Abstract
Background
Over-testing is a recognized problem, but clinicians usually lack information about their personal test ordering volumes. In the absence of data, clinicians rely on self-perception to inform their test ordering practices. In this study we explore clinician self-perception of diagnostic test ordering intensity.
Methods
We conducted a cross-sectional survey of inpatient General Internal Medicine (GIM) attending physicians and trainees at three Canadian teaching hospitals. We collected information about: self-reported test ordering intensity, perception of colleagues test ordering intensity, and importance of clinical utility, patient comfort, and cost when ordering tests. We compared responses of clinicians who self-identified as high vs low utilizers of diagnostic tests, and attending physicians vs trainees.
Results
Only 15% of inpatient GIM clinicians self-identified as high utilizers of diagnostic tests, while 73% felt that GIM clinicians in aggregate (“others”) order too many tests. Survey respondents identified clinical utility as important when choosing to order tests (selected by 94%), followed by patient comfort (48%) and cost (23%). Self-identified low/average utilizers of diagnostic tests were more likely to report considering cost compared to high utilizers (27% vs 5%, P = 0.04). Attending physicians were more likely to consider patient comfort (70% vs 41%, p = 0.01) and cost (42% vs 17%, p = 0.003) than trainees.
Conclusions
In the absence of data, providers seem to recognize that over investigation is a problem, but few self-identify as being high test utilizers. Moreover, a significant percentage of respondents did not consider cost or patient discomfort when ordering tests. Our findings highlight challenges in reducing over-testing in the current era.
Similar content being viewed by others
Background
Diagnostic investigations are instrumental in screening patients for disease, making a diagnosis, and monitoring response to therapy. In Ontario, Canada (population 13.5 million), hospital based laboratories process over 100 million laboratory tests annually (1), and from 2004 to 2012 the annual volume of computed tomography (CT) scans nearly doubled to over 1.5 million (2). Excessive testing is costly, (3) potentially harmful to patients and creates excess work for providers who must review and follow-up on ordered tests (4, 5). Excessive phlebotomy of hospitalised patients causes patient discomfort and iatrogenic anemia (6), while excess radiation exposure is known to increase cancer risk (7). Unnecessary testing can also lead to diagnostic error through incidental findings and “false positives” (8, 9), which can unleash a diagnostic cascade of further testing and unwarranted treatment (10). The combination of expense and patient harm has led groups such as Choosing Wisely to advocate for physician restraint in diagnostic testing of hospitalised patients (11).
Interestingly, while hospital based physicians are increasingly provided with individualized reports on readmission rates, hospital length-of-stay, and mortality, it is still uncommon for physicians to routinely receive data on their personal diagnostic test ordering practices (12, 13). Without data physicians must to rely on self-perception, though self-perceptions are known to be inaccurate in many settings (14, 15). We surveyed inpatient General Internal Medicine (GIM) attending physicians and trainees at three Canadian teaching hospitals to investigate self-perceived diagnostic test ordering intensity. We explore how a clinicians self-perception of their test ordering practices is influenced by their level of training, and how self-perception as a high or low utilizer of diagnostic tests is associated with different factors that physicians consider important when ordering tests.
Methods
Setting and participants
We conducted a survey of trainees (medical students and residents) and staff physicians (aka attendings) from inpatient GIM teaching services at three University of Toronto hospitals between November 2016 and October 2017. Study sites included Toronto General Hospital, Toronto Western Hospital, and Mount Sinai Hospital which are all tertiary/quaternary care hospitals in Toronto, Ontario. Attendings complete nearly all of their clinical work at their primary hospital, while trainees rotate between hospitals.
Survey tool
We developed a survey tool (Additional file 1: Table S1) to investigate physician self-perceived diagnostic test ordering intensity, self-estimated test ordering volumes, and factors considered when ordering tests. Survey questions were developed via consensus by the study authors and refined using an iterative process. The survey was pilot tested with three colleagues and refined for usability, clarity, and content prior to distribution.
We collected respondent demographics including age, sex, and level-of-training/clinical experience. Using a five-point Likert scale with 1 representing negative responses (much lower, too few tests); 5 representing positive responses (much higher, too many tests), we asked respondents to: 1) rate their personal test ordering intensity relative to their GIM peers; 2) rate the test ordering intensity of their peers in aggregate; and 3) rate how often they considered patient comfort, cost, and clinical utility when deciding what tests to order. We also asked respondents to estimate the number of lab tests and imaging investigations (xrays, ECGs, MRIs, etc.) they order on a typical patient during the first 24 h of hospital admission and on follow-up over a 7 day hospitalization. Structured definitions of what we considered an investigation were provided (Additional file 1: Table S1).
Sampling method and sample size
We invited all GIM attending physicians at the three study sites to participate through email. We surveyed a convenience sample of trainees; specifically, we distributed our survey to trainees on their GIM rotations at our participating hospitals who attended a series of eight noon teaching conferences between November 2016 and August 2017 that members of our study team attended. The survey was distributed to trainees attending the noon conferences and survey administration was followed by a 45-min teaching session led by members of our team for trainees on principles of diagnostic test stewardship, test result follow-up, and challenges. All surveys were completed anonymously using an implied consent process and without an incentive. We calculated that a sample size of 125 completed surveys would provide us with 80% power to detect a 0.5 difference in Likert responses for attendings compared to trainees. All data was stored, analyzed, and presented in aggregate. Institutional review board approval was obtained at each hospital site and the University of Toronto.
Statistical analysis
Trainee response rate was calculated as the number of completed surveys divided by the total number of surveys distributed during noon conferences. Attending response rate was the number completed surveys divided by the number of attendings solicited through email. We used descriptive statistics to characterize respondent demographics. We compared responses of attendings versus trainees and self-identified low/average test utilizers (Likert 1–3) versus high test utilizers (4, 5) with respect to estimated test ordering volumes and the importance of patient comfort, test cost, and clinical utility using chi-square and Fisher’s exact tests for categorical variables, and t-tests for continuous variables. Chi-square statistics were used where samples sizes permitted, (16) with Fisher’s exact tests used for smaller cell sizes.
Recognizing that survey respondents may not complete all survey questions, we examined the proportion of missing data for each question (Additional file 2: Table S2). Percentages in the results are reported based on question specific response rates received for each survey item. We conducted subgroup analyses to evaluate potential differences in test ordering according to sex, level of training, attending experience (< 5 years vs > 5-years in practice), and after dichotomizing Likert responses into negative (Likert 1–2) and positive (Likert 4–5) responses, thereby removing intermediate responses (Likert 3). P-values are reported for all comparisons, and p < 0.05 were judged statistically significant. Statistical analyses were performed using Microsoft Excel 2013 (Microsoft Corp, Redmond, WA) and R Version 3.4.0 (R Core Team, Vienna, Austria).
Results
The overall response rate was 83% (132/159); 92% (99/108) for trainees and 65% (33/51) for attendings (p < 0.001). Question specific response rates across all groups of respondents varied from 90 to 100% (Additional file 2: Table S2). The median age of attendings was 42 years (range 28 to 66 years, 38% female) and trainees was 27 years (range 23 to 37 years, 43% female).
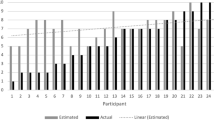
Only 15% (19/130) of respondents self-identified as high utilizers of diagnostic tests relative to their peers, but 73% (96/131) felt that GIM physicians as a group ordered too many tests. The magnitude of this discrepancy was consistent between attendings and trainees (Fig. 1).
Respondents who self-identified as high utilizers of tests did not differ from low/average utilizers in their self-reported testing volumes, nor did estimated test ordering volumes differ between attendings and trainees (Table 1).
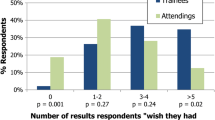
Among all respondents, 94% (122/130) considered clinical utility (i.e., whether a test would impact patient management) most of the time or always (4 or 5 on Likert scale) when deciding what tests to order. 48% (64/132) considered patient comfort most of the time or always and 23% (31/132) considered cost most of the time or always. Attendings were more likely than trainees to identify patient comfort (70% vs 41%, p = 0.01) and cost (42% vs 17%, p = 0.003) as important. Self-identified low/average test utilizers were more likely to identify cost as important compared to high utilizers (27% vs 5%, P = 0.04). Subgroup analyses yielded similar results and are available in Additional file 3: Table S3.
Discussion
In a multi-center study of Canadian inpatient GIM physicians and trainees we investigated self-reported diagnostic test ordering practices. A majority of respondents (73%) identified their colleagues as ordering too many tests, but only 15% self-identified as high test utilizers themselves. We also found infrequent consideration of cost (23%) and patient comfort (48%) when deciding what tests to order. Despite significant efforts to increase awareness of diagnostic minimalism and resource stewardship (11), our findings suggest that important barriers to improvement remain.
Our finding that GIM providers identify their colleagues as high utilizers of diagnostic tests far more often than themselves is mathematically implausible, and may reflect the lack of real-time test ordering feedback to clinicians. GIM physicians in our hospitals receive group-level data on hospital length-of-stay, mortality, and readmission rate, but granular data on diagnostic testing intensity is not routinely available. A number of research teams have demonstrated that audit-and-feedback or computerized “dashboards” providing individualized diagnostic testing data can be helpful (13, 17). Diagnostic test management toolboxes propose interventions to help organizations improve test utilization (18), including individual physician test utilization report cards. While these practices hold promise, they are not widely implemented and a recognized limitation is the need to provide incentives to review and improve performance (18). Lack of real-time diagnostic testing intensity is likely to contribute to well recognized over-use of tests ranging from echocardiography to hemologbin A1c testing (19, 20).
Our findings are also consistent with concepts from behavioural psychology, where the “above average effect” or “comparative optimism effect” describes how individuals look favorably upon personal performance relative to peers (21). Comparative optimism has been shown in surgical residents who over-estimated their global performance (22), and may contribute to diagnostic error though physician anchoring/commitment to a misdiagnosis (23). Our study suggests that self-perceptions are likely to be inaccurate, and again draws attention to the importance of real-time data on diagnostic testing intensity. However, even robust interventions like audit and feedback, if done in isolation, are unlikely to solve all of the challenges with test utilization. Multifaceted and coordinated interventions are likely helpful (18); for example by combining audit and feedback with test ordering decision support tools and de-adoption of obsolete or low-utility tests (8).
It is also important to discuss physician motivations for ordering tests. Survey respondents consistently cited clinical utility (94% overall) as an important consideration which is appropriate since a clinical question should prompt test ordering. Unlike clinical utility, only 24% of respondents cited cost as an important and 48% cited patient comfort; these findings are particularly surprising considering social desirability bias that may have inflated these numbers relative to true beliefs and practice (21). Our finding that many respondents do not consider cost may explain why interventions like displaying test prices to ordering providers have had modest impact (24). The lack of consideration of patient comfort is also worrisome in an era where patient-centered care and patient reported outcomes are increasingly recognized as important (25).
Finally, comparison across respondent groups (high vs low test utilizers and trainees vs attending physicians) warrants comment. Self-reported high utilizers of diagnostic investigations were even less likely than low/average utilizers to report considering cost (5% vs 27%, p = 0.04). This makes us wonder if education about cost is needed, or alternatively, if focusing on cost can ever be effective among providers who do not view fiscal considerations as important. Our finding that trainees were less likely than attendings to consider cost (42% vs 17%) and patient comfort (70% vs 41%) suggests that experience may also play a role in prioritizing these factors. Considering level of training may be important in designing future interventions to curtail over investigation.
Our study has several limitations. First, our study was conducted amongst Internal Medicine trainees and staff physicians at three Toronto teaching hospitals. While our results are likely to be generalizable to Internal Medicine trainees and staff at other Canadian teaching hospitals, extrapolating our findings to other clinical services (e.g., surgery, family medicine), other countries, or community hospitals may be premature. Rather we would suggest our findings need replication in other settings. Second, we relied on physician self-report of test ordering volumes and it is unclear how well self-reported testing behaviors correlate with actual practice. However, most physicians do not regularly receive data on their diagnostic testing utilization so self-perceptions are crucial. Finally, our study focused on inpatient internal medicine wards and it will be important to verify our results in other practice settings.
Conclusions
The absence of real-time data on diagnostic testing utilization forces clinicians to rely upon self-perceptions. In our study, clinicians seem to recognize that over investigation is a problem, but few individuals self-identify as high test utilizers. We also found that a significant percentage of clinicians do not consider cost or patient discomfort when ordering tests. Our findings highlight challenges in reducing over-testing in the current era.
Abbreviations
- CT:
-
(Computed Tomography)
- ECG:
-
(Electrocardiogram)
- GIM:
-
(General Internal Medicine)
- MRI:
-
(Magnetic Resonance Imaging)
References
Ministry of Health and Long-term Care. [Internet]. Laboratory Services Expert Panel 2015. Available from: www.health.gov.on.ca/en/common/ministry/publications/reports/lab_services/labservices. Accessed March 10, 2018.
Canadian Institute for Health Information. [Internet]. Medical Imaging in Canada 2012. Available at: https://www.cihi.ca/en/medical-imaging#_Metadata. Accessed March 10, 2018.
Van Walraven C, Raymond M. Population-based study of repeat laboratory testing. Clin Chem. 2003;49(12):1997–2005.
Darragh PJ, Bodley T, Orchanian-Cheff A, Shojania KG, Kwan JL, Cram P. A systematic review of interventions to follow-up test results pending at discharge. J Gen Intern Med. 2018;33(5):750–8.
Gordon JR, Wahls T, Carlos RC, Pipinos II, Rosenthal GE, Cram P. Failure to recognize newly identified aortic dilations in a health care system with advanced electronic medical record. Ann Intern Med. 2009;151(1):21–7.
Thavendiranathan P, Bagai A, Ebidia A, Detsky AS, Choudhry NK. Do blood tests cause anemia in hospitalized patients? The effect of diagnostic phlebotomy on hemoglobin and hematocrit levels. J Gen Intern Med. 2005;20(6):520–4.
Smith-Bindman R, Lipson J, Marcus R, Kim KP, Mahesh M, Gould R, et al. Radiation dose associated with common computed tomography examinations and the associated lifetime attributable risk of cancer. Arch Intern Med. 2009;169(22):2078–86.
Cadamuro J, Ibarz M, Cornes M, Nybo M, Haschke-Becher E, von Meyer A, et al. Managing inappropriate utilization of laboratory resources. Diagnosis. 2019;6(1):5–13.
Epner PL, Gans JE, Graber ML. When diagnostic testing leads to harm: a new outcomes-based approach for laboratory medicine. BMJ Qual Saf. 2013;22:ii6–ii10.
Carpenter CR, Raja AS, Brown MD. Over testing and the downstream consequences of overtreatment: implications of preventing over diagnosis for emergency medicine. Acad Emerg Med. 2015;22:1484–92.
Choosing Wisely Canada. [Internet]. Internal Medicine: five things physicians and patients should question. Choosing Wisely Canada website. https://choosingwiselycanada.org/internal-medicine. Published April 2, 2014. Accessed August 10, 2018.
Corson AH, Fan VS, White T, Sullivan SD, Asakura K, Myint M, et al. A multifaceted hospitalist quality improvement intervention: decreased frequency of common labs. J Hosp Med. 2015;10(6):390–5.
Kurtzman G, Dine J, Epstein A, Gitelman Y, Leri D, Patel MS, et al. Internal medicine resident engagement with a laboratory utilization dashboard: mixed methods study. J Hosp Med. 2017;12(9):743–6.
Barnsley L, Lyon PM, Ralston SJ, Hibbert EJ, Cunningham I, Gordon FC, et al. Clinical skills in junior medical officers: a comparison of self-reported confidence and observed competence. Med Ed. 2004;38:358–67.
Lipsett PA, Harris I, Downing S. Resident self-other assessor agreement: influence of assessor, competency, and performance level. Arch Surg. 2011;146(8):901–6.
McHugh ML. The chi-square test of independence. Biochemia Medica. 2013;23(2):143–9.
Bhatia RS, Ivers NM, Yin XC, Myers D, Nesbitt GC, Edwards J, et al. Improving the appropriate use of transthoracic echocardiography: the echo WISELY trial. J Am Coll Cardiol. 2017;70(9):1135–44.
Baird G. The laboratory test utilization management toolbox. Biochemia Medica. 2014;24(2):223–34.
Laxmisan A, Vaughan-Sarrazin M, Cram P. Repeated hemoglobin A1C ordering in the VA health system. Am J Med. 2011;124(4):342–9.
Okrah K, Vaghan-Sarrazin M, Cram P. Trends in echocardiography utilization in the veterans administration healthcare system. Am Heart J. 2010;159(3):477–83.
Chambers JR, Windschitl PD. Biases in social comparative judgments: the role of nonmotivated factors in above-average and comparative-optimism effects. Psych Bull. 2004;130(5):813–38.
Berner ES, Graber ML. Overconfidence as a cause of diagnostic error in medicine. Am J Med. 2008;121(5A):S2–23.
Althubait A. Information bias in health research: definition, pitfalls, and adjustment methods. J Multidiscip Healthc. 2016;9:211–7.
Silvestri MT, Bongiovanni TR, Glover JG, Gross CP. Impact of price display on provider ordering: a systematic review. J Hosp Med. 2016;11:65–76.
Ovretveit J, Zubkoff L, Nelson EC, Frampton S, Knudsen JL, Zimichman E. Using patient-reported outcome measurement to improve patient care. Int J Qual Health Care. 2017;29(6):847–9.
Acknowledgements
Not applicable.
Availability of data and material
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
Funding
PC was supported in-part by a K24 award from NIAMS (AR062133) at the US NIH. The funding body had no input on study design, execution, data analysis, or manuscript synthesis.
Author information
Authors and Affiliations
Contributions
TB, PD, JK, and PC conceived the study. TB, PC and JM were involved in study design and data collection. TB and JM synthesized the data and completed the statistical analysis. All authors had full access to the data and take responsibility for the integrity of the data and the accuracy of the data analysis. All five authors contributed to manuscript preparation and refinement. All of the authors read and approved the final manuscript. All of the authors are willing to provide ICMJE authorship disclosures to attest to their contributions.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
An implied consent process was used during in-person and email survey administrations. Each survey had an Institutional Review Board (IRB) approved cover letter explaining the study and consent process. All participants who completed the survey were identified as having consented to the study. Written consent was not required by any of the three IRB approving bodies for this work, which included: the University Health Network (UHN_REB#_16–5633), Mt. Sinai Hospital (MSH_REB#_16–0163), and through the University of Toronto Department of Medicine (Ethics Approval_ Post-graduate Medical Education).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1:
Table S1. Survey Tool: Complete survey tool used during data collection
Additional file 2:
Table S2. Question Specific Response Rates: Response rates for each individual question stratified by level of training (Attendings, Residents, Medical students)
Additional file 3:
Table S3. Subgroup Analysis: Includes Table S1. (Residents compared to Medical Students), Table S2. (Senior Attendings compared to Junior Attendings), Table S3. (Male compared to Female participants), Table S4. (Self-identified High Utilizers of diagnostic tests with Likert 4–5 compared to Low Utilizers with Likert 1–2)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Bodley, T., Kwan, J.L., Matelski, J. et al. Self-reported test ordering practices among Canadian internal medicine physicians and trainees: a multicenter cross-sectional survey. BMC Health Serv Res 19, 820 (2019). https://doi.org/10.1186/s12913-019-4639-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-019-4639-3