Abstract
Background
Falls during hospitalization harbor both clinical and financial outcomes. The modified Morse fall scale [MMFS] is widely used for an in-hospital risk-of-fall assessment. Nevertheless, the majority of patients at risk of falling, i.e. with high MMFS, do not fall. The aim of this study was to ascertain our study hypothesis that certain patients' characteristics (e.g. serum electrolytes, usage of a walking device etc.) could further stratify the risk of falls among hospitalized patients with MMFS.
Methods
This was a retrospective cohort analysis of adult patients hospitalized in Internal Medicine departments.
Results
The final cohort included 428 patients aged 76.8±14.0 years. All patients had high (9 or more) MMFS upon admission, and their mean MMFS was 16.2±6.1. A group of 139 (32.5%) patients who fell during their hospitalization was compared with a control group of 289 (67.5%) patients who did not fall. The fallers had higher MMFS, a higher prevalence of mild dependence, and a greater use of a cane or no walking device. Regression analysis showed the following patients' characteristics to be independently associated with an increased risk of falling: mild dependence (OR=3.99, 95% CI 1.97-8.08; p<0.0001), treatment by anti-epileptics (OR=3.9, 95% CI 1.36-11.18; p=0.011), treatment by hypoglycemic agents (OR=2.64, 95% CI 1.08-6.45; p= 0.033), and hypothyroidism (OR=3.66, 05%CI 1.62-8.30; p=0.002). In contrast to their role in the MMFS, the use of a walker or a wheelchair was found to decrease the risk of falling (OR=0.3, 95% CI 0.13-0.69; p=0.005 and OR=0.25, 95% CI 0.11-0.59; p= 0.002).
Conclusions
Further risk stratification of hospitalized patients, already known to have a high MMFS, which would take into account the characteristics pointed out in this study, should be attained.
Similar content being viewed by others
Background
Falling during hospitalization is a common phenomenon among hospitalized patients, becoming more frequent and hazardous among the elderly and the frail [1, 2]. Many efforts are being made worldwide to find the best means for fall-prevention and a better assessment of the risk of falling during a hospital stay [3]. Nevertheless, falls are still a major public-health concern [2]. Accordingly, there is an ongoing effort for the development of risk assessment tools in order to identify patients with an increased risk of falling as soon as they are hospitalized.
One of the commonly used risk assessment tools is the modified Morse fall scale [4, 5]. All of the patients at the Sheba Medical Center are assessed for a fall risk upon admission by the nurses who use a modified Morse fall scale (MMFS), as presented in Table 1. This version of the MMFS [4] consists of the patient's demographics, background diagnoses, therapeutic agents, functional status, cognition, and other characteristics potentially affecting the risk of falling. It is a detailed version of the MMFS that was adjusted to application in a major, tertiary medical center. For example, the "Use of major tranquilizers" in the MMFS was specifically translated to "undergoing general anesthesia during the previous 24 hours". Patients with high (9 or more) modified Morse fall scale scores are considered to have a higher risk of falling, and accordingly, preventive measures are used in these patients, including instructing them how to avoid obstacles in the hospital, which shoes to wear, and how to call a nurse when getting out of bed at night.
Many patients, especially the elderly frail patients, are considered to be at a high risk of falling according to the modified Morse scale, but only a minority of these will actually fall during their hospital stay, as shown previously in sensitivity analysis (including specificity, positive predictive value (PPV), negative predictive value (NPV) and accuracy) [6]. Our goal, in the present study, was to ascertain our study hypothesis that certain patients' characteristics (some relating to demographics and co-morbidities like hypothyroidism and smoking status, some addressing laboratory parameters like sodium and potassium blood concentrations, some addressing chronic medication like anti-epileptics and some other clinical data like usage of a walking device; fully specified in Table 2) could further stratify the risk of falls among hospitalized patients with MMFS.
Methods
This was a historical prospective study conducted at the Sheba Medical Center, a large tertiary medical center. An institutional ethics committee, approved the study prior to its data collection. Need for consent was waived by the ethics committee.
The study group included all patients who had been admitted to all seven Internal Medicine departments at the Sheba Medical Center during 2013 who also had high modified Morse Fall Scale scores [5] upon admission and also fell during their hospitalization. In the case of readmissions, only the first admission was included in the analysis. The control group included random patients who had been admitted to a single internal medicine department (Internal Medicine T) at the Sheba Medical Center during 2013 who also had high modified Morse Scale scores upon admission but did not fall during their hospital stay. Falls definition was consistent with the Tinetti’s definition: “an event which results in a person coming to rest unintentionally on the ground or other lower level, not as a result of a major intrinsic event (such as stroke) or an overwhelming hazard” [7].
The patients' electronic medical charts were reviewed for the following data: age (years); male gender (yes/no); various chronic co-morbidities (yes/no); living in a nursing home (yes/no); walking device used (either cane/walker/wheelchair); independence in basic activities of daily living (BADL) according to the Katz index [8]; a history of falls during the six months prior to their admission; laboratory findings upon admission whose anomalies might be associated with weakness, falls, and frailty (including hemoglobin blood levels [9], albumin serum levels [10], urea and creatinine serum levels [11], Alanine aminotransferase serum levels [12], and electrolyte serum levels); a list of medications used during hospitalization which might be associated with weakness and falls (anti-Parkinson medications, benzodiazepines, diuretics, anti-epileptics, opiates, statins, oral hypoglycemic agents, insulin, nitrates, neuroleptics, steroids, anti-depressants [13,14,15,16]; and the modified Morse fall scale scores upon admission [5]. Fall events in this cohort, like all other hospitalized patients in our medical center, were reported within 24 hours of event to the unit of patient safety and risks management. This was the data base from which we recorded events of falling.
Continuous variables were expressed as a mean ± standard deviation, median, and inter-quartile range (IQR). The student's t-test was used to compare between the mean values of continuous variables with parametric distributions, and the Mann–Whitney test was used to compare between the mean values of continuous variables with non-parametric distributions. The Fisher's exact test was used to compare between the incidence and the prevalence of categorical variables. A multivariate binary logistic regression analysis with an enter method was used to study which variables were independently associated with in-hospital falls. All variables in the univariate analysis (Table 2) were included in the regression model (Table 3). A receiver-operating characteristic (ROC) curve was used to study how the modified Morse Fall Scale scores (of 9 or more) predict in-hospital falls. Thereafter, a second ROC curve was used to study how all the variables in Table 3 (including the modified Morse Fall Scale scores) together predict in-hospital falls. The area under the second ROC curve was calculated using the probability for in-hospital falls and the actual binary outcome (in-hospital falls).
Two-tailed p<0.05 was considered statistically significant. The statistical analyses were carried out using the 24th version of the SPSS statistical software (SPSS Inc., Chicago, IL, USA).
Results
The final cohort included 428 patients: 218 (50.9%) women and 210 (49.1%) men. The mean age was 76.8±14.0 years (median: 80 years; IQR: 70–86 years) and the mean Modified Morse falls scores was 16.2±6.1 (median: 16; IQR: 11–19). The three most prevalent chronic co-morbidities were: hypertension, ischemic heart disease, and diabetes mellitus. The baseline patients' characteristics are detailed in Table 2.
The study group included 139 (32.5%) patients (fallers) and the control group included 289 (67.5%) patients (non-fallers). Among fallers, most (n=95; 68.3%) of the patients fell in their room, and the rest fell in the bathroom or in the corridor. The mean admission-to-fall time was 6.1±16.9 days (median: 2 days; IQR: 1–6 days). All of the fallers were examined by a physician immediately following the event, and 16 (11.5%) patients also underwent imaging studies or were referred to further consultation.
Compared with non-fallers, fallers had higher modified Morse Scores, a higher prevalence of mild dependence, and a higher use of a cane or no walking device, a higher prevalence of smoking, lower calcium serum levels, lower potassium serum levels, and a higher rate of treatment with anti-epileptics.
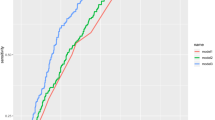
A regression analysis, as detailed in Table 3, showed that except for higher Morse Fall scores, mild dependence, the use of anti-epileptics, the use of oral hypoglycemic agents and hypothyroidism were independently associated with an increased risk of an in-hospital fall. On the other hand, in contrast to their role in the modified Morse scores, the use of a walker or a wheelchair was found to decrease the risk of falling (OR=0.3, 95% CI 0.13-0.69; P = 0.005 and OR=0.25, 95% CI 0.11-0.59; P = 0.002 respectively). Higher potassium serum levels and atrial fibrillation were also found to be independently associated with a decreased risk of an in-hospital fall. A receiver operating characteristic (ROC) curve analysis showed that Morse Fall Scale scores fairly predicts in-hospital falls even when they are 9 or higher (Fig. 1a). Nevertheless, According to the ROC curve presented, in patients with a modified MORSE scale score of 9 or more, the ideal cutoff to predict falls would be 14. The model that included all the variables presented in Table 3 even better predicted in-hospital falls (Fig. 1b).
Discussion
Along with the substantial health sequel of falls, an enormous economic burden results from in-hospital falls and their direct consequences – particularly in the elderly population [17,18,19,20]. Accordingly, substantial efforts are being made world-wide to minimize the risk of falls during hospital stays [18]. A pillar of these efforts is the ability to predict upon the hospital admission the risk of falls for each admitted patient. The modified Morse scale is a widely-used tool for this reason and is thus, widely accepted. Nevertheless, we have noted that there is a huge population of patients which are classified, according to the modified Morse scale, as being at a high risk of falling, but only a minority of them actually fall during their hospital stay. Therefore, we have sought to further stratify this population of high modified Morse score patients (a version applicable to a tertiary, multidisciplinary medical center, as detailed previously in the introduction chapter) aiming at the isolation of the patients' characteristics which could improve our prediction of in-hospital falls.
Contrary to the modified Morse scale score equation, in the current analysis the use of a wheelchair or a walker has been associated with a decreased risk of falling during the hospital stay. This finding is surprising since in previous studies the use of a wheelchair or a walker has been associated with increased risk of falling [21], mainly in nursing-home residents [22]. It is possible, that during the hospital stay, their spouses and their caregivers look after them more intensively since they were using a wheelchair or a walker. This finding could be further investigated in the two following alternative ways: these variables could either have an opposite influence on the summation of a risk in the modified Morse scale score (a reduction of one point rather than adding one point to the total sum), or it could be omitted from the score. In either case, we assume that the modified Morse scale score could be more accurate than the way it is utilized today.
Atrial fibrillation, usually associated with impaired mobility in the elderly [23], is actually associated with reduced risk of falling in the current analysis. This unexpected finding is probably explained by the fact that most of these patients have been hooked-up to an over-head monitor during their hospital stay. The way that this fact should be incorporated into the risk score assessment should be further investigated and discussed.
Anti-epileptic drugs might be sedative and are associated with falls in the elderly [24] as are thyroid disorders [25]. According to our findings, the use of anti-epileptic drugs and hypothyroidism should be incorporated into the future developed scores for a risk assessment and accordingly, should be prospectively assessed.
The main limitation of the study is its small size - being a single-center study. These two drawbacks restrict the potential of generalizing our findings to larger patients' populations. In order to overcome this limitation, the study group has included all patients who have been admitted to all seven Internal Medicine departments at the Medical Center, and the control group has been twice larger. The current cohort size has allowed us to conduct a population-based multivariate analysis and still, larger cohorts should also be tested since it is possible that our final model overestimates the regression coefficients due to a low number of falls per independent variable. The retrospective nature of the study is another limitation due to a myriad of confounding factors that were not controlled in this type of study. Accordingly, prospective studies should be conducted in order to ascertain the findings of our research.
Conclusions
The burden of comorbidities and the complex nature of both acute and chronic conditions for which elderly patients are admitted to hospitals are constantly growing. Therefore, it is only prudent to say that the problem of in-hospital falls will continue to grow. The parameters found in this study as potentially reducing or increasing the accuracy of the modified Morse score should be investigated in prospective studies.
Abbreviations
- IQR:
-
Inter-quartile range
- MMFS:
-
Modified morse fall scale
- ROC:
-
Receiver operating characteristic
References
Severo IM, Almeida M de A, Kuchenbecker R, DFVB V, Weschenfelder ME, LRC P, et al. Risk factors for falls in hospitalized adult patients: an integrative review. Rev Esc Enferm USP [Internet]. 2014;48(3):540–54. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25076284.
Neyens JCL, Dijcks BPJ, Twisk J, Schols JMGA, van Haastregt JCM, van den Heuvel WJA, et al. A multifactorial intervention for the prevention of falls in psychogeriatric nursing home patients, a randomised controlled trial (RCT). Age Ageing [Internet]. 2009;38(2):194–9. Available from: http://ageing.oxfordjournals.org/content/38/2/194.full.
Spoelstra SL, Given BA, Given CW. Fall prevention in hospitals: an integrative review. Clin Nurs Res [Internet]. 2012;21(1):92–112. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21862700.
McFarlane-Kolb H. Falls risk assessment, multitargeted interventions and the impact on hospital falls. Int J Nurs Pract. 2004;10(5):199–206. Available from: http://www.ncbi.nlm.nih.gov/pubmed/15461689.
Morse JM. The modified Morse Fall Scale. Int J Nurs Pract [Internet]. 2006;12(3):174–5. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16674785.
Schwendimann R, De Geest S, Milisen K. Evaluation of the Morse Fall Scale in hospitalised patients. Age Ageing. Oxford University Press; 2006 ;35(3):311–3. Available from: https://academic.oup.com/ageing/article-lookup/doi/10.1093/ageing/afj066.
Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med [Internet]. 319(26):1701–7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/3205267.
Katz S. Assessing self-maintenance: activities of daily living, mobility, and 297 instrumental activities of daily living. J Am Geriatr Soc. 1983;31(12):721–7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/6418786.
Penninx BWJH, Pluijm SMF, Lips P, Woodman R, Miedema K, Guralnik JM, et al. Late-life anemia is associated with increased risk of recurrent falls. J Am 302 Geriatr Soc [Internet]. 2005;53(12):2106–11. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16398894.
Vellas B, Baumgartner RN, Wayne SJ, Conceicao J, Lafont C, Albarede JL, et al. Relationship between malnutrition and falls in the elderly. Nutrition [Internet]. 2016;2:105–8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/1591453.
Dukas LC, Schacht E, Mazor Z. A new significant and 309 independent risk factor for falls in elderly men and women: a low creatinine 310 clearance of less than 65 ml/min. Osteoporos Int [Internet]. 2005;16(3):332–8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/15241585.
Ramaty E, Maor E, Peltz-Sinvani N, Brom A, Grinfeld A, Kivity S, et al. Low ALT blood levels predict long-term all-cause mortality among adults. A historical prospective cohort study. Eur J Intern Med [Internet]. 2014;25(10):919–21. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25468741.
Huang AR, Mallet L, Rochefort CM, Eguale T, Buckeridge DL, Tamblyn R. Medication-related falls in the elderly: causative factors and preventive strategies. Drugs Aging [Internet]. 2012;29(5):359–76. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22550966.
Scott D, Blizzard L, Fell J, Jones G. Statin therapy, muscle function and falls risk in community-dwelling older adults. QJM [Internet]. 2009;102(9):625–33. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19633029.
Schwartz AV, Vittinghoff E, Sellmeyer DE, Feingold KR, de Rekeneire N, Strotmeyer ES, et al. Diabetes-related complications, glycemic control, and falls in older adults. Diabetes Care [Internet]. 2008;31(3):391–6. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=2288549&tool=pmcentrez&rendertype=abstract.
Cumming RG. Epidemiology of medication-related falls and fractures in the elderly. Drugs Aging [Internet]. 1998;12(1):43–53. Available from: http://www.ncbi.nlm.nih.gov/pubmed/9467686.
Barker AL, Morello RT, Ayton DR, Hill KD, Landgren FS, Brand C, A. Development of an implementation plan for the 6-PACK falls prevention programme as part of a randomised controlled trial: protocol for a series of preimplementation studies. Inj Prev [Internet]. 2016; Available from: http://www.ncbi.nlm.nih.gov/pubmed/26932835.
Schwendimann R, Bühler H, De Geest S, Milisen K. Falls and consequent injuries in hospitalized patients: effects of an interdisciplinary falls prevention program. BMC Health Serv Res [Internet]. 2006;6:69. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1534028&tool=pmcentrez&rendertype=abstract.
Hitcho EB, Krauss MJ, Birge S, Claiborne Dunagan W, Fischer I, Johnson S, et al. Characteristics and circumstances of falls in a hospital setting: a prospective analysis. J Gen Intern Med [Internet]. 2004;19(7):732–9. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1492485&tool=pmcentrez&rendertype=abstract.
Bates DW, Pruess K, Souney P, Platt R. Serious falls in hospitalized patients: correlates and resource utilization. Am J Med [Internet]. 1995;99(2):137–43. Available from: http://www.ncbi.nlm.nih.gov/pubmed/7625418.
Stevens JA, Thomas K, Teh L, Greenspan AI. Unintentional fall injuries associated with walkers and canes in older adults treated in U.S. emergency departments. J Am Geriatr Soc [Internet]. 2009;57(8):1464–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19555423.
Kiely DK, Kiel DP, Burrows AB, Lipsitz LA. Identifying nursing home residents at risk for falling. J Am Geriatr Soc [Internet]. 1998;46(5):551–5. Available from: http://www.ncbi.nlm.nih.gov/pubmed/9588366.
Donoghue OA, Jansen S, Dooley C, De Rooij S, Van Der Velde N, Kenny RA. Atrial fibrillation is associated with impaired mobility in community-dwelling older adults. J Am Med Dir Assoc [Internet]. 2014;15(12):929–33. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25294620.
Deandrea S, Lucenteforte E, Bravi F, Foschi R, La Vecchia C, Negri E. Risk Factors for Falls in Community-dwelling Older People. Epidemiology [Internet]. 2010;21(5):658–68. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20585256.
von Heideken WP, Gustafson Y, Kallin K, Jensen J, Lundin-Olsson L. Falls in very old people: the population-based Umeå 85+ study in Sweden. Arch Gerontol Geriatr [Internet]. 2016;49(3):390–6. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19144414.
Acknowledgements
Only the authors mentioned were involved in study design, data collection and analysis. No external members were involved in this study.
Funding
There is no funding information to disclose.
Availability of data and materials
The datasets generated during and/or analyzed during the current study are not publicly available in accord with the IRB regulations.
Author information
Authors and Affiliations
Contributions
All authors had a significant contribution to the study design, data collection and manuscript production: IG was involved in study design, data collection, data analysis and manuscript writing; YS was involved in study design and data collection, II was involved in study design and data collection, DF was involved in data collection and data analysis; NPS was involved in study design and data collection; DJ was involved in study design, data collection, data analysis and manuscript writing; GS was involved in study design, data collection, data analysis and manuscript writing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The institutional ethics committee of the Chaim Sheba medical center, affiliated to the Sackler School of medicine, Tel-Aviv University, approved the study prior to its data collection (Approval ID 0858-13-SMC).
This was a retrospective study and therefore, consent was irrelevant.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Gringauz, I., Shemesh, Y., Dagan, A. et al. Risk of falling among hospitalized patients with high modified Morse scores could be further Stratified. BMC Health Serv Res 17, 721 (2017). https://doi.org/10.1186/s12913-017-2685-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-017-2685-2