Abstract
Background
To improve outcomes in patients with diabetes mellitus (DM) undergoing percutaneous coronary intervention remain an unmet clinical need. The study aimed to evaluate the efficacy and safety of G2-DESs and BP-DESs in patients with and without DM in a single center in China.
Methods
A total of 7666 consecutive patients who exclusively had G2-DES or BP-DES implantation throughout 2013 in our center were studied. The primary efficacy endpoint was any target lesion revascularization (TLR), whereas the primary safety endpoint was a composite of death or myocardial infarction (MI) at 2-year follow-up.
Results
G2-DESs had a similar occurrence of death, non-fatal MI, TLR, stroke, and stent thrombosis compared with BP-DESs in patients with DM (all P > 0.05). The incidence of TVR and TLR was lower for G2-DESs than for BP-DESs in patients without DM (3.2% vs. 5.1%, P = 0.002; 2.2% vs. 4.5%, P < 0.001, respectively). Kaplan–Meier analysis also showed better TVR- and TLR-free survival rates for G2-DESs than for BP-DESs in patients without DM. Multivariate analysis showed that a BP-DES was an independent risk factor for TLR (hazard ratio 1.963, 95% confidence interval 1.390–2.772, P < 0.001) in patients without DM, which was not predictive of other components of major adverse cardiac events (P > 0.05).
Conclusions
G2-DESs have better efficacy, represented by a reduced risk of TLR, and similar safety compared with BP-DESs in patients without DM. G2-DESs have similar efficacy and safety compared with BP-DESs in patients with DM at 2-year follow-up.
Similar content being viewed by others
Background
Coronary stents have been used for more than two decades. During this period, stent designs have been modified to improve safety in patients [1]. Bare metal stents (BMSs) were followed by first-generation permanent polymer drug-eluting stents (paclitaxel- and sirolimus-DESs). These stents were then followed by second-generation permanent polymer DESs (everolimus- and zotarolimus-DESs). Currently, biodegradable polymer DESs (BP-DESs) are being used and potentially improve patients’ outcomes.
First-generation DESs decrease the risk of stent restenosis and ischemia-driven target lesion revascularization (TLR) compared with BMSs in a broad range of patients and coronary lesions [2]. Second-generation DESs (G2-DESs), such as everolimus- and zotarolimus-eluting stents, markedly decrease the risk of early stent thrombosis and repeat revascularization compared with first-generation DESs and BMSs [3,4,5,6]. Nevertheless, these new stents still have limitations, not least the requirement for prolonged dual-antiplatelet therapy and an apparent increase in the incidence of Academic Research Consortium definite early and late stent thrombosis [7]. These problems are likely caused by delayed vessel healing, impaired endothelialization, allergy, inflammation, and the presence of durable polymers [8, 9]. DESs using biodegradable polymers were designed to overcome long-term adverse vascular reactions when drug elution is complete. These stents may reduce the risk of in-stent restenosis and be non-inferior to in-segment late loss after deployment [10,11,12,13].
Interventional treatment of patients with coronary artery disease and diabetes mellitus (DM) remains a challenge. This group of patients suffers from a greater burden and more rapid progression of coronary atherosclerosis compared with non-diabetic patents. DM is associated with an increased risk of in-stent restenosis, TLR, and target vessel revascularization (TVR) in patients undergoing percutaneous coronary intervention (PCI) [14,15,16]. Therefore, adverse outcomes after coronary revascularization in patients with DM remain a concern regarding which type of DES to use [17]. Whether BP-DESs are potentially superior to G2-DESs still remains undetermined in patients with DM. Therefore, this study aimed to compare long-term safety and efficacy after PCI with G2-DESs and BP-DESs in an unrestricted, real-life, single-center population with or without DM in China.
Methods
Study population
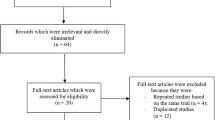
This was a prospective, observational study. Data from all consecutive patients from a single center who underwent PCI were prospectively collected. Between January 1, 2013, and December 31, 2013, a total of 10,724 consecutive patients who underwent PCI were enrolled. Exclusion criteria included the following: (1) patients who received only percutaneous transluminal coronary angioplasty without stent implantation; and (2) patients who received neither G2-DESs nor BP-DESs, or received multiple types of stents concurrently. A total of 7666 patients were enrolled who received either G2-DESs (n = 6094) or BP‑DESs (n = 1572) (Fig. 1). DM was diagnosed on the basis on previous medical records of the patients and data of the therapeutic status based on the drug regimen of glucose-lowering therapy (including insulin, oral antibiotics, and diet and exercise). The stent type and operating strategy were left to the operators’ discretion. In our center, G2-DESs included zotarolimus-eluting stents (Endeavor and Endeavor Resolute; Medtronic Vascular, USA), everolimus-eluting stents (Xience V and Xience Prime; Abbott Vascular, USA, and Promus and Promus Element; Boston Scientific, USA), and domestic sirolimus-eluting stents (Firebird2; MicroPort Medical, China). BP-DESs included sirolimus-eluting stents (FIREHAWK; MicroPort Medical, China, Excel; JW Medical, China, BuMA; Sino Medical, China, NOYA; Medfavour Medical, China, and Tivoli; Essen Technology, China). If patients received PCI treatment in multiple stages because of multivessel disease, we combined the data from all phases of treatment. The study protocol was approved by the institutional review board of our hospital, and all patients provided written informed consent before the study.
Procedural details
The PCI strategy and stent type were left to the discretion of the operating surgeon. Before the procedure, selected patients with PCI who were not on long-term aspirin and/or P2Y12 inhibitors received oral administration of aspirin 300 mg and clopidogrel (loading dose of 300 mg). Patients with acute coronary syndrome (ST-elevation myocardial infarction and NSTE-acute coronary syndrome) who were scheduled for PCI received the same dose of aspirin and clopidogrel (loading dose of 300 or 600 mg) as soon as possible. During the procedure, unfractionated heparin (100 U/kg) was administered to all of the patients, and glycoprotein IIb/IIIa inhibitors were used according to the operator’s judgment. If PCI proceeded for longer than 1 h, an additional 1000 U of heparin sodium was administered. Results of coronary angiography were interpreted by experienced cardiologists. More than 50% stenosis of the left main artery, left anterior descending artery, left circumflex artery, right coronary artery, and main branch of these vessels was defined as coronary artery stenosis. More than 70% stenosis of these vessels was indicated for coronary stent implantation. After the procedure, aspirin was prescribed at a dose of 100 mg daily indefinitely, and clopidogrel 75 mg daily or ticagrelor 90 mg twice daily for at least 1 year after PCI was recommended.
Follow-up and definitions
All of the patients were evaluated by a visit to the clinic or by phone 1, 3, 6, and 12 months postoperatively and annually thereafter up to 2 years. Follow-up data were collected through medical records, telephone calls, or clinical visits, and an independent group of follow-up investigators were in charge of data collection and revision. Patients were advised to return for coronary angiography if indications of ischemic events occurred. The composite of major adverse cardiac events (MACE) was defined as the occurrence of death, nonfatal myocardial infarction (MI), TLR, stent thrombosis, and stroke during follow-up (730 ± 30 days). MI was defined by the Third Universal Definition of myocardial infarction [18]. TVR was defined as revascularization for a new lesion on the target vessel either by PCI or by coronary artery bypass grafting (CABG). TLR was defined as revascularization for a new lesion at or within 5 mm from the previously implanted stent either by PCI or by CABG [19]. Stent thrombosis included definite, probable, and possible stent thrombosis based on the Academic Research Consortium criteria [19]. Death that could not be attributed to a noncardiac etiology was considered cardiac death. Bleeding was quantified according to Bleeding Academic Research Consortium (BARC) criteria [20]. In the present study, major bleeding was defined as BARC type 2, 3, or 5 (type 4, CABG-related bleeding, was excluded). The efficacy endpoint was TLR and the safety endpoint was a composite of death or MI at 2 years. Two independent physicians who were blinded to the laboratory data adjudicated events after reviewing the source documents.
Statistical analysis
Continuous variables are presented as mean ± standard deviation and were compared using the Student’s t-test or one-way analysis of variance, as appropriate. Categorical variables are expressed as numbers and percentages and were compared using the Chi square test or Fisher’s exact test. After significant differences among variables were shown using one-way analysis of variance, post hoc comparisons between groups were performed using the Student–Newman–Keuls method for multiple comparisons. The event-free survival rates were calculated by the Kaplan–Meier method and were compared by the log-rank test. The Cox proportional regression model was used to assess the independent predictors of endpoint events. Variables that had P values of < 0.10 in univariate analysis were included in multivariate COX regression analysis based on the backward stepwise method. All P values were two-sided and P < 0.05 was considered statistically significant. All statistical analyses were performed using SPSS Statistics for Windows, Version 22.0 (IBM Corp., Armonk, NY, USA).
Results
Baseline, angiographic and procedural characteristics of the patients
Among a total of 7666 patients, 2283 (29.8%) patients had DM. A total of 1862 patients with DM used G2-DESs. Among these patients, the Endeavor was used in 4.5%, the Endeavor Resolute in 31.3%, the Xience V in 23.2%, the Xience Prime in 9.9%, the Promus in 0.1%, the Promus Element in 8.8%, and the Firebird2 in 22.2%. A total of 421 patients with DM used BP-DESs. Among these patients, the Excel was used in 75.8%, the BuMA in 5.2%, the NOYA in 1.9%, and the Tivoli in 17.1%. A total of 4232 patients without DM used G2-DESs. Among these patients, the Endeavor was used in 3.6%, the Endeavor Resolute in 30.9%, the Xience V in 22.2%, the Xience Prime in 11.4%, the Promus Element in 9.4%, and the Firebird2 in 22.5%. A total of 1151 patients without DM used BP-DESs. Among these patients, the Excel was used in 69.1%, the BuMA in 8.1%, the NOYA in 1.9%, and the Tivoli in 20.9%.
With regard to baseline characteristics in patients with DM, the BP-DES group had a significantly higher proportion of hypertension (P = 0.023), a history of old myocardial infarction (OMI) (P = 0.013), and previous PCI (P = 0.015) than did the G2-DES group. In patients without DM, the BP-DES group had a significantly higher proportion of ST-elevation myocardial infarction (P = 0.03) and a lower proportion of a history of previous CABG (P = 0.006) than did the G2-DES group. With regard to medication, the proportions of using β‑blockers (P = 0.004) and GP IIb/IIIa inhibitors (P = 0.035) were significantly higher in the BP-DES group than in the G2-DES group in patients with DM. The proportions of using dual-antiplatelet therapy (P = 0.018), GP IIb/IIIa inhibitors (P < 0.001), and proton pump inhibitors (P = 0.012) were significantly higher in the BP-DES group than in the G2-DES group in patients without DM (Table 1).
Angiographic and procedural characteristics were generally similar between patients with DM in the BP-DES and G2-DES groups (all P > 0.05). However, patients without DM in the BP-DES group had a significantly greater number of lesions treated (P = 0.013) and a higher prevalence of thrombolysis in myocardial infarction 0 flow before PCI (P < 0.001), B2 or C lesions (P = 0.013), and chronic total occlusion lesions (CTO) (P < 0.001) compared with the G2-DES group (Table 2).
Two-year clinical outcomes of G2-DESs versus BP-DESs
In patients with DM, the incidence of all-cause death, cardiac death, stent thrombosis, TVR, TLR, stroke, and bleeding were not significantly different between the BP-DES and G2-DES groups at the 2-year follow-up (P > 0.05). Furthermore, in patients with DM, the incidence of non-fatal MI had the higher tended in the G2-DES group compared with the BP-DES group (P = 0.05) (Table 3). In patients without DM, the incidence of all-cause death, cardiac death, non-fatal MI, stent thrombosis, stroke, and bleeding was not significantly different between the BP-DES and G2-DES groups (P > 0.05). However, the incidence of TVR (5.1% vs. 3.2%, P = 0.002) and TLR (4.5% vs. 2.2%, P < 0.001) was significantly higher in the BP-DES group than in the G2-DES group in the 2-year follow-up (Table 3). Kaplan–Meier analysis of the cumulative incidence of TVR and TLR showed no significant difference between the BP-DES and G2-DES groups in patients with DM (P = 0.221, P = 0.103, respectively) (Fig. 2). Kaplan–Meier analysis showed that the cumulative incidence of TVR and TLR was significantly greater in the BP-DES group than in the G2-DES group in patients without DM (P = 0.002, P < 0.001, respectively) (Fig. 3). Regardless of whether patients had DM, Kaplan–Meier analysis of the cumulative incidence of non-fatal MI showed no significant difference between the BP-DES and G2-DES groups (Fig. 4).
In unadjusted univariate analysis, the 2-year cumulative incidence of all-cause death, cardiac death, non-fatal MI, stent thrombosis, TVR, TLR, stroke, and bleeding was not significantly different between the BP-DES and G2-DES groups in patients with DM (Table 4). In unadjusted univariate analysis, the cumulative incidence of all-cause death, cardiac death, stent thrombosis, stroke, and bleeding were not significantly different between the BP-DES and G2-DES groups in patients without DM. However, TVR and TLR were significantly higher in the BP-DES group than in the G2-DES group in patients without DM [hazard ratio (HR) 1.619, 95% confidence interval [CI] 1.193–2.198, P = 0.002; HR 2.109, 95% CI 1.501–2.963, P < 0.001, respectively] (Table 5).
After multivariable analysis with adjustment for age, sex, body mass index, left ventricular ejection fraction, serum creatinine levels, use of a proton pump inhibitor and GPIIa/IIIb, SYNTEX score, a history of coronary heart disease, previous PCI and CABG, OMI, hypertension, current smoker, multivessel disease, B2 or C lesions, the number of target lesions, the transradial approach, and CTO, use of a BP-DES was still not an independent predictor of TLR in patients with DM (HR 1.453, 95% CI 0.891–2.371, P = 0.134) (Table 4). For clinical endpoints that were measured, current smoker, a history of coronary heart disease, and old myocardial infarction were independent predictors of TLR in patients with DM (Additional file 1: Fig. S1). However, before and after applying multivariable analysis, use of a BP-DES was still an independent predictor of TLR in patients without DM (HR 1.963, 95% CI 1.390–2.772, P < 0.001) (Table 5). Furthermore, B2 or C lesions and the SYNTAX score were independent predictors of TLR in patients without DM (Additional file 2: Fig. S2).
Discussion
Main findings in this study
Our prospective, observational study from a high-volume cardiovascular center in China compared the efficacy and safety between G2-DESs and BP-DESs in a large group of patients with and without DM. Based on a 2-year follow-up, our major findings were as follows: (1) G2-DESs were associated with a lower risk of TLR, which suggested better efficacy, and G2-DESs had a similar safety profile to that of BP-DESs in patients without DM; and (2) among patients with DM, G2-DESs had similar efficacy and safety profiles to those of BP-DESs.
Relationship between several types of DESs and adverse cardiac events
G2-DESs are characterized by novel stent platforms, more lipophilic sirolimus analogues, and/or more biocompatible durable polymers. These advantages of durable polymer G2-DESs enabled addition. The design of the stent platform may also shed light on differences in efficacy. The rate of TLR in patients with lesion calcification was lower with G2-DESs than with G1-DESs [21]. Additionally, lower strut thickness was associated with improved re-endothelialization and arterial healing, [22] and arterial repair after G2-DES implantation into vulnerable plaques remains vulnerable, even at 1-year follow-up [23]. Biodegradable polymers, in contrast to durable polymers, can be completely metabolized, potentially reducing the risk of late complications, such as stent uncovering, malapposition, and endothelial dysfunction [24]. Some clinical trials have shown that BP-DESs have a low rate of TVR and TLR in real-world performance, [25, 26] even in high-risk patients, such as those with DM, small vessels, CTO, and AMI [27,28,29]. BP-DESs and G2-DESs could be effective alternatives for drug release from the metallic stent platform. Longer term follow-up might be required to demonstrate the potential benefits of BP-DESs relative to G2-DESs. Some large head-to-head trials and network meta-analyses have shown that safety and efficacy outcomes of BP-BESs were non-inferior to those of G2-DESs 1, 3, and 5 years after stent implantation [30,31,32,33,34].
Efficacy and safety of several types of DESs in patients with and without DM
DM is still one of the major risk factors for stent restenosis [16]. Some studies have shown that patients with DM using BP-DESs, particularly those with insulin-dependent DM, have worse outcomes, such as TLR and mortality, than patients without DM [35, 36]. However, a unified view of the long-term clinical efficacy and safety of different generations of DESs among DM patients has not been well established. Long-term follow-up for at least 1 year is necessary to verify the efficacy and safety of DESs for patients with DM. Our study expands current knowledge of long-term clinical outcomes up to 2 years between G2-DES and BP-DES implantation according to the presence or absence of DM.
In our study, before and after multivariable adjustment, there were no differences in 2-year MACE between G2-DES and BP-DES implantation in patients with or without DM. Before and after multivariable adjustment, BP-DES implantation had almost a 1.5–2.0-fold higher risk of 2-year TLR compared with G2-DESs in patients without DM. However, there were no differences in 2-year TLR between G2-DES and BP-DES implantation in patients with DM, even after multivariable adjustment.
Some previous studies showed that G2-DESs had a lower risk for TLR compared with G1-DESs in patients with DM [37, 38]. This finding was not observed in BP-DES compared with G2-DES implantation in patients with DM in our study, [12, 39,40,41] G2-DESs had a lower risk for TLR compared with BP-DESs in patients without DM in our study. In patients with DM in our study, clinical conditions were more complex in BP-DES implantation, with a higher proportion of hypertension, OMI, and previous PCI than with G2-DES implantation. Additionally, in patients with DM, current smoker, a history of coronary heart disease, and OMI were independent predictors of TLR. Some study had shown that fluctuation of glucose levels may affect vessel healing after DES implantation in patients with CHD [42]. Therefore, fluctuations in glucose levels may be an important target for secondary prevention after coronary stenting. In our study, the average value of HbA1c was 7.8% and control of HbA1c was not ideal in patients with DM. Hence, further control was required. In patients without DM in our study, lesions were more complex in BP-DES implantation, with a higher proportion of CTO and B2 or C lesions. Additionally, B2 or C lesions and the SYNTAX score were independent predictors of TLR in patients without DM. The complexity of the lesion level may have affected the proportion of TLR after BP-DES implantation in patients without DM in our study.
In the current study, the strut thickness of the G2-DES was 81–91 μm. In contrast, most BP-DESs had a higher strut thickness of 120 μm (Excel) and 100 μm (BuMA), [43] which accounted for 79.9% of all BP-DESs used in the study. This may in part explain the finding in the current study that G2-DESs had a similar incidence of stent thrombosis as BP-DESs in patients with or without DM within 2 years after PCI. Additionally, patients in our study had good adherence to dual antiplatelet therapy after PCI. Up to 97.4% of patients received dual antiplatelet therapy for 1 year, which may have played an important role in preventing stent thrombosis and cardiogenic death.
Limitations
There are several limitations in our single-center study. First, as in any non-randomized study, our research was limited by an imbalance in patients and selection of procedures. However, multivariate Cox regression was applied to minimize the dissymmetry between the groups. Second, all of the BP-DESs in our study were sirolimus-eluting stents because of their availability in our center, which limited the generalization of the conclusion to all BP-DES. Third, the fact that our study was from a single center hindered the statistical power. Additionally, a safety issue associated with durable polymers is typically represented by stent thrombosis. However, the 2-year follow-up in our study may not have fully addressed safety concerns in current practice. Therefore, we intended to perform a longer follow-up and update this investigation in the future.
Conclusions
Our prospective, observational study shows that G2-DESs reduce the risk of TLR, and have a similar incidence of death and MI compared with BP-DESs in patients without DM at 2-year follow-up. G2-DESs are similar to BP-DESs regarding the incidence of death, TLR, and stent thrombosis in patients with DM. These findings suggest a similar efficacy and safety between these two types of stents.
Abbreviations
- BARC:
-
Bleeding Academic Research Consortium
- BMS:
-
bare metal stents
- BP-DES:
-
biodegradable polymer drug eluting stents
- CABG:
-
coronary artery bypass grafting
- CTO:
-
chronic total occlusion
- DM:
-
diabetes mellitus
- MACE:
-
major adverse cardiac events
- MI:
-
myocardial infarction
- OMI:
-
old myocardial infarction
- PCI:
-
percutaneous coronary interventions
- G2-DES:
-
second-generation drug eluting stents
- SYNTEX:
-
synergy between percutaneous coronary interventions with TAXUS and cardiac surgery
- TLR:
-
target lesion revascularization
- TVR:
-
target vessel revascularization
References
Stefanini GG, Holmes DR Jr. Drug-eluting coronary-artery stents. N Engl J Med. 2013;368(3):254–65.
Kastrati A, Dibra A, Spaulding C, Laarman GJ, Menichelli M, Valgimigli M, Di Lorenzo E, Kaiser C, Tierala I, Mehilli J, et al. Meta-analysis of randomized trials on drug-eluting stents vs. bare-metal stents in patients with acute myocardial infarction. Eur Heart J. 2007;28(22):2706–13.
Kimura T, Morimoto T, Nakagawa Y, Kawai K, Miyazaki S, Muramatsu T, Shiode N, Namura M, Sone T, Oshima S, et al. Very late stent thrombosis and late target lesion revascularization after sirolimus-eluting stent implantation: five-year outcome of the j-Cypher Registry. Circulation. 2012;125(4):584–91.
Palmerini T, Biondi-Zoccai G, Della Riva D, Stettler C, Sangiorgi D, D’Ascenzo F, Kimura T, Briguori C, Sabate M, Kim HS, et al. Stent thrombosis with drug-eluting and bare-metal stents: evidence from a comprehensive network meta-analysis. Lancet. 2012;379(9824):1393–402.
Nakagawa Y, Kimura T, Morimoto T, Nomura M, Saku K, Haruta S, Muramatsu T, Nobuyoshi M, Kadota K, Fujita H, et al. Incidence and risk factors of late target lesion revascularization after sirolimus-eluting stent implantation (3-year follow-up of the j-Cypher Registry). Am J Cardiol. 2010;106(3):329–36.
Poder TG, Erraji J, Coulibaly LP, Koffi K. Percutaneous coronary intervention with second-generation drug-eluting stent versus bare-metal stent: systematic review and cost-benefit analysis. PLoS ONE. 2017;12(5):e0177476.
Palmerini T, Biondi-Zoccai G, Della Riva D, Mariani A, Sabate M, Valgimigli M, Frati G, Kedhi E, Smits PC, Kaiser C, et al. Clinical outcomes with drug-eluting and bare-metal stents in patients with ST-segment elevation myocardial infarction: evidence from a comprehensive network meta-analysis. J Am Coll Cardiol. 2013;62(6):496–504.
Garg S, Bourantas C, Serruys PW. New concepts in the design of drug-eluting coronary stents. Nat Rev Cardiol. 2013;10(5):248–60.
Virmani R, Guagliumi G, Farb A, Musumeci G, Grieco N, Motta T, Mihalcsik L, Tespili M, Valsecchi O, Kolodgie FD. Localized hypersensitivity and late coronary thrombosis secondary to a sirolimus-eluting stent: should we be cautious? Circulation. 2004;109(6):701–5.
Natsuaki M, Kozuma K, Morimoto T, Kadota K, Muramatsu T, Nakagawa Y, Akasaka T, Hanaoka KI, Tanabe K, Morino Y, et al. Five-year outcome of a randomized trial comparing second generation drug-eluting stents using either biodegradable polymer or durable polymer: the NOBORI Biolimus-eluting versus XIENCE/PROMUS everolimus-eluting stent trial (NEXT). EuroIntervention. 2018. https://doi.org/10.4244/EIJ-D-17-01050.
Meredith IT, Verheye S, Dubois C, Dens J, Farah B, Carrie D, Walsh S, Oldroyd K, Varenne O, El-Jack S, et al. Final five-year clinical outcomes in the EVOLVE trial: a randomised evaluation of a novel bioabsorbable polymer-coated, everolimus-eluting stent. EuroIntervention. 2018;13(17):2047–50.
Lefevre T, Haude M, Neumann FJ, Stangl K, Skurk C, Slagboom T, Sabate M, Goicolea J, Barragan P, Cook S, et al. Comparison of a novel biodegradable polymer sirolimus-eluting stent with a durable polymer everolimus-eluting stent: 5-year outcomes of the randomized BIOFLOW-II trial. JACC Cardiovasc Interv. 2018;11(10):995–1002.
Kufner S, Byrne RA, Valeskini M, Schulz S, Ibrahim T, Hoppmann P, Schneider S, Laugwitz KL, Schunkert H, Kastrati A, et al. Five-year outcomes from a trial of three limus-eluting stents with different polymer coatings in patients with coronary artery disease: final results from the ISAR-TEST 4 randomised trial. EuroIntervention. 2016;11(12):1372–9.
Schofer J, Schluter M, Rau T, Hammer F, Haag N, Mathey DG. Influence of treatment modality on angiographic outcome after coronary stenting in diabetic patients: a controlled study. J Am Coll Cardiol. 2000;35(6):1554–9.
West NE, Ruygrok PN, Disco CM, Webster MW, Lindeboom WK, O’Neill WW, Mercado NF, Serruys PW. Clinical and angiographic predictors of restenosis after stent deployment in diabetic patients. Circulation. 2004;109(7):867–73.
Qin SY, Zhou Y, Jiang HX, Hu BL, Tao L, Xie MZ. The association of diabetes mellitus with clinical outcomes after coronary stenting: a meta-analysis. PLoS ONE. 2013;8(9):e72710.
Bangalore S, Toklu B, Feit F. Outcomes with coronary artery bypass graft surgery versus percutaneous coronary intervention for patients with diabetes mellitus: can newer generation drug-eluting stents bridge the gap? Circ Cardiovasc Interv. 2014;7(4):518–25.
Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD, Writing Group on the Joint ESCAAHAWHFTFftUDoMI, Thygesen K, Alpert JS, White HD, et al. Third universal definition of myocardial infarction. Eur Heart J. 2012;33(20):2551–67.
Cutlip DE, Windecker S, Mehran R, Boam A, Cohen DJ, van Es GA, Steg PG, Morel MA, Mauri L, Vranckx P, et al. Clinical end points in coronary stent trials: a case for standardized definitions. Circulation. 2007;115(17):2344–51.
Mehran R, Rao SV, Bhatt DL, Gibson CM, Caixeta A, Eikelboom J, Kaul S, Wiviott SD, Menon V, Nikolsky E, et al. Standardized bleeding definitions for cardiovascular clinical trials: a consensus report from the Bleeding Academic Research Consortium. Circulation. 2011;123(23):2736–47.
Nishida K, Nakatsuma K, Shiomi H, Natsuaki M, Kawai K, Morimoto T, Kozuma K, Igarashi K, Kadota K, Tanabe K, et al. Second-generation vs. first-generation drug-eluting stents in patients with calcified coronary lesions- pooled analysis from the RESET and NEXT trials. Circ J. 2018;82(2):376–87.
Foin N, Lee RD, Torii R, Guitierrez-Chico JL, Mattesini A, Nijjer S, Sen S, Petraco R, Davies JE, Di Mario C, et al. Impact of stent strut design in metallic stents and biodegradable scaffolds. Int J Cardiol. 2014;177(3):800–8.
Kawai K, Ichikawa M, Masuyama T, Kijima Y. Angioscopic comparison of arterial repair after second-generation drug-eluting stent implantation into vulnerable and stable coronary plaques. Int J Cardiol. 2016;221:855–8.
Rodriguez-Granillo A, Rubilar B, Rodriguez-Granillo G, Rodriguez AE. Advantages and disadvantages of biodegradable platforms in drug eluting stents. World J Cardiol. 2011;3(3):84–92.
Godino C, Beneduce A, Ferrante G, Ielasi A, Pivato AC, Chiarito M, Cappelletti A, Perfetti G, Magni V, Prati E, et al. One-year clinical outcome of biodegradable polymer sirolimus-eluting stent in all-comers population. Insight from the ULISSE registry (ULtimaster Italian multicenter all comerS Stent rEgistry). Int J Cardiol. 2018;260:36–41.
Maupas E, Lipiecki J, Levy R, Faurie B, Karsenty B, Moulichon ME, Brunelle F, Maillard L, de Poli F, Lefevre T. Safety and efficacy outcomes of 3rd generation DES in an all-comer population of patients undergoing PCI: 12-month and 24-month results of the e-Biomatrix French registry. Catheter Cardiovasc Interv. 2017;90(6):890–7.
Kornowski R, Roguin A, Danenberg H, Assa HV, Abergel E, Rozenbaum E, Guetta V, Landes U, Jabara R, Merdler A, et al. BIOFLOW-III satellite-One-year clinical outcomes of diabetic patients treated with a biodegradable polymer sirolimus-eluting stent and comprehensive medical surveillance. Cardiovasc Revasc Med. 2017;18(5):338–43.
Waltenberger J, Brachmann J, van der Heyden J, Richardt G, Frobert O, Seige M, Erglis A, Dewilde W, Winkens M, Hegeler-Molkewehrum C, et al. Real-world experience with a novel biodegradable polymer sirolimus-eluting stent: twelve-month results of the BIOFLOW-III registry. EuroIntervention. 2016;11(10):1106–10.
Meliga E, Lupi A, Latib A, Gagnor A, Boccuzzi G, Alcantara M, Lombardi P, Sticchi A, Aranzulla TC, Scrocca I, et al. Biolimus-Eluting StenT For de-novo coRonary artery dIsease in patiENts with Diabetes mellituS: the BESTFRIENDS multicentre registry. J Cardiovasc Med. 2016;17(10):729–35.
Cassese S, Byrne RA, Juni P, Wykrzykowska JJ, Puricel S, Ndrepepa G, Schunkert H, Fusaro M, Cook S, Kimura T, et al. Midterm clinical outcomes with everolimus-eluting bioresorbable scaffolds versus everolimus-eluting metallic stents for percutaneous coronary interventions: a meta-analysis of randomised trials. EuroIntervention. 2018;13(13):1565–73.
Sakurai R, Burazor I, Bonneau HN, Kaneda H. Long-term outcomes of biodegradable polymer biolimus-eluting stents versus durable polymer everolimus-eluting stents: a meta-analysis of randomized controlled trials. Int J Cardiol. 2016;223:1066–71.
Vlachojannis GJ, Smits PC, Hofma SH, Togni M, Vazquez N, Valdes M, Voudris V, Slagboom T, Goy JJ, den Heijer P, et al. Biodegradable polymer biolimus-eluting stents versus durable polymer everolimus-eluting stents in patients with coronary artery disease: final 5-year report from the COMPARE II trial (abluminal biodegradable polymer biolimus-eluting stent versus durable polymer everolimus-eluting stent). JACC Cardiovasc Interv. 2017;10(12):1215–21.
Raungaard B, Christiansen EH, Botker HE, Hansen HS, Ravkilde J, Thuesen L, Aaroe J, Villadsen AB, Terkelsen CJ, Krusell LR, et al. Comparison of durable-polymer zotarolimus-eluting and biodegradable-polymer biolimus-eluting coronary stents in patients with coronary artery disease: 3-year clinical outcomes in the randomized SORT OUT VI trial. JACC Cardiovasc Interv. 2017;10(3):255–64.
El-Hayek G, Bangalore S, Casso Dominguez A, Devireddy C, Jaber W, Kumar G, Mavromatis K, Tamis-Holland J, Samady H. Meta-analysis of randomized clinical trials comparing biodegradable polymer drug-eluting stent to second-generation durable polymer drug-eluting stents. JACC Cardiovasc Interv. 2017;10(5):462–73.
Wiemer M, Stoikovic S, Samol A, Dimitriadis Z, Ruiz-Nodar JM, Birkemeyer R, Monsegu J, Finet G, Hildick-Smith D, Tresukosol D, et al. Third generation drug eluting stent (DES) with biodegradable polymer in diabetic patients: 5 years follow-up. Cardiovasc Diabetol. 2017;16(1):23.
Li Y, Han Y, Zhang L, Jing Q, Wang X, Yan G, Ma Y, Wang G, Wang S, Chen X, et al. Clinical efficacy and safety of biodegradable polymer-based sirolimus-eluting stents in patients with diabetes mellitus insight from the 4-year results of the create study. Catheter Cardiovasc Interv. 2013;81(7):1127–33.
Nakatsuma K, Shiomi H, Natsuaki M, Morimoto T, Igarashi K, Kadota K, Muramatsu T, Tanabe K, Morino Y, Akasaka T, et al. Second-generation versus first-generation drug-eluting stents in patients with and without diabetes mellitus: pooled analysis from the RESET and NEXT trials. Cardiovasc Interv Ther. 2018;33(2):125–34.
Kedhi E, Gomes ME, Lagerqvist B, Smith JG, Omerovic E, James S, Harnek J, Olivecrona GK. Clinical impact of second-generation everolimus-eluting stent compared with first-generation drug-eluting stents in diabetes mellitus patients: insights from a nationwide coronary intervention register. JACC Cardiovasc Interv. 2012;5(11):1141–9.
Harada Y, Colleran R, Kufner S, Giacoppo D, Rheude T, Michel J, Cassese S, Ibrahim T, Laugwitz KL, Kastrati A, et al. Five-year clinical outcomes in patients with diabetes mellitus treated with polymer-free sirolimus- and probucol-eluting stents versus second-generation zotarolimus-eluting stents: a subgroup analysis of a randomized controlled trial. Cardiovasc Diabetol. 2016;15(1):124.
Sprimont P, Pierard S, Vanoverschelde JL, Debbas N. Efficacy and safety of biodegradable polymer biolimus A9-eluting stent versus durable polymer everolimus-eluting stent in diabetic patients: a prospective non-randomized single-centre long-term comparison. Acta Cardiol. 2014;69(5):523–31.
Franzone A, Pilgrim T, Heg D, Roffi M, Tuller D, Vuilliomenet A, Muller O, Cook S, Weilenmann D, Kaiser C, et al. Clinical outcomes according to diabetic status in patients treated with biodegradable polymer sirolimus-eluting stents versus durable polymer everolimus-eluting stents: prespecified subgroup analysis of the BIOSCIENCE trial. Circ Cardiovasc Interv. 2015;8(6):e002319.
Kuroda M, Shinke T, Otake H, Sugiyama D, Takaya T, Takahashi H, Terashita D, Uzu K, Tahara N, Kashiwagi D, et al. Effects of daily glucose fluctuations on the healing response to everolimus-eluting stent implantation as assessed using continuous glucose monitoring and optical coherence tomography. Cardiovasc Diabetol. 2016;15:79.
Qian J, Zhang YJ, Xu B, Yang YJ, Yan HB, Sun ZW, Zhao YL, Tang YD, Gao Z, Chen J, et al. Optical coherence tomography assessment of a PLGA-polymer with electro-grafting base layer versus a PLA-polymer sirolimus-eluting stent at three-month follow-up: the BuMA-OCT randomised trial. EuroIntervention. 2014;10(7):806–14.
Authors’ contributions
JQY, BX, and XFT contributed to conception and design of the study; JQY, BX, XFT, RLG, YJY, SBQ, XYZ, and ZG contributed to performing the experiments and acquisition of data; XFT, YLM, YS, JJX, YY, CH, HHW, PJ, LJ, and RL contributed to analysis and interpretation of data; JQY, BX, XFT, RLG, YJY, and SBQ contributed to drafting the article or revising it critically for important intellectual content. All authors read and approved the final manuscript.
Acknowledgements
We are grateful to the Department of Cardiology, Cardiovascular Institute of Fuwai hospital for its help in recruiting patients. We thank all members who contributed to the study. We thank Ellen Knapp, Ph.D., from Liwen Bianji, Edanz Group China (http://www.liwenbianji.cn/ac), for editing the English text of a draft of this manuscript.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The Ethics Committee of Fuwai Hospital of the National Center for Cardiovascular Diseases and Chinese Academy of Medical Sciences approved the study protocol. Written informed consent was obtained from all participants before any study procedure. Notes: This study was a single-center observational study and was not registered on relevant websites, which only through the approval of the hospital ethics committee.
Funding
This study was supported by the National Science and Technology Support Program of China and sub-project (Nos. 2016YFC1301300 and 2016YFC1301301), the National Natural Science Foundation of China (81470486), and the National Natural Science Foundation for Young Scholars of China (81600292).
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Additional files

Additional file 1: Figure S1.
Multivariate analysis for TLR in patients with DM. TLR: target lesion revascularization, DM: diabetes mellitus, CHD: coronary heart disease, CTO: chronic total occlusion, OMI: old myocardial infarction, CABG: coronary artery bypass grafting, PCI: percutaneous coronary interventions, GP: glycoprotein, PPI: proton pump inhibitors, EF: ejection fraction, BMI: body mass index.

Additional file 2: Figure S2.
Multivariate analysis for TLR in patients without DM. TLR: target lesion revascularization, DM: diabetes mellitus, SYNTEX: Synergy between percutaneous coronary interventions with TAXUS and Cardiac Surgery, CHD: coronary heart disease; CTO: chronic total occlusion; OMI: old myocardial infarction; CABG: coronary artery bypass grafting; PCI: PCI: percutaneous coronary interventions; GP: glycoprotein; PPI: proton pump inhibitors; EF: ejection fraction; BMI: body mass index.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Tang, XF., Ma, YL., Song, Y. et al. Biodegradable polymer drug-eluting stents versus second-generation drug-eluting stents in patients with and without diabetes mellitus: a single-center study. Cardiovasc Diabetol 17, 114 (2018). https://doi.org/10.1186/s12933-018-0758-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-018-0758-0