Abstract
Background
Cardiovascular disease (CVD) is a major cause of mortality in type 1 diabetes (T1D). A pro-calcific drift of circulating monocytes has been linked to vascular calcification and is marked by the surface expression of osteocalcin (OCN). We studied OCN+ monocytes in a unique population with ≥50 years of T1D, the 50-Year Joslin Medalists (J50M).
Methods
CD45 bright/CD14+/OCN+ cells in the circulating mononuclear blood cell fraction were quantified by flow cytometry and reported as percentage of CD45 bright cells. Mechanisms were studied by inducing OCN expression in human monocytes in vitro.
Results
Subjects without history of CVD (n = 16) showed lower levels of OCN+ monocytes than subjects with CVD (n = 14) (13.1 ± 8.4% vs 19.9 ± 6.4%, p = 0.02). OCN+ monocytes level was inversely related to total high density lipoprotein (HDL) cholesterol levels (r = −0.424, p = 0.02), large (r = −0.413, p = 0.02) and intermediate (r = −0.445, p = 0.01) HDL sub-fractions, but not to small HDL. In vitro, incubation with OxLDL significantly increased the number of OCN+ monocytes (p < 0.01). This action of OxLDL was significantly reduced by the addition of HDL in a concentration dependent manner (p < 0.001). Inhibition of the scavenger receptor B1 reduced the effects of both OxLDL and HDL (p < 0.05).
Conclusions
Low OCN+ monocytes levels are associated with lack of CVD in people with long duration T1D. A possible mechanism for the increased OCN+ monocytes could be the elevated levels of oxidized lipids due to diabetes which may be inhibited by HDL. These findings suggest that circulating OCN+ monocytes could be a marker for vascular disease in diabetic patients and possibly modified by HDL elevation.
Similar content being viewed by others
Background
Type 1 diabetes (T1D) is a disease characterized by hyperglycemia due to autoimmune destruction of pancreatic beta-cells. Several end-organ complications develop as a consequence of chronic exposure to hyperglycemia. Among these, cardiovascular disease (CVD) is the major cause of decreased life expectancy [1]. Factors other than hyperglycemia also contribute to the pathogenesis of CVD in T1D. In particular inflammation and dyslipidemia play a pivotal role in the development of atherosclerotic diseases [2,3,4]. Overall, an imbalance between mechanisms of injury and protective factors contributes to vascular complications in diabetes [5]. In particular, our recent data suggest circulating progenitor cells are associated with protection from CVD in subjects with long-standing T1D [6]. On the other hand, circulating osteoprogenitor cells, defined as circulating cells co-expressing osteocalcin (OCN) together with the progenitor stem cell antigen CD34, have been found increased in subjects with cardiovascular disease with and without diabetes [7]. Because of their pro-calcific phenotype, these cells are hypothesized to contribute to the development of vascular calcification and atherosclerosis [8]. Recently, the differentiation towards a pro-calcific phenotype of circulating monocytes has been related to vascular calcification and CVD in those with type 2 diabetes (T2D) [9, 10]. The surface expression of the bone-related protein OCN is the first and essential marker of this drift [9, 11]. Growing evidence demonstrates the ability of circulating OCN+ mononuclear cells to contribute to ectopic ossification [12,13,14].
Some clinical and pathological features of CVD differ between T1D and T2D [15]. Following this, OCN+ monocytes have not yet been explored in T1D. In addition, characterizing factors modulating the expression of OCN in monocytes, especially in diabetes could be important. Oxidized low density lipoprotein (OxLDL) is a known activator of monocytes which are involved in the pathogenesis of atherosclerosis. OxLDL can also induce osteogenic differentiation of different cell types including smooth muscle and endothelial cells [16, 17]. As monocytes are the primary target cells of oxidized lipids, we hypothesized that OxLDL could induce OCN expression in these cells. Moreover, as high density lipoprotein (HDL) actively interacts with monocytes to protect from the development of CVD we hypothesized HDL may counteract the effects of oxidized lipids. We previously identified a cohort of subjects, who were protected from clinically significant CVD after 50 years or more of T1D (50-Year Medalists) which appeared to be associated with elevated HDL-c levels [18]. Therefore the hypothesis of whether OCN+ monocytes were related to CVD and HDL-c was tested in this cohort, then the action of OxLDL and HDL on OCN expression and possible mechanisms were characterized in vitro.
Methods
Study population
Details of the 50-Year Medalist Study and its methods have been extensively described elsewhere [19,20,21,22]. In brief, participants have 50 or more years of documented insulin dependence since time of diagnosis. All individuals were assessed at the Joslin Diabetes Center in Boston, MA, by clinical exam, electrocardiogram, and standard laboratory measures. Thirty-three consecutive Medalist Study participants were enrolled from March 2015 to November 2015 and screened for this sub-study. Subjects with chronic immobilization, hematologic or neoplastic diseases in progress, history of hyper- or hypoparathyroidism were excluded (n = 3) from the study. Positive cardiovascular history was defined as self-reported history of coronary angioplasty, cardiac bypass surgery, hospitalization for heart attack, leg bypass surgery, leg angioplasty or stroke [21]. Other diabetic complications were assessed according to pre-specified criteria [23, 24] (Additional file 1: Additional methods). Urine and blood specimens were collected for biochemical assays (Additional file 1: Additional methods). The Lipoprint system (Quantimetrix, Inc., Redondo Beach, CA) was used to assess HDL and LDL subfractions distinguishing ten HDL and seven LDL subfractions. HDL subfractions were grouped into 3 categories: large (HDL 1–3), intermediate (HDL 4–7), and small (HDL 8–10) [25]. Small and dense LDL were identified as LDL 3-7 fractions [26].
Identification and quantification of circulating OCN+ monocytes by flow cytometry
Based on previous reports [10, 27], OCN+ monocytes were searched in the peripheral blood mononuclear cells (PBMCs) fraction. Blood samples were collected while subjects were fasting and peripheral blood mononuclear cells (PBMCs) were isolated within 2 h (Additional file 1: Additional methods). Freshly isolated PBMCs were washed 3 times in phosphate-buffered saline (PBS) with 1% fetal bovine serum (FBS) and then incubated for 45 min at 4 °C in the dark with BrilliantViolet421-conjugated anti-human CD45 (BioLegend, San Diego, CA), PE/Dazzle594-conjugated anti-human CD14 (BioLegend, San Diego, CA) and AlexFluor488-conjugated anti-human osteocalcin antibodies (R&D Systems, Minneapolis, MN), according to the manufacturers’ instructions. All antibodies were titrated to achieve working concentrations. After incubation samples were washed other three times in PBS with 1% FBS and then assessed by flow cytometry. Ten minutes before cell counts, cells were stained for viability with 7-aminoactinomycin D (7AAD). Up to one million events were recorded for each sample. Data were analyzed with FlowJo software (Tree Star, Ashland, OR) according to the gating strategy described in Additional file 1. Samples were processed in duplicate; the mean of two runs was used as levels of circulating OCN+ monocytes.
THP-1 and U937 culture and treatments
THP-1 and U937 cells (ATCC® TIB-202 and ATCC® CRL-1593.2 Manassas, VA) were treated with 40 μg/ml Oxidized-LDL (OxLDL) ± HDL ± 40 μg/ml LDL (AlfaAesar, ThermoFisher Scientific, Waltham, MA). The chemical inhibitor BLT-1 (SML0059, Sigma, St. Louis, MO) and scavenger receptor, class B, type I (SR-BI) specific blocking antibody (NB400-101, Novus Biologicals, Littleton, CO) were used to inhibit the SR-B1. Anti-rabbit IgG (Sigma, St. Louis, MO) was used as a control Ab. Cells were treated with 0.25 μM BLT-1 or SR-BI antibody (1:800 and 1:500, respectively) for 1 h, and then OxLDL and/or HDL were added as described above.
Assessment of osteocalcin expression in THP-1 and U937 cells
Osteocalcin expression in THP-1 and U937 cells was assessed by immunoblot analysis and by flow cytometry as described in Additional file 1: Additional methods. OCN mRNA was assessed by quantitative real time polymerase chain reaction (qRT-PCR) as described in Additional file 1: Additional methods.
Assessment of nuclear levels of run-related transcription factor 2 in THP-1 and U937 cells
Nuclear and cytosolic fractions were isolated from THP-1 and U937 cells using the Compartment Protein Extraction Kit (Millipore, Cat#2145, Billerica, MA). Nuclear and cytosolic protein concentrations were measured using the Bradford assay. The proteins were blotted with an antibody specific for RUNX2 and Lamin B1 purchase from Abcam (Cambridge, MA) at 1:1000 dilution.
Statistical analysis
Values are expressed as mean ± SD or as medians (25th–75th percentile range) for continuous variables and as proportions for categorical variables (%). Variables were tested for normality using the Shapiro–Wilk test. Comparisons were done using Student’s t test, Kruskal–Wallis, and Chi square or Fisher exact test depending on distribution and sample size. One-way, two-way or three-way analysis of variance (ANOVA) were used as appropriate. Correlations were tested by Pearson or Spearman test depending on distribution. Linear models were used for multivariable analyses to adjust for covariates, with p < 0.05 considered significant for testing in the final model with main effect and outcome. All statistical analyses were performed using Stata/IC 12.1 software (StataCorp, College Station, TX).
Results
Population features
Thirty-three consecutive subjects enrolled in the 50-Year Joslin Medalist Study were screened for participation in this study and three excluded according to the pre-specified exclusion criteria: two for hematologic diseases (chronic lymphocytic leukemia and lymphoma), and 1 due to hyperparathyroidism, leaving 14 males and 16 females eligible. Population features in the whole population and by CVD are summarized in Table 1. For complications, 14 (46.7%) had reported CVD, 18 (60.0%) had diabetic retinopathy, three (10.0%) had nephropathy and 15 (50.0%) had neuropathy. Twenty-three (76.7%) subjects were on lipid lowering agents, 20 (66.7%) on anti-hypertensive medications and 3 (10.0%) on anti-osteoporotic drugs. There were no differences in gender, age, disease duration and anthropometric parameters between subjects with and without CVD. Median [Q1–Q3] HbA1c was 6.9% [6.6–7.3], and similar between subjects with and without CVD (p = 0.92). Those with and without CVD did not have significant differences in eGFR (69.5 [53.0–90.4] vs 92.0 [72.0–96.4] ml/min/1.73 m2, p = 0.093). HDL cholesterol levels trended higher (65 [55–85] vs 61 [45–71] mg/dl, p = 0.09) while intermediate HDL sub-fractions were significantly higher in those without CVD (29.6 ± 7.1 vs 24.3 ± 4.6 mg/dl, p = 0.03). Yet, no significant differences were found in large (32.1 ± 12.5 vs 27.0 ± 11.5 mg/dl, p = 0.26) and small HDL sub-particles (8.6 ± 2.6 vs 7.6 ± 1.7 mg/dl, p = 0.20). Total cholesterol, triglycerides, LDL, 25-OH vitamin D, calcium, alkaline phosphatase and hs-CRP levels did not differ between those with and without CVD. Additionally, no differences in these markers were found by sex. A higher level of large particle HDL was found in females relative to males (34.1 ± 11.7 vs 24.8 ± 11.0 mg/dl, p = 0.03). Yet, no differences by sex were found in intermediate (28.5 ± 6.6 vs 25.5 ± 6.3 mg/dl, p = 0.22) and small HDL (7.8 ± 2.5 vs 8.6 ± 1.9 mg/dl, p = 0.32).
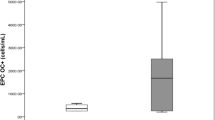
OCN+ monocytes levels differ by CVD and its risk factors
Subjects without CVD showed significantly lower levels of circulating CD45_bright/CD14+/OCN+ cells than subjects with CVD (13.1 ± 8.4% vs 19.9 ± 6.4%, p = 0.02) (Fig. 1). No significant differences were found in the overall levels of CD45_bright and CD45_bright/CD14+ cells between CVD groups indicating no bias in the overall number of cells (Additional file 2: Figure S1a, b). Three subjects with overt diabetic nephropathy had reported history of CVD and corresponding higher levels of CD45_bright/CD14+/OCN+ cells compared to subjects without nephropathy (27.3 ± 3.1% vs 15.1 ± 7.6%, p = 0.03) (Additional file 3: Figure S2A). Additionally, circulating levels of CD45_bright/CD14+/OCN+ were neither associated with proliferative diabetic retinopathy (p = 0.31) nor neuropathy (p = 0.53) (Additional file 3: Figure S2B, C).
As the clinical relationship of HDL and CVD was further explored with levels of circulating CD45_bright/CD14+/OCN+, we found these cells were significantly and inversely associated to total HDL cholesterol levels (r = −0.424, p = 0.019) (Fig. 2a). Additionally, similarly to the analysis of CVD, examination of HDL sub-fractions showed the levels of OCN+ cells were inversely related to the favorable large (r = −0.413, p = 0.02) and intermediate (r = −0.445, p = 0.01) subfractions, while no significant relationship was found with small subfraction levels (Fig. 2b–d). Differently from HDL, CD45_bright/CD14+/OCN+ cell levels were not related to total cholesterol, LDL cholesterol and triglycerides. However, the analysis of LDL subfractions showed a trend towards a positive association between small and dense LDL and CD45_bright/CD14+/OCN+ cell levels (r = 0.336, p = 0.07).
In parallel with the above, CD45_bright/CD14+/OCN+ cell levels were not related to age, disease duration, glycemic control, renal function, calcium, 25-OH vitamin D, alkaline phosphatase or hs-CRP (Additional file 4: Table S1). The use of lipid lowering agents and anti-hypertensive drugs was also not associated with the levels of CD45_bright/CD14+/OCN+ cells.
OxLDL and HDL action on osteocalcin expression in monocyte cell lines through SR-B1
To evaluate a possible direct interaction between HDL and expression of OCN, we studied its expression by HDL and OxLDL in THP-1 cells, a human monocyte cell line. After treatment with 40 μg/ml OxLDL for 12, 24, 48 and 72 h, the number of THP-1 cells expressing osteocalcin, as evaluated by flow cytometry, significantly increased three to tenfolds (p < 0.001) (Fig. 3a–c).
Effect of OxLDL, LDL and HDL on OCN surface expression in THP-1 cells. a OCN + THP1 cells were measured by flow cytometry after treatment with 40 μg/ml OxLDL ± 200 μg/ml HDL at different time points (n = 4 in each group). Three-way ANOVA for multiple comparisons: p < 0.001. Kruskal–Wallis test for pairwise comparison: *p < 0.05 vs untreated; #p < 0.05 vs OxLDL treated. b OCN + THP1 cells were measured by flow cytometry after treatment with 40 μg/ml OxLDL and different concentrations of HDL for 48 h (n = 5 in each group). Two-way ANOVA for multiple comparisons: *p < 0.001. c OCN + THP1 cells were measured by flow cytometry after 48 h treatment with 40 μg/ml OxLDL ± 200 μg/ml HDL ± 40μg/ml LDL (n = 3 in each group). Three-way ANOVA for multiple comparison: p < 0.001. *p values at the Kruskal–Wallis test for pairwise comparisons
To determine whether HDL can directly modify the expression of OCN, we incubated THP1 cells with HDL at a starting concentration of 50 μg/ml and titrated up to 400 μg/ml with and without OxLDL (Fig. 3b). HDL alone had no effects on the number of OCN+/THP1 cells. A 30% reduction in OxLDL stimulated-OCN+/THP1 cells after 48 h exposure to 50 and 100 μg/ml HDL, 40% reduction with 200 μg/ml HDL and approximately 70% reduction with 400 μg/ml (p < 0.001) were observed (Fig. 3b). Time course and dose-dependent studies showed the effect increased with incubation time and dose of HDL (Fig. 3a, b). Henceforth, stimulation experiments were performed by incubating cells for 48 h. with 200 μg/ml of HDL, a condition which mimicked human physiology [28].
To evaluate whether non-oxidized LDL may affect OCN expression, THP1 cells were incubated for 48 h with 40 μg/ml LDL with and without OxLDL and HDL (Fig. 3c). Differently from OxLDL, non-oxidized LDL did not change the expression of OCN and did not interact with HDL.
To better characterize the effect of HDL on OCN+ cells, the effect of SR-B1 inhibition was studied. As shown in Fig. 4, the number of OCN+ cells was increased by incubation with OxLDL by 9 (±2) fold and were reduced by 50.1% (±9.3%) in the presence of HDL. The addition of SR-B1 Ab at 1:800 and 1:500 decreased the effect of OxLDL by 29.8% (±9.9%) and 39.2% (±15.7%), which was similar to HDL above. Similar results were obtained using BLT-1, a small molecule inhibitor of HDL’s actions via HDL receptor SR-B1 (Fig. 4).
Inhibition of the scavenger receptor B1. Treatment of THP-1 cells with inhibitors of SR-B1–SRB1-Ab (a) and BLT1 (b)—mitigates the effects of both OxLDL and of HDL in terms of OCN+ cell as evaluated by flow cytometry. Three-way ANOVA: p < 0.001. *p values at the Kruskal–Wallis test for pairwise comparisons
The increases in OCN expression on circulating monocytes induced by OxLDL appears to be at the protein level since Ocn mRNA levels were not changed by exposure to OxLDL, LDL or HDL (Fig. 5a). However, total protein levels of OCN in monocytes were significantly increased by OxLDL and returned to baseline by the addition of HDL, while LDL alone did not affect OCN protein in monocytes (Fig. 5c). Consistent with the absence of changes in gene expression, no significant differences in the expression of the Run-related transcription factor 2 (Runx2), a major regulator of the OCN gene, was observed both at the gene and protein levels (Fig. 5b–d).
Effect of OxLDL, LDL and HDL on OCN and Runx2 gene and protein expression in THP1 cells. mRNA and protein levels were quantified after treatment with 40 μg/ml OxLDL ± 200 μg/ml HDL ± 40μg/ml LDL for 8 and 24 h (RT-PCR) or for 48 h (immunoblot). OCN (a) and Runx2 (b) mRNA levels (n = 3 for each group) did not change after 8 or 24 h incubation with OxLDL, LDL or HDL. Three-way ANOVA for multiple comparison: p > 0.05. c A representative immunoblot is shown for both OCN and Runx2 proteins. The bar graph shows the quantification of the immunoblot for OCN (n = 3 in each group). OCN protein level significantly increased after incubation with OxLDL alone, but not after incubation with OxLDL + HDL. LDL did not affect OCN levels. Three-way ANOVA for multiple comparison: p < 0.001. *p < 0.05 at the Kruskal–Wallis test for pairwise comparisons. Quantification of Runx2 expression did not show significant changes between groups (data not shown). d Nuclear Runx2 protein levels did not change after incubation with OxLDL, HDL or LDL (n = 3 in each group). Three-way ANOVA for multiple comparison: p > 0.05
Experiments were repeated using another monocyte cell line (U937). The results of the new experiments confirming those from the previous work are reported in Additional file 5: Figure S3 and Additional file 6: Figure S4.
Discussion
In this study a reduced number of OCN+ monocytes was associated with reduced prevalence of cardiovascular disease and higher HDL-c levels. In addition, data from cellular models support the clinical finding HDL significantly reduces the number of monocytes expressing OCN due to OxLDL by interacting with SR-B1, a receptor already known for interacting with HDL to effect cholesterol efflux [29]. Overall, this suggests a potential link between increased HDL-c and lowering the risk of cardiovascular disease by decreasing the expression of OCN in monocytes.
Eghbali-Fatourechi et al. reported circulating osteoblast progenitors as mononuclear circulating OCN+ cells are able to form mineralized nodules when cultured in osteoblast-differentiating medium [13]. Subsequently other investigators have confirmed that circulating mesenchymal osteoprogenitors ability to cause ectopic vascular calcification [30,31,32,33]. Monocytes have recently been described as a source of mesenchymal progenitors which can differentiate into osteoblast-like cells [8, 34] contributing to atherosclerotic calcification [14], and some reports have suggested circulating myeloid cells with osteogenic potential may affect CVD in the general population [9, 10]. Our studies extend the association of OCN+ monocytes and CVD in T1D which while having similarities with T2D also differs in that individuals with T1D develop CVD often without the typical insulin resistance hallmarks seen in T2D [15].
OCN is the most abundant non-collagenous bone matrix protein, with several functions beyond skeletal health. In particular, circulating levels of serum osteocalcin have been associated with both glucose metabolism [35,36,37] and cardiovascular disease [38, 39], but with contrasting results. As a bone-related protein, OCN is mainly produced and secreted by osteoblasts. However, different cell types involved in CVD express OCN, such as platelets, monocytes and endothelial progenitor cells [8, 40]. The presence in the bloodstream of circulating cells with an osteogenic phenotype linked to CVD supports the existence of a bone-vascular axis we have recently described also in the Medalists [22]. Therefore, further studies should be designed to clarify whether an association exists between markers of bone health (bone-turnover markers, bone mineral density, etc.) and circulating osteogenic cells.
Here we propose a mechanism which stimulates the pathological expression of OCN in circulating monocytes and a means to reverse it, with support from in vitro experiments. Accumulated OxLDL in the arterial walls may lead to vascular calcification by inducing the trans-differentiation of vascular smooth muscle cells into calcifying cells through the upregulation of Runx2, which is a major regulator of osteoblast differentiation [16, 41]. Our data show OxLDL promotes the pro-calcific phenotypic drift of monocytes as well, demonstrated by an increased number of cells expressing OCN on the cell surface. However, this does not seem related to genetic regulation as neither changes in Ocn mRNA levels nor in the expression of Runx2, the main transcription factor regulating Ocn were seen; thus suggesting other mechanisms causing a change in OCN protein levels and surface expression not accompanied by gene expression change. One possibility is protein recycling which has been associated with HDL action on monocytes [29, 42]. Alternatively, the changes observed in protein levels by immunoblot could also be due to post-translational processing of OCN regulated by HDL and OxLDL. Further studies should be performed to clarify this issue.
Consistently with the absence of relationships between LDL cholesterol levels and CD45_bright/CD14+/OCN+ cell levels in the Medalists, in vitro studies also showed non-oxidized LDL have no effect on OCN expression. However, we describe a trend towards a positive association between CD45_bright/CD14+/OCN+ circulating cell levels and small and dense LDL, but not with large LDL. This is consistent with the in vitro study as small and dense LDL represent the LDL fractions more prone to oxidation with higher atherogenic properties than LDL particles with higher size and lower density [43, 44].
Other mechanisms we did not investigate here may lead to the induction of osteogenic drift of monocytes and should be searched in future studies. Overall, it is evident that different stimuli such as hyperglycemia, dyslipidemia, chronic inflammation and hypoxia [7,8,9], all of which are pathologically elevated in people affected by diabetes, combine leading to the pro-calcific milieu contributing to the high prevalence of vascular calcification observed in people with diabetes.
Importantly, our data show both in vivo and in vitro, HDL is a relevant factor which can counteract the increased expression of OCN. The inverse relationship between OCN+ monocytes and HDL-c suggests a potential new mechanism for HDL to lower the risk for CVD. In particular the larger and intermediate sub-particles of HDL, which facilitate cholesterol efflux and are associated with lower cardiovascular risk [45,46,47], are correlated with lower levels of OCN+ cells. This supports our previous epidemiologic work demonstrating protection from CVD in the 50-Year Medalist is associated with HDL-c levels [18]. This is consistent with several other studies reporting an inverse relationship between HDL cholesterol levels and CVD in those with type 2 diabetes and those with the disease [48, 49]. However, interventional trials aimed at increasing HDL-c levels have not shown success in decreasing cardiovascular events [50], highlighting the importance of a greater mechanistic understanding of HDL-mediated cardiovascular protection. The interaction between HDL and monocytes/macrophages has always been considered a key for the maintenance of healthy vessels. Previously, this relationship was confined to HDL’s effect on cholesterol efflux and anti-inflammatory actions, preventing foam cell formation and inflammation [51]. Based on our results, we propose a new mechanism by which HDL and monocytes interact to protect from cardiovascular disease by counteracting monocytes differentiation into pro-calcific cells.
The surface receptors ATP-binding cassette A1 and C1 and SR-B1 are the main molecules mediating the action of HDL on monocytes/macrophages. Of these, SR-B1 appears to contribute both to the mechanisms of cholesterol diffusion and retro-endocytosis [29]. Our data suggests SR-B1 is also a key receptor in the regulation of OCN expression by both OxLDL and HDL, providing a potential target to reduce vascular stiffness and/or increase plaque stability.
A bias of the study may be that it was done in an older population with T1D who have a median age of 65 years. However, this is an advantage as it is a population who have reached their end-phenotype- those who will or will not develop significant CVD. The extreme phenotype provides more power with a smaller sample size. This provides added value as current knowledge about CVD in T1D is from studies conducted in the previous era of less intensive glycemic control, in those of lesser duration or extrapolated from studies in T2D [15]. Moreover, the changing epidemiology of T1D, characterized by increased longevity and longer disease duration without complications increases the need for understanding of what makes survival possible, particularly for CVD, the largest cause of mortality among this group [52]. Yet, these findings were confirmed in via in vitro experiments performed on two different types of monocyte cell lines (THP-1 and U937) and not on primary monocytes from this selected population. THP-1 and U937 cells have been widely used to investigate monocytes/macrophages pathophysiology in the cardiovascular system and it has been shown that these cell lines have features of primary monocytes derived from control human donors [53]. The absence of a control group of healthy subjects without T1D may also limit our study. However, previous studies have already widely shown that non-diabetic people have lower levels of OCN+ monocytes [7, 9, 10]. While the main mechanism of vascular damage associated to OCN+ monocytes should be ectopic calcification in the vessel wall, we acknowledge that the lack of direct measurements of vascular calcification in the Medalist cohort should be considered as a limit of this study. However, this was not the primary aim of our study as previous studies already investigated the contribution of OCN+ monocytes to vascular calcification [13, 14] and it has been widely demonstrated that vascular calcification is among the main pathological findings in T1D with CVD [15].
Conclusions
In conclusion, this study supports an association between CVD protection and lower levels of circulating osteogenic cells of myeloid origin in long duration T1D, along with higher HDL-c levels, particularly those of larger sub-particle size. Our data suggest a mechanism for the increased OCN+ monocytes due to oxidized lipids found in diabetes, and that this may be mitigated by HDL. These findings indicate that circulating OCN+ monocytes may be a marker for vascular disease in diabetic patients and may be modified by HDL elevation. Results regarding the regulation of OCN expression on monocytes by OxLDL and HDL through SR-B1 and its relationship with CVD in T1D provide new information on vascular pathophysiology. Indeed, these findings may provide new insights on the mechanism of HDL-mediated cardiovascular protection and promote advances in therapeutic strategies.
Abbreviations
- T1D:
-
type 1 diabetes
- CVD:
-
cardiovascular disease
- OCN:
-
osteocalcin
- T2D:
-
type 2 diabetes
- OxLDL:
-
oxidized low density lipoprotein
- HDL:
-
high density lipoprotein
- HDL-c:
-
high density lipoprotein cholesterol
- PBMCs:
-
peripheral blood mononuclear cells
- PBS:
-
phosphate-buffered saline
- FBS:
-
fetal bovine serum
- 7AAD:
-
7-aminoactinomycin D
- SR-BI:
-
scavenger receptor, class B, type I
- qRT-PCR:
-
quantitative real time polymerase chain reaction
- ANOVA:
-
analysis of variance
References
Morrish NJ, Wang SL, Stevens LK, Fuller JH, Keen H. Mortality and causes of death in the WHO multinational study of vascular disease in diabetes. Diabetologia. 2001;44(Suppl 2):S14–21.
Wadwa RP, Kinney GL, Ogden L, Snell-Bergeon JK, Maahs DM, Cornell E, et al. Soluble interleukin-2 receptor as a marker for progression of coronary artery calcification in type 1 diabetes. Int J Biochem Cell Biol. 2006;38:996–1003.
Lopes-Virella MF, Carter RE, Gilbert GE, Klein RL, Jaffa M, Jenkins AJ, et al. Risk factors related to inflammation and endothelial dysfunction in the DCCT/EDIC cohort and their relationship with nephropathy and macrovascular complications. Diabetes Care. 2008;31:2006–12.
Pérez A, Wägner AM, Carreras G, Giménez G, Sánchez-Quesada JL, Rigla M, et al. Prevalence and phenotypic distribution of dyslipidemia in type 1 diabetes mellitus: effect of glycemic control. Arch Intern Med. 2000;160:2756–62.
Rask-Madsen C, King GL. Vascular complications of diabetes: mechanisms of injury and protective factors. Cell Metab. 2013;17:20–33.
Hernandez SL, Gong JH, Chen L, Wu I-H, Sun JK, Keenan HA, et al. Characterization of circulating and endothelial progenitor cells in patients with extreme-duration type 1 diabetes. Diabetes Care. 2014;37:2193–201.
Fadini GP, Albiero M, Menegazzo L, Boscaro E, Agostini C, de Kreutzenberg SV, et al. Procalcific phenotypic drift of circulating progenitor cells in type 2 diabetes with coronary artery disease. Exp Diabetes Res. 2012;2012:921685.
Fadini GP. A reappraisal of the role of circulating (progenitor) cells in the pathobiology of diabetic complications. Diabetologia. 2014;57:4–15.
Fadini GP, Albiero M, Menegazzo L, Boscaro E, de Kreutzenberg SV, Agostini C, et al. Widespread increase in myeloid calcifying cells contributes to ectopic vascular calcification in type 2 diabetes. Circ Res. 2011;108:1112–21.
Collin J, Gössl M, Matsuo Y, Cilluffo RR, Flammer AJ, Loeffler D, et al. Osteogenic monocytes within the coronary circulation and their association with plaque vulnerability in patients with early atherosclerosis. Int J Cardiol. 2015;181:57–64.
Long MW, Williams JL, Mann KG. Expression of human bone-related proteins in the hematopoietic microenvironment. J Clin Investig. 1990;86:1387–95.
Otsuru S, Tamai K, Yamazaki T, Yoshikawa H, Kaneda Y. Bone marrow-derived osteoblast progenitor cells in circulating blood contribute to ectopic bone formation in mice. Biochem Biophys Res Commun. 2007;354:453–8.
Eghbali-Fatourechi GZ, Lamsam J, Fraser D, Nagel D, Riggs BL, Khosla S. Circulating osteoblast-lineage cells in humans. N Engl J Med. 2005;352:1959–66.
Albiero M, Rattazzi M, Menegazzo L, Boscaro E, Cappellari R, Pagnin E, et al. Myeloid calcifying cells promote atherosclerotic calcification via paracrine activity and allograft inflammatory factor-1 overexpression. Basic Res Cardiol. 2013;108:368.
de Ferranti SD, de Boer IH, Fonseca V, Fox CS, Golden SH, Lavie CJ, et al. Type 1 diabetes mellitus and cardiovascular disease: a scientific statement from the American Heart Association and American Diabetes Association. Diabetes Care. 2014;37:2843–63.
Yan J, Stringer SE, Hamilton A, Charlton-Menys V, Götting C, Müller B, et al. Decorin GAG synthesis and TGF-β signaling mediate Ox-LDL-induced mineralization of human vascular smooth muscle cells. Arterioscler Thromb Vasc Biol. 2011;31:608–15.
Liu L, Liu Z, Chen H, Zhang G, Kong Y, Kang X. Oxidized low-density lipoprotein and β-glycerophosphate synergistically induce endothelial progenitor cell ossification. Acta Pharmacol Sin. 2011;32:1491–7.
He ZH, D’Eon SA, Tinsley LJ, Fitzgerald S, Hastings SM, Khamaisi M, et al. Cardiovascular disease protection in long-duration type 1 diabetes and sex differences. Diabetes Care. 2015;38:e73–4.
Keenan HA, Costacou T, Sun JK, Doria A, Cavellerano J, Coney J, et al. Clinical factors associated with resistance to microvascular complications in diabetic patients of extreme disease duration: the 50-year medalist study. Diabetes Care. 2007;30:1995–7.
Keenan HA, Sun JK, Levine J, Doria A, Aiello LP, Eisenbarth G, et al. Residual insulin production and pancreatic ß-cell turnover after 50 years of diabetes: Joslin Medalist Study. Diabetes. 2010;59:2846–53.
Sun JK, Keenan HA, Cavallerano JD, Asztalos BF, Schaefer EJ, Sell DR, et al. Protection from retinopathy and other complications in patients with type 1 diabetes of extreme duration: The Joslin 50-Year Medalist Study. Diabetes Care. 2011;34:968–74.
Maddaloni E, D’Eon S, Hastings S, Tinsley LJ, Napoli N, Khamaisi M, et al. Bone health in subjects with type 1 diabetes for more than 50 years. Acta Diabetol. 2017;54:479–88.
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150:604–12.
Early Treatment Diabetic Retinopathy Study Research Group. Fundus photographic risk factors for progression of diabetic retinopathy. ETDRS report number 12. Ophthalmology. 1991;98:823–33.
Berthold HK, Rizzo M, Spenrath N, Montalto G, Krone W, Gouni-Berthold I. Effects of lipid-lowering drugs on high-density lipoprotein subclasses in healthy men—a randomized trial. PLoS ONE. 2014;9:e91565.
Oravec S, Mikl J, Gruber K, Dostal E. A non-atherogenic and atherogenic lipoprotein profile in individuals with dyslipoproteinemia. In: Lipoproteins-role in health and diseases. Rijeka: InTech; 2012.
Menegazzo L, Albiero M, Millioni R, Tolin S, Arrigoni G, Poncina N, et al. Circulating myeloid calcifying cells have antiangiogenic activity via thrombospondin-1 overexpression. FASEB J. 2013;27:4355–65.
Sloop CH, Dory L, Roheim PS. Interstitial fluid lipoproteins. J Lipid Res. 1987;28:225–37.
Röhrl C, Stangl H. HDL endocytosis and resecretion. Biochim Biophys Acta. 2013;1831:1626–33.
Gössl M, Mödder UI, Atkinson EJ, Lerman A, Khosla S. Osteocalcin expression by circulating endothelial progenitor cells in patients with coronary atherosclerosis. J Am Coll Cardiol. 2008;52:1314–25.
Flammer AJ, Gössl M, Widmer RJ, Reriani M, Lennon R, Loeffler D, et al. Osteocalcin positive CD133+/CD34−/KDR+ progenitor cells as an independent marker for unstable atherosclerosis. Eur Heart J. 2012;33:2963–9.
Pignolo RJ, Kassem M. Circulating osteogenic cells: implications for injury, repair, and regeneration. J Bone Miner Res. 2011;26:1685–93.
Fadini GP, Rattazzi M, Matsumoto T, Asahara T, Khosla S. Emerging role of circulating calcifying cells in the bone-vascular axis. Circulation. 2012;125:2772–81.
Kuwana M, Okazaki Y, Kodama H, Izumi K, Yasuoka H, Ogawa Y, et al. Human circulating CD14+ monocytes as a source of progenitors that exhibit mesenchymal cell differentiation. J Leukoc Biol. 2003;74:833–45.
Booth SL, Centi A, Smith SR, Gundberg C. The role of osteocalcin in human glucose metabolism: marker or mediator? Nat Rev Endocrinol. 2012;9:43–55.
Hwang Y-C, Jeong I-K, Ahn K-J, Chung H-Y. Circulating osteocalcin level is associated with improved glucose tolerance, insulin secretion and sensitivity independent of the plasma adiponectin level. Osteoporos Int. 2012;23:1337–42.
Maddaloni E, D’Onofrio L, Lauria A, Maurizi AR, Strollo R, Palermo A, et al. Osteocalcin levels are inversely associated with Hba1c and BMI in adult subjects with long-standing type 1 diabetes. J Endocrinol Investig. 2014;37:661–6.
Luo Y, Ma X, Hao Y, Xiong Q, Xu Y, Pan X, et al. Relationship between serum osteocalcin level and carotid intima-media thickness in a metabolically healthy Chinese population. Cardiovasc Diabetol. 2015;14:82.
Sheng L, Cao W, Cha B, Chen Z, Wang F, Liu J. Serum osteocalcin level and its association with carotid atherosclerosis in patients with type 2 diabetes. Cardiovasc Diabetol. 2013;12:22.
Foresta C, Strapazzon G, De Toni L, Fabris F, Grego F, Gerosa G, et al. Platelets express and release osteocalcin and co-localize in human calcified atherosclerotic plaques. J Thromb Haemost. 2013;11:357–65.
Taylor J, Butcher M, Zeadin M, Politano A, Shaughnessy SG. Oxidized low-density lipoprotein promotes osteoblast differentiation in primary cultures of vascular smooth muscle cells by up-regulating osterix expression in an Msx2-dependent manner. J Cell Biochem. 2011;112:581–8.
Pagler TA, Rhode S, Neuhofer A, Laggner H, Strobl W, Hinterndorfer C, et al. SR-BI-mediated high density lipoprotein (HDL) endocytosis leads to HDL resecretion facilitating cholesterol efflux. J Biol Chem. 2006;281:11193–204.
Berneis KK, Krauss RM. Metabolic origins and clinical significance of LDL heterogeneity. J Lipid Res. 2002;43:1363–79.
de Graaf J, Hak-Lemmers HL, Hectors MP, Demacker PN, Hendriks JC, Stalenhoef AF. Enhanced susceptibility to in vitro oxidation of the dense low density lipoprotein subfraction in healthy subjects. Arterioscler Thromb Vasc Biol. 1991;11:298–306.
Asztalos BF, Cupples LA, Demissie S, Horvath KV, Cox CE, Batista MC, et al. High-density lipoprotein subpopulation profile and coronary heart disease prevalence in male participants of the Framingham Offspring Study. Arterioscler Thromb Vasc Biol. 2004;24:2181–7.
Asztalos BF, Collins D, Cupples LA, Demissie S, Horvath KV, Bloomfield HE, et al. Value of high-density lipoprotein (HDL) subpopulations in predicting recurrent cardiovascular events in the veterans affairs HDL intervention trial. Arterioscler Thromb Vasc Biol. 2005;25:2185–91.
Lamon-Fava S, Herrington DM, Reboussin DM, Sherman M, Horvath KV, Cupples LA, et al. Plasma levels of HDL subpopulations and remnant lipoproteins predict the extent of angiographically-defined coronary artery disease in postmenopausal women. Arterioscler Thromb Vasc Biol. 2008;28:575–9.
Gordon T, Castelli WP, Hjortland MC, Kannel WB, Dawber TR. High density lipoprotein as a protective factor against coronary heart disease. The Framingham Study. Am J Med. 1977;62:707–14.
Gordon DJ, Probstfield JL, Garrison RJ, Neaton JD, Castelli WP, Knoke JD, et al. High-density lipoprotein cholesterol and cardiovascular disease. Four prospective American studies. Circulation. 1989;79:8–15.
Singh IM, Shishehbor MH, Ansell BJ. High-density lipoprotein as a therapeutic target: a systematic review. JAMA. 2007;298:786–98.
Yamamoto S, Narita I, Kotani K. The macrophage and its related cholesterol efflux as a HDL function index in atherosclerosis. Clin Chim Acta. 2016;457:117–22.
Tinsley LJ, Kupelian V, D’Eon SA, Pober D, Sun JK, King GL, et al. Association of glycemic control with reduced risk of large vessel disease after more than 50 years of type 1 diabetes. J Clin Endocrinol Metab. 2017. doi:10.1210/jc.2017-00589.
Qin Z. The use of THP-1 cells as a model for mimicking the function and regulation of monocytes and macrophages in the vasculature. Atherosclerosis. 2012;221:2–11.
Authors’ contributions
EM collected and analyzed data and prepared the manuscript; YX, QL, RSL and MK assisted in data collection; KP collected data and critically reviewed the manuscript; SD, LJT contributed to subject enrollment, data management and analysis; GLK contributed to study design, data interpretation, mechanistic studies and manuscript review; HAK designed the study, contributed to data analysis and wrote the manuscript. HAK had full access to all of the data in the study and had final responsibility for the decision to submit for publication. All authors read and approved the final manuscript.
Acknowledgements
We would like to thank the staff the Joslin Clinical Research Center and the 50-Year Medalists and their families.
Competing interests
The authors declare that they have no competing interests
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
The Ethic Committee on human subjects of the Joslin Diabetes Center approved the study protocol. Informed consent was obtained from all subjects prior to participation in the study.
Funding
The 50 Year Medalist Study is funded by NIDDK (P30DK036836, UL1 RR025758-03, DP3 DK094333-01), JDRF (17-2013-310), the NIDDK Diabetic Complications Consortium (DiaComp, http://www.diacomp.org), grant DK076169, the Tom Beatson, Jr Foundation and many Medalists. EM was in part supported by the Albert Renold Travel Fellowship of the European Foundations for the Study of Diabetes. The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Additional files
12933_2017_599_MOESM2_ESM.eps
Additional file 2: Figure S1. CD45_bright and CD45_bright/CD14+ PBMCs by presence of cardiovascular disease. No differences were found between Medalists with and without history of cardiovascular disease.
12933_2017_599_MOESM4_ESM.docx
Additional file 4: Table S1. Linear regression analysis for association between CD45_bright/CD14+/OCN+ (dependent variable) and different clinical and biochemical factors (independent variables).
12933_2017_599_MOESM5_ESM.eps
Additional file 5: Figure S3. OCN surface expression in U937. A. OCN+ U937 cells were measured by flow cytometry after 48 h treatment with 40 μg/ml OxLDL ± 200 μg/ml HDL ± 40μg/ml LDL (n = 3 in each group). Three-way ANOVA for multiple comparison: p < 0.001. *p < 0.05 at the Kruskal–Wallis test for pairwise comparisons. B and C. Treatment of U937 cells with inhibitors of SR-B1–SRB1-Ab (B) and BLT1 (C)—mitigates the effects of both OxLDL and of HDL in terms of OCN+ cell as evaluated by flow cytometry. Three-way ANOVA: p < 0.001. *p values at the Kruskal–Wallis test for pairwise comparisons.
12933_2017_599_MOESM6_ESM.eps
Additional file 6: Figure S4. OCN and Runx2 gene and protein expression in U937 cells. A, B. OCN and Runx2 mRNA levels (n = 3 for each group). Three-way ANOVA for multiple comparison: p > 0.05. C. A representative immunoblot is shown for both OCN and Runx2 proteins. The bar graph shows the quantification of the immunoblot for OCN (n = 3 in each group). OCN protein level significantly increases after incubation with OxLDL alone, but not after incubation with OxLDL + HDL. Three-way ANOVA for multiple comparison: p < 0.001. *p < 0.05 at the Kruskal–Wallis test for pairwise comparisons. Quantification of Runx2 expression did not show significant changes between groups (data not shown). D. Nuclear Runx2 protein levels does not change after incubation with OxLDL, HDL or LDL (n = 3 in each group). Three-way ANOVA for multiple comparison: p > 0.05.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Maddaloni, E., Xia, Y., Park, K. et al. High density lipoprotein modulates osteocalcin expression in circulating monocytes: a potential protective mechanism for cardiovascular disease in type 1 diabetes. Cardiovasc Diabetol 16, 116 (2017). https://doi.org/10.1186/s12933-017-0599-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-017-0599-2