Abstract
Background
The country received malaria-free certification from WHO in September 2016, becoming only the second country in the WHO South East Asia region to be declared malaria-free. Imported malaria cases continue to be reported, with 278 cases reported between 2013 and 2017. The diagnosis of a severe Plasmodium vivax patient co-infected with HIV and tuberculosis is discussed with an overview of the rapid response mounted by the Anti Malaria Campaign (AMC), Sri Lanka.
Case presentation
A Sri Lankan gem miner who returned from Madagascar on the 6th of April 2018 presented to a private hospital for a malaria diagnostic test on the 21st April, 2 days after the onset of fever. He came on his own for this test due to the awareness he had regarding the risk of imported malaria. As the patient was positive for P. vivax malaria, he was admitted to a government hospital for further management. The patient had features of severe malaria upon admission with a systolic BP < 80 mmHg and thrombocytopaenia (38,000 cells/mm3). Treatment with IV artesunate was initiated immediately and management was carried out rapidly and efficiently by the clinicians with guidance from the staff of the AMC headquarters, which resulted in a rapid recovery of the patient. IV artesunate was followed by a course of artemether plus lumefantrine and the blood smear was negative for malaria by the 2nd day. A 14-day course of primaquine was commenced after excluding a G6PD deficiency. Due to an accidental needle stick injury of a health care worker attending on the patient was tested for HIV and subsequently tuberculosis and was found to be positive for both infections. The patient was discharged on the 1st of May with instructions for follow up visits for malaria. Management of the HIV and tuberculosis infections was attended to by the clinicians and staff of the appropriate disease control programmes (i.e. the national STD/AIDS Control Programme in Sri Lanka and the National Programme for tuberculosis control and chest diseases).
Conclusions
It is important to consider comorbid conditions and immunosuppression when a patient with a benign form of malaria presents with severe manifestations. Measures should be strengthened to prevent importation of diseases, such as malaria and AIDS through migrant workers who return from high-risk countries.
Similar content being viewed by others
Background
Sri Lanka was certified as a malaria-free country by World Health Organization in 2016. Prevention of re-introduction of malaria and maintaining zero mortality due to malaria are current objectives of Anti-Malaria Campaign (AMC), Sri Lanka. Early diagnosis and proper management of malaria infections is a key strategy in achieving these objectives. Since the last indigenous malaria case was diagnosed in Sri Lanka in October 2012, only imported malaria cases have been reported in Sri Lanka, totalling 278 cases from 2013 to 2017. In spite of severe malaria patients being reported in the country (e.g. three severe malaria cases in 2017, all due to Plasmodium falciparum), zero mortality has been maintained since 2007.
Severe malaria is most commonly caused by P. falciparum infections, but Plasmodium vivax [1,2,3,4,5,6] and Plasmodium knowlesi [7, 8] has also been increasingly reported as causing severe disease. The risk of severe P. vivax malaria is high among children and people with comorbid conditions [9]. This publication describes a severe P. vivax case in Sri Lanka in a patient with HIV and tuberculosis, illustrating the rapid response mounted in response to it, and discusses case management and challenges faced in a country that has eliminated malaria.
Case presentation
A 36 year-old Sri Lankan national and gem miner by occupation who returned to Sri Lanka from Madagascar on the 6th of April 2018, visited the AMC headquarters 4 days after his arrival for a malaria diagnostic test (Fig. 1). Even though both microscopy and the rapid diagnostic test (RDT) were negative for malaria, the attending medical officer at AMC headquarters advised him to get tested for malaria if he developed fever subsequently. The patient developed fever on the 19th of April. Remembering the advice given at AMC headquarters, he requested 2 days later a blood smear for malaria diagnosis at a private health care institute situated in his home town, a previously non-endemic area for malaria of the Western Province. The blood smear reported positive for malaria parasites (P. vivax).
As the patient had dyspnoea at the time of presentation he was resuscitated with oxygen and requested to get admitted. The patient got admitted immediately to a government hospital in the same district for management of the malaria infection. He complained of severe headache and fatigue at admission (D0). On examination the patient was afebrile (98.4 °C), had a heart rate of 116 (tachycardic), blood pressure of 80/54 mmHg (which 4 h later reduced to 74/44 mmHg) and had dyspnoea (with a respiratory rate of 28, O2 saturation was normal). He was centrally cyanosed but conscious and rational with a Glasgow coma scale at 15/15. There was no pallor, jaundice or hepatosplenomegaly. Figure 1 gives the time lines in relation to the illness of this patient.
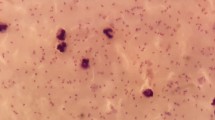
The case was reported to the Anti Malaria Campaign (AMC) telephone hotline at 2.55 pm. In spite of being a weekend, the staff members’ on-call was rapidly mobilized to attend to the patient. The diagnosis of P. vivax malaria was confirmed by examination of thick and thin Giemsa-stained blood smears by the Public Health Laboratory Technician (PHLT) of the government hospital. At admission (day 0) parasitaemia of 26,973 parasites per microlitre of blood was reported with the presence of rings, trophozoites and gametocytes. The morphology of the infected red blood cells was compatible with a P. vivax infection (Fig. 2). A RDT performed by the PHLT also gave a positive pLDH band. Results of PCR assay which was done at the Central laboratory of the AMC confirmed a mono-infection with P. vivax.
Laboratory investigations showed normal haemoglobin concentration (13.4 g/dl, reference range 11–16.5), which subsequently reduced to 9 g/dl by day 6 of admission), with a slightly elevated leukocyte count 12,120 (reference range 4000–11,000) (N 83%, L 14%), severe thrombocytopaenia (38,000 cells/mm3, reference range 150,000–400,000 cells/mm3) and a normal capillary blood sugar level of 124 mg/dl (reference range 100–200 mg/dl). There were features of acute renal failure as the serum creatinine levels increased steadily from the time of admission 1.17 mg/dl (at admission) to 1.37 mg/dl (at 2 pm the same day) to 2.27 mg/dl (at 6 pm the same day) (reference range 0.8–1.2 mg/dl) with a reduced urine output. The C Reactive protein level was elevated (73. 8 mg/l, reference range 0–3 mg/l). His liver enzymes levels were SGPT 53U/L (10-40), SGOT 59 U/l (13-31), bilirubin level 5.03 mg/dl (0.1–1.2 mg/dl). Ultra sound scan abdomen showed a mild splenomegaly (BPL 12 cm) and no hepatomegaly was detected. Blood culture was negative for microorganisms.
Following good hydration with IV normal saline and IV noradrenaline infusion for 24 h, his blood pressure stabilized and serum creatinine returned to the normal level (1.22 mg/dl) with improved urine output by the next day. For the management of malaria, the AMC medical officer on-call visited the patient with IV artesunate (2.4 mg/kg body weight) and treatment was initiated by the ward medical staff based on the national treatment guidelines under the guidance of AMC consultant, with the first dose being administered within 4.5 h of admission to the hospital and two more doses given 12 hourly apart the next day. Following this, oral artemisinin-based combination therapy (artemether–lumefantrine) was commenced and continued for 3 days. With the commencement of treatment, the parasitaemia reduced to 3137 parasites per microlitre the next day (day 1) and the blood smear was negative for parasites by day 2. A 14-day course of primaquine was initiated on the sixth day after excluding a G6PD deficiency.
Following a needle prick injury to an attending health care worker, consistent with a circular issued by the Ministry of Health, Sri Lanka, HIV screening was carried out in this patient and he was found to be positive [10]. HIV status was confirmed by ELISA which was also positive. Further confirmation of the HIV status was done by Western blot technique. Screening for tuberculosis indicated that sputum was negative for acid-fast bacilli, but the Mantoux test was strongly positive (15 cm). Due to the presence of a bluish discolouration of his nails, mild dyspnoea, persistent tachycardia with recurrent fever spikes since the 3rd day of admission (with repeat blood smears for malaria parasites being negative) and a rising CRP (130 mg/dl), a Pneumocystis carinii infection was suspected. Even though the chest X-ray was normal, the patient was started on oral cotrimoxazole (4 tablets stat and 3 tablets three times a day for 21 days). IV caftazidime was also started along with oral cotrimoxazole to cover other possible infections.
The patient was discharged from the hospital on the 1st of May with a malaria diagnosis card issued by the AMC. The especially designed card highlights the importance of completing the treatment and the indicate follow up dates to confirm the absence of malaria parasites (Fig. 3). Both the Public Health Inspector (PHI) of the patients’ area of residence and the PHI from AMC headquarters ensured that the balance primaquine was taken as required by home visits. Management of the HIV and tuberculosis infections was dealt with by the attending physicians in collaboration with the appropriate disease control programmes (i.e. the national STD/AIDS Control Programme in Sri Lanka and the National Programme for tuberculosis control and chest diseases).
The patient had left Sri Lanka for Madagascar on the 26th of December 2017, but had not taken chemoprophylaxis, but indicated that he slept under a mosquito net. The patient who is a frequent visitor to Madagascar since the year 2005, initially obtained malaria prophylaxis, but stopped taking the drugs as he would have to use the prophylactic medicines long term. He gave a past history of several episodes of malaria with the last episode being in August 2017.
Malaria case investigation and response
Case investigation which comprises both parasitological and entomological surveillance to ensure that no onward malaria transmission takes place commenced on the same day. A detailed history obtained from the patient indicated the presence of two other contacts who had returned from Madagascar with the patient. On contact tracing (a form of reactive case detection practiced in Sri Lanka), one individual had already been diagnosed with malaria in December 2017 and was being followed up by the AMC. The other person, who returned with the above patient was negative for malaria at the time. Reactive case detection by parasitological screening was carried out in 154 neighbourhood contacts of the patient according to standard surveillance guidelines and procedure of the AMC.
Entomological surveillance was conducted around the residence of the patient, but Anopheles culicifacies, the primary vector of malaria in the country was not found. However, three (0.6 per 100 dips) larvae and one adult of Anopheles subpictus, the secondary vector were detected. Larvivorous fish were introduced to the cemented pond where An. subpictus larvae was detected and a round of night fogging with insecticides was conducted to destroy any adult mosquitoes.
Public and health care workers in the vicinity were made aware of the need to be vigilant on malaria.
Discussion
This is the first case of severe P. vivax malaria with HIV and tuberculosis co-infection reported from Sri Lanka. Maintaining zero mortality due to malaria in Sri Lanka since 2007 is a noteworthy achievement considering that in most countries where imported malaria cases are diagnosed, fatalities due to imported malaria are reported. In China, between 2011 and 2015, 8653 imported P. falciparum cases were diagnosed leading to 98 deaths (11.3 per 1000 cases) [11], while in UK, of 1400 cases reported in 2015, and 1618 in 2016, six deaths were reported each year [12]. Stepien and Rosinska [13] have reported of fatalities due to imported falciparum malaria in Poland due to delay in seeking medical care and delay in diagnosis. Operation of rapid response teams, maintaining a 24-h telephone hotline, strategic distribution of antimalarial drugs to reach a patient within a few hours of diagnosis of malaria, guidance provided to the attending physicians on case management and creating awareness among health care workers and high risk groups are some of the key activities implemented by the AMC, Sri Lanka to ensure early detection and proper case management of malaria which in turn contributes to maintaining zero mortality.
Regular active case detection along with intensive awareness programmes carried out by the AMC amongst high-risk groups such as gem miners employed in African countries has made travellers aware of the need to get a blood smear examined for malaria upon arrival in Sri Lanka or if they develop fever within a year of their return. In 2017 alone, nine imported malaria cases were reported amongst Sri Lankans arriving from Madagascar. Awareness regarding mechanisms to prevent imported malaria has been further strengthened by providing informative printed material, such as airline ticket holders prior to departure (Fig. 4), and visually displaying key messages at the arrival lounge at the Bandaranaike International Airport. It is compulsory for the travellers to African countries to get vaccinated against yellow fever before their travel which is provided at the Port Health Office in Sri Lanka. The AMC works in close collaboration with staff of the Port Health Office to ensure that travellers visiting to obtain the yellow fever vaccination are referred to AMC. The AMC will then provide education, advice and guidance on the risk of malaria and preventive measures including the provision of medicines for chemoprophylaxis free of charge. These mechanisms led to this patient seeking the assistance of the AMC headquarters to get himself screened for malaria immediately after arrival on 6th of April, and again to seek a malaria diagnosis on developing fever 13 days later. This patient had not obtained chemoprophylaxis for malaria prior to departure. High-risk groups not only stay for a long duration of time but also travel between the two countries frequently. Providing prophylaxis to these long-term travellers is another challenge faced by AMC since adherence and tolerability are important aspects to be considered in long-term chemoprophylaxis. Only few studies have been reported on the use of chemoprophylaxis for more than 6 months [14].
In spite of a negative blood smear in the first instance, which could have been due to the presence of only liver stage of P. vivax at that point or undetectable levels of blood parasitaemia, the patient was vigilant enough to once again seek a diagnosis of malaria at a private health care institute when he developed fever, where malaria was promptly diagnosed. This reflects the impact of frequent training programmes carried out by AMC for the private health sector on malaria diagnosis. In the absence of evidence of locally-transmitted malaria in Sri Lanka and the patient having been in Madagascar recently it is very likely that the patient acquired malaria infection in Madagascar. Not only is P. vivax endemic in Madagascar [15], but also UNAIDS estimates that the number of people infected with HIV is rising steadily in that country [16].
The AMC mounted a rapid response in confirming the diagnosing and managing this patient. On receiving information on the 24-h telephone hotline of the AMC that a malaria positive patient was detected 40 km away from the AMC headquarters, the medical officer on call visited the patient, ensured that the diagnosis was confirmed and provided antimalarial medicines. The AMC is the sole importer and stockiest of anti-malarial medicines in the country. Due to the low incidence of imported malaria in the country and hence the very low usage of anti-malarial medicines, stocks are maintained only at the AMC and major government hospitals. For other health care institutions anti-malarial medicines are delivered to the clinicians immediately on request. This also ensures that any suspected malaria case is immediately reported to AMC headquarters whose consultants provide guidance on case management on all reported malaria cases based on the National Malaria Treatment guidelines [17]. Following treatment the patient made a full recovery of his malaria infection. Health care personnel serving around the area of residence of the patient were informed of the presence of a malaria positive patient and the need to rule out malaria in patients presenting with fever. To ensure early detection and proper case management by clinicians in the face of a very low number of malaria cases in the country, regular clinical awareness programs are carried out by the AMC and information is provided through the newsletter of the Sri Lanka Medical Association [18, 19].
This malaria infection was classified as severe based on the fact the patient had a systolic BP < 80 mmHg, acute kidney failure [20] and thrombocytopaenia (platelet count < 50,000 cells/mm3). Severe thrombocytopaenia (< 50,000 cells/mm3) has been reported as the most common “severe” manifestation among 77 studies reporting severe vivax malaria [21]. In the presence of this low platelet count (38,000 cells/mm3), should this patient not have requested a malaria diagnostic test at the private laboratory, it is very likely that dengue infection may have been the first differential diagnosis of the clinicians, and that malaria would have been overlooked, as has happened in many cases of imported malaria in the country in the past few years. This is because of an on-going dengue epidemic in the country with over 186,101 cases and 413 deaths reported in 2017 [22]. The severity of the malaria infection would have been very likely due to the concurrent HIV infection and the resulting immunocompromised state in the patient. The HIV co-infection in this patient was detected during a routine investigation for a needle stick injury to the attending health worker.
Sri Lanka has been able to prevent the re-introduction of indigenous malaria for over 5 years since October 2012 due to the many strategies it implements—awareness programs, a rapid response on detection of a malaria case, and intensive case investigation and management of patients by the AMC in addition to entomological surveillance and response. This is a noteworthy achievement given the challenges of high receptivity in a tropical country and the increased vulnerability afforded by increased foreign travel among Sri Lankans to malaria endemic countries and tourists and visitors, including foreign labour, from malaria endemic countries. The situation calls for continued vigilance to prevent the re-introduction of malaria to the country.
Conclusions
This manuscript highlights the importance of mechanisms in place to sustain malaria elimination in Sri Lanka and the key strategies followed by the Anti Malaria Campaign of Sri Lanka when a malaria case is reported. It is important to consider comorbid conditions and immunosuppression when a patient with benign forms of malaria present with severe manifestations. Measures should be strengthened to prevent importation of diseases such as malaria and AIDS through migrant workers who travel to high-risk countries.
Abbreviations
- AMC:
-
Anti Malaria Campaign
- pLDH:
-
parasite lactate dehydrogenase
- PCR:
-
polymerase chain reaction
- PHI:
-
Public Health Inspector
- PHLT:
-
Public Health Laboratory Technician
- RDT:
-
rapid diagnostic test
- WHO:
-
World Health Organization
References
Alexandre MA, Ferreira CO, Siqueira AM, Magalhaes BL, Mourao MP, Lacerda MV, et al. Severe Plasmodium vivax malaria, Brazilian Amazon. Emerg Infect Dis. 2010;16:1611–4.
Lacerda MV, Fragoso SC, Alecrim MG, Alexandre MA, Magalhaes BM, Siqueira AM, et al. Postmortem characterization of patients with clinical diagnosis of Plasmodium vivax malaria: to what extent does this parasite kill? Clin Infect Dis. 2012;55:e67–74.
Nurleila S, Syafruddin D, Elyazar IRF, Baird JK. Serious and fatal illness associated with falciparum and vivax malaria among patients admitted to hospital at West Sumba in eastern Indonesia. Am J Trop Med Hyg. 2012;87:41–9.
Baird JK. Evidence and implications of mortality associated with acute Plasmodium vivax malaria. Clin Microbiol Rev. 2013;26:36–57.
Naing C, Whittaker MA, Wai VN, Mak JW. Is Plasmodium vivax malaria a severe malaria?:a systematic review and meta-analysis. PLoS Neglect Trop Dis. 2014;8:e3071.
Im JH, Hea Kwon Y, Baek J, Park SW, Durey A, Hee Lee K, et al. Severe Plasmodium vivax infection in Korea. Malar J. 2017;16:51.
Grigg MJ, William T, Barber BE, Rajahram GS, Menon J, Schimann E, et al. Age-related clinical spectrum of Plasmodium knowlesi malaria and predictors of severity. Clin Infect Dis. 2018;67:350–9.
Millar SB, Singh JC. Human infections with Plasmodium knowlesi-zoonotic malaria. Clin Microbiol Infect. 2015;21:640–8.
WHO. Management of severe malaria, Practical Handbook. 3rd ed. Geneva: World Health Organization; 2012.
Ministry of Health, Nutrition and Indigenous Medicine. Management of healthcare workers following occupational exposure to blood and other body fluids and post exposure prophylaxis for HIV. 2017. http://www.health.gov.lk/CMS/cmsmoh1/upload/english/01-19-2017-eng.pdf. Accessed 29 April 2018.
Lai S, Wardrop NA, Huang Z, Bosco C, Sun J, Bird T, et al. Plasmodium falciparum malaria importation from Africa to China and its mortality: an analysis of driving factors. Sci Rep. 2016;6:e39524.
Public Health England. Malaria imported to United Kingdom: 2016-implications for those advising travellers. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/686034/Malaria_imported_into_the_UK_2016_FINAL_REVISED.pdf. Accessed 12 May 2018.
Stępień M, Rosińska M. Imported malaria in Poland 2003 to 2011: implications of different travel patterns. J Travel Med. 2014;21:189–94.
WHO. International Travel and Health, World Health Organization. Geneva. 2012. http://www.who.int/ith/2017-ith-chapter7.pdf. Accessed 12 May 2018.
Ménard D, Barnadas C, Bouchier C, Henry-Halldin C, Gray LR, Ratsimbasoa A, et al. Plasmodium vivax clinical malaria is commonly observed in Duffy-negative Malagasy people. Proc Natl Acad Sci USA. 2010;107:5967–71.
UNAIDS. Country Fact sheet Madagascar. 2016. http://www.unaids.org/en/regionscountries/countries/madagascar. Accessed 29 April 2018.
Guidelines on malaria chemotherapy & management of patients with malaria. Ministry of Health, Nutrition and Indigenous Medicine, Sri Lanka. http://www.malariacampaign.gov.lk/precentation/treatmentguide.aspx. Accessed 12 May 2018.
The newsletter of the Sri Lanka Medical Association, 2018;1:3. http://slma.lk/wp-content/uploads/2018/02/SLMA-January-2018-Newsletter-for-web.pdf. Accessed 13 May 2018.
The newsletter of the Sri Lanka Medical Association, 2018;2:7. http://slma.lk/wp-content/uploads/2018/04/March-Newsletter-2018-V-1.6-Final-Draft-FYA.pdf. Accessed 13 May 2018.
WHO. Guidelines for treatment of malaria. 3rd edn, 2015. Geneva: World Health Organization; 2015. https://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0093121/#ch7.s1. Accessed 5 May 2018.
Rahimi BA, Thakkinstian A, White NJ, Sirivichayakul C, Dondorp AM, Chokejindachai W. Severe vivax malaria: a systematic review and meta-analysis of clinical studies since 1900. Malar J. 2014;13:481.
Epidemiology Unit, Ministry of Health, Sri Lanka. http://www.epid.gov.lk/web/index.php?option=com_content&view=article&id=171&Itemid=487&lang=en. Accessed 13 May 2018.
Authors’ contributions
The malaria case was confirmed by WMKTdeAWG. The patient was managed by RMJKR and RH. Preventive measures to prevent secondary cases were done by DR, PS and WMKTdeAWG. Overall management and supervision was done by DR and HDBH. The manuscript was prepared by DF and DR. All authors read and approved the final manuscript.
Acknowledgements
The authors wish to thank Dr. Kamini Mendis for advising on management of the patient and reading and providing useful comments to improve the quality of the manuscript. We are grateful to the all Anti Malaria Campaign staff who were involved in the management and follow up of this patient. We thank the staff of both the private and government hospital for the prompt management of this patient.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
Information regarding this patient is kept confidentially by the Anti Malaria Campaign.
Consent for publication
Ethical approval to investigate and follow up any patient diagnosed with malaria in Sri Lanka for research purpose has been obtained from the Ethical Review Committee, Faculty of Medicine, University of Colombo and the Ethics Review Committee of the Sri Lanka Medical Association. Consent was obtained from the patient to publish the findings.
Funding
None.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Ranaweera, D., Kanchana Rajapaksha, R.M.J., Silva, P. et al. Severe Plasmodium vivax malaria, HIV, tuberculosis co-infection in a Sri Lankan traveller: case management and challenges during the prevention of malaria reintroduction phase. Malar J 17, 429 (2018). https://doi.org/10.1186/s12936-018-2581-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12936-018-2581-1