Abstract
Background
Domestic violence and abuse (DVA) is experienced by about 1/3 of women globally and remains a major health concern worldwide. IRIS (Identification and Referral to Improve Safety of women affected by DVA) is a complex, system-level, training and support programme, designed to improve the primary healthcare response to DVA. Following a successful trial in England, since 2011 IRIS has been implemented in eleven London boroughs. In two boroughs the service was disrupted temporarily. This study evaluates the impact of that service disruption.
Methods
We used anonymised data on daily referrals received by DVA service providers from general practices in two IRIS implementation boroughs that had service disruption for a period of time (six and three months). In line with previous work we refer to these as boroughs B and C. The primary outcome was the number of daily referrals received by the DVA service provider across each borough over 48 months (March 2013–April 2017) in borough B and 42 months (October 2013–April 2017) in borough C. The data were analysed using interrupted-time series, non-linear regression with sensitivity analyses exploring different regression models. Incidence Rate Ratio (IRR), 95% confidence intervals and p-values associated with the disruption were reported for each borough.
Results
A mixed-effects negative binomial regression was the best fit model to the data. In borough B, the disruption, lasted for about six months, reducing the referral rate significantly (p = 0.006) by about 70% (95%CI = (23,87%)). In borough C, the three-month service disruption, also significantly (p = 0.005), reduced the referral rate by about 49% (95% CI = (18,68%)).
Conclusions
Disrupting the IRIS service substantially reduced the rate of referrals to DVA service providers. Our findings are evidence in favour of continuous funding and staffing of IRIS as a system level programme.
Similar content being viewed by others
Background
Domestic violence and abuse (DVA) includes threatening behaviour, violence or psychological, physical, sexual, financial, or emotional abuse between adults that are relatives, partners or ex-partners [1]. DVA is a violation of human rights with long term damage to health, experienced by one third of women globally [2]. In England and Wales an estimated 2 million women aged 16 to 59 years have experienced DVA in the year ending March 2018 with on average two women killed by their partner or ex-partner every week [3]. In addition to physical effects, women affected by DVA can also suffer chronic health problems including gynaecological problems, gastrointestinal disorders, neurological symptoms, chronic pain, cardiovascular conditions and mental health problems [4,5,6,7].
Over recent years, a consensus has been emerging that in order to improve the healthcare of women affected by DVA, greater health services involvement and better experiences of health services for these women is necessary [3, 8, 9]. For example, for improved delivery of sexual and reproductive health care, identification and management of DVA needs to be central not a tangential add-on service [10]. Therefore, commissioning of health services that are able to respond to DVA, should occur in a unified, coordinated fashion - not be fragmented between multiple organisations [11].
IRIS (Identification and Referral to Improve Safety of women affected by DVA) is a, system-level, training and support programme, designed to improve the primary healthcare response to DVA [12]. The programme focuses on primary care clinicians identifying women who experience domestic abuse, discussing and offering, and, if the woman agrees to it, a referral to a named specialist within a DVA advocacy service.
A one-year cluster randomised controlled trial (RCT) evaluated the IRIS intervention in 24 intervention practices, with 24 control practices, across two areas (London Borough of Hackney and Bristol). IRIS substantially increased (2110%; 95%confidence interval CI = (1150,4240%)) the number of referrals to DVA service providers [12]. Trial data modelling showed that IRIS was cost-effective, with NHS and societal cost savings of £1 and £37 respectively per female patient aged 16 and over, per practice, per year [13]. IRIS has been found to be an acceptable intervention for both clinicians and patients [14, 15].
Implementation of IRIS outside of a trial [16] resulted in a large increase in referrals received by DVA service providers (3024%; 95%CI = (2055,4477%)), with no increase in 61 general practices in the fifth borough that did not fund IRIS, but instead provided DVA information sessions to which general practice clinicians were invited [17]. IRIS outside the trial setting is also cost-effective, from the NHS and societal perspective, good value for the NHS, cost saving for society – incremental net monetary benefit was £22 and £42 respectively [18]. A mixed method implementation process evaluation and a qualitative study found that staff mix and IRIS’ joined up approach, bridging the planets of general practice and specialist domestic abuse support services is crucial to making IRIS work [19, 20].
IRIS became a commissionable programme in 2010 and has been implemented across more than 40 different sites in England and Wales, with over 850 general practices fully IRIS trained to date that have referred over 14,000 women to specialist support through their GPs, with an estimated 50,000 women who have discussed DVA with a primary care clinician [21]. One quarter of areas that have commissioned IRIS since 2010 are no longer funding IRIS. Different local IRIS services have different referral rates with our process evaluation suggesting that short term funding and temporary IRIS service disruptions due to loss of trust in the service, results in drop in referral rates [19].
In our interrupted time series study [17], in two boroughs the provision of IRIS service was disrupted for a period of three and six months respectively. Our research question is whether the service disruption in each borough had an effect on the referral rate, during the period within which the disruption occurred. Using statistical analysis we thus quantify the impact of this disruption of IRIS as a service providing support to women affected by DVA, and hence learn lessons for future implementation of DVA programmes in health service contexts. The aim of this analysis is to determine whether transient IRIS service disruptions would decrease IRIS effectiveness, decreasing the referral rate of women affected by DVA, by clinicians to DVA workers.
Methods
This study is a multidisciplinary collaboration of academic GPs, DVA specialists, qualitative and quantitative researchers.
IRIS service description
IRIS core components include: 1. Practice based training to help identify women affected by DVA - two initial two-hour clinical sessions, with third for refresher training 2. Local GP delivering clinically relevant DVA training 3. IRIS advocate educator (AE) who receives referrals directly from trained clinicians, sees patients affected by DVA, usually within the practice, dispensing expert advocacy and ensuring direct access for women to specialist abuse services. Women can also self-refer if they see IRIS publicity material displayed within a practice [17].
Data
For each borough, we included data from female patients aged 16 and above, registered at each general practice within the two boroughs. We used anonymised data on daily referrals received by DVA specialists from general practices in two boroughs, referred to as borough B and borough C in line with our previous work [17].
In borough B service disruption was due to funding of IRIS temporarily stopping, while in borough C funding was still in place but service disruption was due to the IRIS AE leaving with no replacement. In borough B, clinicians were told to refer women affected by DVA, to a different DVA service provider based in borough B. In borough C, clinicians were told to continue referring women affected by DVA to the local IRIS service, though these referrals were redirected to the host DVA service provider based in borough C. iris service provision was disrupted for a period of six and three months respectively in boroughs B and C. The dates of IRIS service disruption, implementation and data collection were collected for each borough (Table 1 and Table S2 in the Additional file 1).
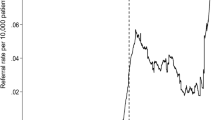
The primary outcome was the number of daily referrals received by the DVA service provider from each of the 36 and 37 general practices in boroughs B and C respectively over 48 months (March 2013 and April 2017) in borough B and 42 months (October 2013–April 2017) in borough C (details in Table 1). Table 1 shows for each borough, the start date of data collection, the start of IRIS implementation, the start of the IRIS service disruption, the end of IRIS service disruption and the end date of data collection (respectively times T0, T1, T2, T3 and T4), with the average referral rate in the periods before, during and after IRIS service interruption. T0, T1, T2, T3 and T4 are also labelled in Fig. 1 (a)-(b).
(a)-(b): Smoothened time series of the data from 73 GPs across two different boroughs (blue lines) and best fit fractional polynomial to the data (maroon solid and dashed lines) with equation and specific parameters outlined in the supplementary material. The graphs show the daily referral rate (\( \frac{number\ of\ referrals}{GP\ size}\ast \mathrm{10,000}\Big) \)) over the period for which we have data in borough B (in (a)) and borough C (in (b)). Boroughs B and C had a disruption of IRIS service for respectively six and three months (time period (T3 − T2) in (a)-(b)). The dashed lines in (a) and (b) illustrate the temporal trajectory of the fitted polynomials in the scenario where “no disruption of IRIS service” would have occurred in these boroughs b and c
Statistical analysis
The outcome of interest was the number of daily referrals received by the DVA service provider from general practices, with the rate per 10,000 patients calculated as \( \frac{number\ of\ referrals}{practice\ size}\ast \mathrm{10,000} \). We modelled this outcome separately for each borough and testing different regression models (negative binomial, mixed-effect negative binomial models or mixed-effect Poisson model- details in Additional file 1). Practice size was included in the model as an offset term. The model allowed for differences in referral rates between GP practices via a random intercept for GP practice. Since the daily number of referrals contained a large proportion of zeroes, we also assessed whether a zero-inflated mixed effects negative binomial model or a zero-inflated mixed effects Poisson model improved the fit to the data. For each regression model, we calculated the Akaike Information Criterion (AIC) and the Bayesian Information Criterion (BIC) to compare models. The best-fit model was chosen based on the smallest values of these quantities (details are in Table S1 of Additional file 1).
Exploratory analysis showed that the referral rate during the IRIS implementation period was not constant over time, even outside the period of interruption. We therefore modelled the post-implementation trend of the referral rate as a non-linear function of time. This allows us to derive a model-based estimate of the referral rate over the whole period under consideration in this analysis. By adding an indicator variable for days falling into the disruption period, we could estimate the difference in the referral rate due to the interruption during the period within which it occurred. Our model assumes that the effect of the disruption on the referral rate is immediate, suggesting that even transient IRIS service disruptions would immediately raise the barrier for GPs to make referrals for DVA.
We used fractional polynomials, with two time transformations as well as an indicator variable for the disruption period, to identify the optimal transformations of time for our models separately for each borough (Model 1 in Additional file 1 with details of the transformations in Tables S3 and S4). For graphical display, we smoothed the observed average daily referral rate over all practices using a moving average with uniform weights (101 and 45 lagged and forward terms for each referral respectively in boroughs B and C respectively).
Sensitivity analyses
To investigate the robustness of our model fit and account for different ways of modelling temporal fluctuations in the referral rate, we conducted a sensitivity analysis for each borough by fitting both a simpler and a more complex model in comparison to Model 1. The simple model (Model 2 in Additional file 1) assumes that the referral rate is constant over time, other than during the disruption period, and calculates and tests the simple difference in the average referral rate between the implementation and disruption periods, albeit controlling for between-practice differences in the base referral rate. Within this Model 2, the model included two predictors: one time transformation, as the random intercept for time, and the indicator variable for the disruption period (see Additional file 1 for details). In contrast, for the more complex model (Model 3 in the Additional file 1), we allowed 5 predictors within the mixed effects negative binomial model: four time transformations as well as the indicator variable for the disruption period. By allowing the fractional polynomials to have higher number of terms, we allowed a closer fit of the modelled referral rate to the observed referral rate over time (see Additional file 1 for details).
For each of the Models 1–3, and for both boroughs B and C, we calculated the incidence rate ratio (IRR), their 95% CI and the p-value, quantifying the impact and significance of the IRIS service disruption (details in Tables S3 and S4 in Additional file 1). To add robustness to the results, we added bootstrapped calculations for the standard errors with 500 replications. All analyses were done in STATA version 15.1.
Results
Descriptive results
Table 1 shows the mean referral rates over all practices in each borough in the periods before, during, and after disruption of the IRIS service illustrating that the mean referral rate is reduced during the disruption period in both boroughs. The mixed-effect negative binomial model was the best-fit model for the data in both boroughs, since both AIC and BIC were minimal for this model (see Table S1 in Additional file 1 for details). The best-fit models superimposed over the corresponding smoothed time-series of the data for boroughs B and C are shown in Fig. 1(a)-(b). Descriptively, in both boroughs we see a steep increase of the referral rate after the start of the IRIS intervention. The referral rate then remains high for a few months, before declining over time in both boroughs. For a few months before the disruption period, there is a surge in referral rates in both boroughs, before a sharp decline in both boroughs during the disruption period. The referral rate stays approximately stable during the disruption period with referral rate recovering to pre-suspension levels in borough C, but not in borough B, where it remains low.
Estimated effect of the service disruption
The estimated IRR for the effect of the suspension in each borough are shown in Table 2. In borough B, our model estimated an IRR of 0.301 (95% CI = (0.128, 0.774), p = 0.006). Thus we estimate that the referral rate was reduced by about 70% (between 23 and 87%) during the disruption period, compared to what it would have been without the service disruption.
In borough C, our model estimated an IRR of 0.513 (95% CI = (0.322,0.817), p = 0.005). Thus we estimate that the referral rate was reduced by about 49% (between 18 and 68%) during the disruption period, compared to what it would have been without the service disruption.
Sensitivity analyses
For both boroughs, our chosen model fitted the data best, the simpler model being underfitted, and the complex model being overfitted (Tables S3 and S4 in Additional file 1). However, in each borough all three models gave approximately equivalent results: both in terms of the IRRs and their 95% CI (see Table S3 and S4 in Additional file 1) and the significant difference in the referral rate during the disruption period (p-value is less than 0.05 across all three models – see Tables S3-S4 for details).
Discussion
Our results are evidence that temporary disruption of IRIS, as a programme providing support to women affected by DVA, had a substantial effect on referrals of women affected by DVA to specialist services in both implementation boroughs. In borough B, disruption lasted for six months. The referral rate to DVA specialist services was reduced by 70% during the disruption and did not recover after the disruption. In borough C, the disruption was shorter, lasting three months. During this disruption, the referral rate was reduced by 49%. However, in this borough, although the disruption reduced the referral rate, this reduction was temporary. Once the disruption stopped, the mean referral rate recovered to almost pre-disruption levels (Table 1 and Fig. 1(b)).
Since these disruptions were substantial regardless of their length, our study provides evidence that sustainability of a DVA programme in general practice requires on-going reinforcement strategies and processes in place, not just from the outset but also continually as the programme progresses. For the IRIS programme, this requires the physical presence in general practices of the IRIS AE – without which, as seen in borough C, even short IRIS service disruption that clinicians were unaware of substantially reduced referrals. This is unsurprising, as DVA remains largely an invisible issue in clinical consultations and society.
The challenge in the current health care commissioning and financial climate in the United Kingdom is to ensure that DVA is made visible, with IRIS programmes prioritised in local health policy and wider needs assessments. IRIS offers a cost effective and evidence-based solution along with simple, specialised and effective referral pathways. It should be funded and sustained as routinely as other health care services.
This is the first study that quantifies the impact and significance of disrupting a system-level programme that offers support to woman who experience DVA outside of a trial setting. The analysis we report here extends our previous multi-disciplinary research utilising a rich data set of DVA referrals from a large number of practices across multiple London boroughs [17, 19]. We have applied ITS and non-linear regression analysis to make predictions from a data set comprising of DVA referrals from a large number of practices across two London boroughs. This is accepted as a robust and efficient method for evaluation of public health and primary care evaluations [22, 23].
Whilst regression modelling is useful in drawing conclusion for the duration of the study where fitted curves mimic the data, the presence of turning points in the non-linear fits makes them unreliable for prediction beyond the period for which data are available. An alternative would be to develop and utilise dynamic temporal models that use the data to calibrate the equations to the historic pattern, and then be used to make future prediction.
As further data on the DVA referrals in IRIS implementation settings become available, further analysis can explore the longer-term impact of the intervention. Comparing IRIS implementation across different settings would be an interesting extension of this work. Furthermore, evaluating adapted versions of the IRIS model that are currently being piloted is a feasible extension of this work. For example, following a successful pilot in two sexual health clinics, further work is ongoing to develop this into a commissionable service [24, 25].
Conclusions
Disrupting the IRIS primary healthcare domestic violence programme substantially reduced the rate of referrals to DVA service providers. Our work yields important lessons for the implementation of health care-based DVA programmes in general and specifically for future IRIS implementation in the UK, revealing the negative and enduring impact of disrupting a primary care service for woman who experience DVA, highlighting the need for continual support and funding of such service provision.
Availability of data and materials
The datasets used and analysed during this study and the numerical codes used to generate the outcomes of this paper are available from the corresponding author on reasonable request.
Abbreviations
- DVA:
-
Domestic violence and abuse
- IRIS:
-
Identification and Referral to Improve Safety
- GP:
-
General practitioner
- NHS:
-
National Health Service
- IRR:
-
Incidence rate ratio
- ITS:
-
Interrupted time series
- RCT:
-
Randomised control trial
- AIC:
-
Akaike Information Criterion
- BIC:
-
Bayesian Information Criterion
- CI:
-
Confidence interval
- AE:
-
Advocate educator
References
NICE. Domestic violence and abuse: How social care, health services and those they work with can respond effectively. London: NICE; 2014. https://www.nice.org.uk/guidance/ph50/chapter/glossary#domestic-violence-and-abuse, Assessed 27 June 2019.
WHO. Global and regional estimates of violence against women: prevalence and health effects of intimate partner violence and non-partner sexual violence. Geneva: WHO; 2013.
Domestic Abuse in England and Wales, Office of National Statistics. https://www.ons.gov.uk/peoplepopulationandcommunity/crimeandjustice/bulletins/domesticabuseinenglandandwales/yearendingmarch2018. Assessed 27 June 2019.
Bonomi AE, Anderson ML, Reid RJ, et al. Medical and psychosocial diagnoses in women with a history of intimate partner violence. Arch Intern Med. 2009;169:1692–7. https://doi.org/10.1001/archinternmed.2009.292.
Campbell JC. Health consequences of intimate partner violence. Lancet. 2002;359:1331–6. https://doi.org/10.1016/S0140-6736(02)08336-8.
Tollestrup K, Sklar D, Frost FJ, et al. Health indicators and intimate partner violence among women who are members of a managed care organization. Prev Med. 1999;29:431–40. https://doi.org/10.1006/pmed.1999.0552.
Coid J, Petruckevitch A, Chung WS, et al. Abusive experiences and psychiatric morbidity in women primary care attenders. Br J Psychiatry. 2003;183:332–9. discussion 40-1. https://doi.org/10.1192/bjp.183.4.332.
National Institute for Health and Care Excellence. Domestic violence and abuse: multi-agency working NICE guidelines, February 2014. https://www.nice.org.uk/guidance/ph50 , assessed 12th June 2019.
Department of Health and Social Care. Responding to domestic abuse: a resource for heath professionals, March 2017. https://www.gov.uk/government/publications/domestic-abuse-a-resource-for-health-professionals, assessed 12th June 2019.
Starrs AM, Ezeh AC, Barker G, Basu A, Bertrand JT, Blum R, Coll-Seck AM, Grover A, Laski L, Roa M, Sathar ZA, Say L, Serour GI, Singh S, Stenberg K, Temmerman M, Biddlecom A, Popinchalk A, Summers C, Ashford LS. Accelerate progress—sexual and reproductive health and rights for all: report of the Guttmacher–lancet commission. Lancet. 2018;391:2642–92. https://doi.org/10.1016/S0140-6736(18)30293-9.
Pathak N, Tariq S. Underfunded and fragmented – a storm is brewing for sexual and reproductive health services. Nat Rev Urol. 2018;15(8):472–3. https://doi.org/10.1038/s41585-018-0038-5.
Feder G, Davies RA, Baird K, Dunne D, Eldridge S, Griffiths C, Gregory A, Howell A, Johnson M, Ramsey J, Rutterford C, Sharp D. Identification and referral to improve safety (IRIS) of women experiencing domestic violence with a primary care training and support programme: a cluster randomised controlled trial. Lancet. 2011;378:1788–95. https://doi.org/10.1016/S0140-6736(11)61179-3.
Devine A, Spencer A, Eldridge S, Norman R, Feder G. Cost-effectiveness of identification and referral to improve safety (IRIS), a domestic violence training and support programme for primary care: a modelling study based on a randomised controlled trial. BMJ Open. 2012;2:e001008. https://doi.org/10.1136/bmjopen-2012-001008.
Malpass A, Sales K, Johnson M, Howell A, Agnew Davies R, Feder G. Women’s experiences of referral to a domestic violence advocate in UK primary care settings: a service-user collaborative study. Br J Gen Pract. 2014;64(620):e151–8. https://doi.org/10.3399/bjgp14X677527.
Yeung H, Chowdhury N, Malpass A, Feder GS. Responding to domestic violence in general practice: a qualitative study on perceptions and experiences. Int J Family Med. 2012;2012:960523. https://doi.org/10.1155/2012/960523.
Sohal AH, Feder G, Barbosa E, Beresford L, Dowrick A, El-Shogri F, Howell A, Lewis N, Johnson M, Nightingale C, Boomla K, Morris S, Eldridge S, Griffiths C. Improving the healthcare response to domestic violence and abuse in primary care: protocol for a mixed method evaluation of the implementation of a complex intervention. BMC Public Health. 2018;18(1):971. 30075711. https://doi.org/10.1186/s12889-018-5865-z.
Sohal AH, Feder G, Boomla K, Dowrick A, Hooper R, Howell A, Johnson M, Lewis N, Rutterford C, Eldridge S, Griffiths C. Improving the healthcare response to domestic violence and abuse in UK primary care: interrupted time series evaluation of a system-level training and support programme. BMC Med. https://doi.org/10.1186/s12916-020-1506-3 Publication date 5.03.20.
Barbosa EC, Verhoef TI, Morris S, et al. Cost-effectiveness of a domestic violence and abuse training and support programme in primary care in the real world: updated modelling based on an MRC phase IV observational pragmatic implementation study. BMJ Open. 2018;8(8):e021256. https://doi.org/10.1136/bmjopen-2017-021256 PMID: 30158224.
Lewis NV, Dowrick A, Sohal A, Feder G, Griffiths C. Implementation of the identification and referral to improve safety programme for patients with experience of domestic violence and abuse: a theory-based mixed-method process evaluation. Health Soc Care Community. 2019;00:1–15. https://doi.org/10.1111/hsc.12733.
Dowrick A, Kelly M, Feder G. Boundary spanners: Negotiating connections across primary care and domestic violence and abuse services. Soc Sci Med. 2019. https://doi.org/10.1016/j.socscimed.2019.112687.
IRISi information; https://www.bristol.ac.uk/primaryhealthcare/news/2017/irisi-launch.html, assessed 12th June 2019.
Penfold RB, Zhang F. Use of interrupted time series analysis in evaluating health care quality improvements. Methods in QI Res. 2013;13(6):38–44. https://doi.org/10.1016/j.acap.2013.08.002.
Bernal JL, Cummins S, Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiology. 2017;46(1):348–55. https://doi.org/10.1093/ije/dyw098.
Horwood J, Morden A, Bailey JE, Pathak N, Feder G. Assessing for domestic violence in sexual health environments: a qualitative study. Sex Transm Infect. 2018;94(2):88–92. https://doi.org/10.1136/sextrans-2017-053322 Epub 2017 Aug 4.
Sohal AH, Pathak N, Blake S, Apea V, Berry J, Griffiths C, Feder G. Improving the healthcare response to domestic violence and abuse in sexual health clinics: feasibility study of a training, support and referral intervention. Sex Transm Infect. 2017:sextrans-2016-052866. https://doi.org/10.1136/sextrans-2016-052866.
Acknowledgements
We are most grateful to the practitioners delivering IRIS in each local area, including the general practice staff, IRIS clinical leads, advocate educators, their managers, the third sector DVA host agencies and commissioners based within Primary Care, Public Health and Local Authorities within the participating boroughs. The women affected by DVA, seen in general practice, continue to inspire our work.
Funding
This research was funded by the National Institute for Health Research (NIHR) Applied Health Research and Care North Thames at Bart’s Health NHS Trust (NIHR ARC North Thames). This funder had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The views expressed in this article are those of the authors and not necessarily those of the NHS, the NIHR, or the Department of Health and Social Care. The costs of funding IRIS in each local area was covered by a variety of bodies including Clinical Commissioning Groups, Public Health and Local Authorities.
Author information
Authors and Affiliations
Contributions
The study was led by JPG and AS. AS had the idea of the study and JPG designed and undertook the statistical analysis with input from PM. SE provided statistical oversight for the study. MJ and AH delivered core components of the intervention. AS, NL, MJ and AH collected and collated the data for analysis. JPG and AS drafted the paper with inputs from PM, SE, EBC, MJ, GF, NL and CG. All authors contributed to the manuscript’s revision, refinement and final approval. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study used secondary anonymised data set for which no ethics approval or consent to participate was required.
Consent for publication
Not applicable.
Competing interests
AH and MJ were DVA IRIS advocate educators, at time of original IRIS trial; and are now both funded to facilitate IRIS dissemination in the UK, with MJ the CEO of IRISi. Positive trial findings would support their career development. GF is an IRISi board member. The other authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1:
Supplementary material for paper entitled: Disruption of a primary health care domestic violence and abuse service in two London boroughs: interruptedtime series evaluation. Appendix A: Details of the statistical and sensitivity analysis.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Panovska-Griffiths, J., Sohal, A.H., Martin, P. et al. Disruption of a primary health care domestic violence and abuse service in two London boroughs: interrupted time series evaluation. BMC Health Serv Res 20, 569 (2020). https://doi.org/10.1186/s12913-020-05397-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-020-05397-x