Abstract
Background
To assess the use of updated comorbidity information over time on ability to predict mortality among adults with newly diagnosed hypertension.
Methods
We studied adults 18 years and older with an incident diagnosis of hypertension from Alberta, Canada. We compared the prognostic performance of Cox regression models using Charlson comorbidities as time-invariant covariates at baseline (TIC) versus models including Charlson comorbidities as time-varying covariates (TVC) using Akaike Information Criterion (AIC) for testing goodness of fit.
Results
The strength of the association between important prognostic clinical variables and mortality varied by modeling technique; for example, myocardial infarction was less strongly associated with mortality in the TIC model (Hazard Ratio 1.07; 95% Confidence Interval (CI): 1.05 to 1.1) than in the TVC model (HR 1.20; 95% CI: 1.18 to 1.22). All TVC models slightly outperformed TIC models, regardless of the method used to adjust for comorbid conditions (individual Charlson Comorbidities, count of comorbidities or indices). The TVC model including all 17 Charlson comorbidities as individual independent variables showed the best fit and performance.
Conclusion
Accounting for changes in patient comorbidity status over time more accurately captures a patient’s health risk and slightly improves predictive model fit and performance than traditional methods using TIC assessment.
Similar content being viewed by others
Background
Comorbidity is an important component of individual risk and health status. It has been shown to be an important determinant of health care utilization, predictor of health outcomes and mortality. Studies using large administrative data-based cohorts to predict death have historically adjusted for individual risk on the basis of comorbidities present at baseline [1, 2]. However, disease severity, and the presence and progression of comorbidities, is not static. Risk adjustment for comorbidities often ignores the nature of disease progress in the observational period. Little is known about how comorbidities developing during follow-up and/or how changes in disease severity over time impact the ability to predict important outcomes such as mortality.
The Charlson comorbidity index (CCI) [3] was developed as a prognostic classification and weighting methodology that predicts mortality based on disease burden. Short-term studies predicting 30-day and 1-year mortality using time-invariant baseline Charlson comorbidities adjustment have shown good performance. Recent studies suggest that predictive models solely relying on baseline measures of comorbidity may be less accurate in longer follow-up studies where novel conditions or changes in disease severity are more likely to occur [2, 4–6]. However, few studies account for changes in disease state after baseline and there is contradictory evidence about the value of time-varying effects in prognostic model performance [1, 7].
The purpose of this study was to determine whether predictive models accounting for changes in patient comorbidity status over time may more accurately capture a patient’s health risk and better predict long-term survival than models using only baseline measures of comorbidity.
Methods
Data sources
Administrative databases used in the study included: (1) Hospital discharge abstracts (DAD), (2) the Alberta Health Care Insurance Plan (AHCIP) registry, (3) Physician billing claims, and (4) vital statistics. Clinical visit information for all patients discharged from Alberta hospitals is abstracted and recorded. Clinical information in DAD includes up to 16 possible diagnoses abstracted using International Classification of Disease (ICD), 9th Revision (i.e., ICD-9), ICD-9 Clinical Modification (ICD-9-CM) and up to 25 possible diagnoses abstracted using ICD-10 Canadian Modification (i.e., ICD-10-CA) [8]. The AHCIP includes individually identifiable demographic information (Personal Health Number (PHN), date of birth, sex, and postal code) for all Alberta residents eligible to receive universally covered healthcare services. Physician fee-for-service and shadow billing claims submitted to the provincial government includes information on type of provider, patient and clinic information, with at least one, but up to three, ICD-9 diagnostic codes for both outpatient as well as inpatient hospital services provided by Alberta physicians to eligible Albertans who have registered under the AHCIP.
Study population
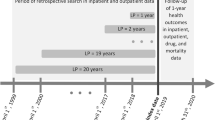
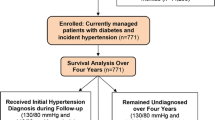
The study population included all adults aged 18 years and older who were residents of the Province of Alberta and newly diagnosed with hypertension. We identified individuals with hypertension, using relevant ICD-9 (401.x, 402.x, 403.x, 404.x, or 405.x) and ICD-10-CA codes (I10.x, I11.x, I12.x, I13.x, or I15.x), and assigned the earliest date of a physician visit or hospital separation as the index date using methods previously described [9]. We excluded patients with an index date between April 1, 1994 and March 31, 1997 (the washout period), thereby focusing on patients newly diagnosed with hypertension between April 1, 1997 and March 31, 2009. We excluded patients from the study if they met any of the following criteria: 1) hypertensive patients diagnosed in the washout period (between April 1, 1994 and March 31, 1997); 2) patients with myocardial infarction, heart failure or stroke during the 3 years leading up to the study or within 30 days following the diagnosis of hypertension; 3) patients who died the same day that they were diagnosed with hypertension; 4) patients with less than 1-year of follow.
Outcome and independent variables
The outcome variable was all-cause mortality between April 1, 1997 and March 31, 2009. We followed patients from diagnosis until death or the end of the study (March 31, 2010). We measured survival time from the date of the initial hypertension diagnosis to the date of death or the last observation date and censored observations at the AHICP coverage end date or study end date of March 31, 2010 if death did not occur. Deaths were identified from Vital Statistics [10].
The primary independent variables were the 17 Charlson comorbidities present at baseline (included in both time-invariant covariate (TIC) and in time-varying covariate (TVC) analyses) or developing between April 1 1997 and March 31 2009 (included only in TVC analysis). We obtained comorbidity data from the physician claims and DAD databases and age and sex information from the APCIP. We assigned median household income quintiles (lowest quintile Q1 to highest quintile Q5), a proxy for socioeconomic status, and rural or urban residential location based on their residential postal code, mapped to 2006 Statistics Canada Census data [11].
The onset of a patient’s disease comorbidity was determined as the earliest date of diagnosis obtained from DAD or physician claims data following a patient’s index of hypertension diagnosis date. If more than one record was identified for the same condition, we chose the first date of encounter as date of the chronic condition. In TVC models, we used the last observation carried forward approach. Once identified, each condition was considered ongoing, with models capturing onset of comorbidity in their original form along with time at risk in the period between diagnosis and the remainder of the study [1].
Statistical analysis
We used descriptive statistics to summarize data on age, sex, socio-economic status and area of residence. We analyzed survival data using the Kaplan-Meier method and Cox Regression, and tested associations using the log-rank test and Wald test with two-sided P < 0.05 as statistical significance level. We calculated crude hazard ratios (cHR) and adjusted hazard ratios (aHR) using non-disease reference populations for Cox’s regression models and reported 95% Confidence Intervals (95% CI) as a measure of uncertainty around each estimate.
We used four methods to adjust for patient case-mix for both TIC and TVC models along with other potential confounders including age, sex, median household income, and area of residence. These four methods included 1) 17 individual Charlson comorbidities, 2) the original Charlson comorbidity index summary score, 3) an updated Charlson comorbidity index summary score using 12 of the original 17 comorbidities and 4) a count of Charlson comorbidities [12].
We studied the slope of the line of the Schoenfeld residuals over time to verify that the hazard proportionality assumption was met. Because of the large sample size, we excluded violations if the coefficient of the slope was within the pre-specified range of 0 ± 0.05, regardless of whether it was statistically significantly different from zero. In sensitivity analyses we checked if the log-hazard ratios differed by more than 10% when time was split in quarterly segments.
We fit eight multivariate prognostic survival models controlling for a standard set of confounding variables; one set of TIC and one set of TVC Models using standard Cox regression including each of all four methods described above. Each Cox regression included one condition such as myocardial infarction (presence or absence). We compared model fit using the Akaike Information Criterion (AIC), which does not require the models under comparison to be nested. Generally, improved model performance (better fit and parsimony) is supported by a decrease in the AIC score [13].
Results
Between April 1 1997 and March 31 2009, 456,263 newly diagnosed Alberta hypertensive patients were identified. After excluding those who had died on date of diagnosis (n = 2529), there were 453,734 patients. Patients predominantly lived in urban areas (80.7%) and 50.6% were male. The median age was 57.5 and 67.9% were younger than 65 years. There were 29,717 (6.5%) patients missing median income information and 1255 (.27%) patients with missing residence information. Missing data on these variables were included in the analysis. During the follow-up (a median follow-up time of 5.75 years, inter-quartile range (IQR) 5.74 to 5.76 years) 72,490 died and mortality was 15.98% (95% CI: 15.86 to 16.01) (Table 1).
The prevalence of the 17 Charlson Comorbidities differed substantially between baseline and the end of the study period (Table 2), increasing from 36.8% of patients with at least one comorbid condition to 60.4% at the end of study. The prevalence for each comorbidity increased substantially during the study period, from 1.74 times (chronic obstructive pulmonary disease) to 3.81 times (metastatic solid tumors).
Because mortality was relatively low in this cohort, there was no death in some subgroups. In fact, while the crude analysis showed that patient survival was affected by all 21 independent variables, we calculated survival time for 10 comorbidity-defined subgroups. Conditions not reaching a reportable endpoint had median survival longer than the 12-year study follow-up. Comorbidities associated with the shortest median survival time included metastatic solid tumors (n = 4784, 2.17 years, 95% CI 1.97-2.39), dementia (n = 8890, 3.67 years, 95% CI 3.58-3.79) and moderate or severe liver disease (n = 968, 4.10 years, 95% CI 3.72-5.15) years. Comorbidities associated with increased mortality included hemiplegia and paraplegia (cHR: 7.90, 95 % CI: 7.51-8.43), renal disease (cHR: 8.67, 95% CI 8.34-9.08), cerebrovascular disease (cHR: 9.84, 95 % CI: 9.58-10.14), peripheral vascular disease (cHR: 9.16, 95 % CI: 8.80-9.44) and malignancy (cHR: 10.38, 95 % CI: 10.00-10.73).
While the direction of the association between predictor and mortality remained the same for all variables included in the TIC and TVC models, the strength of each association (and even whether it was statistically significant or not) differed between the two model formulations for several important prognostic variables (Tables 3 and 4). aHR estimates for seven comorbidities increased in the TVC model compared with that in TIC models: myocardial infarction, congestive heart failure, cerebrovascular disease, hemiplegia/paraplegia, mild or sever liver disease, cancer, metastatic solid tumors. For example, the aHR (95% CI) for myocardial infarction was 1.07 (1.05-1.1) in the TIC model and 1.2 (1.18-1.22) in the TVC model and for chronic obstructive pulmonary disease was 1.18 (1.13-1.24) in the TIC model and 1.03 (0.99- 1.07) in the TVC model.
Fit and performance analyses shows that models including all 17 Charlson comorbidities as individual covariates out-performed models using summary measures. These results were consistent in nested model comparisons for both TIV and TVC models. Based on these findings, we compared the performance of these models when all 17 Charlson comorbidities were included as individual covariates. The TVC model out-performed the baseline model achieving the lowest AIC = 1,670,491 (Tables 3 and 4).
Discussion
We used a large cohort of adults with newly diagnosed hypertension to compare the performance of survival models according to the use of comorbidity data either at baseline (TIC approach) or with information updated during follow-up (TVC approach)). In this cohort of 475,345 newly diagnosed hypertensive patients identified over a 12 year period in Alberta, Canada, and followed for an average of 6 years, we found that prognostic models using updated disease occurrence information were more accurate than the baseline method in predicting individual risk of death.
In our study of relatively healthy adults with a new diagnosis of hypertension, the comorbidity burden increased significantly over time; nearly one quarter of patients developed at least one new comorbid condition following their initial diagnosis of hypertension. Consistent with other studies, the prevalence of Charlson comorbidities differed substantially between baseline and the follow-up end [1].
In order to capture mortality in people newly diagnosed with hypertension, long-term follow-up is necessary. Our median patient follow-up time was 5.75 years while our projected median survival time was in excess of 20-years. As a result, deaths were infrequent. Supported by previous study findings [14], we observed that TVC models had better fit and were more accurate in predicting mortality than TIC models. While differences in a healthy population were considered small, capturing change in comorbidities throughout the study period would improve prediction of individual risk. This may have implications for patient management and may alter the course of patient care to include aggressive prevention strategies as well as risk estimation for future studies.
TVC models captured incremental changes in disease state over time based on the serial measurement method [12]. Six comorbidities show decrease in the estimate of aHR indicating a potential overestimation of the strength of the association when only baseline information is used to predict mortality. Baseline survival models captured disease status at a single point in time. As a result, the interpretations of aHR for each chronic condition, collected at a single point in time, are attributed to the entire study period [15]. On the other hand, TCV models calculate a series of measures, breaking up the patient follow up time into smaller time windows. The start of each time window coincides with the onset of each additional disease and represents an increase in risk. TVC calculates a single weighted aHR for the entire study period using the series of aHRs from each time window. This allows TVC models to incorporate disease onset, changes in disease severity and exposure time, more accurately reflecting overall patient risk. The result of correctly classifying patients using TVC increases the average number of comorbidities for each patient while patient survival time remained the same. These findings have implications for existing and future studies using baseline assessment of comorbidity and highlight how disease misclassification could lead to errors in reporting.
Comparison between individual and summary measures shows that predictive models adjusting for all 17 individual Charlson comorbidities outperformed models using summary measures. Results from the literature are mixed. Austin et al. validated the performance and use of summary measures like the CCI and Elixhauser score as substitutes for individual comorbidities [14]. Sundararajan reported that using individual comorbidities performed better than the CCI, while Lieffers reported opposing results [16, 17]. Ghali suggested that summary measures calculated using study specific data had superior performance [18]. Acknowledging the variation in the literature, case mix adjustment using summary scores continues to be used in research for studies with small sample sizes.
Our comparisons and interpretations of aHRs between models took into consideration the natural history of the 17 Charlson comorbidities. Comorbidities with higher aHRs in TVC models compared to that in baseline models were considered to have higher risk of mortality in the short-term versus the entire study follow-up. Consistent with this interpretation, the aHRs and its 95% CI for hemiplegia or paraplegia (2.36, 2.29-2.43 in TIC and 2.89, 2.83-2.95 in TVC), were interpreted as a higher risk of death in short term following the onset of a disease or condition. Supporting this interpretation, Divanoglou reported that the highest mortality rate was within the first year of diagnosis or injury, with a 1-year mortality of 18.8% [19]. Conversely, a higher chronic obstructive pulmonary disease (COPD) aHR in the baseline model than in the TVC model could be interpreted as patients experiencing a low risk of death in the short term but with increasing risk in a longer timeframe. Shah and Kotloff [20] demonstrated that the natural history of COPD was slow to develop, with patients seeing minimal decline over short timeframes.
Limitations
Our study focused on newly diagnosed adults with hypertension, a relatively healthy population requiring a long-term follow-up to observe mortality outcomes. Patients with newly diagnosed hypertension were identified over a 12-year period (April 1 1997 to March 31 2009), with a median follow-up time of 5.75 years, well short of median survival expected for hypertensive middle aged patients (median expected survival time of 20 + years). Future research using mortality as a study outcome should focus on populations with a higher risk of mortality, such as those with acute conditions or post intervention.
Use of administrative datasets may underestimate comorbidity burden for asymptomatic conditions (such as dyslipidemia or type 2 diabetes mellitus) in a relatively healthy, newly diagnosed hypertensive population. Without blood pressure measurement, asymptomatic hypertensive patients may not seek primary or acute care, and thus are not included in our study. The case definition we used has a high specificity (95 to 97%) but low sensitivity (66 to 72%), potentially under sampling low risk hypertensive patients [21].
Consistent with previous studies, we found that there was a lack of consistency and validated analytical procedures to compare improvements between TIC and TVC models [2].
Conclusions
To the best of our knowledge this is the first large scale, population based study using administrative data investigating the onset of new comorbidities over time and its’ impact on predicting mortality risk in patients with a chronic disease. The resulting improvements in fit and performance of TVC predictive models were slight compared with method of using comorbidity assessed at baseline.
Abbreviations
- AHCIP:
-
Alberta Health Care Insurance Plan
- aHR:
-
Sdjusted hazard ratios
- AIC:
-
Akaike information criterion
- AMI:
-
Acute myocardial infarction
- CCI:
-
Charlson comorbidity index
- cHR:
-
Crude hazard ratios
- CI:
-
Confidence intervals
- COPD:
-
Chronic obstructive pulmonary disease
- DAD:
-
Hospital discharge abstracts
- ICD:
-
International Classification of Disease
- ICD-10-CA:
-
International Classification of Disease 10th revision Canadian Modification
- ICD-9-CM:
-
International Classification of Disease 9th revision Clinical Modification
- IQR:
-
Inter-quartile range
- log-HRs:
-
Log hazard ratios
- NR:
-
Not reportable
- PHN:
-
Personal Health Number
- Q1:
-
Lowest quintile
- Q5:
-
Highest quintile
- SD:
-
Standard deviation
- TIC:
-
Time-invariant covariates
- TVC:
-
Time-varying covariates
References
Wang CY, Baldwin L-M, Saver BG, Dobie SA, Green PK, Cai Y, Klabunde CN. The contribution of longitudinal comorbidity measurements to survival analysis. Med Care. 2009;47(7):813–21.
Giolo SR, Krieger JE, Mansur AJ, Pereira AC. Survival Analysis of Patients with Heart Failure: Implications of Time-Varying Regression Effects in Modeling Mortality. PLoS ONE. 2012;7(6):e37392.
Charlson ME, Pompei P, Ales KL, Mackenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chronic Dis. 1987;40:373–83.
Kovesdy CP, Anderson JE, Kalantar-Zadeh K. Paradoxical Association Between Body Mass Index and Mortality in Men With CKD Not Yet on Dialysis. Am J Kidney Dis. 2007;49(5):581–91.
Fleishman JA, Cohen JW. Using Information on Clinical Conditions to Predict High-Cost Patients. Health Serv Res. 2010;45(2):532–52.
Wong J, Taljaard M, Forster AJ, Escobar GJ, van Walraven C. Addition of time-dependent covariates to a survival model significantly improved predictions for daily risk of hospital death. J Eval Clin Pract. 2012;19(2):351–7.
Ahern TP, Lash TL, Thwin SS, Silliman Ra RA. Impact of acquired comorbidities on all-cause mortality rates among older breast cancer survivors. Med Care. 2009;47(1):73–9.
Canadian Institute for Health Information. Discharge Abstract Database. https://www.cihi.ca/en/dad_data_elements_2013_2014_en.pdf. (Accessed 6 Jan 2016).
Li B, Quan H, Fong A, Lu M. Assessing record linkage between health care and Vital Statistics databases using deterministic methods. BMC Health Serv Res. 2006;6:48.
Quan H, Chen G, Tu K, Bartlett G, Butt DA, Campbell NR, Hemmelgarn BR, Hill MD, Johansen H, Khan N, Lix LM, Smith M, Svenson L, Walker RL, Wielgosz A, McAlister FA. Outcomes among 3.5 million newly diagnosed hypertensive Canadians. Can J Cardiol. 2013;29(5):592–7.
Southern DA, Faris PD, Knudtson ML, Ghali WA. Prognostic relevance of census-derived individual respondent incomes versus household incomes. Can J Public Health. 2006;97(2):113–7.
Quan H, Li B, Couris CM, Fushimi K, Graham P, Hider P, Januel JM, Sundararajan V. Updating and Validating the Charlson Comorbidity Index and Score for Risk Adjustment in Hospital Discharge Abstracts Using Data From 6 Countries. Am J Epidemiol. 2011;173(6):676–82.
Akaike, H. “Prediction and entropy”, in Atkinson, A.C.; Fienberg, S.E., A Celebration of Statistics, Springer, 1985; p.1-24.
Austin SR, Wong YN, Uzzo RG, Beck JR, Egleston BL. Why Summary Comorbidity Measures Such As the Charlson Comorbidity Index and Elixhauser Score Work. Med Care. 2015;53(9):e65–72.
Dekker FW, de Mutsert R, van Dijk PC, Zoccali C, Jager KJ. Survival analysis: time-dependent effects and time-varying risk factors. Kidney Int. 2008;74(8):994–7.
Sundararajan V, Quan H, Halfon P, et al. Cross-National comparative performance of three versions of the ICD-10 Charlson Index. Med Care. 2007;45:1210–5.
Lieffers JR, Baracos VE, Winget M, Fassbender K. A comparison of Charlson and Elixhauser comorbidity measures to predict colorectal cancer survival using administrative health data. Cancer. 2011;117(9):1957–65.
Ghali WA, Hall RE, Rosen AK, et al. Searching for an improved clinical comorbidity index for use with ICD-9-CM administrative data. J Clin Epidemiol. 1996;49:273–8.
Divanoglou A, Westgren N, Seiger A, Hulting C, Levi R. Late mortality during the first year after acute traumatic spinal cord injury: a prospective, population-based study. J Spinal Cord Med. 2010;33(2):117–27.
Shah RJ, Kotloff RM. Lung transplantation for obstructive lung diseases. Semin Respir Crit Care Med. 2013;34(3):288–96.
Quan H, Khan N, Hemmelgarn BR, Tu K, Chen G, Campbell N, Hill MD, Ghali WA, McAlister FA. Validation of a case definition to define hypertension using administrative data. Hypertension. 2009;54(6):1423–8.
Acknowledgements
None.
Funding
This is part of the large project funded by Canadian Institute for Health Information (grant number MOP-97823). Dr Quan’s and Dr. McAlister’s salaries are supported by Alberta Innovates Health Solution. Dr Hemmelgarn is supported by the Roy and Vi Baay Chair in Kidney Research. Dr. McAlister is supported by the University of Alberta Chair in Cardiovascular Outcomes Research.
Availability of data and materials
The data that support the findings of this study are available from the Analytics unit of Alberta Health Services but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. All aggregate level data is available in the manuscript and appendices. Individual data are available from the authors upon reasonable request and with permission of the Analytics unit of Alberta Health Services.
Authors’ contributions
PeR made substantial contributions to conception and design, acquisition of data, analysis and interpretation of data; drafted the manuscript; given final approval of the version to be published. GC made substantial contributions to conception and design, acquisition of data, analysis and interpretation of data; drafted the manuscript; given final approval of the version to be published. PiR made substantial contributions to conception and design; been involved in drafting the manuscript and revising it critically for important intellectual content; given final approval of the version to be published. BRH made substantial contributions to conception and design; been involved in drafting the manuscript and revising it critically for important intellectual content; given final approval of the version to be published. FAM made substantial contributions to conception and design; been involved in drafting the manuscript and revising it critically for important intellectual content; given final approval of the version to be published. HQ made substantial contributions to conception and design; been involved in drafting the manuscript and revising it critically for important intellectual content; given final approval of the version to be published. DAS made substantial contributions to analysis and interpretation of data; been involved in revising it critically for important intellectual content; given final approval of the version to be published. RW made substantial contributions to analysis and interpretation of data; been involved in revising it critically for important intellectual content; given final approval of the version to be published. All authors participated sufficiently in the work to take public responsibility for appropriate portions of the content; and agrees to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Ethics approval was obtained from the Conjoint Health Research Ethics Board from the University of Calgary. A Research Agreement was signed with Alberta Health Services Analytics who is the data custodian.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Rymkiewicz, P., Ravani, P., Hemmelgarn, B.R. et al. Effects of longitudinal changes in Charlson comorbidity on prognostic survival model performance among newly diagnosed patients with hypertension. BMC Health Serv Res 16, 671 (2016). https://doi.org/10.1186/s12913-016-1910-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-016-1910-8