Abstract
Background
Delivery of quality healthcare in resource-limited settings is an important, understudied public health priority. Thirty-day (early) hospital readmission is often avoidable and an important indicator of healthcare quality.
Methods
We investigated the prevalence of all-cause early readmission and its associated factors using age and sex adjusted risk ratios (RR) and 95% confidence intervals (CI). A retrospective review of the medical ward database at Kamuzu Central Hospital in Lilongwe, Malawi was conducted between February and December 2013.
Results
There were 3547 patients with an index admission of which 2776 (74.4%) survived and were eligible for readmission. Among these patients: 49.7% were male, mean age was 39.7 years, 36.1% were HIV-positive, 34.6% were HIV-negative, and 29.3% were HIV-unknown. The prevalence of early hospital readmission was 5.5%. Diagnoses associated with 30-day readmission were HIV-positive status (RR = 2.41; 95% CI: 1.64–3.53) and malaria (RR = 0.45; 95% CI: 0.22–0.91). Other factors associated with readmission were multiple diagnoses (excluding HIV) (RR = 1.52; 95% CI: 1.11–2.06), and prolonged length of stay (≥ 16 days) at the index hospitalization (RR = 3.63; 95% CI: 1.72–7.67).
Conclusion
Targeting HIV-infected inpatients with multiple diagnoses and longer index hospitalizations may prevent early readmission and improve quality of care.
Similar content being viewed by others
Background
Delivery of quality healthcare in resource limited settings is an important public health priority. Quality healthcare, defined as safe, effective, patient-centered, timely, efficient, and equitable [1] care is associated with improved patient outcomes [2, 3]. Early hospital readmission (returning within 30 days of discharge from an index hospitalization) is an indicator of healthcare quality [4]. Early readmissions are often avoidable and commonly reflect inadequate or incomplete treatment during the first hospitalization or poor coordination of services at the time of discharge [4,5,6,7]. Early readmissions, which increase healthcare costs and burden individuals, have been well characterized in developed countries [8].
In sub-Saharan Africa, early readmission is not well characterized. A range of quality-related concerns have been described, such as misdiagnosis, poor communication during handover, non-adherence to evidence-based diagnostic and treatment guidelines, and safety violations [9,10,11]. However, few assessments of readmission [12,13,14,15,16,17,18,19,20] have been conducted, and research on such healthcare indicators is needed to guide quality improvement [21].
Additionally, the disease burden in Sub-Saharan Africa differs from developed countries. Importantly, HIV is highly prevalent in the region and many HIV-infected patients experience high morbidity and mortality, even after the scale-up of combination antiretroviral therapy (cART) [22, 23]. In previous assessments of readmission in the region, HIV-infected patients were more likely to be readmitted. However, these assessments did not focus on early readmission [24], were conducted before the introduction of cART rollout [25], or among specific subpopulations [19], before significant ART roll-out. Understanding predictors of early readmission in a large tertiary referral environment after cART rollout is an important area to explore.
At Kamuzu Central Hospital (KCH), a tertiary hospital in Lilongwe, Malawi, we analyzed readmission patterns in the inpatient medicine wards. We described the prevalence of all- cause early readmission, assessed factors associated with early readmission, characterized readmission diagnoses, and explored the impact of HIV/AIDS on all readmission.
Methods
Sample and setting
KCH is a 1000 bed facility that serves a catchment area of 5 million people. Each year 46,000 adults are first admitted to the medical short stay, the triage department for non-trauma related acute cases. From here, most are managed and discharged, and approximately 5000 are admitted to the general medicine wards [26]. The short stay and medical wards are staffed by 9 nurses and 4 medical teams. Each team consists of one consultant, two registrars, one clinical officer, and 2 interns [27].
Admission to the hospital and all medical services are provided at no cost, including medication. An onsite laboratory has the capability for blood cultures, chemistry, transfusion services, microscopic analysis, and testing for common infectious diseases. Radiology services such as x-ray, ultrasound, and CT scans are also available. These diagnostic modalities are on-site, though often unavailable, due to lack of supplies or staff. Lastly, an on campus housing facility is also available for family members or other caretakers, which reduces pressure for discharge from patients or family members.
Routine HIV testing was conducted in the wards by trained HIV testing and counseling (HTC) counselors using opt-out procedures described previously [23]. Briefly, the counselors systematically screened all patients admitted to the wards. Patients with a previous unknown HIV status or a negative HIV test (> 3 months ago) were offered opt-out HTC by the HTC counselor (serial testing with Determine HIV 1/2 and Unigold HIV 1/2) [23, 27]. The results of the test were then recorded in the patient’s file and health passport book.
KCH medical wards database
Patient information was routinely collected in paper patient files. Information from these files was then abstracted by study ward clerks using a paper data abstraction tool. The abstraction tool includes name, age, hospital ID number, gender, date of admission, hospitalization outcome, date of outcome, and select clinical information. Clinical information included HIV status of index admission, HTC result, up to four admission diagnoses (not including HIV), and up to four discharge diagnoses. Data abstractors classified admission and discharge diagnoses into one of sixty common conditions based on clinician notes. One of these diagnoses was sepsis. Due to lack of routine blood culture tests, the diagnosis of sepsis was largely made on clinical grounds. HIV positive patients with a history of fever often received a diagnosis of sepsis if the rapid malaria test was negative, there were no chest findings, and there was improvement with empiric broad spectrum antibiotic treatment. This is the standard of practice in under-resourced healthcare facilities in Malawi. These abstracted data were then entered into the KCH Medical Wards Access database by a research assistant [23].
Identification of readmissions
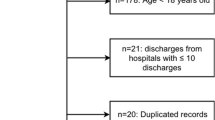
A retrospective review of this database was conducted in February 2014 to determine the prevalence and predictors of readmission. All patients 14 years and older, with an initial admission between February 1, 2013 and November 30, 2013 were included in the analysis. This presumed first hospitalization in the medical ward was defined as an index admission. A readmission was defined as a subsequent hospitalization in the medical ward between February 2 and December 31. Follow-up time was administratively censored on December 31, 2013. It was possible that patients who appeared to be presenting for the first time in early 2013 were actually patients presenting for readmission from a 2012 index admission. In order to assess potential misclassification of the index admission, we conducted a sensitivity analysis excluding all index admissions from February.
Linkage of the index admission and readmission records was conducted manually by study staff and investigators. Two or more database records with identical hospital IDs, names, and ages were considered linked admissions. Records with similar information on these three variables (N = 101/4057, 2.5%) were adjudicated by clinical staff, who often remembered the patients, and a trained research assistant. Typically, if discrepancies seemed like clerical errors, such as reversal of digits or misspellings, the original data abstraction tool or patient file was consulted. Time to readmission was calculated as the number of days between the date of the outcome from the index hospitalization and the date of entry at readmission or censorship at the end of the study period. Readmission of < 30 days were defined as “early readmission,” the primary outcome.
Variables
HIV status was the primary factor of interest. Persons were classified as HIV-infected if an HIV-positive status was known at the time of admission (known positive) or if a new HIV-positive result was documented during the index hospitalization (new positive). HIV-uninfected was defined as known HIV-negative status within three months at the time of admission or a new HIV-negative result documented during the index hospitalization. Patients were classified with an unknown HIV status if the HIV status was unknown at the time of admission and no HIV status was documented during the index hospitalization.
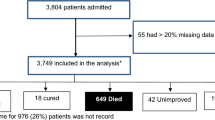
Other variables included in the analysis included age, gender, index hospitalization outcome, index discharge diagnoses, co-morbidity, and length of stay at the index hospitalization. Index and readmission hospitalization outcomes were categorized as discharge, abscond, transfer, or death. Persons who died during the index hospitalization were not included in the readmission analysis (Fig. 1). Multiple diagnoses were classified based on the discharge diagnosis list. This list did not include HIV status. Persons with two or more diagnoses were classified as having multiple diagnoses. Length of stay (LOS) was defined as the time period between the date of admission of the index hospitalization and the date of death, discharge, abscond, or transfer. This variable was categorized as 0–1 day, 2–7 days, 8–15 days, and ≥ 16 days. The ten most prevalent discharge diagnoses were each categorized into dichotomous variables.
Data analyses
Among those at risk for early readmission, we compared the distribution of age, gender, and length of stay by HIV status using chi-squared tests. Risk factors of early readmission were assessed using generalized linear models with a log link and binomial distribution to estimate risk ratios. We implemented unadjusted models and a multivariate adjusted model. To arrive at the adjusted model, we first included all variables that had p-values < 0.2 in unadjusted analysis. We then retained those variables that had p-values < 0.05 in the full multivariate model. Using these same variables, we also conducted an analysis stratified by HIV status (HIV-infected versus HIV-uninfected patients) to assess whether these factors of interest differed by HIV status. Finally, we assessed whether HIV status was associated with mortality at the readmission hospitalization.
We also explored time to readmission beyond thirty days. Kaplan-Meier curves were generated to depict time to readmission by HIV status (negative, positive, and unknown) and compared using log rank tests. We implemented Cox proportional hazards regression models to assess whether factors of interest were associated with time to readmission.
Results
Characteristics
A total of 3547 patients had at least one hospitalization during the 10 months of observation (Fig. 1). Most (N = 2646, 74.8%) were discharged at their index hospitalization, 63 (1.78%) absconded, 60 (1.69%) were transferred, 7 (0.20%) had a missing outcome, and 771 died (21.7%) and were therefore not at risk for readmission. A total of 2776 patients were at risk for readmission (Table 1). Of these patients, the mean age was 39.7 years (SD 16.5), 49.7% were males, and the median LOS was 4 days (IQR, 2–7). Distribution of HIV status was 36.1% HIV-positive, 34.6% HIV-negative, and 29.3% HIV-unknown. The distribution of age, outcome, and length-of-stay differed by HIV status (Table 1).
Early readmission
One hundred fifty three patients (5.5%) experienced an early readmission. Forty six patients had a second readmission, thirteen had a third readmission, five had a fourth readmission, and one had a fifth readmission. Of patients with a second readmission, 18 had a second readmission within 30 days; 6 had a third readmission within 30 days; 1 had a fourth readmission within 30 days. The median time to early readmission was 11 days (IQR, 7–19 days). At the first early readmission, 63.4% were discharged, 34.0% died, and 0.7% absconded at their readmission hospitalization.
Among early readmissions, 84 (55%) were known HIV-infected persons, 8 (5%) were newly diagnosed HIV-infected persons, 34 (22%) were HIV-uninfected, and 27 (18%) had an unknown HIV status. Persons who were HIV-infected were more likely to experience an early readmission (9.2%) than those who were HIV-uninfected (3.5%) or with an unknown HIV status (3.3%) (p < 0.0001).
The ten most prevalent discharge conditions were anemia, malaria, sepsis, pneumonia, heart failure, pulmonary tuberculosis, diabetes, malignancy, acute gastroenteritis, and meningitis (Fig. 2). The readmission rates ranged from 1.8% for malaria to 10% for malignancy. HIV prevalence also varied substantially among readmitted patients with a range of 7.1% among those with malignancy to 100% for sepsis, acute gastroenteritis, and meningitis.
Risk of early readmission
Results of unadjusted and adjusted analyses are reported in Table 2. In the adjusted analysis, age and gender were not associated with risk of early readmission (Table 2). Malaria (RR = 0.45, 95% CI: 0.22, 0.91) was the only clinical diagnosis associated with decreased risk of early readmission. Patients with multiple diagnoses had an increased risk of early readmission (RR = 1.52, 95% CI: 1.11, 2.06) compared to those with only one condition. The longer the LOS at the index admission, the higher the risk of early readmission (RR = 3.63, 95% CI: 1.72, 7.67) comparing ≥ 16 days to ≤ 1 day). When we excluded February readmissions, no coefficient changed by more than 10%, suggesting our results were robust to the index classification.
In analyses stratified by HIV status, we found very similar results to our main analyses (Table 3). Multiple discharge diagnoses remained associated with higher early readmission in HIV-infected patients, although estimates were less precise.
In both unadjusted and adjusted analyses, being HIV-positive was associated with an increased risk of early readmission (RR = 2.60 and RR = 2.41). Patients with an HIV-unknown status had a similar risk of early readmission as HIV-negative patients when adjusted (Table 2). A separate adjusted analysis showed that HIV-positive patients who knew their HIV status at index admission were 2.17 times more likely to have an early readmission compared to those who learned their HIV-positive status at the index hospitalization (95% CI: 1.08, 4.42).
Patients who were HIV-positive were also more likely to have earlier time to readmission than those who were HIV-negative or HIV-unknown status (p < 0.0001) (Fig. 3). The results of unadjusted Cox proportional hazard regression were similar to the unadjusted risk model: HIV positive status (HR = 2.63, 95% CI: 1.96, 3.54), anemia (HR = 1.68, 95% CI: 1.24, 2.27), malignancy (HR = 2.77, 95% CI: 1.74, 4.42), multiple diagnoses (HR = 1.26, 95% CI: 1.00, 1.60), and LOS > 16 days (HR = 2.88, 95% CI: 1.69, 4.91).
Patients who were HIV-positive at early readmission were 1.80 times as likely to die at the readmission visit as those who were HIV-negative (95% CI: 0.95, 3.39). Those with HIV-unknown status were somewhat less likely to die than those who were HIV-negative (RR = 0.62, 95% CI: 0.32, 1.20), but these results were not statistically significant.
Discussion
Our study is among the first to investigate all-cause early readmissions among medicine inpatients in a resource-limited tertiary healthcare facility in Sub-Saharan Africa, in the era of cART rollout. We found that a substantial proportion of patients eligible for readmission were HIV-positive (36.1%) and that these persons were more than twice as likely to experience an early readmission. In addition, HIV-positive patients were readmitted earlier, and were more likely to die at the readmission hospitalization. Multiple diagnoses, and prolonged length of stay during the index hospitalization were also associated with an increased risk of early readmission. The only clinical diagnosis associated with decreased risk of early readmission was malaria.
Our finding that HIV infection is associated with early readmission is consistent with other assessments. HIV infection was found to be associated with readmission among all-cause medicine [24] and pediatric malaria patients in other low-resource settings [19]. Elevated readmission rates were also documented among HIV-infected inpatients in this setting, but prior to ART scale-up [25].
There are a few possible explanations for our findings of elevated readmission for HIV-infected patients. First, HIV is a chronic disease that requires involved management. Patients who are on HAART may experience side effects and toxicity, treatment failures, and immune reconstitution syndrome [24] which may result in readmission. Next, low adherence to treatment predisposes the patient to AIDS-related morbidities [24, 28,29,30,31,32]. Sub-optimal management of such conditions during the initial hospitalization may force HIV-positive patients to return to the hospital shortly after discharge. Another possibility is poor transition of care from the inpatient setting to self-management at home due to weak linkage to outpatient care [33]. Lastly, cessation of therapy post-discharge, due to lack of follow-up, may have led to further deterioration of their medical condition and re-hospitalization. Additional information on disease status and patient management may elucidate the most plausible explanation for this finding. It is necessary to further investigate and identify specific shortcomings in in-hospital practices which contribute to inadequate HIV inpatient care [34].
Multiple diagnoses were also associated with increased risk of early readmission. Multiple diagnoses have been implicated as a predictor for 30-day readmission among general medical patients [35, 36], patients with acute myocardial infarction [37], community acquired pneumonia [38], or heart failure at index hospitalization [39]. Patients with multiple diagnoses are usually more complex. Inadequate management of multiple conditions during hospitalization may lead to complications post-discharge [6, 36]. In addition, the acute illness superimposed on an underlying condition may cause a relapse in the immediate post-hospitalization time period [36]. Lastly, persons in under-resourced settings may experience greater difficulties with management of multiple conditions in an unsupported home environment post-discharge [36]. These challenges with care inside the hospital and transition to self-care at home may amplify chances of readmission.
Prolonged LOS was also associated with increased risk of early readmission. This assumed a dose-response relationship: the longer someone stayed in the hospital, the more likely they were to return. This is comparable to some studies, which have demonstrated a positive relationship [40], and contrasts with other studies which demonstrate an inverse relationship [28, 41, 42]. In our setting, longer LOS in the hospital may be a proxy for delays in the execution of care due to low staff to patient ratios, bed availability, disjointed flow, lack of access to supplies, and other organizational factors that inhibit optimal care [10]. Alternatively, this association could reflect severity of disease or time needed to manage multiple disease conditions, particularly among HIV-infected persons [28].
Readmission rates in developed nations range from 1.1% - 25% [8]. Studies among subpopulations of patients in Africa reported readmission rates between 8.5% - 70% [12,13,14,15,16,17,18,19,20], higher than our 30-day readmission rate of 5.5%. However these studies contain longer readmission intervals up to 1 year, which may help account for the difference.
Similarly, the proportion of HIV-infected patients that were readmitted early (9.2%) in our study was lower than US estimates of over 19% [28,29,30]. A number of reasons may explain the lower than expected readmission rate. Patients in our setting face high barriers to accessing care, such as transport and lack of supportive care outside the hospital, which hinders their return to the hospital [43]. Some patients may have died before they could present for readmission, which may actually reflect a high post-discharge mortality [44]. Next, some patients may have sought care at other facilities, rather than returning to a tertiary facility. Lastly, some may not have been captured due to difficulty with record linkage.
Early readmission is a single indicator that does not provide a complete understanding of quality of care. In fact, the discordance between early readmission and other quality markers, such as 30-day mortality, further underscores the limitations of this indicator [45]. Future studies should assess multiple quality indicators, such as markers of process of care, in conjunction with early readmission [2, 45, 46]. This will more fully inform quality of care and also augment our understanding of specific clinical activities that could be targeted for improvement.
Record linkage was challenging in this setting due to an inconsistent unique identifier. We matched patient records based on hospital ID number, name, and age. Ward clerks and the data personnel were consulted on any possible matches, which were resolved by looking up the file, but some patients may have been erroneously classified. We may have under-estimated or over-estimated early readmission due to missed matches or false matches of readmissions.
There were several analyses that we were not able to conduct. We were not able to conduct a review of patient files to distinguish avoidable versus unavoidable readmissions. Information on factors such as severity of disease during the index hospitalization, measure of comorbidity, cART use and initiation, outpatient follow-up, and patterns of referrals for readmission are needed to understand their impact on readmission.
Markers of quality of inpatient care and hospital discharge practices are lacking in low and middle income countries, particularly for HIV-infected patients [34]. Our study sought to address this knowledge gap with the characterization of early readmissions in a medical facility in a low-resource, high HIV prevalence setting. While the overall frequency of early readmission was low, it provides a reference value for this indicator for similar settings in the region. We learned that interventions to reduce readmission should target inpatients with multiple disease conditions, prolonged LOS during index hospitalization, and HIV infection. The assessment of early readmission provides critical information that can guide strategies to optimize medical care activities and transition of care, particularly for HIV-positive inpatients [34].
Conclusion
The study shows high early hospital readmission amongst HIV positive patients with multiple diagnoses, and prolonged length of stay during the index hospitalization. The study further shows the need to optimize inpatient medical care and linkages to outpatient care to avoid readmission and associated mortality amongst HIV positive patients. Therefore, strategic interventions targeting HIV-infected inpatients with multiple diagnoses and longer index hospitalizations are needed to prevent early readmission and improve quality of care.
Abbreviations
- cART:
-
antiretroviral therapy
- CI:
-
confidence intervals
- HIV:
-
Human Immunodeficiency virus
- HTC:
-
HIV testing and counseling
- KCH:
-
Kamuzu Central Hospital
- LOS:
-
Length of stay
- RR:
-
adjusted risk ratios
References
Institute of Medicine (US) Committee on Quality of Health Care in America. Crossing the quality chasm: a new health system for the 21st century. Washington, DC: National Academies Press; 2001.
Kruk ME, Freedman LP. Assessing health system performance in developing countries: a review of the literature. Health Policy. 2008;85(3):263–76.
Peabody JW, Taguiwalo MM, Robalino DA, et al. Chapter 70, improving the quality of Care in Developing Countries in. In: Jamison DT, Breman JG, Measham AR, Alleyne G, Claeson M, Evans DB, editors. Disease control priorities in developing countries. 2nd ed. Washington D.C: World Bank; 2006. p. 1293–308.
Ashton CM, Del Junco DJ, Souchek J, Wray NP, Mansyur CL. The association between the quality of inpatient care and early readmission: a meta-analysis of the evidence. Med Care. 1997;35(10):1044–59.
Ashton CM, Wray NP. A conceptual framework for the study of early readmission as an indicator of quality of care. Soc Sci Med. 1996;43(11):1533–41.
Halfon P, Eggli Y, van Melle G, Chevalier J, Wasserfallen JB, Burnand B. Measuring potentially avoidable hospital readmissions. J Clin Epidemiol. 2002;55(6):573–87.
Halfon P, Eggli Y, Pretre-Rohrbach I, Meylan D, Marazzi A, Burnand B. Validation of the potentially avoidable hospital readmission rate as a routine indicator of the quality of hospital care. Med Care. 2006;44(11):972–81.
van Walraven C, Bennett C, Jennings A, Austin PC, Forster AJ. Proportion of hospital readmissions deemed avoidable: a systematic review. CMAJ. 2011;183(7):E391–402.
Jha AK, Prasopa-Plaizier N, Larizgoitia I, Bates DW. Patient safety research: an overview of the global evidence. Qual Saf Health Care. 2010;19(1):42–7.
Agyeman-Duah JN, Theurer A, Munthali C, Alide N, Neuhann F. Understanding the barriers to setting up a healthcare quality improvement process in resource-limited settings: a situational analysis at the medical Department of Kamuzu Central Hospital in Lilongwe, Malawi. BMC Health Serv Res. 2014;14(1)
Kalata NL, Kamange L, Muula AS. Adherence to hand hygiene protocol by clinicians and medical students at queen Elizabeth central hospital, Blantyre-Malawi. Malawi Med J. 2013;25(2):50–2.
Schamroth C. Management of acute coronary syndrome in South Africa: insights from the ACCESS (acute coronary events - a multinational survey of current management strategies) registry. Cardiovasc J Afr. 2012;23(7):365–70.
Munywoki PK, Ohuma EO, Ngama M, Bauni E, Scott JA, Nokes DJ. Severe lower respiratory tract infection in early infancy and pneumonia hospitalizations among children, Kenya. Emerg Infect Dis. 2013;19(2):223–9.
Boubaker K, Harzallah A, Ounissi M, Becha M, Guergueh T, Hedri H, et al. Rehospitalization after kidney transplantation during the first year: length, causes and relationship with long-term patient and graft survival. Transplant Proc. 2011;43(5):1742–6.
Shavadia J, Yonga G, Mwanzi S, Jinah A, Moriasi A, Otieno H. Clinical characteristics and outcomes of atrial fibrillation and flutter at the Aga khan university hospital, Nairobi. Cardiovasc J Afr. 2013;24(2):6–9.
Foldès P, Cuzin B, Andro A. Reconstructive surgery after female genital mutilation: a prospective cohort study. Lancet. 2012;380(9837):134–41.
Niehaus DJ, Koen L, Galal U, Dhansay K, Oosthuizen PP, Emsley RA, et al. Crisis discharges and readmission risk in acute psychiatric male inpatients. BMC Psychiatry. 2008;8(44):8–44.
Moïsi JC, Gatakaa H, Berkley JA, Maitland K, Mturi N, Newton CR, et al. Excess child mortality after discharge from hospital in Kilifi, Kenya: a retrospective cohort analysis. Bull World Health Organ. 2011;89:725–32.
Malamba S, Hladik W, Reingold A, Banage F, McFarland W, Rutherford G, et al. The effect of HIV on morbidity and mortality in children with severe malarial anaemia. Malar J. 2007;6:143.
Sliwa K, Davison BA, Mayosi BM, Damasceno A, Sani M, Ogah OS, et al. Readmission and death after an acute heart failure event: predictors and outcomes in sub-Saharan Africa: results from the THESUS-HF registry. Eur Heart J. 2013;34(40):3151–9.
Maru DS, Andrews J, Schwarz D, Schwarz R, Acharya B, Ramaiya A, et al. Crossing the quality chasm in resource-limited settings. Glob Health. 2012;8:41.
UNAIDS. Global report: UNAIDS report on the global AIDS epidemic 2013. Geneva, Switzerland: UNAIDS; 2013. Available online at: http://www.who.int/hiv/pub/me/unaids_global_report/en.
Kendig CE, McCulloch DJ, Rosenberg NE, Samuel JC, Mabedi C, Shores CG, et al. Prevalence of HIV and disease outcomes on the medical and surgical wards at Kamuzu central hospital, Lilongwe, Malawi. Trop Med Health. 2013;41(4):163–70.
Stanley A, Graham N, Parrish AA. Review of internal medicine re-admissions in a peri-urban south African hospital. S Afr Med J. 2008;98(4):291–4.
Kelly PM, Cumming RG, Kaldor JM. HIV and tuberculosis in rural sub-Saharan Africa: a cohort study with two year follow-up. Trans R Soc Trop Med Hyg. 1999;93(3):287–93.
Akinkuotu A, Roemer E, Richardson A, Namarika DC, Munthali C, Bahling A, et al. In-hospital mortality rates and HIV: a medical ward review, Lilongwe, Malawi. Int J STD AIDS. 2011;22(8):465–70.
SM LC, Chester FM, Matoga M, Munthali C, Nsona D, Haac B, et al. Implementation of routine counselor-initiated opt-out HIV testing on the adult medical ward at Kamuzu central hospital, Lilongwe, Malawi. J Acquir Immune Defic Syndr. 2015; [Epub ahead of print]
Berry SA, Fleishman JA, Yehia BR, Korthuis PT, Agwu AL, Moore RD, et al. Thirty-day hospital readmission rate among adults living with HIV. AIDS. 2013;27(13):2059–68.
Nosyk B, Sun H, Li X, Palepu A, Anis AH. Highly active antiretroviral therapy and hospital readmission: comparison of a matched cohort. BMC Infect Dis. 2006;6:146.
Nijhawan AE, Clark C, Kaplan R, Moore B, Halm EA, Amarasingham R. An electronic medical record-based model to predict 30-day risk of readmission and death among HIV-infected inpatients. J Acquir Immune Defic Syndr. 2012;61(3):349–58.
Palepu A, Sun H, Kuyper L, Schechter MT, O'Shaughnessy MV, Anis AH. Predictors of early hospital readmission in HIV-infected patients with pneumonia. J Gen Intern Med. 2003;18(4):242–7.
Grant RW, Charlebois ED, Wachter RM. Risk factors for early hospital readmission in patients with AIDS and pneumonia. J Gen Intern Med. 1999;14(9):531–6.
Rosen S, Fox MP. Retention in HIV care between testing and treatment in sub-Saharan Africa: a systematic review. PLoS Med. 2011;8(7):e1001056.
Ahonkhai AA, Bassett IV, Ferris TG, Freedberg KA. Improving HIV outcomes in resource-limited countries: the importance of quality indicators. BMC Health Serv Res. 2012;12:427.
Silverstein MD, Qin H, Mercer SQ, Fong J, Haydar Z. Risk factors for 30-day hospital readmission in patients >/=65 years of age. Proc (Bayl Univ Med Cent). 2008;21(4):363–72.
Donze J, Lipsitz S, Bates DW, Schnipper JL. Causes and patterns of readmissions in patients with common comorbidities: retrospective cohort study. BMJ. 2013;347:f7171.
Dunlay SM, Weston SA, Killian JM, Bell MR, Jaffe AS, Roger VL. Thirty-day rehospitalizations after acute myocardial infarction: a cohort study. Ann Intern Med. 2012;157(1):11–8.
Jasti H, Mortensen EM, Obrosky DS, Kapoor WN, Fine MJ. Causes and risk factors for rehospitalization of patients hospitalized with community-acquired pneumonia. Clin Infect Dis. 2008;46(4):550–6.
Au AG, McAlister FA, Bakal JA, Ezekowitz J, Kaul P, van Walraven C. Predicting the risk of unplanned readmission or death within 30 days of discharge after a heart failure hospitalization. Am Heart J. 2012;164(3):365–72.
Hasan O, Meltzer DO, Shaykevich SA, Bell CM, Kaboli PJ, Auerbach AD, et al. Hospital readmission in general medicine patients: a prediction model. J Gen Intern Med. 2010;25(3):211–9.
Carey K, Lin MY. Hospital length of stay and readmission: an early investigation. Med Care Res Rev. 2014;71(1):99–111.
Kaboli PJ, Go JT, Hockenberry J, Glasgow JM, Johnson SR, Rosenthal GE, et al. Associations between reduced hospital length of stay and 30-day readmission rate and mortality: 14-year experience in 129 veterans affairs hospitals. Ann Intern Med. 2012;157(12):837–45.
Govindasamy D, Ford N, Kranzer K. Risk factors, barriers and facilitators for linkage to antiretroviral therapy care: a systematic review. AIDS. 2012;26(16):2059–67.
Bassett IV, Wang B, Chetty S, Mazibuko M, Bearnot B, Giddy J, et al. Loss to care and death before antiretroviral therapy in Durban, South Africa. J Acquir Immune Defic Syndr. 2009;51(2):135–9.
Press MJ, Scanlon DP, Ryan AM, Zhu J, Navathe AS, Mittler JN, et al. Limits of readmission rates in measuring hospital quality suggest the need for added metrics. Health Aff (Millwood). 2013;32(6):1083–91.
Catumbela E, Certal V, Freitas A, Costa C, Sarmento A, da Costa Pereira A. Definition of a core set of quality indicators for the assessment of HIV/AIDS clinical care: a systematic review. BMC Health Serv Res. 2013;13:236.
Acknowledgements
We would like to thank the study ward clerks, Swinthurn Chiomole and Albert Mulozowa, for their support with data acquisition.
Funding
NER was supported by the National Institutes of Health (K99 MH104154-01A1, R25 TW009340, and P30 AI50410).
Availability of data and materials
The full data set supporting the conclusions of this article is held by the authors and can be made available on request.
Author information
Authors and Affiliations
Contributions
KSC,CK, NER, and MCH - conception, design, analysis and interpretation of data, drafting and revision of the drafts; CS – data analysis; MM and CK – conception and acquisition of data; AM and JN – acquisition of data. All provided final approval.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval was obtained from the Malawi National Health Science Research Committee and the University of North Carolina Medical School institutional review board. This analysis used de-identified data from KCH Ward Database. The review boards above exempt formal consenting when analyzing retrospective, de-identified, existing data. Administrative permission to access and use the KCH medical ward database was obtained from the hospital’s director.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Chawla, K.S., Rosenberg, N.E., Stanley, C. et al. HIV and early hospital readmission: evaluation of a tertiary medical facility in Lilongwe, Malawi. BMC Health Serv Res 18, 225 (2018). https://doi.org/10.1186/s12913-018-3050-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-018-3050-9