Abstract
Background
Substantial improvements have been observed in coverage and access to maternal health services in Ethiopia. However, the quality of care has been lagging behind. Therefore, this study aimed to assess the level of quality of Option B+ PMTCT in Northern Ethiopia.
Methods
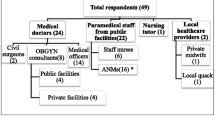
A facility based survey was conducted from February to April 2016 in Northern Ethiopia. Twelve health facilities were enrolled in the study. Mixed method approach was used in line with Donabedian (Input- Process-Output) service quality assessment model. Data of 168 HIV positive mothers & their infant were abstracted from registers, and follow up charts. During the Option B+ service consultation, a total of 60 sessions were involved for direct observation. Of which, 30 clients and 12 service providers were subjected for exit and in-depth interview respectively. Facilities were categorized rendering good service quality based on predetermined quality judgment criteria. Reasons of good and bad service quality were thematically fitted with each quality component based on emerging themes (TM1-TM3), and categories (CA1-CA6).
Results
Of the total 12 study health facilities, 2(16.7%) were achieved the desired level of service quality based on the three quality components. The input quality was better and judged as good in 33.3% health facilities. However; process and output service quality were realized in one - fourth of them.
Conclusion
Insignificant numbers of facilities fulfilled the aspired level of service quality. Quality of care was found influenced by multiple inputs, processes, and output related barriers and facilitators. Comprehensive Program monitoring is needed based on three quality components to improve the overall service quality.
Similar content being viewed by others
Background
Globally, Mother to Child Transmission (MTCT) of HIV accounts for 90% of new pediatric HIV infection worldwide. Sub-Saharan Africa experienced the greatest share [1]. In order to increase the likelihood of children being born free from HIV, World Health Organization (WHO) had been implementing different strategies (Option A, Option B, Option B+) for optimizing PMTCT care and support for low and middle income countries since 2001 [2]. Under Option A, women receive antepartum (starting at 14 weeks of gestation) and intrapartum ARV prophylaxis to reduce the risk of drug resistance. Meanwhile, women receive triple ARVs starting as early as 14 weeks of gestation and this is continued through childbirth if not breastfeeding or until one week after the cessation of breastfeeding in cases of Option B+ in MNCH Platform [2, 3].
During PMTCT scale up period (Option A, & B), significant achievements were obtained in rolling back new pediatric HIV infection by 70% [3]. Nevertheless; programmatic, clinical, and other operational challenges were reminded that lead high attrition and lost to follow up of HIV positive pregnant and lactating women from HIV chronic care. In 2010, an estimated 23% of HIV positive women lost to follow up and nearly 150,000 new pediatric HIV infections were reported worldwide [1,2,3]. Besides, fewer than 20% of HIV infected pregnant women received any PMTCT intervention and as many as 14% of infants bore from HIV infected women were tested positive for HIV in Malawi [4]. The high attrition rate of HIV positive women from HIV chronic care was reported from Sub-Saharan Africa (28%) and Cameroon (24.3%) [3,4,5].
It had been a great challenge in Ethiopia in which only 10% of HIV positive pregnant and lactating women complete PMTCT program until infant HIV confirmatory testing at 18 months of age [6]. In the early 2013, a third option (Option B+) has advocated to provide lifelong first line regimen of tenofovir/lamivudine/efavirenz (TDF/3TC/EFV) to all HIV infected pregnant and lactating women regardless of CD4 cell count [7]. This new alternative approach has programmatic and clinical advantage in which it is fully integrated in to MNCH platforms, test and treat strategy regardless of CD4 count that could accelerate progress towards eliminating new pediatric HIV infections [8]. This programmatic update also emphasized additional advantages such as providing better protection for maternal health and reduction in sexual transmission of HIV [7, 8].
Option B+ was first conceived and implemented in Malawi. Preliminary findings of routine Option B+ PMTCT programme in a rural district in Malawi showed a fivefold increase in ART initiation and 88% client retention in the first quarter of its implementation in 2011 [9,10,11].
In Ethiopia, it was rolled out in the early 2013 as an MTCT elimination strategy in 2020 [12, 13]. However; only 60.6% of HIV positive pregnant and lactating women were enrolled to HIV chronic care in 2015 [13]. Mothers were still faced a challenge to retain in the service. As evidenced from North East Ethiopia, 16% LTF was documented in which 11.9% was reported at 6 months, 15.7% at 12 months and 22.6% at 24 months follow up period [14]. Similar evidence was reported from Eastern Ethiopia in which LTF was 9.8 and 14.8% at 6 and 12 months respectively [15]. Facility based studies revealed that poor service quality was the main challenge. As an input quality item, some health facilities were made operational with supply chain related problems. Besides, inadequacy of trained human resource was an input related barrier that renders service quality [13, 16]. The lack of service integration, poor adherence to service standards, prolonged waiting time, and confidentiality issues were factors that affect process service quality [16,17,18].
Improving service quality of Maternal and Child Health services including Option B+ was a priority agenda in the Health Sector Transformation Plan (HSTP) of Ethiopia to achieve the three 90’s (90–90-90) in 2020 [13]. The barriers reported that affect quality service in the previous studies were input-process-output related factors. As a result, we preferred to use Donabedian model of quality assessment framework to evaluate the service quality [19]. National technical guideline to ensure the provision of Option B+ was also developed based on the three quality components as depicted in the figure (Fig. 1) [20, 21]. Therefore, this study aimed to assess the level of quality of Option B+PMTCT service provision in public health facilities in Mekelle Zone, Northern Ethiopia using Donabedian Model.
Methods
Aim
The study aimed to assess the level of quality of OptionB+PMTCT and to explore reasons for good and bad service quality.
Study design and settings
This study was a facility based cross-sectional survey conducted between February to April 2016. Mixed method approach was used involving both quantitative and qualitative data collection methods. Donabedian model was used [19] as depicted in the figure below (Fig. 1).
The study was conducted in Mekelle zone, Tigray of Northern Ethiopia, 802KMs from Addis Ababa, the capital city of Ethiopia. It is among the top three high HIV prevalence areas in Tigray region [22]. According to the projected national census in 2018 [23], the total population was projected to 320,000. A total of 12 health facilities have been provided Option B+ under MNCH continuum of care. Of which three of them were in hospitals.
Sampling and sample size determination
All health facilities (nine health centers and three hospitals) providing Option B+ under MNCH platforms were involved in the study. Study participants were HIV positive mother & their infants. They were newly diagnosed women and enrolled under Option B+ package aiming “test and treat” strategy. Besides, who were under continuous follow up for more than one year prior to data collection in MNCH clinic for the purpose of complete clinical history. To come up with the final sample, review of all patient records and follow up charts were conducted which fulfilled predetermined eligibility criteria. First, a total of 219 HIV positive mother & infant pairs were reviewed. However, 48 study participants were excluded since they were transferred from other facilities and did not have a complete clinical history. Similarly, three newly diagnosed HIV positive women spent only six months in HIV chronic care were not included in the study. Hence, the total participants enrolled for the study were 168.
Convenience sampling method was used to recruit participants for qualitative study, until information saturation was obtained [24]. Observation and interviews were conducted during & after service consultation. A total of 60 sessions were involved for direct observation. Of which, 30 HIV positive women and 12 service providers were subjected for exit and in-depth interview respectively to identify reasons for good and bad service quality in respective quality components. Health workers have been providing Option B + PMTCT in MNCH clinic for more than one year were included in the study.
Data collection and measurements
Quantitative data
Quantitative data were collected by four midwives and master’s level supervisor who had an experience in public health data collection.
Input service quality
For input quality, 47 indicators were adopted from the national guidelines [20, 21]. Facility inventory was conducted to ensure the availability of essential equipments, drugs and supplies. See list of input quality verification variables (Additional file 1).
Process service quality
A total of 43 process related indicators were articulated for assessing process quality [16, 17, 25]. Non-participant observation was conducted using a checklist to observe service adheres to standard practices. The intention was to observe 10 sessions from each facility during each round of data collection. However, this was not possible since too few women came for Option B+PMTCT services during the data collection period; indeed, 60 clients in which five for each facility were participated. In addition, some process related variables were obtained from recorded review. See list of process quality verification variables (Additional file 1).
Output service quality
Output quality was assessed using 13 items adopted from national guideline [20, 21]. Data were abstracted retrospectively from logbooks and/or records and individual medical records for 168 mother infant pairs using a data abstraction tool. Besides, 12 HIV exposed infant follow up charts were reviewed about the utilization of the Option B+ service package in MNCH clinic. Confidentiality around patient records was protected; communication was made with only authorized person. Patient codes were used and documents were locked. See list of output quality verification variables (Additional file 1).
Overall service quality was assessed by combining input, process, and output service quality items. Facilities were categorized rendering good input service quality, if the average weighted score of input quality performance standards is 100% [10], and 90% or more for process, output, and overall quality performance standards [10, 20]. See the score of each variable for respective quality components (Additional file 1).
Qualitative data
Qualitative data collection was guided by principal investigator (corresponding author) who had an experience on qualitative data collection. Both interviews were conducted in Tigrigna (local language), and audio recording was involved.
Exit -interviews (EI)
Exit interviews were conducted with mothers who were provided oral consents for participation at the end of service consultation. After 30 interviews were involved with clients, information saturation was obtained; no further interviews were conducted since no new information was being generated. Interviews were guided by using a pre-tested flexible interview guide with probes to identify client views on service utilization. Interviews were lasted within the range of 30–40 min.
Key informant interview (KII)
In-depth interviews were held by appointment with service providers during the study. Twelve key informant interviews were conducted until information saturation was obtained. The interviews were guided by using a pre-tested, flexible interview guide with probes to identify their role in providing PMTCT services and reasons for good and bad service quality. Interviews were lasted within 15–25 min.
Data quality assurance
To enhance data quality, training was provided for data collectors and supervisor with the objective of the study, the nature of the data collection tools, and ways of approaching during interview, observe, record and chart review. During the data collection period there was a strict supervision scheme. Completed questionnaires were checked on a daily basis by supervisor and principal investigator.
Data management and analysis
Quantitative data were coded, cleaned, and entered into EPI info version 7 and then exported and analyzed using SPSS version 21 software. Univariate data analysis was conducted to estimate the prevalence of variables for respective quality components. The Findings were presented in tables (Tables 1, 2, 3 and 4) and figure (Fig. 2).
Summary of Option B + PMTCT service quality in studied health facilities in Mekelle Zone, Northern Ethiopia. [Note: (0/3): number of facilities not achieved any of the three quality components; (1/3): number of facilities achieved any one of the three quality components; (2/3): number of facilities achieved two of the three quality components; (3/3): number of facilities achieved all three quality components]
Qualitative data were analyzed manually using the content thematic approach [24]. Data analysis was done by the first author in collaboration with a second author (experienced qualitative researcher). This involved reading script several times, translating transcripts from local language (Tigrigna) to English, identifying themes (TM1-TM3 …) and categories (CA1-CA6). The main study themes were fitted with three quality components, whilst categories were motivators and barriers for good and bad service quality in each identified themes. All authors were involved in discussions of study themes, & categories. This process facilitated researcher triangulation. Direct quotations were presented reflecting reasons for good and bad service quality.
Operational definitions
Input dimension: this dimension was used to assess the availability of human resources, materials, drugs, equipment, and supplies needed for Option B+ PMTCT service provision [17].
Process dimension: this dimension used to reflect how service providers adhere to service standards during a service consultation of Option B+PMTCT service in MNCH unit [18].
Output dimension: used to evaluate the ultimate service result of Option B+PMTCT service and patient satisfaction level [17].
Overall quality: this particular dimension was determined by combining predetermined three quality components; input, process, and output [25].
DBS result turnaround time: The date for DBS sample collection from HIV-exposed infants to the date when HIV screening results was arrived at health facility [26].
Results
The study was assessed based on Donabedian input-process-output service quality assessment model. A total of 12 health facilities (9 health centers and 3 hospitals) were included which has been providing Option B+PMTCT under MNCH continuum of care.
Quantitative component
Overall service quality
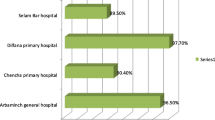
The study showed that the overall level of service quality of Option B+PMTCT was rendered as good in one out of six(16.7%) of studied health facilities. Specifically, input service quality was judged as good in 33.3% of health facilities, but only 25% of them realized good process and output service quality respectively (Fig. 2).
Input service quality
Regarding input service quality, the study revealed that the majority of the health facilities were equipped with clinical care supplies and drugs for Option B+PMTCT service provision. Long life ARV regimen (TDF + 3TC + EFV), and other basic obstetric care supplies for Option B+ were not reported as stock out for the past one year (additional file one). However; critical input related items for the Option B+ service provision were missed in considerable no of studied health facilities. Only, half of the health facilities kept on hand the necessary trained service providers, drugs for opportunistic infections, and DBS test kits necessary for the desired input service quality (Table 1).
Process service quality
With regards to process quality, some prominent key interventions had been missed during service consultation. Option B+ ARV drug adherence counseling and partner notification were offered in 58.3% of the health facilities. The women were greeted on arrival only in 58.3% of the health facilities which had an impact on poor quality service. Prolonged waiting time was also an issue observed during a service consultation [10]. It had been noted that health service providers in the majority of health facilities were observed not adhered to service standards while providing service consultation (Table 2).
Output service quality
As an Option B + PMTCT service output, majority; 91.7% of mother infant pair were alive and in their first line recommended treatment regimen in the past one year. However; high DBS result turnaround time and low patient satisfaction level were vital issues which needed great attention while the service has been provided (Table 3).
Qualitative component
Input service quality (TM1)
Reason for good input service quality (CA1) (Table 4)
The majority of service providers recognized that building team work among program directors and district level experts enabled them to identify availability related factors on time. This is an identified contributing facilitator for facilities to be judged providing good input service quality (Fig. 2). This was illustrated clearly by the following service provider:
“ … ...we have been conducted weekly meetings with program managers and district level experts with availability related factors and prepare an action plan to resolve input related constraints on time”(PMTCT service provider ≠12 ).
Reasons for bad input service quality (CA2) (Table 4)
Health workers expressed their opinion on shortage of trained human workforce and supply chain issues for Option B+ as a barrier for input related factor. Sometimes, trained staffs were also preferred to serve health care services other than MNCH unit as described below:
“ … …Imagine only two health care providers trained on Option B+and serving more than an average of 80 clients per day. Having this reality, how can we provide quality? Therefore, without allocating an appropriate number of trained health care providers , only integrating the service to MNCH unit may not be successful” (PMTCT service provider ≠4). This finding is consistent with quantitative evidence summarized in (Table 1).
“ … …Some drug list used for opportunistic infection such as co-trimoxazole prophylactic therapy was reported as stock out for more than six months in the past year lack of transportation was a reason given to us when requested”(PMTCT service provider≠8 ).
Process service quality (TM2) (Table 4)
Reasons for good process service quality (CA3) (Table 4)
Task shifting to scale up Option B+ by integrating the delivery of Option B+ ART initiation as one service packages in MNCH unit, initiation of ARV regardless of CD4 count, and simplicity of ARV regimen was greatly appreciated by majority of service providers and clients during an interview:
“ … ...discrimination is not my concern for the past two years after the adoption of Option B+. I am confident enough to attend my follow up visit together with HIV negative mothers in MNCH clinic. This is because; we all received our follow up care in one room and with the same health professionals” (PMTCT client ≠ 18).
“… … Before the introduction of Option B+PMTCT high lost (3%) and dropout rate (4%) was documented in our facility. The main reason forwarded by the majority of the clients was repeated appointments for CD4 count for ART initiation but after its adoption, patient high patient retention was documented”(PMTCT service provider ≠ 2).
“ … ...the drug provided for me during PMTCT visit was comfortable and easy to use. I selected a fixed time at 7:00 PM and I am taking the drug usually with a specified time and I don’t want to miss even a fraction of seconds”(PMTCT client≠ 21).
“ … …During the time of Option A and B, multiple ARV drugs were prescribed and patients were complaining about the situation, but now patient were easily adhered to the regimen and no more need of continuous adherence support”(PMTCT service provider ≠5).
Reasons for bad process service quality (CA4) (Table 4)
The majority of service providers had good experience regarding Option B+. However, one health care provider reported her experience of considering CD4 count as criteria for initiating ART which resulted poor service compliance with service standards. Some other providers criticized its integration as creating workload and prolonged waiting time as described as follows:
“… ...I am not aware of prescribing ARV drugs regardless of CD4 count and I appointed two PMTCT clients for CD4 investigation before prescribing the drug”(PMTCT service provider ≠10 ).
“… ...before the introduction of the Option B+mother living with HIV were under follow up at ART clinic but now they had been enrolled in the MNCH clinic during their maternal and child health care visit which resulted additional work load in our health facility”(PMTCT service provide≠3).
“… ...my great concern during my PMTCT follow up visit was an issue of timing to get the service on time since there was delayed service as a result, I have been thinking to miss the opportunity”(PMTCT client ≠19).
Output service quality (TM3) (Table 4)
Reasons for good output service quality (CA5) (Table 4)
As described by majority of service providers, client’s belief in the efficacy of ARVs, absence of stigma and discrimination were facilitators for high patient retention as articulated below:
“… ...before the introduction of option B+high patient lost and drop out were documented but now Option B+was highly accepted by patents”(PMTCT service provide≠5).
Reasons for bad output service quality (CA6) (Table 4)
Big issue forwarded by almost all participants was high turnaround time for DNAPCR virological test result communication which was arrived within 4–6 months time period of the health facility from the central testing unit that can hinder the success of early infant diagnosis as explained below:
“… ...I am always worried regarding delay of my new borne baby’s HIV virological test result. As you have seen, am receiving exposed infant test result today after six months. Unfortunately, I am very much happy today since his result non-reactive. But the past six months were painful for me”(PMTCT client ≠28).
“… ...I am always communicating using mobile phone with laboratory experts in the central testing unit an issue of DBS result delay but they told me that the machine was under maintenance” (PMTCT service provider≠ 7).
Discussion
The primary aim of this study was to evaluate the level of quality of option B+PMTCT and to explore factors for good and bad service quality in Mekelle Zone of Northern Ethiopia. The evaluation was conducted based on three quality components suggested in the Donabedian model and under the umbrella of the national guidelines for Option B+PMTCT service provision in Ethiopia [20, 21].
Accordingly, the study result showed that the overall level of service quality of Option B+PMTCT was rendered as good in one out of six(16.7%) of studied health facilities. Specifically, 33.3% were judged as providing good in terms of input quality but only 25% for the process and output service quality respectively. However, it’s important to note that the three quality components are interlinked to each other and the effect of one component had its own impact on the other [19].
This finding was by far from pre-determined national target in 2020 [13] and evidences from Southern Ethiopia [16, 27]. The reason for such discrepancies might be due to the stretched nature of the second health sector transformation plan and methodological difference in which only client interview was conducted to assess client satisfaction in the latter two studies.
Regarding input quality, it was found better provided than its counterparts. The study showed that only, 33.3% of the studied health facilities had the necessary inputs to provide quality delivery service. It was relatively lower when compared to some other African countries [9, 28, 29]. This discrepancy might be due to variation in national guideline and performance targets that lead to variation in service quality. However, the study revealed the finding was almost consistent with a report from Northern and South West Ethiopia [18, 25]. From the qualitative finding, absence of continuous and timely inventory of resources at facility level lead shortage of input related resources as described by key informants from Southern parts of Ethiopia [27]. This had an impact primarily on input quality [19].
The study also revealed that only one fourth of the study health facilities fulfilled service adherence to process related service delivery of Option B+ according to the national guideline. This finding was comparable with evidence from Northern and South West Ethiopia [18, 25]. But lower when compared with evidence from Malawi [30]. A variation of the finding in the latter study might be due to their good experience in implementing the service since it was an area in which Option B+PMTCT first piloted internationally [9]. Identified barriers for process related factors during an interview were poor service adherence to service standards, work load, and prolonged waiting time which were similarly reported from [27, 31, 32]. This process related factors had serious implications in compromising the overall quality of care currently aspired in 2020 [13, 19].
Similar to process quality, the study showed good service quality was archived in one fourth of the studied health facilities in terms of service utilization and satisfaction of mothers for Option B+PMTCT. Patient satisfaction is one of the desired items in the measure of output service quality [19]. The overall client satisfaction about the service was reported low (58.3%) which had an impact on service output quality. Qualitative finding suggested that high turnaround time for DBS result communication and prolonged waiting time to get the service genuinely forecasted that significantly affect service output. This finding seems very plausible and significantly associated with other evidences [33,34,35,36].
Conclusions
The study revealed that health facilities that achieved the aspired level of service quality were insignificant in number. Only, 16.7% of study health facilities fulfilled the desired level of quality based on predetermined quality judgment criteria in each quality components. To realize the current aspired level of service quality in the country’s health sector transformation plan, comprehensive program monitoring is needed based on three quality components in line with identified reasons for good and bad service quality to improve the overall service quality. This was due to their interrelated effect of one another [19]. Good partnership, service integration, ART initiation regardless of CD4 count, simplicity of ART regimen were facilitators positively influencing the quality of care; whilst, resource constraints, poor service compliance, prolonged waiting time, workload,and high DBS result turnaround time were barriers negatively affecting the service quality.
Study limitations
The model used in this study had its own drawbacks that considered only linear assumption that do not infer casual relationships. In measuring process quality, overestimations of findings could happen due to either Hawthorn or social desirability biases during service observations. Use of small sample size may affect finding generalizablity but in process evaluation generazablity is not an issue. In addition, the rigor statistical test was not done since it was program based process evaluation and use of sophisticated statistical analysis is not a must unlike outcome evaluation [37].
Availability of data and materials
The datasets generated and analyzed during the current study were not publicly available due to the nature of sensitive data on HIV/AIDS and confidentiality issues. The data can be available upon reasonable request to the corresponding author.
Abbreviations
- MTCT:
-
Mother to Child Transmission
- DBS:
-
Dried blood spot test
- PCR:
-
Polymeric Chain Reaction
- HIV:
-
Human -Immune -Virus
- MNCH:
-
Maternal, Neonatal, and Child Health
- ART:
-
Antiretroviral Therapy
- ARV:
-
Antiretroviral Medication
- PMTCT:
-
Prevention of Mother-to-Child Transmission
- WHO:
-
World Health Organization
- KII:
-
Key Informant Interview
- TM:
-
Themes
- CA:
-
Categories
References
UNAIDS. Children and HIV. Factsheet July 2016. Joint United Nations Programme on HIV/AIDS (UNAIDS), Geneva, Switzerland; 2016; 2016. Availablefrom:http://www.unaids.org/sites/default/files/media_asset/FactSheet_Children_en.pdf.
World Health Organization. Towards universal access: scaling up of HIVAIDS intervention in the health sector. Geneva: WHO; 2016.
World Health Organization. Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection: Recommendations for a public health approach. Geneva: World Health Organization; 2013.
Van Lettow M, Bedell R, Landes M, et al. Update and outcomes of a prevention-of-mother-to-child (PMTCT) program in Zomba District. Malawi BMC Public Health. 2011;11:426.
Sama C-B, Feteh VF, Tindong M, Tanyi JT, Bihle NM, Angwafo FF III. Prevalence of maternal HIV infection and knowledge on mother–to–child transmission of HIV and its prevention among antenatal care attendees in a rural area in Northwest Cameroon. PLoS One. 2017;12(2):e0172102. https://doi.org/10.1371/journal.pone.0172102.
Moges NA, Kassa GM, Boneya DJ. Rate of HIV transmission and associated factors among HIV-exposed infants in selected health facilities of East and West Gojjam Zones, Northwest Ethiopia; retrospective cohort study. BMC Infect Dis. 2017; 17(1):475. Published 2017 Jul 6. Doi: https://doi.org/10.1186/s12879-017-2578-3.
Van Lettow M, Bedell R, Landes M, et al. Uptake and outcomes of a prevention-of mother-to-child transmission (PMTCT) program in Zomba district, Malawi. BMC Public Health. 2011;11:426. https://doi.org/10.1186/1471-2458-11-426.
United Nations Children's Fund. Key considerations for countries to implement an equity-focused approach: eliminating new HIV infections among children and keeping mothers living with HIV alive and well. UNICEF; 2012. Available at: http://www.unicef.org/aids/files/hiv_Key_considerations_options_B.pdf (accessed 29 Nov 2013).
Kalua T, Tippett Barr BA, van Oosterhout JJ, et al. Lessons Learned from Option B+ in the Evolution Toward "Test and Start" From Malawi, Cameroon, and the United Republic of Tanzania. J Acquire Immune Defic Syndr. 2017;75 Suppl 1(Suppl 1):S43–50. https://doi.org/10.1097/QAI.0000000000001326.
Tweya H, Keiser O, Haas AD, et al. Comparative cost-effectiveness of Option B+ for prevention of mother-to-child transmission of HIV in Malawi. AIDS (London, England). 2016;30(6):953–62. https://doi.org/10.1097/QAD.0000000000001009.
Hoffman RM, et al. Factors associated with retention in Option B+ in Malawi: a case control study. Journal of the International AIDS Society. 2017;20(1):21464. https://doi.org/10.7448/IAS.20.01.21464.
Ethiopian Federal Ministry of Health. National Comprehensive PMTCT training participants manual. Adama. Ethiopia: MNCH Directorate; 2016..
FMOH. Health sector transformation plan (HSTP) 2015/16–2019/20. Addis Ababa, Ethiopia: Federal Ministry of Health; 2015.
Mitiku I, et al. Factors associated with loss to follow-up among women in Option B+ PMTCT programme in northeast Ethiopia: a retrospective cohort study. Journal of the International AIDS Society. 2016;19(1) Gale Academic OneFile, Accessed 12 May 2020.
Seifu W, Ali W, Meresa B. Predictors of loss to follow up among adult clients attending antiretroviral treatment at Karamara general hospital, Jigjiga town, eastern Ethiopia, 2015: a retrospective cohort study. BMC Infect Dis. 2018;18:280. https://doi.org/10.1186/s12879-018-3188-4.
Bachore BB, Tafese F, Gebissa F, Mekango DE. Quality of prevention of mother to child transmission (PMTCT) of HIV Services in Public Hospitals of Hadiya zone, southern Ethiopia. Health Syst Policy Res. 2018;5(2):73.
Abaynew Y. Quality of prevention of mother to child transmission (PMTCT) Services in Dessie Referral Hospital, Dessie City Administration, Ethiopia: client perspective. Neonatal Pediatric Med. 2016;3:123. https://doi.org/10.4172/2572-4983.1000123.
Bayou NB, Tsehay YE. Quality of PMTCT Services in Gebretsadiq Shawo Memorial Hospital, Kafa zone, south West Ethiopia: a descriptive study. Open Access Library J. 2015;2:e1499. https://doi.org/10.4236/oalib.1101499.
Donabedian A. The quality of care: how can it be assessed? J Am Med Assoc. 1988;260:17431748. https://doi.org/10.1001/jama.1988.03410120089033.
Federal Democratic Republic of Ethiopia Ministry of Health (FDRE MOH). National guidelines for Prevention of Mother-to – Child Transmission of HIV in Ethiopia. Addis Ababa: FMOH; 2007. accessed in https://www.ilo.org/wcmsp5/groups/public/-ed_protect/-protrav/-ilo_aids/documents/legaldocument/wcms_125389.pdf.
Federal Democratic Republic of Ethiopia Ministry of Health (FDRE MOH). National guidelines for comprehensive HIV prevention, care and treatment. Addis Ababa: FMOH; 2013. accessed in https://aidsfree.usaid.gov/sites/default/files/ethiopia_natl_gl_2014.pdf.
Tigary Regional Health Bureau. Annual health profile. Northern Ethiopia: Tigray; 2007.
ECSA (2018). Ethiopian household consumption expenditure (HCE) survey statically reportfile:///C:/users/THRI/downloads/HCE%202016%20Statistical20Report20Tigray%20region.Pdf.
Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004 Feb;24(2):105–12. https://doi.org/10.1016/j.nedt.2003.10.001.
Fissha G, Birhane Y, Worku A, Terfe W. Quality of the delivery services in health facilities in Northern Ethiopia. BMC Health Serv Res. 2017;17(1):187. https://doi.org/10.1186/s12913-017-2125-3.
Wondafrash B, Hiko D. Dried blood spot test for HIV exposed infants and children and their anti-retro viral treatment status in selected hospitals in Ethiopia. Ethiop J Health Sci. 2016;26(1):17–24. https://doi.org/10.4314/ejhs.v26i1.5.
Tesfaye DJ, Hibistu DT, Abebo TA, et al. Option B plus antiretroviral therapy adherence and associated factors among HIV positive pregnant women in southern Ethiopia. BMC Pregnancy Childbirth. 2019;19:82. https://doi.org/10.1186/s12884-019-2228-4.
Kim YM, Chilila M, Shasulwe H, et al. Evaluation of a quality improvement intervention to prevent mother-to-child transmission of HIV (PMTCT) at Zambia defence force facilities. BMC Health Serv Res. 2013;13:345. Published 2013 Sep 8. https://doi.org/10.1186/1472-6963-13-345.
Rosenberg NE, Pettifor AE. Taking Malawi's option B+ programme from a B+ to an a. Lancet HIV. 2018;5(12):e672–3. https://doi.org/10.1016/S2352-3018(18)30320-5.
Herce ME, et al. Supporting Option B+ scale up and strengthening the prevention of mother-to-child transmission cascade in central Malawi: results from a serial cross-sectional study. BMC infectious diseases. 2015;15:328. https://doi.org/10.1186/s12879-015-1065-y.
DiCarlo AL, Gachuhi AB, Mthethwa-Hleta S, et al. Healthcare worker experiences with option B+ for prevention of mother-to-child HIV transmission in eSwatini: findings from a two-year follow-up study. BMC Health Serv Res. 2019;19:210. https://doi.org/10.1186/s12913-019-3997-1.
Sanga ES, Mukumbang FC, Mushi AK, et al. Understanding factors influencing linkage to HIV care in a rural setting, Mbeya, Tanzania: qualitative findings of a mixed methods study. BMC Public Health. 2019;19:383. https://doi.org/10.1186/s12889-019-6691.
Girum T, Wasie A, Worku A. Trend of HIV/AIDS for the last 26 years and predicting achievement of the 90–90-90 HIV prevention targets by 2020 in Ethiopia: a time series analysis. BMC Infect Dis. 2018;18:320. https://doi.org/10.1186/s12879-018-3214-6.
Bernhart MH, Wiadnyana IG, Wihardjo H, Pohan I. Patient satisfaction in developing countries. Soc Sci Med. 1999;48:989–96. https://doi.org/10.1016/S0277-9536(98)00376-1.
Westaway MS, Rheeder P, Van Zyl DG, Seager JR. Interpersonal and organizational dimensions of patient satisfaction: the moderating effects of health status. Int J Qual Health Care. 2003;15:337–44. https://doi.org/10.1093/intqhc/mzg042.
Andaleeb, S.S.: Service Quality Perceptions and Patient Satisfaction: A Study of Hospitals in Developing Coun- N. B. Bayou, Y. E. Tsehay OALibJ | DOI:https://doi.org/10.4236/oalib.1101499 10 May 2015 | Volume 2 | e1499 tries. Social Science & Medicine, 52, 1359–1370. https://doi.org/10.1016/S0277-9536(00)00235-5.
Moore G, Audrey S, Barker M, et al. Process evaluation in complex public health intervention studies: the need for guidance. J Epidemiol Community Health. 2014;68(2):101–2.
Acknowledgments
The authors would like to thank the Tigray Regional Health Bureau, Mekelle University School of Public Health, and the study team for their support and contribution to the study. The authors are also grateful to the study participants.
Funding
The study was funded by Mekelle University School of Public Health. Additional funding also allocated from the Tigray Regional Health Bureau. The funders had no role in the study design, data collection, and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
KF and AD designed the study; KF developed the protocol, analyzed data, interpret data, and preparing the first draft of the manuscript. All authors were involved in revising and approving the final version of the manuscript.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
The study was approved by Mekelle University Institutional Review Board (MUIRB) (MUEB/2016). Verbal informed consent was approved by the ethics committee since majority of study participants were unable to read and write. Based on the ERB recommendation, oral consents were documented by obtaining signatures from MCH focal person with the assurance of confidentiality.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1.
Excel files showing the detail scores for the three quality components.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ajemu, K.F., Desta, A. Level of quality of option B+PMTCT service provision in public health facilities in Mekelle zone, northern Ethiopia: cross-sectional study. BMC Health Serv Res 20, 547 (2020). https://doi.org/10.1186/s12913-020-05429-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-020-05429-6