Abstract
Background
Vaginal candidiasis is frequent among pregnant women and it is treated with anti-fungal medication (conazoles). Conazoles have anti-androgenic properties and prenatal exposure in rodents is associated with a shorter (less masculine) anogenital distance (AGD) in male offspring. To our knowledge this has never been studied in humans.
Method
In the Odense Child Cohort pregnant women residing in Odense municipality, Denmark, were recruited at gestational age 8–16 weeks between 2010 and 2012. Of the eligible 2421 mother-child pairs, 812 mother-son pairs were included. Questionnaire data on medicine use were collected in first and third trimester and physical examination at age 3 month was performed.
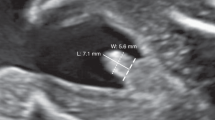
Ano-scrotal distance; measured from the centre of anus to the posterior base of scrotum (AGDas). Ano-cephalad distance; measured from the centre of anus to the cephalad insertion of the penis (AGDap) and penile width; measured at the base of the penis.
Results
Eighty seven women had used antifungal medicine during pregnancy. Maternal use of oral fluconazole (n = 4) was associated with a 6.4 mm shorter AGDas (95% CI: -11.9;-0.9) in the male offspring. Use of antifungal vaginal tablets (n = 21), was associated with a non-significantly shorter AGDas (−1.9 mm; 95% CI: -4.3; 0.5) whereas exposure to vaginal cream (n = 23) was not associated to AGDas. Use of antifungal medicine in the window of genital development between 8 and 14 weeks of gestation was associated with a larger reduction in AGDas than exposure outside this window. Antifungal medicine intake was not associated with AGDap and penil width.
Conclusion
Our preliminary findings prompted us to hypothesize that maternal use of conazole antifungal medication during pregnancy may affect the masculinization of male offspring. If confirmed, pregnant women should be advised to use antifungal medicine with caution.
Similar content being viewed by others
Background
In pregnancy, the prevalence of vaginal candidiasis is increased compared to those not pregnant [1]. Treatment is antifungal compounds administered locally or systemically depending on the severity of symptoms [2]. In Denmark, antifungal vaginal tablets and antifungal vaginal cream with either the active ingredients miconazole or clotrimazole (both imidiazoles) are recommended as first treatment for vaginal candidiasis. Oral fluconazole (triazole) is only recommended for severe cases when the woman is pregnant [3,4,5,6,7,8,9]. Imidazole and triazole compounds are anti-mycotic through inhibition of a specific cytochrome P450 enzyme (CYP51) involved in fungal cell wall synthesis, [10, 11] but they are also known inhibitors of a range of other CYP enzymes including those involved in androgen biosynthesis [11, 12]. Accordingly, anti-androgenic properties have been demonstrated for several conazole fungicides [12, 13].
In pregnancy, hormonal changes increase the risk of vaginal candidiasis, [1, 14, 15] and as the fetus is particularly vulnerable to endocrine disruption, use of anti-fungal medication might affect development of the genitalia [16,17,18]. A recent Danish study among 1,405,663 pregnant women found an association between use of oral fluconazole during pregnancy and miscarriage [19]. Case reports have linked high-dose, long-term treatment with oral fluconazole during pregnancy to a pattern of skeletal and craniofacial birth defects seen in the offspring. This has raised concern regarding the safety of oral fluconazole use during pregnancy [20,21,22,23]. Other studies have examined the association between maternal use of antifungal medicine and malformations in the offspring, but no consistent associations have been found [14, 24, 25]. Subtle signs of anti-androgen action have not been studied in children whose mothers used anti-fungal medication during pregnancy.
Anogenital distance (AGD: distance from anus to genitals) is routinely used in animal toxicology studies and is a sensitive test of exposure of the male fetus to anti-androgenic agents [26,27,28]. In rodents, AGD has been shown to reflect the amount of androgen to which a male fetus is exposed in early development: in utero exposure to lower levels of androgens results in a shorter AGD, which is one marker of de-masculinisation [26, 28]. A vulnerable fetal masculinisation programming window (MPW) has been identified in rodent models in which androgens must act to masculinise the components of the reproductive tract and to allow the later complete development. This MPW has been identified in human to occur between gestation weeks 8–14 [29].
To our knowledge, no human studies have examined the association between maternal exposure to antifungal medicine and AGD in the male offspring. We therefore prospectively investigated the association between systemic or local use of antifungal medicine during pregnancy and the subsequent AGD and penile width in the male offspring at 3 months of age in the Odense Child Cohort (OCC) study.
Methods
Newly pregnant women at gestational age 8–16 weeks residing in Odense Municipality, Denmark, between 2010 and 2012 were recruited: at a voluntary information meeting about ultrasound examinations; at their first antenatal midwife visit; or at their ultrasound examination at Odense University Hospital. All of the pregnant women in the study completed two questionnaires, one during the first and one during the third trimester [30]. Serum samples were collected twice and urine samples once during pregnancy and stored in freezers at the Odense Patient data Explorative Network (OPEN) [30]. The study was carried out in accordance with the Helsinki Declaration II and was approved by the Regional Scientific Ethical Committees for Southern Denmark (S-20090130).
Of the eligible population of 6707 pregnant women, 4017 women were informed about the study and 2421 live born singletons with birth register data participated in the study and are currently being followed up. Participants were better educated (high school +1 year or more) and more often of Danish origin than non-participants [30].
In the questionnaire administered during the first trimester, participants were asked whether they had taken any topical or systemic medications (both prescription and over the counter) and if so to provide the name, dose and gestational week/s of use of each named medication. In the second questionnaire (administered during the third trimester) the women were asked to state whether they had experienced specific diseases or symptoms (including vaginal candidiasis) during the last 3 months of pregnancy. Furthermore, the women were asked to state whether they had ever used any type of medication during their entire pregnancy. They were asked to note names of medication, doses, total number of days of use and in which gestational week(s) it was used.
The answers from both questionnaires were categorised into: overall use of any type of antifungal medicine during pregnancy; use of fluconazole oral tablets; use of antifungal vaginal tablets (including antifungal vaginal cream if used in combination with vaginal tablets); use of antifungal vaginal cream only; and unspecific use of antifungal medicine (women who had not specifically noted which type of antifungal medicine they had used). In addition, we categorised use of antifungal oral and vaginal tablets into exposure in and outside the MPW (gestation weeks 8–14).
Three months after the expected date of birth, regardless of actual gestational age at birth, the children were invited for a clinical examination, which included measurements of length, weight and AGD. The two measurements of AGD, and the measurement of penile width were made using a Vernier caliper, which is the recommended instrument for AGD measurement [31]. The shorter AGD measurement was measured from the centre of anus to the posterior base of scrotum (AGDas) and the longer from the centre of anus to the cephalad insertion of the penis (AGDap). Penile width was measured at the base of the penis. All of these measurements were made three times and the arithmetic mean was calculated. Expert-trained technicians performed the examinations [30]. 13 boys had AGD measured by two examiners. The coefficient of variation (CV) was 3% for all the triplicate AGD measurements. Inter-examiner CV was respectively 4%, 3% and 4% for AGDas, AGDap and penile width indicating a high degree of consistency.
Statistical analysis
Use of antifungal medicine during pregnancy was categorized into: no use (reference group); fluconazole oral tablets; vaginal tablets; vaginal cream; and use of antifungal medicine of unspecified type. Differences in distributions of use of antifungal medicine according to population characteristics were assessed by chi-square.
Univariate associations between use of antifungal medicine during pregnancy, and AGD and penile width at 3-months of age, were examined. Multiple linear regressions were then used to adjust for potential confounding factors. AGD values vary with age and weight of the child, and because the clinical examination was scheduled to take place three months after expected date of birth we constructed a measure of ‘post-conceptional age’ defined as the sum of gestational age at birth (in days) and the age of the child at the AGD measurements (in days). Multiple regression analyses were thus adjusted for the post-conceptional age and individual weight-for-age standard deviation score (Z-score) [32]. We examined several potential confounding factors including maternal age, maternal body mass index, ethnicity, smoking, alcohol consumption as well as parity, socioeconomic status, gestational age at the 3-month examination and birth weight. None of these factors changed the estimated beta-coefficient more than 10% and were therefore excluded from the final models.
We evaluated the fit of the regression models by testing the residuals for normality and by inspecting the residual plots. All statistical analyses were conducted in STATA13. P-values were considered significant when they were <0.05, and 95% confidence intervals were calculated.
Results
A total of 2421 live born singletons with birth registry data were included in the original OCC dataset. After the initial exclusions, as shown in Fig. 1, the final dataset consisted of 812 mother-son pairs with measurements at 3 months of whom there were 795 AGDap measurements, 810 AGDas measurements and 802 measurements of penile width.
Pregnant women using anti-fungal medicine were more often of non-European origin and had a shorter gestational age, but there were no differences in age, parity, smoking habit, alcohol intake, BMI or birth weight (Table 1).
Of the overall study population of 812 mother-son pairs, 87 (11%) women had used antifungal medicine during pregnancy (Table 1) of whom 4 women had been treated with oral tablets containing fluconazole (a single dose of 150 mg) within the MPW. In addition, 21 women had used vaginal tablets containing 500 mg to 1200 mg miconazole or clotrimazole of whom 11 had used them in the MPW. Furthermore, of the 21 women who had used vaginal tablets, 11 had used only antifungal vaginal tablets and the other 10 had used them in combination with antifungal vaginal cream. There were 23 women who had only used antifungal vaginal cream (active ingredients miconazole or clotrimazole) and 39 women had used antifungal medicine but did not specify type (Table 2 and Additional file 1).
After adjustment for weight-adjusted z-score and post-conceptional age, boys prenatally exposed to oral fluconazole had a significantly shorter AGDas (−6.4 mm; 95% CI: -11.9; −0.9) at their 3-month examination compared to unexposed boys (Table 2, Figs. 2 and 3). In addition, maternal use of antifungal vaginal tablets containing miconazole or clotrimazole was marginally associated with a shorter AGDas (−1.9 mm; 95% CI: -4.3; 0.5). Boys exposed to vaginal tablets containing either miconazole or clotrimazole in the MPW had shorter AGDas than those exposed outside the MPW (Table 2). When dividing use of vaginal tablets into only use of vaginal tablets and vaginal tablet use in combination with cream, boys prenatally exposed to only vaginal tablets had shorter AGDas than those prenatally exposed to a combination (Table 2).
Column scatterplot of AGDas in mm among boys not prenatally exposed to antifungal medicine (green dots), boys prenatally exposed to antifungal vaginal tablets outside the MPW (red dots), boys prenatally exposed to antifungal vaginal tablets in the MPW (blue dots), and boys prenatally exposed to oral fluconazole (purple dots)
An association was found between unspecific antifungal medicine use and penile width (−0.5 mm; 95%CI: -0.9; −0.1) but no association was seen for penile width and other exposure groups (see Additional file 1). No association was found between prenatal exposure to any antifungal medicine and AGDap.
Discussion
Four pregnant women taking fluconazole orally gave birth to boys with a significantly shorter AGDas (−6.4 mm) than unexposed boys. In addition, maternal use of antifungal vaginal tablets containing miconazole or clotrimazole was associated with a shorter AGDas, although not significantly, whereas use of the same compounds in the form of vaginal creams did not affect AGDas. AGDap and penile width were not affected apart from a shorter penile width among boys to mothers with unspecific use, which was probably due to chance. Interestingly, use of antifungal medicine in the window of genital development between 8 and 14 weeks of gestation was associated with a larger reduction in AGDas than exposure outside of this window. This is in accordance with the sensitivity of this window to the effects of prenatal anti-androgen exposure in rodent studies [27]. We acknowledge that our rather preliminary findings are based on four cases, but they are biologically plausible and of public health importance as up to 20% of pregnant women experience vaginal candidiasis. In addition, a 6.4 mm shorter AGD corresponds to a 20% decrease and may be of clinical importance as it has been associated with abnormal adult male reproduction [33, 34].
This is to our knowledge the first human study to examine the association between maternal exposure to antifungal medicine and AGD in the offspring. Our findings are biologically plausible, as conazole antifungals have known anti-androgenic properties, [12] and exposure to chemicals with anti-androgenic action (e.g. phthalates) have been associated with shorter AGD in several human studies [32, 35,36,37,38]. Rodent studies have shown that an impairment of androgen action within the MPW can result abnormal development and function of reproductive organs [27]. Hence, exposure to anti-androgenic chemicals, including conazole antifungals, during the MPW have resulted in hypospadias, cryptorchidism and shortened AGD in rodent studies [26, 27].
Two large registry-based Danish studies found no association between oral intake of fluconazole during the first trimester and 15 different birth defects in the offspring [24, 25], however, they did not measure AGD. Similar findings have been reported in other smaller studies [14, 15, 24], which also studied hypospadias, but none of the studies measured AGD, which may be a more sensitive marker of prenatal exposure to anti-androgens [32].
The association between maternal use of antifungal vaginal tablets and AGD was weaker than among boys exposed to oral treatment. This may be due to less potent anti-androgenic action of miconazole and clotrimazole and/or lower exposure from vaginal tablets. The same reasoning may be used for the lack of effect of vaginal cream exposure on AGDas, as exposure levels from creams, is expected to be even lower. Miconazole in vaginal tablets have been demonstrated to be absorbed systemically [39]. Women using vaginal tablets without combination with antifungal vaginal cream typically used tablets containing higher doses of miconazole or clotrimazole than women who used both tablets and cream. Thus, the fetus may be exposed to a higher dose after use of vaginal tablets alone compared to the combined treatment of vaginal tables and cream which was seen by a shorter ADGas in this group.
Participation rate was 43% [30] and only 11% of the women reported use of antifungal medicine, which is lower than the estimated 20% of all pregnant women suffering vaginal candidiasis [14, 15]. This could be due to the fact that our study population was higher educated and therefore more aware of the importance of avoiding medication use during pregnancy. Information about use of antifungal medicine was self-reported which might have led to misclassification. This is, however, not likely to be associated with AGD as the women were unaware of this measure when answering the questionnaires leading to an underestimation of the association.
AGD measurements has acceptable intra- and inter-examiner reliability, but with large inter-individual variation in measurements especially in AGDap measured from the anus to the top of the cephalad insertion of the penis. AGDap is therefore more dependent on the size of the child, introducing a higher inaccuracy of the measurement. Also, penile width is small and thus the same absolute measurement error is of relatively larger importance. Confounding by indication may explain our findings, as the overgrowth of Candida albicans organism may be associated with a reduction in AGD, rather than the use of antifungal medication. We adjusted for relevant confounders but we cannot exclude the possibility of residual confounding from for example co-exposure to other environmental chemicals, lifestyle or health behavior.
In male rodents, the shortened AGD persists into adulthood confirming that interference of androgenic activity permanently alters the reproductive tissues [29]. In cross-sectional studies among adult men, AGD has been shown to have a significant positive association with sperm count [34]. In fact, AGD is now considered part of the spectrum of male intrauterine testicular disruption called the testicular dysgenesis syndrome (TDS) [18]. Therefore, the observed reduction in AGD may have potential long-term consequences for male reproductive health.
Conclusion
Based on our findings that four pregnant women taking fluconazole orally gave birth to boys with a significantly shorter AGD we hypothesize that maternal use of antifungal medication may cause anti-androgenic effects. Further studies on maternal antifungal use during pregnancy are needed. In the interim, pregnant women should be advised to use antifungal medicine with caution.
Abbreviations
- AGDap:
-
Anogenital distance measured from the centre of anus to the cephalic insertion of the penis
- AGDas:
-
Anogenital distance measured from the centre of anus to the posterior base of scrotum
- MPW:
-
Masculinization programming window
- OCC:
-
Odense child cohort
- TDS:
-
Testicular dysgenesis syndrome
References
Sobel JD. Vulvovaginal candidosis. Lancet. 2007;369(9577):1961–71. doi:10.1016/S0140-6736(07)60917-9.
Soong D, Einarson A. Vaginal yeast infections during pregnancy. Canadian family physician Medecin de famille canadien. 2009;55(3):255–6. Epub 2009/03/14. PubMed PMID: 19282531; PubMed Central PMCID: PMCPMC2654841
Dansk LI. Fluconazol Pro medicin: Pro.medine.dk; 2014 [cited 2015 03–02]. Available from: http://pro.medicin.dk/Medicin/Praeparater/3095.
Dansk LI. Brentan Pro medicine: Pro.medicin.dk; 2014 [cited 2015 03–02]. Available from: http://pro.medicin.dk/Medicin/Praeparater/4269.
Dansk LI. Brentacore Pro medicin: Pro.medicin.dk; 2014 [cited 2015 03–02]. Available from: http://pro.medicin.dk/Medicin/Praeparater/355.
Dansk LI. Canesten Pro Medicin: Pro.medicin.dk; 2014 [cited 2015 03–02]. Available from: http://pro.medicin.dk/Medicin/Praeparater/3718.
Dansk LI. Diflucan Pro Medicin: Pro.medicin.dk; 2014 [cited 2015 03–02]. Available from: http://pro.medicin.dk/Medicin/Praeparater/1209.
Dansk LI. Canvag, vaginaltabletter og creme 100 mg+10 mg-g.doc Produktresume.dk Lægemiddelstyrrelsen; 2014 [cited 2015 03–02]. Available from: http://www.produktresume.dk/docushare/dsweb/ApplySimpleSearch.
Cottreau JM, Barr VO. A review of antiviral and antifungal use and safety during pregnancy. Pharmacotherapy 2016;36(6):668-678. Epub 2016/05/04. doi: 10.1002/phar.1764. PubMed.
Como JA, Dismukes WE. Oral azole drugs as systemic antifungal therapy. N Engl J Med 1994; 330(4):263-272. Epub 1994/01/27. doi:10.1056/nejm199401273300407. PubMed.
Zarn JA, Bruschweiler BJ, Schlatter JR. Azole fungicides affect mammalian steroidogenesis by inhibiting sterol 14 alpha-demethylase and aromatase. Environ Health Perspect. 2003;111(3):255–61. Epub 2003/03/04. PubMed PMID: 12611652; PubMed Central PMCID: PMCPMC1241380.
Kjaerstad MB, Taxvig C, Nellemann C, Vinggaard AM, Andersen HR. Endocrine disrupting effects in vitro of conazole antifungals used as pesticides and pharmaceuticals. Reproductive toxicology (Elmsford, NY). 2010;30(4):573–82. Epub 2010/08/17 doi:10.1016/j.reprotox.2010.07.009. PubMed
Loose DS, Kan PB, Hirst MA, Marcus RA, Feldman D. Ketoconazole blocks adrenal steroidogenesis by inhibiting cytochrome P450-dependent enzymes. J Clin Invest. 1983;71(5):1495–9. Epub 1983/05/01. PubMed PMID: 6304148; PubMed Central PMCID: PMCPmc437014
Carter TC, Druschel CM, Romitti PA, Bell EM, Werler MM, Mitchell AA. Antifungal drugs and the risk of selected birth defects. Am J Obstet Gynecol. 2008;198(2):191–e1-7. Epub 2008/01/30 doi:10.1016/j.ajog.2007.08.044. PubMed
Pilmis B, Jullien V, Sobel J, Lecuit M, Lortholary O, Charlier C. Antifungal drugs during pregnancy: an updated review. J Antimicrob Chemother 2015; 70(1):14-22. Epub 2014/09/11. doi:10.1093/jac/dku355. PubMed.
Diamanti-Kandarakis E, Bourguignon JP, Giudice LC, Hauser R, Prins GS, Soto AM, et al. Endocrine-disrupting chemicals: an Endocrine Society scientific statement. Endocr Rev. 2009;30(4):293–342. Epub 2009/06/09. doi:10.1210/er.2009-0002. PubMed PMID: 19502515; PubMed Central PMCID: PMCPMC2726844
Schug TT, Janesick A, Blumberg B, Heindel JJ. Endocrine disrupting chemicals and disease susceptibility. J Steroid Biochem Mol Biol. 2011;127(3–5):204–15. Epub 2011/09/09. doi:10.1016/j.jsbmb.2011.08.007. PubMed PMID: 21899826; PubMed Central PMCID: PMCPMC3220783
Skakkebaek NE, Rajpert-De Meyts E, Buck Louis GM, Toppari J, Andersson AM, Eisenberg ML, et al. Male reproductive disorders and fertility trends: influences of environment and genetic susceptibility. Physiol Rev 2016;96(1):55-97. Epub 2015/11/20. doi:10.1152/physrev.00017.2015. PubMed.
Molgaard-Nielsen D, Svanstrom H, Melbye M, Hviid A, Pasternak B. Association between use of oral Fluconazole during pregnancy and risk of spontaneous abortion and stillbirth. JAMA 2016; 315(1):58-67. Epub 2016/01/10. doi:10.1001/jama.2015.17844. PubMed.
Aleck KA, Bartley DL. Multiple malformation syndrome following fluconazole use in pregnancy: report of an additional patient. Am J Med Genet. 1997;72(3):253–6. Epub 1997/10/23 22:26. PubMed
Lee BE, Feinberg M, Abraham JJ, Murthy AR. Congenital malformations in an infant born to a woman treated with fluconazole. Pediatr Infect Dis J 1992; 11(12):1062-1064. Epub 1992/12/01. PubMed.
Lopez-Rangel E, Van Allen MI. Prenatal exposure to fluconazole: an identifiable dysmorphic phenotype . Birth Defects Res Part A Clin Mol Teratol 2005; 73(11):919-923. Epub 2005/11/03. doi:10.1002/bdra.20189. PubMed.
Pursley TJ, Blomquist IK, Abraham J, Andersen HF, Bartley JA. Fluconazole-induced congenital anomalies in three infants. Clin Infect Dis 1996; 22(2):336-340. Epub 1996/02/01. PubMed.
Norgaard M, Pedersen L, Gislum M, Erichsen R, Sogaard KK, Schonheyder HC, et al. Maternal use of fluconazole and risk of congenital malformations: a Danish population-based cohort study. J Antimicrob Chemother 2008; 62(1):172-176. Epub 2008/04/11. doi:10.1093/jac/dkn157. PubMed.
Molgaard-Nielsen D, Pasternak B, Hviid A. Use of oral fluconazole during pregnancy and the risk of birth defects. N Engl J Med 2013; 369(9):830-839. Epub 2013/08/30. doi:10.1056/NEJMoa1301066. PubMed.
Macleod DJ, Sharpe RM, Welsh M, Fisken M, Scott HM, Hutchison GR, et al. Androgen action in the masculinization programming window and development of male reproductive organs. Int J Androl 2010; 33(2):279-287. Epub 2009/12/17. doi:10.1111/j.1365-2605.2009.01005.x. PubMed.
Welsh M, Saunders PT, Fisken M, Scott HM, Hutchison GR, Smith LB, et al. Identification in rats of a programming window for reproductive tract masculinization, disruption of which leads to hypospadias and cryptorchidism. J Clin Invest. 2008;118(4):1479–90. Epub 2008/03/15. doi:10.1172/jci34241. PubMed PMID: 18340380; PubMed Central PMCID: PMCPMC2267017
Christiansen S, Scholze M, Dalgaard M, Vinggaard AM, Axelstad M, Kortenkamp A, et al. Synergistic disruption of external male sex organ development by a mixture of four Antiandrogens. Environ Health Perspect. 2009;117(12):1839–46. doi:10.1289/ehp.0900689. PubMed PMID: 20049201; PubMed Central PMCID: PMCPmc2799456
Welsh M, Suzuki H, Yamada G. The masculinization programming window. Endocr Dev 2014; 27:17-27. Epub 2014/09/24. doi:10.1159/000363609. PubMed.
Kyhl HB, Jensen TK, Barington T, Buhl S, Norberg LA, Jorgensen JS, et al. The Odense child cohort: aims, design, and cohort profile. Paediatr Perinat Epidemiol 2015; 29(3):250-258. Epub 2015/03/11. doi:10.1111/ppe.12183. PubMed.
Arbuckle TE, Hauser R, Swan SH, Mao CS, Longnecker MP, Main KM, et al. Meeting report: measuring endocrine-sensitive endpoints within the first years of life. Environ Health Perspect. 2008;116(7):948–51. Epub 2008/07/17. doi:10.1289/ehp.11226. PubMed PMID: 18629319; PubMed Central PMCID: PMCPMC2453165
Swan SH. Environmental phthalate exposure in relation to reproductive outcomes and other health endpoints in humans. Environ Res. 2008;108(2):177–84. Epub 2008/10/25. PubMed PMID: 18949837; PubMed Central PMCID: PMCPMC2775531
Juul A, Almstrup K, Andersson AM, Jensen TK, Jorgensen N, Main KM, et al. Possible fetal determinants of male infertility. Nat Rev Endocrinol 2014; 10(9):553-562. Epub 2014/06/18. doi:10.1038/nrendo.2014.97. PubMed.
Mendiola J, Stahlhut RW, Jorgensen N, Liu F, Swan SH. Shorter anogenital distance predicts poorer semen quality in young men in Rochester, New York. Environ Health Perspect. 2011;119(7):958–63. Epub 2011/03/08. doi:10.1289/ehp.1103421. PubMed PMID: 21377950; PubMed Central PMCID: PMCPMC3222997
Swan SH, Main KM, Liu F, Stewart SL, Kruse RL, Calafat AM, et al. Decrease in anogenital distance among male infants with prenatal phthalate exposure. Environ Health Perspect. 2005;113(8):1056–61. Epub 2005/08/05. PubMed PMID: 16079079; PubMed Central PMCID: PMCPmc1280349
Swan SH, Sathyanarayana S, Barrett ES, Janssen S, Liu F, Nguyen RH, et al. First trimester phthalate exposure and anogenital distance in newborns. Human reproduction (Oxford, England). 2015;30(4):963–72. Epub 2015/02/24. doi:10.1093/humrep/deu363. PubMed PMID: 25697839; PubMed Central PMCID: PMCPMC4359397
Martina CA, Weiss B, Swan SH. Lifestyle behaviors associated with exposures to endocrine disruptors. Neurotoxicology. 2012;33(6):1427–33. Epub 2012/06/29. doi:10.1016/j.neuro.2012.05.016. PubMed PMID: 22739065; PubMed Central PMCID: PMCPMC3641683
Bornehag CG, Carlstedt F, Jonsson BA, Lindh CH, Jensen TK, Bodin A, et al. Prenatal phthalate exposures and anogenital distance in Swedish boys. Environ Health Perspect. 2015;123(1):101–7. Epub 2014/10/30. doi:10.1289/ehp.1408163. PubMed PMID: 25353625; PubMed Central PMCID: PMCPMC4286276
Kjaerstad MB, Nielsen F, Nohr-Jensen L, Zwisler S, Brosen K, Andersen HR. Systemic uptake of miconazole during vaginal suppository use and effect on CYP1A2 and CYP3A4 associated enzyme activities in women. Eur J Clin Pharmacol 2010; 66(12):1189-97. Epub 2010/10/07. doi:10.1007/s00228-010-0906-2. PubMed.
Acknowledgements
The technicians at Hans Christian Andersen’s children’s Hospital are acknowledged for their careful examination of the children.
Funding
This work was supported by the Danish Foundation for Scientific Innovation and Technology (09–067180), The Danish Research Council (4004-00352B_FSS), Ronald McDonald Children Foundation, K. A. Rohde’s and wife’s Foundation, Odense University Hospital and Region of Southern Denmark, Municipality of Odense, The Danish Council for Strategic Research, Program Commission on Health, Food andWelfare (2101–08-0058), Odense University Hospital Research Foundation and Odense Patient data Exploratory Network (OPEN).
Availability of data and materials
The dataset supporting the conclusions of this article is available by contacting Tina Kold Jensen.
Authors’ contributions
DMM and MBP did data cleaning, performed the data analysis and interpretation and drafted the manuscript. TKJ and DVL provided assistance with data analysis and interpretation and revised and edited the manuscript. HBK was responsible for the overall data collection and revised and edited the manuscript. NES, HRA, AJ, SS, DMK and MSA assisted with interpretation and revised the manuscript. All authors read and approved the final manuscript.
Competing interests
No authors have any competing financial interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The study was carried out in accordance with the Helsinki Declaration II and was approved by the Regional Scientific Ethical Committees for Southern Denmark (S-20090130).
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Additional file
Additional file 1: Table S1.
Use of antifungal vaginal tablets (active ingredients clotrimazole or miconazole) and oral fluconazole and in relation to anogenital distance (AGDas, AGDap) and penile width measurements among 25 mother/boy pairs. Table S2. Mean (SD) penile width in mm in boys at three months according to maternal use of antifungal medicine in pregnancy. Beta values represent adjusted mean difference (95% confidence intervals, 95% CI) in penile width in boys whose mothers used antifungal medicine in pregnancy, and non-users. (DOCX 110 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Mogensen, D.M., Pihl, M.B., Skakkebæk, N.E. et al. Prenatal exposure to antifungal medication may change anogenital distance in male offspring: a preliminary study. Environ Health 16, 68 (2017). https://doi.org/10.1186/s12940-017-0263-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12940-017-0263-z