Abstract
Background
It is unknown to what extent Choosing Wisely recommendations about income-generating treatments apply to members of the society generating the recommendations.
The primary aim of this study is to determine the proportion of Choosing Wisely recommendations targeting income-generating treatments, and whether recommendations from professional societies on income-generating treatments are more likely to target members or non-members. The secondary aim is to determine the prevalence of qualified statements, and whether qualified statements are more likely to appear in recommendations targeting income-generating or non-income-generating treatments that apply to members.
Methods
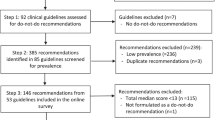
We performed a content analysis of all Choosing Wisely recommendations, with data extracted from Choosing Wisely websites. Two researchers coded recommendations as test or treatment-based, for or against a procedure, containing qualified statements, income-generating and applying to members. Disagreements were resolved by discussion or consultation with a third researcher. A Chi-squared test evaluated whether society recommendations on income-generating treatments were more likely to target members or non-members; and whether qualified statements were more likely to appear in recommendations targeting income-generating or non-income-generating treatments that apply to members.
Results
We found 1293 Choosing Wisely recommendations (48.3% tests and 48.6% treatments). Ninety-eight treatment recommendations targeted income-generating treatments (17.8%), and recommendations on income-generating treatments were less likely to target members compared to non-members (15.6% vs. 40.4%, p < 0.001). Nearly half of all recommendations were qualified (41.9%), with a similar proportion of recommendations targeting income-generating and non-income-generating treatments that apply to members containing qualified statements (49.4% vs. 42.0%, p = 0.23).
Conclusions
Many societies provide Choosing Wisely recommendations that minimise impact on their own members. Only 20% of treatment recommendations target income-generating treatments, and of these recommendations mostly target non-members. Many recommendations are also qualified. Increasing the number of recommendations from societies that are unqualified and target member clinicians responsible for de-implementation of low-value and costly treatments should be a priority.
Similar content being viewed by others
Background
Choosing Wisely is a major public awareness campaign that aims to reduce low-value care through increasing discussions between patients and clinicians about the inappropriate use of medical tests and treatments [1]. Low-value care is care that provides little-to-no benefit or causes harm, provides a benefit too small given its cost, and is unlikely be desired by an adequately informed patient [2]. Choosing Wisely began in April 2012 as an initiative of the American Board of Internal Medicine (ABIM) Foundation, drawing inspiration from earlier initiatives, such as “Medicine’s Ethical Responsibility for Health Care Reform – The Top Five List” [3]. Today, Choosing Wisely is a global campaign with active campaigns in more than 15 countries (e.g. United States, Canada, United Kingdom, Australia, Italy, Netherlands). Choosing Wisely continues to expand and inspire the development of similar initiatives, such as EVOLVE [4] and the Value Based Insurance Design (VBID) Health’s Task Force on Low-value Care [5].
In an effort to reduce low-value care, professional societies from a variety of health disciplines (including surgery, medicine, diagnostics and allied health) have published Choosing Wisely lists [1]. Choosing Wisely lists comprise recommendations intended to facilitate open patient-clinician discussions about tests and treatments that are unnecessary, and that both patients and clinicians should question. There are over 1000 Choosing Wisely recommendations published worldwide but there is yet to be an evaluation of their content.
An ongoing concern is whether the recommendations made by professional societies focus on the low value care specifically provided by their members [6, 7]. Because of a lack of research it is unclear if recommendations typically refer to treatments provided by members of the society generating the recommendations, and whether recommendations are less likely to target treatments provided by members when income is involved. Ensuring recommendations refer to treatments provided by members (hereafter referred to as recommendations that ‘apply to members’) is likely to increase awareness of low-value treatments among the practitioners providing those procedures. Further, if Choosing Wisely is to have a meaningful impact on reducing healthcare waste, ensuring society recommendations target income-generating treatments provided by their own members is important.
Societies may be naturally cautious about publishing recommendations that could reduce the income of their members and may consequently publish recommendations (unintentionally or intentionally) that apply to non-members or use qualified wording (‘not complete or absolute’). For example, societies primarily involved in providing surgical procedures could target non-surgical treatments provided by non-members or focus on recommendations targeting low-value diagnostic tests. Although this practice could still raise awareness of low-value tests and treatments, there is a missed opportunity to raise awareness of low-value and costly procedures provided by members of that society. Recommendations that are qualified (and therefore open to interpretation) might also limit the impact Choosing Wisely has on reducing low-value care. The wording of practice recommendations is an important factor for increasing adoption [8]. Guidelines advocating that recommendations are actionable (e.g. “don’t”), avoid ambiguity, and are clear enough as a stand-alone resource [9,10,11]. Using qualified phrases like “when possible”, “don’t routinely” or “unless necessary” may be used to capture clinical complexity but they also give clinicians some latitude to choose an interpretation that avoids practice change.
The primary aim of this study is to determine the proportion of Choosing Wisely recommendations targeting income-generating treatments, and whether society recommendations on income-generating treatments are more likely to target members or non-members. The secondary aim is to determine the prevalence of qualified statements, and whether qualified statements are more likely to appear in recommendations targeting income-generating or non-income-generating treatments that apply to members. We hypothesise that society recommendations on income-generating treatments are less likely to target members compared to non-members, and that qualified statements are more likely to appear in recommendations targeting income-generating treatments (compared to non-income-generating treatments) that apply to members.
Methods
We performed a content analysis of all published Choosing Wisely recommendations; extracting data from Choosing Wisely websites and The DIANA (Dissemination of Initiatives to ANalyse Appropriateness) in Healthcare website (http://dianasalud.com/index.php) until June 2018. Duplicates were excluded and all recommendations (including corresponding data on the professional society, year, and country) were copied into a spreadsheet. We used the following rules to code each recommendation.
Characteristics of recommendations
Diagnostic test or treatment
Recommendations targeting procedures that are performed to identify or confirm the presence of disease or injury were coded as ‘diagnostic tests’. Recommendations targeting interventions provided to individuals with disease or injury (excluding diagnostic tests) were coded as ‘treatments’. Recommendations targeting diagnostic tests and treatments were coded as ‘both’, while recommendations that did not involve the patient were coded as ‘neither’ (e.g. “Don’t replace hand hygiene with the use of non-sterile disposable gloves”).
For or against a procedure
Recommendations were coded as ‘don’t’ if they advised against a procedure and ‘do’ if they recommended a procedure. Most of the time the distinction between a ‘do’ and ‘don’t’ was clear. For example, “Don’t use glucosamine and chondroitin to treat patients with symptomatic osteoarthritis of the knee” compared to “Offer PSA screening for detecting prostate cancer only after engaging in shared decision making.” However, some ‘do’ recommendations were less clear by starting with the word ‘don’t’. For example, “Don’t delay basic level palliative care for women with advanced or relapsed gynaecologic cancer, and when appropriate, refer to specialty level palliative medicine”. We coded these recommendations as ‘do’. Recommendations that were coded as ‘don’t’ but provided an alternative to de-implementation were noted. For example, “Do not use percutaneous feeding tubes in patients with advanced dementia; instead use oral assisted feeding.”
Qualified statements
Recommendations that contained ‘qualified statements’ (statements that were ‘not complete or absolute’) typically used words or phrases like, ‘consider avoiding’, ‘don’t routinely’, ‘don’t overuse’, ‘don’t rely on’, ‘don’t use X unless necessary’, ‘don’t use X without an appropriate clinical indication’. For example, “Don’t routinely transfuse patients with sickle cell disease (SCD) for chronic anemia or uncomplicated pain crisis without an appropriate clinical indication”. Examples of qualified statements are outlined in Additional file 1. Recommendations that we considered clear and absolute were coded as ‘unqualified’. For example, “Don’t transfuse red blood cells in hemodynamically stable, non-bleeding ICU patients with a hemoglobin concentration greater than 7 g/dL.”
Income-generating treatments
Treatments that attract a fee for service and are performed outside of a routine clinical encounter (i.e. a scheduled procedure) were coded as ‘income-generating’ for the clinician performing the treatment (e.g. surgery, insertion of an instrument or device for a therapeutic purpose, and radiotherapy). The full list of income-generating treatments found among Choosing Wisely recommendations is reported in Additional file 1. ‘Non-income-generating’ treatments included, but were not limited to, medication, electrotherapy, injection therapies (excluding vitreal injections), blood transfusions, inserting a catheter, and administering supplemental oxygen. These treatments could not be considered ‘income-generating’ by the above definition (i.e. they could be provided within a routine clinical encounter).
Recommendations that apply to members
Recommendations that targeted treatments provided or performed by members of the society generating the recommendation were considered to ‘apply to members’. We did not code recommendations for diagnostic tests because radiologists and pathologists provide or perform the majority of these tests in most healthcare settings (excluding the use of diagnostic tests by, for example, emergency physicians, general physicians and cardiologists). In other words, most recommendations targeting diagnostic tests would be coded as ‘non-income-generating’ and ‘apply to non-members’ if not published by a diagnostic society. We excluded ‘do’ recommendations, recommendations from societies not linked with the delivery of health services (e.g. The International Society of Doctors for the Environment), and recommendations from groups of societies or societies that had members across health disciplines (e.g. nursing, surgery, medicine).
Rater panel
The panel was comprised of an orthopaedic surgeon, a senior resident in orthopaedic surgery, and two physiotherapists; all of whom were clinician researchers (two were professors; three had PhDs). Collectively the panel had decades of clinical experience in a range of healthcare settings in Australia and abroad.
Data analysis
All four researchers independently coded the first 150 recommendations to assess agreement and refine the coding rules. Once the researchers agreed upon the final coding rules, two researchers, drawn from the panel of four, independently coded all the recommendations, resolving all disagreements by discussion or consultation with a third researcher where necessary. Although two researchers independently coded the recommendations and all disagreements were resolved, we were interested in testing the reliability of the coding framework. Kappa statistics (95% confidence intervals (CI)) and percent exact agreement were calculated to assess agreement between reviewers for coding the characteristics of all recommendations. Kappa (k) statistics were interpreted as follows: < 0.00 = “poor”, 0.00–0.20 = “slight”, 0.21–0.40 = “fair”, 0.41–0.60 = “moderate”, 0.61–0.80 = “substantial”, ≥0.81 = “almost perfect” [12].
Descriptive statistics (counts and percentages) were used to report the coded data, as well as the number of recommendations, and the professional societies that published Choosing Wisely lists (including the country). A Chi-squared test evaluated whether society recommendations on income-generating treatments are more likely to target members or non-members; and whether qualified statements were more likely to appear in recommendations targeting income-generating or non-income-generating treatments that apply to members. We then stratified our main analyses by society (categorised as medical, surgical, diagnostic, allied health – including nursing, pharmacy and dentistry – and other). All analyses were performed in STATA statistical software (version 13.1).
Results
We found 1293 Choosing Wisely recommendations across the United States (n = 535, 41.4%), Canada (n = 309, 23.9%), Italy (n = 174, 13.5%), Australia (n = 172, 13.3%), the United Kingdom (n = 56, 4.3%), Netherlands (n = 30, 2.3%), New Zealand (n = 12, 0.9%; 117 duplicate recommendations were excluded), and Japan (n = 5, 0.4%) (Table 1). Choosing Wisely campaigns were also found (or mentioned) in Austria, Brazil, Denmark, France, Israel, Portugal, South Korea, Switzerland, and Wales but no recommendations were readily available. Germany published 10 recommendations only intended to guide the development of future recommendations, and these were therefore not included in the analysis. Of the included recommendations, 646 (50.0%) were from medical societies, 243 (18.8%) from surgical societies, 181 (14.0%) from diagnostic societies (e.g. radiology, pathology), 137 (10.6%) from allied health societies (including nursing, pharmacy and dentistry), and 86 (6.7%) from other societies (Table 1). A detailed breakdown of the societies across countries is in Additional file 2.
Characteristics of choosing wisely recommendations
There were 624 (48.3%) recommendations concerning diagnostic tests, 628 (48.6%) concerning treatments, 24 (1.8%) concerning both, and 17 (1.3%) that did not involve patient care so could not be classified as either a diagnostic test or treatment. There were 1210 (93.6%) recommendations that advised against a procedure and 83 (6.4%) that recommended a procedure. Of the 1210 recommendations that advised against a procedure, only 55 (4.5%) provided an alternative test or treatment. There were 98 (17.8%) recommendations targeting income-generating treatments and 454 (82.3%) recommendations targeting non-income-generating treatments (Table 1). The coding of all recommendations can be found in Additional file 3.
Agreement between reviewers for coding recommendations was ‘almost perfect’ for diagnostic tests or treatments (k = 0.94, 95% CI: 0.92 to 0.95), ‘substantial’ for qualified statements (k = 0.71, 95% CI: 0.67 to 0.75) and income-generating treatments (k = 0.79, 95% CI: 0.71 to 0.85), and ‘moderate’ for recommendations for or against a procedure (k = 0.48, 95% CI: 0.37 to 0.57) and recommendations that apply to members (k = 0.42, 95% CI: 0.29 to 0.55) (Table 2). Percent exact agreement was high across all coding domains (range: 86 to 97%).
Income-generating treatments that apply to members
There were 98 (17.8%) treatment recommendations targeting income-generating treatments, and recommendations regarding income-generating treatments were less likely to target members compared to non-members (15.6% vs. 40.4%, p < 0.001) (Table 3) (Fig. 1). Recommendations targeting income-generating treatments were most common across surgical societies (45.5%) and least common across medical (12.9%) and allied health societies (4.0%). Moreover, recommendations regarding income-generating treatments were only less likely to target members compared to non-members across medical (9.3% vs. 92.3%, p < 0.001) and diagnostic societies (13.6% vs. 50.0%, p = 0.03) (Fig. 1).
Qualified wording
Five-hundred and forty-two (41.9%) recommendations were qualified and 751 (58.1%) were unqualified (Table 1), with medical (46.6%) and surgical societies (42.0%) displaying the highest proportion of ‘qualified’ recommendations (Additional file 4). A similar proportion of recommendations targeting income-generating and non-income-generating treatments that apply to members contained qualified statements (49.4% vs. 42.0%, p = 0.23). (Table 4). There was no difference in the proportion of qualified statements among all income-generating and non-income-generating treatment recommendations (45.9% vs. 41.4%, p = 0.41), and among treatment recommendations targeting members and non-members (43.2% vs. 31.9%, p = 0.16) (Additional file 5).
Discussion
Choosing Wisely recommendations are framed in ways that lessen potential impact on the members of the society making the recommendation. Only 20% of treatment recommendations refer to income-generating treatments, and these are less likely to target members compared to non-members. Although nearly half of Choosing Wisely recommendations are qualified, qualified statements were not more likely to appear in recommendations targeting income-generating treatments that apply to members. Societies need to generate recommendations that specifically target the practice of members, and reduce, if not eliminate, qualified recommendations from Choosing Wisely.
Strengths and weakness of the study
This study has numerous strengths, including being the first to evaluate the content of all Choosing Wisely recommendations. We searched both Choosing Wisely websites and The DIANA in Healthcare website to ensure a systematic evaluation of all available recommendations. The method used to code the data was robust as four researchers independently rated 150 recommendations and discussed disagreements to pilot the checklist. The research team had decades of clinical experience in a range of healthcare settings in Australia and abroad. This experience was sufficient to develop a reliable coding tool; percent exact agreement ranged from 86 to 97% across all coding domains. Further, any limitations of the coding tool are unlikely to influence the results since two researchers independently rated all 1293 recommendations and resolved any disagreements by discussion or consultation with one of the other two researchers. The primary limitation is that differences in reimbursement systems between countries might influence what treatments generate income for clinicians. Nevertheless, we are confident the treatments classified as ‘income-generating’ (Additional file 1) would remain in this category across most healthcare systems.
Meaning of the study
Choosing Wisely aims to reduce waste in healthcare. However, pursuit of this aim is arguably compromised when society recommendations on income-generating treatments are less often targeted towards members compared to non-members. In addition, almost half of Choosing Wisely recommendations target low-value diagnostic tests, with only 20% of test recommendations coming from diagnostic societies. Increasing awareness of low-value testing is important, but when societies mainly look for waste in fields other than their own, their recommendations are likely to have less impact [6, 7]. To illustrate these points, 23 societies have published recommendations about imaging for low back pain, and five have published recommendations about imaging for acute ankle sprains. In contrast, of the eight societies that include orthopaedic surgeons (n = 48 recommendations), there are only 9 recommendations about low-value surgery (e.g. knee arthroscopy, spinal fusion and subacromial decompression) [13,14,15].
Choosing Wisely recommendations are often qualified, using phrases like ‘don’t routinely’, ‘don’t overuse’ or ‘unless necessary’. Although qualified statements may be necessary for some areas of practice, the counter argument is that they give clinicians latitude to adopt an interpretation of the recommendation that best suits their practice and make it difficult to appropriately measure adherence [8, 16, 17]. With this in mind, it might not be surprising that 1 year after the launch of the campaign there was little-to-no change in the de-implementation of a number of low-value practices in the United States (e.g. imaging for low back pain and human papillomavirus testing in young women) [18]. We acknowledge that this evaluation was limited to a small number of recommendations and that increased awareness of Choosing Wisely since it was launched in 2012 might have increased the impact it has had on reducing low-value care [1]. Nevertheless, if Choosing Wisely is to maximise its impact on improving patient care and reducing the enormous amount of healthcare waste worldwide [19,20,21], recommendations may need to be unqualified.
Unanswered questions and future research
A few studies suggest some societies are averse to targeting income-generating treatments provided by their members [7, 22, 23], and instead “pick the low hanging fruit that was so low it was lying on the ground” (Vikas Saini – cardiologist and president of the Lown Institute) [7]. Although this behaviour is understandable, research exploring the drivers of this behaviour is essential if Choosing Wisely hopes to realise its goal of reducing low-value care and healthcare waste. A recent editorial [24] on ‘Why do surgeons continue to perform unnecessary surgery?’ provided some insight on these barriers from a surgeon’s perspective. The authors suggest that surgeons continue to provide low-value surgery because of incentives – either from income, status, or both – and because they are trained to do surgery. Further, selective anecdotes of successful cases and years of education and training might foster a strong attachment to surgery, making de-implementation even more difficult [25]. With this in mind, surgical societies might be the most averse to targeting income-generating treatments provided by members. However, we found this was not the case. The proportion of recommendations targeting income-generating treatments provided by members was highest across surgical societies (45.5%), and much lower across medical (12.9%) and diagnostic societies (18.0%). In addition, society recommendations on income-generating treatments were significantly less likely to target members compared to non-members across medical and diagnostic societies, but not across surgical societies. These findings are likely explained by many recommendations from medical societies targeting surgical procedures and many recommendations from diagnostic societies targeting treatments. Medical and diagnostic societies should therefore consider how their Choosing Wisely lists could better target unnecessary and high-cost care provided by their members.
Investigating strategies to increase adoption of Choosing Wisely recommendations should be a research priority. Compared to more intensive implementation strategies such as audit and feedback or educational outreach, refining the wording of Choosing Wisely recommendations is simple and cheap, making it a logical first step towards increasing adoption among clinicians. Re-wording recommendations so they are unqualified will send a clear message to clinicians and is necessary to ensure de-implementation is measurable [8]. Further, there is underuse of recommendations that provide an alternative to de-implementation and including ‘do’ and ‘don’t’ statements within a recommendation could increase clinicians’ willingness to replace low-value care with the suggested high-value alternative. The evaluative linguistic framework developed by Buchbinder and colleagues also shows promise for judging and enhancing the quality of medical information (e.g. drug leaflets) [26, 27] and could be adapted to evaluate the quality of Choosing Wisely recommendations. For example, the tool judges the clarity of what ‘action’ must be taken, who is responsible for the ‘action’, and the importance or urgency of the ‘action’. Ensuring Choosing Wisely recommendations clearly address these factors could be vital for increasing clinicians’ willingness to follow them. The next step for Choosing Wisely should be research investigating how the wording of Choosing Wisely recommendations influences adoption, as this will have important implications for refining existing recommendations and developing new ones.
Conclusion
Our analysis found that Choosing Wisely recommendations made by societies are often framed to minimise impact on their members. Only 20% of recommendations target income-generating treatments, and of these recommendations most target non-members. Nearly half of Choosing Wisely recommendations are qualified. Increasing the proportion of Choosing Wisely recommendations that are unqualified and target member clinicians responsible for de-implementation of low-value treatments should be a priority.
Availability of data and materials
All data generated or analysed during this study are included in this published article (see Additional file 3).
Abbreviations
- ABIM:
-
American Board of Internal Medicine
- CI:
-
Confidence interval
- DIANA:
-
Dissemination of Initiatives to ANalyse Appropriateness
- k:
-
Kappa
References
Choosing Wisely. An initiative of the ABIM foundation. Clinician lists http://www.choosingwisely.org/. Accessed 30 Apr 2019.
Scott IA, Duckett SJ. In search of professional consensus in defining and reducing low-value care. Med J Aust. 2015;203(4):179–81.
Brody H. Medicine's ethical responsibility for health care reform — the top five list. N Engl J Med. 2010;362:283–5.
Morrisroe K, Nakayama A, Soon J, Arnold M, Barnsley L, Barrett C. EVOLVE: the Australian rheumatology Association's 'top five' list of investigations and interventions doctors and patients should question. Intern Med J. 2018;48(2):135–43.
Value Based Insurance Design (VBID) Health. Reducing Use of Low-value Medical Care - Task Force on Low-value Care. http://www.vbidhealth.com/low-value-care-task-force.php. Accessed 14 July 2019.
Morden NE, Colla CH, Sequist TD, Rosenthal MB. Choosing wisely — the politics and economics of labeling low-value services. N Engl J Med. 2014;370(7):589–92.
Lenzer J. Choosing wisely: setbacks and progress. BMJ. 2015;351:h6760.
Michie S, Johnston M. Changing clinical behaviour by making guidelines specific. BMJ. 2004;328(7435):343–5.
Hussain T, Michel G, Shiffman RN. The Yale guideline recommendation corpus: a representative sample of the knowledge content of guidelines. Int J Med Inform. 2009;78(5):354–63.
Promoting Transparent and Actionable Clinical Practice Guidelines: Viewpoint from the National Guideline Clearinghouse/National Quality Measures Clearinghouse (NGC/NQMC) Editorial Board. http://www.guidelines.gov/expert/expert-commentary.aspx?id=24556. Accessed 30 Apr 2019.
National Institute for Health and Clinical Excellence: Guidance. https://www.nice.org.uk/process/pmg6/chapter/developing-and-wording-guideline-recommendations. Accessed 30 Apr 2019.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–74.
Saltychev M, Eskola M, Laimi K. Lumbar fusion compared with conservative treatment in patients with chronic low back pain: a meta-analysis. Int J Rehabil Res. 2014;37(1):2–8.
Beard DJ, Rees JL, Cook JA, Rombach I, Cooper C, Merritt N, et al. Arthroscopic subacromial decompression for subacromial shoulder pain (CSAW): a multicentre, pragmatic, parallel group, placebo-controlled, three-group, randomised surgical trial. Lancet. 2018;391(10118):329–38.
Sihvonen R, Paavola M, Malmivaara A, Itälä A, Joukainen A, Nurmi H, et al. Arthroscopic partial meniscectomy versus sham surgery for a degenerative meniscal tear. N Engl J Med. 2013;369(26):2515–24.
Grimshaw JM, Shirran L, Thomas R, Mowatt G, Fraser C, Bero L, et al. Changing provider behavior: an overview of systematic reviews of interventions. Med Care. 2001;39(8 Suppl 2):Ii2–45.
Shetty KD, Meeker D, Schneider EC, Hussey PS, Damberg CL. Evaluating the feasibility and utility of translating choosing wisely recommendations into e-measures. Healthc (Amst). 2015;3(1):24–37.
Rosenberg A, Agiro A, Gottlieb M, Barron J, Brady P, Liu Y, et al. Early trends among seven recommendations from the choosing wisely campaign. JAMA Intern Med. 2015;175(12):1913–20.
Brownlee S, Chalkidou K, Doust J, Elshaug AG, Glasziou P, Heath I, et al. Evidence for overuse of medical services around the world. Lancet. 2017;390(10090):156–68.
Elshaug AG. Over 150 potentially low-value health care practices: an Australian study. Med J Aust. 2013;198(2):85.
Institute of Medicine. Best Care at Lower Cost: the path to continuously learning health Care in America. Washington, DC: The National Academies Press; 2013. https://doi.org/10.17226/13444.
Kerr EA, Jersey C, Jeremy BS, Mandi LK, Brahmajee KN. Stress testing before low-risk surgery: so many recommendations, so little OveruseStress testing before low-risk surgery. JAMA Int Med. 2015;175(4):645–7.
Colla CH, Sequist TD, Rosenthal MB, Schpero WL, Gottlieb DJ, Morden NE. Use of non-indicated cardiac testing in low-risk patients: choosing wisely. BMJ Qual Saf. 2015;24(2):149–53.
Stahel PF, VanderHeiden TF, Kim FJ. Why do surgeons continue to perform unnecessary surgery? Patient Saf Surg. 2017;11:1.
Scott IA, Soon J, Elshaug AG, et al. Countering cognitive biases in minimising low value care. Med J Aust. 2017;206:407–11.
Clerehan R, Hirsh D, Buchbinder R. Medication information leaflets for patients: the further validation of an analytic linguistic framework. Commun Med. 2009;6(2):117–27.
Hirsh D, Clerehan R, Staples M, Osborne RH, Buchbinder R. Patient assessment of medication information leaflets and validation of the evaluative linguistic framework (ELF). Patient Educ Couns. 2009;77(2):248–54.
Acknowledgements
Not applicable.
Funding
The authors received no specific funding for this work.
Author information
Authors and Affiliations
Contributions
All authors critically revised the manuscript for important intellectual content and approved the final manuscript. Please find below a detailed description of the role of each author: JZ: conception and design, analysis and interpretation of data, drafting and revision of the manuscript, and final approval of the version to be published. JF: conception and design, acquisition and interpretation of data, drafting and revision of the manuscript, and final approval of the version to be published. IH: conception and design, interpretation of data, drafting and revision of the manuscript, and final approval of the version to be published. CM: conception and design, interpretation of data, drafting and revision of the manuscript and final approval of the version to be published. The Corresponding Author (JZ) attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Authors’ information
Dr. Joshua Zadro is a postdoctoral research fellow and physiotherapist. Dr. John Farey is a senior resident of orthopaedic surgery. Prof Ian Harris is a professor of orthopaedic surgery and practicing orthopaedic surgeon. Prof Christopher Maher is an NHMRC Principal Research Fellow and physiotherapist.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1.
Examples of qualified statements and income-generating treatments.
Additional file 2.
Choosing Wisely recommendations across individual societies and country.
Additional file 3.
Coding of all recommendations.
Additional file 4.
Wording of Choosing Wisely recommendations across societies. n: number of recommendations; %: percentage of all recommendations within each society; *including nursing, dentistry and pharmacy.
Additional file 5.
Wording of treatment recommendations (n = 552). n: number of recommendations; *: percentage of income-generating treatments; †: percentage of non-income generating treatments; ‡: percentage of treatment recommendations provided by members; §: percentage of treatment recommendations provided by non-members.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Zadro, J.R., Farey, J., Harris, I.A. et al. Do choosing wisely recommendations about low-value care target income-generating treatments provided by members? A content analysis of 1293 recommendations. BMC Health Serv Res 19, 707 (2019). https://doi.org/10.1186/s12913-019-4576-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-019-4576-1