism and cognitive task performance. Aviat Space Environ Med. 1989;60(5):428–32.
Hudnell HK, Benignus VA. Carbon monoxide exposure and human visual detection thresholds. Neurotoxicol Teratol. 1989;11(4):363–71.
Adir Y, Merdler A, Ben Haim S, Front A, Harduf R, Bitterman H. Effects of exposure to low concentrations of carbon monoxide on exercise performance and myocardial perfusion in young healthy men. Occup Environ Med. 1999;56(8):535–8.
Tikuisis P, Kane DM, McLellan TM, Buick F, Fairburn SM. Rate of formation of carboxyhemoglobin in exercising humans exposed to carbon monoxide. J Appl Physiol. 1992;72(4):1311–9.
Benignus VA, Hazucha MJ, Smith MV, Bromberg PA. Prediction of carboxyhemoglobin formation due to transient exposure to carbon monoxide. J Appl Physiol. 1994;76(4):1739–45.
Amitai Y, Zlotogorski Z, Golan-Katzav V, Wexler A, Gross D. Neuropsychological impairment from acute low-level exposure to carbon monoxide. Arch Neurol. 1998;55(6):845–8.
Kizakevich PN, McCartney ML, Hazucha MJ, Sleet LH, Jochem WJ, Hackney AC, Bolick K. Noninvasive ambulatory assessment of cardiac function in healthy men exposed to carbon monoxide during upper and lower body exercise. Eur J Appl Physiol. 2000;83(1):7–16. https://doi.org/10.1007/s004210000256.
Ren X, Dorrington KL, Robbins PA. Respiratory control in humans after 8 h of lowered arterial PO2, hemodilution, or carboxyhemoglobinemia. J Appl Physiol. 2001;90(4):1189–95.
Vesely AE, Somogyi RB, Sasano H, Sasano N, Fisher JA, Duffin J. The effects of carbon monoxide on respiratory chemoreflexes in humans. Environ Res. 2004;94(3):227–33. https://doi.org/10.1016/s0013-9351(03)00107-5.
Thomassen O, Brattebo G, Rostrup M. Carbon monoxide poisoning while using a small cooking stove in a tent. Am J Emerg Med 2004, 22(3):204-206. doi: S0735675704000476.
Mayr FB, Spiel A, Leitner J, Marsik C, Germann P, Ullrich R, Wagner O, Jilma B. Effects of carbon monoxide inhalation during experimental endotoxemia in humans. Am J Respir Crit Care Med. 2005;171(4):354–60.
Resch H, Zawinka C, Weigert G, Schmetterer L, Garhofer G. Inhaled carbon monoxide increases retinal and choroidal blood flow in healthy humans. Invest Ophthalmol Vis Sci. 2005;46(11):4275–80. https://doi.org/10.1167/iovs.05-0417.
Morse CI, Pritchard LJ, Wust RC, Jones DA, Degens H. Carbon monoxide inhalation reduces skeletal muscle fatigue resistance. Acta Physiol (Oxf). 2008;192(3):397–401. https://doi.org/10.1111/j.1748-1716.2007.01757.x.
Ayres SM, Mueller HS, Gregory JJ, Giannelli S Jr, Penny JL. Systemic and myocardial hemodynamic responses to relatively small concentrations of carboxyhemoglobin (COHB). Arch Environ Health. 1969;18(4):699–709.
Ayres SM, Giannelli S Jr, Mueller H. Myocardial and systemic responses to carboxyhemoglobin. Ann N Y Acad Sci. 1970;174(1):268–93.
Aronow WS, Harris CN, Isbell MW, Rokaw SN, Imparato B. Effect of freeway travel on angina pectoris. Ann Intern Med. 1972;77(5):669–76.
Anderson EW, Andelman RJ, Strauch JM, Fortuin NJ, Knelson JH. Effect of low-level carbon monoxide exposure on onset and duration of angina pectoris. A study in ten patients with ischemic heart disease. Ann Intern Med. 1973;79(1):46–50.
Aronow WS, Isbell MW. Carbon monoxide effect on exercise-induced angina pectoris. Ann Intern Med. 1973;79(3):392.
Aronow WS, Stemmer EA, Isbell MW. Effect of carbon monoxide exposure on intermittent claudication. Circulation. 1974;49(3):415–7.
Aronow WS, Charter R, Seacat G. Effect of 4% carboxyhemoglobin on human performance in cardiac patients. Prev Med. 1979;8(5):562–6.
Aronow WS. Aggravation of angina pectoris by two percent carboxyhemoglobin. Am Heart J. 1981;101(2):154–7.
Sheps DS, Adams KF Jr, Bromberg PA, Goldstein GM, O'Neil JJ, Horstman D, Koch G. Lack of effect of low levels of carboxyhemoglobin on cardiovascular function in patients with ischemic heart disease. Arch Environ Health. 1987;42(2):108–16. https://doi.org/10.1080/00039896.1987.9935805.
Adams KF, Koch G, Chatterjee B, Goldstein GM, O'Neil JJ, Bromberg PA, Sheps DS. Acute elevation of blood carboxyhemoglobin to 6% impairs exercise performance and aggravates symptoms in patients with ischemic heart disease. J Am Coll Cardiol. 1988;12(4):900–9. https://doi.org/10.1016/0735-1097(88)90452-4.
Allred EN, Bleecker ER, Chaitman BR, Dahms TE, Gottlieb SO, Hackney JD, Hayes D, Pagano M, Selvester RH, Walden SM. Acute effects of carbon monoxide exposure on individuals with coronary artery disease. Res Rep Health Eff Inst. 1989;25:1–79.
Hinderliter AL, Adams KF Jr, Price CJ, Herbst MC, Koch G, Sheps DS. Effects of low-level carbon monoxide exposure on resting and exercise-induced ventricular arrhythmias in patients with coronary artery disease and no baseline ectopy. Arch Environ Health. 1989;44(2):89–93. https://doi.org/10.1080/00039896.1989.9934381.
Kleinman MT, Davidson DM, Vandagriff RB, Caiozzo VJ, Whittenberger JL. Effects of short-term exposure to carbon monoxide in subjects with coronary artery disease. Arch Environ Health. 1989;44(6):361–9. https://doi.org/10.1080/00039896.1989.9935908.
Sheps DS, Herbst MC, Hinderliter AL, Adams KF, Ekelund LG, O'Neil JJ, Goldstein GM, Bromberg PA, Dalton JL, Ballenger MN, et al. Production of arrhythmias by elevated carboxyhemoglobin in patients with coronary artery disease. Ann Intern Med. 1990;113(5):343–51.
Sheps DS, Herbst MC, Hinderliter AL, Adams KF, Ekelund LG, O'Neil JJ, Goldstein GM, Bromberg PA, Ballenger M, Davis SM, et al. Effects of 4 percent and 6 percent carboxyhemoglobin on arrhythmia production in patients with coronary artery disease. Res Rep Health Eff Inst. 1991;41:1–46. discussion 47-58
Allred EN, Bleecker ER, Chaitman BR, Dahms TE, Gottlieb SO, Hackney JD, Pagano M, Selvester RH, Walden SM, Warren J. Effects of carbon monoxide on myocardial ischemia. Environ Health Perspect. 1991;91:89–132.
Chaitman BR, Dahms TE, Byers S, Carroll LW, Younis LT, Wiens RD. Carbon monoxide exposure of subjects with documented cardiac arrhythmias. Res Rep Health Eff Inst. 1992;(52):1, 26. discussion 27-37
Dahms TE, Younis LT, Wiens RD, Zarnegar S, Byers SL, Chaitman BR. Effects of carbon monoxide exposure in patients with documented cardiac arrhythmias, J am Coll Cardiol. 1993;21(2):442–50. 0735-1097(93)90687-V.
Leaf DA, Kleinman MT. Urban ectopy in the mountains: carbon monoxide exposure at high altitude. Arch Environ Health. 1996;51(4):283–90.
Kleinman MT, Leaf DA, Kelly E, Caiozzo V, Osann K, O'Niell T. Urban angina in the mountains: effects of carbon monoxide and mild hypoxemia on subjects with chronic stable angina. Arch Environ Health. 1998;53(6):388–97. https://doi.org/10.1080/00039899809605726.
Aronow WS, Ferlinz J, Glauser F. Effect of carbon monoxide on exercise performance in chronic obstructive pulmonary disease. Am J Med. 1977;63(6):904–8.
Aronow WS, Schlueter WJ, Williams MA, Petratis M, Sketch MH. Aggravation of exercise performance in patients with anemia by 3% carboxyhemoglobin. Environ Res. 1984;35(2):394–8.
Harbin TJ, Benignus VA, Muller KE, Barton CN. The effects of low-level carbon monoxide exposure upon evoked cortical potentials in young and elderly men. Neurotoxicol Teratol. 1988;10(2):93–100. doi: 0892-0362(88)90072-4.
U.S. Environmental Protection Agency. Integrated science assessment for carbon monoxide. Final report. Washington, DC: EPA; 2010. http://cfpub.epa.gov/ncea/cfm/recordisplay.cfm?deid=218686.
Coburn RF. Carbon monoxide uptake and excretion: testing assumptions made in deriving the Coburn-Forster-Kane equation. Respir Physiol Neurobiol. 2013;187(3):224–33. https://doi.org/10.1016/j.resp.2013.04.006.
Benignus VA, Coleman TG. Simulations of exercise and brain effects of acute exposure to carbon monoxide in normal and vascular-diseased persons. Inhal Toxicol. 2010;22(5):417–26. https://doi.org/10.3109/08958370903576806.
U.S. Environmental Protection Agency. Quantitative risk and exposure assessment for carbon monoxide - amended. Research Triangle Park, NC: EPA; 2010. https://www3.epa.gov/ttn/naaqs/standards/co/data/CO-REA-Amended-July2010.pdf.
Franck U, Leitte AM, Suppan P. Multifactorial airborne exposures and respiratory hospital admissions--the example of Santiago de Chile. Sci Total Environ. 2015;502:114–21. https://doi.org/10.1016/j.scitotenv.2014.08.093.
Arbex MA, de Souza Conceicao GM, Cendon SP, Arbex FF, Lopes AC, Moyses EP, Santiago SL, Saldiva PH, Pereira LA, Braga AL. Urban air pollution and chronic obstructive pulmonary disease-related emergency department visits. J Epidemiol Community Health. 2009;63(10):777–83. https://doi.org/10.1136/jech.2008.078360.
Yallop D, Duncan ER, Norris E, Fuller GW, Thomas N, Walters J, Dick MC, Height SE, Thein SL, Rees DC. The associations between air quality and the number of hospital admissions for acute pain and sickle-cell disease in an urban environment. Br J Haematol. 2007;136(6):844–8. https://doi.org/10.1111/j.1365-2141.2007.06493.x.
Mekontso Dessap A, Contou D, Dandine-Roulland C, Hemery F, Habibi A, Charles-Nelson A, Galacteros F, Brun-Buisson C, Maitre B, Katsahian S. Environmental influences on daily emergency admissions in sickle-cell disease patients. Medicine (Baltimore). 2014;93(29):e280. https://doi.org/10.1097/md.0000000000000280.
Bathoorn E, Slebos DJ, Postma DS, Koeter GH, van Oosterhout AJ, van der Toorn M, Boezen HM, Kerstjens HA. Anti-inflammatory effects of inhaled carbon monoxide in patients with COPD: a pilot study. Eur Respir J. 2007;30(6):1131–7. https://doi.org/10.1183/09031936.00163206.
Tian LW, Ho KF, Wang T, Qiu H, Pun VC, Chan CS, Louie PKK, Yu ITS. Ambient carbon monoxide and the risk of hospitalization due to chronic obstructive pulmonary disease. Am J Epidemiol. 2014;180(12):1159–67. https://doi.org/10.1093/aje/kwu248.
Camiciottoli G, Bigazzi F, Magni C, Bonti V, Diciotti S, Bartolucci M, Mascalchi M, Pistolesi M. Prevalence of comorbidities according to predominant phenotype and severity of chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2016;11:2229–36. https://doi.org/10.2147/copd.s111724
Similowski T, Agustí A, MacNee W, Schönhofer B. The potential impact of anaemia of chronic disease in COPD. Eur Respir J. 2006;27(2):390–6. https://doi.org/10.1183/09031936.06.00143704.
Wheeler-Martin K, Soghoian S, Prosser JM, Manini AF, Marker E, Stajic M, Prezant D, Nelson LS, Hoffman RS. Impact of mandatory carbon monoxide alarms: an investigation of the effects on detection and poisoning rates in new York City. Am J Public Health. 2015;105(8):1623–9. https://doi.org/10.2105/AJPH.2015.302577.
Lavonas E, Kerns W, Tomaszewski C, Blackwell T, Galaska P, Hay T, McCormick G, Brown A, Mott J. Use of carbon monoxide alarms to prevent poisonings during a power outage--North Carolina, December 2002. MMWR Morb Mortal Wkly Rep. 2004;53(9):189–92.
McDonald EM, Gielen AC, Shields WC, Stepnitz R, Parker E, Ma X, Bishai D. Residential carbon monoxide (CO) poisoning risks: correlates of observed CO alarm use in urban households. J Environ Health. 2013;76(3):26–32.
Vogel JA, Gleser MA. Effect of carbon monoxide on oxygen transport during exercise. J Appl Physiol. 1972;32(2):234–9.
Kane LA, Ryan BJ, Schmidt W, Byrnes WC. Acute, low-dose CO inhalation does not Alter energy expenditure during submaximal exercise. Int J Sports Med. 2016;37(1):19–24. https://doi.org/10.1055/s-0035-1554641.
Zavorsky GS, Smoliga JM, Longo LD, Uhranowsky KA, Cadman CR, Duffin J, Fisher JA. Increased carbon monoxide clearance during exercise in humans. Med Sci Sport Exer. 2012;44(11):2118–24. https://doi.org/10.1249/MSS.0b013e3182602a00.
Acknowledgments
We would like to thank Michele Wiens (National Collaborating Centre for Environmental Health) for leading our literature search, as well as Erna van Balen (previously with National Collaborating Centre for Environmental Health) for helping us with the initial stages of the review.
Availability of data and supporting material sections
Data sharing not applicable to this article as no datasets were generated for this review.
Funding
This work was funded by the Water, Air, and Climate Change Bureau, Health Canada (contract number 4500325958).
Author information
Authors and Affiliations
Contributions
All authors conceived of the paper and contributed to its development and writing, and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Barn, P., Giles, L., Héroux, ME. et al. A review of the experimental evidence on the toxicokinetics of carbon monoxide: the potential role of pathophysiology among susceptible groups. Environ Health 17, 13 (2018). https://doi.org/10.1186/s12940-018-0357-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12940-018-0357-2