Abstract
Background
Are creativity and compliance mutually exclusive? In clinical settings, this question is increasingly relevant. Hospitals and clinics seek the creative input of their employees to help solve persistent patient safety issues, such as the prevention of bloodstream infections, while simultaneously striving for greater adherence to evidence-based guidelines and protocols. Extant research provides few answers about how creativity works in such contexts.
Methods
Cross-sectional survey data were collected from employees in 24 different U.S.-based outpatient hemodialysis clinics. Linear mixed-effects models were utilized to test study hypotheses. Professional status, clinic climate variables, and interaction terms were modeled as fixed effects, with a random effect for clinic included in all models.
Results
Our results show that high status employees contributed more creative patient safety improvement ideas compared to low status employees. However, when high status employees were part of clinics with a stronger safety climate of compliance, they contributed fewer creative ideas compared to their counterparts working in clinics with a reduced compliance orientation. We also predicted low status employees working in less punitive clinics would contribute more creative ideas, but this hypothesis was not fully supported.
Conclusions
This study suggests that in hospitals and clinics that rely on strict protocols and formal hierarchies to meet their goals, the factors that promote creativity may be distinctively context-dependent. Implications for theory, practice, as well as future directions for research examining creativity in healthcare and safety critical contexts are discussed.
Similar content being viewed by others
Background
Creativity, the production of novel and useful ideas [1, 2] is a clear leadership priority in the modern health care organization [3, 4]. Though forward-thinking healthcare leaders may be motivated to facilitate creativity among their clinicians and front-line staff, it remains largely unclear how to most effectively achieve such outcomes. Extant research in management and organizational behavior reveals several important factors that positively influence employee creativity such as perceived leader support [5], empowering leadership style [6] and organizational culture and climate [7]; however, little work to date examines the influence of such factors in clinical settings, that, unlike many business organizations, do not typically follow a mission centered around creativity.
Much of the existing empirical work to date focuses on organizations in sectors focused on strategic innovation, such as technology firms and research and development laboratories. These types of organizations typically try to provide an environment conducive to individual creativity. For example, employees may be provided with greater opportunities for autonomous work [8], a factor shown to encourage workplace creativity [9]. While these types of provisions are possible in some organizations for certain types of roles, great autonomy is not typically characteristic of many of the job roles in safety critical settings, such as health care facilities. Most hospitals and clinics rely on highly specified behavioral protocols to run safely and efficiently (e.g., pre- and post-operative checklists, hand hygiene, catheter insertion, maintenance, and removal bundles protocols). Behavioral protocols have certain advantages in that they can limit the margin of error for certain processes and procedures thereby helping to promote or maintain safety. However, research has shown that limiting the behavior of individuals this way can have negative consequences on the individual’s creative performance [9]. Furthermore, while these procedures do provide important guidelines for practice standardization, many problems they aim to address continue to remain unsolved [10]. The persistence of such issues has prompted many organizations to search for new, creative solutions; however, progress has been slow [11, 12].
In addition to the strict behavioral protocols that often underlie approaches to safety, the hierarchical orientation of health care settings is another factor that may influence creative problem solving ability [13]. Hospitals and clinics have formal hierarchies with salient differences in the relative professional status of roles [14]. These roles are often well defined and dictated by factors such as education, licensure, and job title. In other words, it is uncommon for any single individual or role to have complete knowledge of all care processes that unfold daily in any single care area, clinic, or department. Therefore, when solving patient safety problems, not having the input of individuals of differing status might be a significant hindrance because only certain individuals may be able to provide key details related to local work processes, inefficiencies and/or vulnerabilities.
The pursuit of creative solutions to clinical patient safety problems in healthcare presents an interesting quandary. Creativity in this context could be thought of in terms of Reason’s description of a person versus system approach to human fallibility [15]. According to Reason, a person approach focuses squarely on individual errors and the blaming of individuals in an effort to achieve safety; whereas, a system approach, accepts human error as a given and focuses on the conditions under which people work as the most effective levers of safety. In terms of creativity, the system approach allows for individuals to remain open and respond to what they see and experience. In sharp contrast, the person approach extinguishes any incentive to think or behave differently, which is a prerequisite for identifying novel and useful ideas and solutions to problems.
Other factors that are inherent to organizations, such as strong hierarchies, can also produce unintended barriers to creativity. In theory, hierarchical organizations with safety climates that strongly reinforce routinization and procedural consistency may unintentionally inhibit the creative potential of employees necessary to identify and implement solutions to complex problems [16,17,18]. Research has shown that employee creativity can be difficult to facilitate even in organizations that actively encourage members to innovate [19, 20]. Therefore, the question of how creativity is affected in highly proceduralized, safety-critical environments is an important empirical question explored in this study.
To this end, we hypothesized and tested several factors that may influence the creative participation of clinicians and staff working in outpatient hemodialysis clinics. First, we examined the effect of professional status on creativity. Our prediction was that low status clinical staff would contribute less creative ideas concerning patient safety opportunities compared to high status clinicians. We also explored two dimensions of organizational safety climate hypothesized to influence creativity among higher and lower status staff based upon theoretical relationships proposed in Vogus, Sutcliffe, and Weick’s [21] model of organizational safety and well accepted definitions and measures of creative problem solving from management and organizational behavior research [22]. Specifically, we predicted that high status clinicians working in clinics with stronger supervisory expectations about safety would perform less creatively than those working in clinics with climates that were less compliance oriented, and low status clinical staff would perform more creatively in clinics with a safety climate that is less punitive in response to error compared to clinics with more punitive climates.
Methods
Research setting and procedures
Our study was conducted among a sample of outpatient hemodialysis clinics participating in a quality improvement initiative designed to reduce clinic-level bloodstream infection (BSI) rates. Hemodialysis clinics are a novel safety critical setting in which to study creativity because of their participation in a growing national movement to reduce the incidence of blood-stream infections experienced by patients undergoing this treatment [23]. Significant human and financial resources have been put toward overcoming this challenge [24, 25], making it an excellent example of an organizational safety problem in need of creative solutions.
Hemodialysis is a 3 to 5-h blood filtering treatment received three times per week by individuals who suffer from chronic kidney disease or kidney failure. When receiving treatment, individuals are connected to a dialyzer machine via one of three methods: fistula, graft or catheter [26]. Between 60 and 80% of patients initiate dialysis via catheter, a method that is particularly vulnerable to infection and yields higher rates of patient morbidity and mortality [10, 27]. The CDC estimates that 37,000 catheter-related bloodstream infections occur every year at an average cost of $23,000 per hospitalization, and up to a quarter of these infections ultimately result in death [10]. Interventions to reduce the incidence of these infections have been developed and demonstrated success in hospital-based critical care settings [25]; however, outpatient dialysis clinics have not yet realized the same reductions in infection rates. Therefore, many clinics have attempted to utilize quality improvement interventions designed to elicit ideas from their staff to implement in practice.
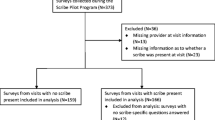
Cross-sectional survey data were collected from clinical staff working in 24 different hemodialysis clinics participating in this longitudinal quality improvement initiative [24]. All clinics were in major metropolitan areas in the United States. Data from three clinics were excluded from the analyses because they either withdrew from the project or had less than 10% staff participation. Two individual participants were removed from our analyses because they worked with more than one clinic in the sample. All other individuals in the sample worked exclusively at a single clinic. Our final sample included 229 respondents nested in 21 separate clinics.
Measures
Creativity
Our dependent variable, creativity, was assessed using an adapted version of the Staff Safety Assessment (SSA) [28]. The SSA asks clinic staff to individually generate ideas for patient safety and quality improvement. Specifically, participants were asked to identify “the most important patient safety opportunity” in their clinical area. Two expert coders familiar with the operations of hemodialysis clinics coded the entire sample of ideas (n = 229) for novelty and usefulness [1, 2] on a 5-point Likert scale (1 = strongly disagree, 5 = strongly agree). Coders were selected based on their expertise in safety and quality improvement efforts in outpatient dialysis settings. Coders were blind to our hypotheses and any potentially identifying respondent information including job title and location. A single creativity score was created for each response by multiplying the novelty score and the usefulness score [29, 30]. The highest creativity scores represented ideas that were both novel and useful. During coding, 21 responses were removed due to missing data. Agreement on ratings of novelty (α = .81) and usefulness (α = .73) was good, and therefore the two coders’ scores were averaged together to form a composite score.
Status
Clinical practice regulations require that staff members with less formal education practice under the supervision of clinicians with more formal education. Because education level accurately mirrors the relative differences in position and influence in the clinical care domain, it was used as a proxy indicator of professional status. Status was operationalized in terms of the amount of education beyond high school required to hold a position. This operationalization is consistent with measures used by other researchers who conduct organizational research in clinical care settings [31].
Participants were categorized into Roles 1, 2, 3, or 4 (See Table 1 and Fig. 1). Role 1 is comprised of patient care technicians (PCTs) who are required to have a high school diploma or equivalent training. Licensed Practical Nurses (LPNs) and Registered Nurses (RNs) were categorized separately in our analyses. LPNs complete less formal education, possess different credentialing, are compensated differently, and have less decision-making ability compared to RNs. Furthermore, RNs tend to mediate between strategy and day-to-day operations whereas LPNs work mostly in the procedural domain [32]. Therefore, in our study, LPNs are categorized as Role 2 and RNs are categorized as Role 3. Clinical staff in Role 4 have education beyond a bachelor’s degree and include physicians and clinic administrators.
Clinic climate
Clinician and staff perceptions of clinic safety climate included in the dataset were originally collected using a version of the Hospital Survey on Patient Safety Culture (HSOPS) [33] with minimal adaptations for the outpatient hemodialysis setting. The survey asks participants about the culture in their clinic as it pertains to safety, including two dimensions that were hypothesized to moderate the effects of status on individual creativity. Supervisory expectations regarding patient safety and compliance with safety practices was measured using the 4-item composite scale, Supervisor Expectations and Actions Regarding Safety. Non-punitive climate was measured by the 3-item composite scale, Non-Punitive Response to Error. The specific items comprising these scales and relevant scale properties are reported in the Appendix. Participants used a 5-point Likert-type scale to indicate the degree to which they agreed or disagreed with each survey item (1 = strongly disagree, 5 = strongly agree). The HSOPS has demonstrated sound psychometric properties across a variety of samples and has demonstrated predictive validity for meaningful outcomes, including patient outcomes [34]. The survey was administered to all clinicians and staff electronically using a commercially available online survey platform. The average number of survey respondents per clinic was 11.43 (SD = 7.70) and the average survey response rate among the 21 included clinics was 57% (SD = 0.32).
In line with survey scoring parameters [33], individual respondent scores were pooled to create a clinic level score on each dimension that reflects the percentage of clinic team members who responded positively on the dimension. Indices of within-clinic agreement supported aggregating individual responses to clinic-level scores for both Supervisory Expectations and Non-Punitive Response to Error. ICC(1) values ranged from 0.33 to 0.46 and rWG(j) scores [35, 36] ranged from 0.68 to 0.80, indicating reasonable within-clinic agreement (see Appendix).
Additionally, to ensure there was adequate between-clinic variation in clinic-level climate scores to warrant hypothesis testing, we conducted separate Multiple Analyses of Variance (MANOVA) with clinic as the independent variable and the specific items included in each climate dimension entered as dependent variables. Results indicated significant between clinic variation for both climate dimensions (Wilks’ λsupervisory expectations = 0.64, p < 0.001 and Wilks’ λnon-punitive climate = 0.76, p = 0.005).
Infection rate
Clinic infection rates are reported as the number of central venous catheter infections per 100 patient months in line with the CDC’s national surveillance system for hemodialysis-associated infections [37].
Analyses
Linear mixed-effects models, also referred to as hierarchical linear models, were utilized to test study hypotheses and account for the nesting of individual respondents within clinics. Professional status, clinic-level climate variables, and interaction terms were modeled as fixed effects, with a random effect for clinic included in all models. In simple terms, mixed-effect linear models enabled regression coefficients to vary from clinic to clinic, and then averages these estimates to obtain a coefficient reflecting the overall effect of the variables of interest on creativity. Analyses were conducted using STATA 12.
Results
Descriptive statistics and correlations among study variables are displayed in Table 2.
To test our first hypothesis, a mixed effects model (Model 1) including Professional Status as a fixed effect and random effect for clinic was conducted. Results from Model 1 (displayed in the upper portion of Table 3) indicated that status was significantly related to Clinic Staff Creativity after accounting for variation between clinics (χ2 = 13.82, p = 0.003). In support of our initial hypothesis, clinical staff in Role 4 exhibited greater creativity compared to staff in Role 1 (β = 2.52, 95% CI: 1.08, 3.97), however the effect of status was not clearly linear. Post-hoc analyses indicated that Role 1 and Role 2 did not differ significantly (p = 0.17), though those in Role 4 exhibited significantly greater creativity than those in Role 3 (p = 0.004). This model also suggests that meaningful variance in creativity (13%) was explained at the clinic level. Following these results, supervisory expectations and non-punitive climate were investigated as hypothesized moderators of the observed professional status-creativity relationship.
Omnibus tests of hypothesized moderation effects
To test hypothesized moderation effects of Supervisory Expectations and Non-Punitive Climate on the observed status-creativity relationship, separate clinic-level simple linear regression models (SLR) were first examined. These models regressed the correlation between status and creativity on each of the climate dimensions. The SLR models provide a preliminary omnibus test of hypothesized moderation effects and were examined prior to conducting more complex mixed effects regression models. This method is commonly used for testing moderation hypotheses in biostatistics. Results suggested that Supervisory Expectations (F (1,17) = 10.91, p = 0.004) significantly moderated the relationship between status and creativity, such that the relationship between status and creativity was significantly reduced as supervisory expectations regarding compliance increased. This provided initial support for moderation Hypothesis 2, and prompted additional exploration regarding the directionality of this effect using mixed effects modeling. The SLR model, however, did not detect a significant moderation effect for Non-Punitive Climate (p = 0.76); and therefore, we did not find adequate support to suggest further testing of Hypothesis 3.
Examining the moderating effect of supervisory expectations
We used mixed-effects regression modeling (Model 2) to further explore the moderating effect of supervisory expectations. Results are summarized in the lower \portion of Table 3. In Model 2, creativity was regressed onto status, supervisory expectations, and the interaction between supervisory expectations and status. Clinic was again modeled as a random effect parameter. As seen in the lower portion of Table 3, the interaction model explained significant variance in creativity (χ2 = 28.52, p < .001). In clinics with stronger supervisory expectations regarding compliance, Role 1 staff contributed ideas that were as creative as those ideas contributed by Role 4 staff (β = − 0.23; 95% CI: -0.40, − 0.05). More specifically, in these clinics, the creativity of low status clinical staff was slightly higher, but the creativity of high status clinicians was significantly inhibited (see Fig. 1).
Supplemental analysis: Supervisory expectations and infection rates
A supplemental analysis was conducted to examine the extent to which clinic-level scores on supervisory expectations related to clinic-level central venous catheter infections rates. A median split was utilized to categorize clinics into low and high supervisory expectations groups. Results of a two-sample t-test did not detect any significant differences in patient infection rates between these groups (p = 0.59; see Table 4). These findings, in tandem with the moderation analyses, suggest that clinics with higher supervisor expectations regarding safety and compliance did not achieve significantly higher levels of patient safety, though they were creating environments that could potentially reduce the creativity of their higher status team members.
Discussion
This study examined the influence of professional status and two aspects of safety climate on creativity among clinicians working in outpatient hemodialysis clinics. Our results demonstrate that, as predicted, high status clinicians contributed more creative patient safety improvement ideas compared to low status clinical staff. However, in clinics with stronger supervisory expectations about safety and compliance, the creativity of the two highest status groups (Roles 3 & 4) was dampened. Though we did not specifically predict a drop in the creativity of clinicians in Role 3 (RNs), we find this result interesting and worth further exploration. Some work in management suggests that it is more difficult for middle status members of organizations to be creative due to pressures from above and below [38]. It is possible that middle status conformity pressure interacts with compliance focus in a way that could explain these results more thoroughly. Moreover, the inhibition of creativity was significantly greater for those clinicians of highest status (Role 4). We also predicted that low status staff in clinics operating under a less punitive climate would contribute significantly more creative ideas; however, this hypothesis was not supported.
Our research is not without limitations. First, because our sample was dependent on surveys, the possibility of non-response bias should be noted. It is possible that some individuals did not respond based on potentially meaningful, but unmeasured variables. Additionally, the mix of roles varied across clinics. For example, one clinic did not have any LPNs. Second, the generalizability of our findings may be constrained given our sample of outpatient hemodialysis clinics. It is possible that these results may not be exactly the same in an acute, hospital care setting or another organization operating in a different safety critical industry. It should also be noted that the participating clinics were providing safe care at higher levels compared to national averages [39].Footnote 1 It is possible that the relatively advanced level of care at which these clinics were operating may have influenced the results. For example, in organizations that exhibit poor performance, clinical staff might have many more ideas about how to improve patient safety simply because there is a greater opportunity for improvement. Additional studies with larger or different clinical settings and staff samples could help determine the extent to which these limitations might be of any significant concern.
Furthermore, our findings suggest that there may be diminishing returns on some aspects of organizational performance associated with strong supervisory expectations about safety and compliance. In this sample of clinics, a greater supervisory focus on safety and compliance did not result in a significant difference in infection rates,Footnote 2 but it did reduce creativity among high status clinicians. One potential explanation for these findings is that highly compliance-oriented organizations may inhibit creativity because they shape and reinforce a less mindful approach to safety and to work tasks in general [40,41,42]. Research by Vogus and Sutcliffe [40] demonstrates that a mindful approach to safety is characterized by proactive and deliberate behavior rather than rote compliance. Employees working in organizations that promote mindfulness in safety tend to think critically about their organization as an entire system, and they are encouraged to think creatively about real or potential areas of risk. This type of approach may permit individuals to express their creativity even under the constraints of highly proceduralized work, whereas an overly compliance-oriented climate may greatly reduce the motivation to be creative [1, 2, 8].
Within health care management and safety research, this work highlights an important opportunity to integrate the topic of creativity as an effective tool in managing the changes that many organizations currently face. Though not necessarily specific to creativity, researchers have also recommended managing the dimensions of the safety critical organizational context in order to meet certain goals. For example, Weick and Sutcliffe [41] encourage deference to legitimate expertise rather than heavy reliance on formal hierarchy when problem solving. Their logic echoes what we found in our results – compliance should be emphasized appropriately but not to the point where it overshadows other important benefits to the organization.
This work also contributes to our understanding of creativity in context by providing additional insight into the effects that certain facet-specific forms of safety climate may have on creativity. In our sample of hemodialysis clinics, a stronger climate of compliance significantly inhibited the creative contributions of high status clinicians. The reduction of creativity in these individuals is noteworthy given that these team members are in positions of influence and increasingly tasked with helping to solve patient safety and quality problems. Moreover, these staff members have a large impact on the local clinical climate. Given these important consequences, we argue that these preliminary results warrant further exploration.
Our prediction about the influence of a non-punitive climate on the creative performance of low status staff yielded null results. This prediction was grounded in existing theory [42] and although our results did not fully support this hypothesis, the results did inspire some pertinent questions for future study. For instance, it is possible that the facilitation and motivation of creativity for low status individuals in this context requires stronger, dedicated psychological interventions. Related research may provide some key clues as to what variables may be important to explore. For example, some research [31] suggests that leaders must both explicitly demonstrate that they value contributions from low status employees and those employees must perceive the environment as being psychologically safe to achieve their stated safety goals. Given their close proximity to patients and responsibilities of direct care tasks, we reiterate our original argument for the investigation of how to facilitate the creative potential of lower status clinical staff in proceduralized organizational contexts. The active participation of these members may help organizations find solutions to pervasive problems concerning preventable patient and consumer harm, and we encourage future studies of this relationship.
Practical implications and opportunities for future research
Our findings suggest several interesting practical implications as well. First, health care practitioners are seeking creative solutions to challenging problems with little to no context-specific guidance for managing such behavior. For instance, three of the top ten strongly encouraged evidence-based patient safety strategies identified by Shekelle and colleagues [43] included itemized checklists and standardized hand hygiene protocols that, when designed or implemented sans frontline staff input or leadership, could be interpreted as tools focused squarely on compliance and adherence. The opportunity to facilitate the development of creative solutions certainly exists in this domain, but they have not yet made their way into mainstream patient safety practice. Furthermore, what is available by way of traditional organizational research on creativity caters mostly to organizations that are structured in ways that are almost diametrically opposed to the typical safety critical work environment, such as a clinic. Additional research will need to be conducted to identify effective methods and practices for cultivating creativity and implementing innovative solutions to these and other existing problems specific to these types of settings.
Second, future research is necessary to more fully understand and address the barriers to implementing change in clinical care settings that are likely tied to these organizations’ focus on compliance and safety. For example, future studies might examine whether a climate that is highly focused on compliance could influence the cognitive approach that individuals take to identifying, understanding, and investigating potential opportunities for improvement in perhaps unintended ways. Demonstrating that individuals respond differently to certain dimensions of safety climate that are typical of this setting would be an important contribution because it may suggest that information and messaging regarding safety should be tailored specifically to the target audience rather than presented uniformly across an organization as it is often done. It is important for practitioners to be able to gauge the boundary conditions of these effects as it relates to clinical staff and consider actionable ways to achieve high levels of patient safety through simultaneous focus on creative problem solving while maintaining adherence to known, effective solutions.
Conclusion
This work is presented as an empirical prelude to the continued study of creativity in a variety of safety critical contexts, including health care environments that rely on behavioral and procedural protocols and formal hierarchies to meet their goals. Our results suggest that the roadmap to creativity may look meaningfully different for safety critical organizations like hospitals and clinics. Many of these organizations are actively encouraging creativity, even if it is in the service of another goal (e.g., safety, quality improvement, etc.). Expanding the scope of safety research to encompass this change is necessary to clarify the boundaries of our existing knowledge. By expanding the application of creativity to organizations in these sectors, researchers may be able to have a greater impact to both the field and practitioners.
Notes
In terms of organizational safety performance, this sample of clinics was comparable to national indices of patient safety outcomes including BSI (mean catheter-related infection rate in our sample = 3.1 per 100 patient months) versus most recently available national average catheter-related BSI rate for outpatient hemodialysis clinics = 4.2 per 100 patient months [39].
We conducted a supplementary analysis to examine the extent to which supervisory expectations was related to clinic-level BSI rates. A median split was utilized to categorize clinics into low and high compliance-focused groups. Results of a two-sample t-test did not detect any significant differences in patient infection rates between these groups (p = 0.57).
References
Amabile TM. Creativity in context. Boulder, CO: Westview Press; 1996.
Woodman R, Sawyer J, Griffin R. Toward a theory of organizational creativity. Acad Manag Rev. 1993;18:293–321.
Berwick D, Bauchner H, Fontanarosa PB. Innovations in health care delivery: call for papers for a yearlong series. JAMA. 2015;314:675–6.
Zuckerman B, Margolis PA, Mate KS. Health services innovation: the time is now. JAMA. 2013;309:1113–4.
Amabile TM, Schatzel EA, Moneta GB, Kramer SJ. Leader behaviors and the work environment for creativity: perceived leader support. Leadersh Q. 2004;15:5–32.
Carmeli A, Gelbard R, Reiter-Palmon R. Leadership, creative problem-solving capacity, and creative performance: the importance of knowledge sharing. Hum Resour Manag. 2013;52:95–121.
Tesluck PE, Farr JL, Klein SR. Influences of organizational climate and climate on individual creativity. J Creat Behav. 2007;31:27–41.
Grant AM, Berry JW. The necessity of others is the mother of invention: intrinsic and prosocial motivations, perspective taking, and creativity. Acad Manag J. 2011;54:73–96.
Amabile TM, Conti R, Coon J, Lazenby J, Herron M. Assessing the work environment for creativity. Acad Manag J. 1996;39:1154–84.
Centers for Disease Control (CDC). National health care safety network (NHSN): Tracking infections in outpatient dialysis facilities. 2013. http://www.cdc.gov/nhsn/dialysis/. Accessed 13 Nov 2018.
National Patient Safety Foundation. Free from harm: Accelerating patient safety improvement fifteen years after To Err is Human. 2015. http://www.npsf.org/?page=freefromharm. Accessed 13 Nov 2018.
Wachter RM. Patient safety at ten: unmistakable progress, troubling gaps. Health Aff. 2010;29:165–73.
Paulus PB, Yang HC. Idea generation in groups: a basis for creativity in organizations. Organ Behav Hum Decis Process. 2000;82:76–87.
Edmondson AC. Speaking up in operating room: how team leaders promote learn interdisciplinary action teams. J Manage Stud. 2003;40:1419–52.
Reason J. Human Error: Models and Management. BMJ. 2000;320:768–70.
Cameron KS, Quinn RE. Diagnosing and changing organizational culture: based on the competing values framework. San Francisco: Jossey-Bass; 2005.
Conchie SM, Taylor PJ, Donald IJ. Promoting safety voice with safety-specific transformational leadership: the mediating role of two dimensions of trust. J Occup Health Psychol. 2012;17:105–15.
Hartnell CA, Ou AY, Kinicki A. Organizational culture and organizational effectiveness: a meta-analytic investigation of the competing values framework's theoretical suppositions. J Appl Psychol. 2011;96:677–94.
Kim SH, Vincent LC, Goncalo JA. Outside advantage: can social rejection fuel creative thought? J Exp Psychol Gen. 2013;142:605–11.
Mueller JS, Melwani S, Goncalo JA. The bias against creativity: why people desire but reject creative ideas. Psychol Sci. 2012;23:13–7.
Vogus TJ, Sutcliffe KM, Weick KE. Doing no harm: enabling, enacting, and elaborating a culture of safety in health care. Acad Manag Perspect. 2010;24:60–77.
Zhou J, Hoever IJ. Research on workplace creativity: a review and redirection. Annu Rev Organ Psychol Organ Behav. 2014;1:333–59.
Kuehn BM. Reducing dialysis-related infections. JAMA. 2013;309:2542.
Kishnan M, Van Wyck D, Culkin N, Holland J, Goeschel C, Lubomski LH, et al. Meeting the challenge: Translating effective quality improvement strategies from the inpatient to the outpatient setting. Poster presented at the 2012 Healthcare-Associated Infections (HAI) Data Summit. US Department of Health & Human Services. Kansas City, MO.
Pronovost P, Needham D, Berenholtz S, Sinopoli D, Chu H, Cosgrove S, et al. An intervention to decrease catheter-related bloodstream infections in the ICU. N Engl J Med. 2006;355:2725–32.
National Kidney Foundation. Hemodialysis: What you need to know. National Kidney Foundation. 2007. https://www.kidney.org/sites/default/files/11-50-0214_hemodialysis.pdf. Accessed 13 Nov 2018.
Besarab A, Pandey R. Catheter management in hemodialysis patients: delivering adequate flow. Clin J Am Soc Nephrol. 2011;6:227–34.
Pronovost PJ, Weast B, Rosenstein B, Sexton JB, Holzmueller CG, Paine L, et al. Implementing and validating a comprehensive unit-based safety program. J Patient Saf. 2005;1:33–40.
Brophy DR. Understanding, measuring, and enhancing individual creative problem-solving efforts. Creat Res J. 1998;11:123–50.
Reiter-Palmon R, Robinson EJ. Problem identification and construction: what do we know, what is the future? Psychol Aesthet Creat Arts. 2009;3:43–7.
Nembhard IM, Edmondson AC. Making it safe: the effects of leader inclusiveness and professional status on psychological safety and improvement efforts in health care teams. J Organ Behav. 2006;27:941–66.
Birken SA, Lee S, Weiner BJ, Chin MH, Chiu M, Schaefer CT. From strategy to action: how top managers’ support increases middle managers’ commitment to innovation implementation in healthcare organizations. Health Care Manag Rev. 2015;40:159–68.
Sorra J, Nieva VF. Hospital survey on patient safety culture. Agency for Healthcare Research and Quality; 2004.
Jackson J, Sarac C, Flin R. Hospital safety climate surveys: measurement issues. Curr Opin Crit Care. 2010;16:632–8.
James RL, Demaree RG, Wolf G. Rwg: an assessment of within-group interrater agreement. J Appl Psychol. 1993;78:306–9.
LeBreton JM, Senter JL. Answers to 20 questions about interrater reliability and interrater agreement. Organ Res Methods. 2007;11:815–52.
Tokars JI, Miller ER, Stein G. New national surveillance system for hemodialysis-associated infections: initial results. Am J Infect Control. 2002;30:288–95.
Duguid MM, Goncalo JA. Squeezed in the middle: the middle status trade creativity for focus. J Pers Soc Psychol. 2015;109:589.
Klevens RM, Edwards JR, Andrus ML, Peterson KD, Dudeck MA, Horan TC, et al. Dialysis surveillance report: National Healthcare Safety Network (NHSN)-data summary for 2006. Sem Dialysis. 2008;21:24–8.
Vogus TJ, Sutcliffe KM. The safety organizing scale: development and validation of a behavioral measure of safety culture in hospital nursing units. Med Care. 2007:46–54.
Weick KE, Sutcliffe KM. Mindfulness and the quality of organizational attention. Organ Sci. 2006;17:514–24.
Weick KE, Sutcliffe KM. Managing the unexpected: resilient performance in an age of uncertainty: John Wiley & Sons; 2011.
Shekelle PG, Pronovost PJ, Wachter RM, McDonald KM, Schoelles K, Dy SM, Walshe K, et al. The top patient safety strategies that can be encouraged for adoption now. Ann Intern Med. 2013;158:365–8.
Acknowledgements
The authors would like to acknowledge Nancy Culkin, Pam Earll, Christine A. Goeschel, Lisa H. Lubomski, Allen R. Nissenson, Levi Njord, Peter J. Pronovost, Brenda Smolinski, Kathleen Sutcliffe, Kathryn Taylor, David Van Wyck for their help and support of this project.
Funding
DaVita, Inc. (contract DaVita/08/2011) through contractual agreements with Johns Hopkins University, for and on behalf of the Armstrong Institute for Patient Safety & Quality.
Availability of data and materials
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
SK, SW, and MR contributed to manuscript conceptualization, writing, analysis interpretation and revision. TY conducted analyses and interpretation of findings. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This project was approved by the Johns Hopkins Medicine IRB (NA_00087953: Safety Climate in Outpatient Hemodialysis Care).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:
STROBE Statement. Checklist of items that should be included in reports of cross-sectional studies. (DOCX 34 kb)
Appendix
Appendix
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Kim, S.H., Weaver, S.J., Yang, T. et al. Managing creativity and compliance in the pursuit of patient safety. BMC Health Serv Res 19, 116 (2019). https://doi.org/10.1186/s12913-019-3935-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-019-3935-2