Abstract
Background
There are serious safety risks associated with chemotherapy, often associated with interdependencies in regimens administered over months or years. Various strategies are used to manage these risks. Computerized provider order entry (CPOE) systems are also implemented to improve medication safety. Little is known regarding the effect of CPOE on how clinicians manage chemotherapy interdependencies and their associated safety strategies.
Methods
We conducted a multi-method qualitative study in a paediatric hospital. We analysed 827 oncology incidents reported following CPOE implementation and carried out semi-structured interviews with doctors (n = 10), nurses (n = 6), a pharmacist, and oncology CPOE team members (n = 2). Results were interpreted according to safety models (ultra-safe, high-reliability organisations [HROs], or ultra-adaptive).
Results
Incident reports highlighted two interrelated types of interdependencies: those within organisation of clinical activities and those inherent in chemotherapy regimens. Clinicians reported strategies to address chemotherapy risks and interdependencies. These included rigid rules and ‘no go’ contexts for treatment to proceed, typical of the ultra-safe model; use of time (e.g. planning only so far ahead) and sensitivity to operations, typical of HROs. We identified three different time horizons in CPOE use in relation to patients’ treatments: life-long, the whole regimen, and the ‘here and now’. CPOE supported ultra-safe strategies through automation and access to rules/standardisation, but also created difficulties and contributed to incidents. It supported the ‘here and now’ better than a life-long or whole regimen view of a patient treatment. Sensitivity to operations was essential to anticipate and resolve uncertainties, hazards, CPOE limitations, and mismatches between CPOE processes and workflow in practice.
Conclusions
Within oncology, CPOE appears to move the ‘mix’ of risk strategies towards ultra-safe models of safety and protocol-mandated care. However, in order to operate ultra-safe strategies embedded in CPOE and stay on protocol it is essential for clinicians to be thoughtful and show sensitivity to operations in CPOE use. CPOE design can be advanced by better consideration of mechanisms to support interdependencies.
Similar content being viewed by others
Background
Chemotherapy medications are hazardous, high risk treatments; errors with these medications can cause severe harm, especially in children [1]. Chemotherapy regimens are administered often in combination with other medications and over many months, and errors are often associated with interdependent elements of chemotherapy regimens, such as number of cycles, dose scheduling, cumulative doses, and monitoring [1, 2].
To reduce harm from chemotherapy, risk management strategies must be in place [3], individual patient regimens must be based on documented and referenced protocols [4], and work processes organised with reference to accepted standards [4,5,6,7] and designed to reduce the possibility of error [8, 9]. Computerized provider order entry (CPOE) systems with decision support are a further strategy for improving safety with chemotherapy. CPOE can reduce medication errors and unwanted protocol deviations by automatically calculating chemotherapy doses based on patient height and weight, providing warnings, assisting in scheduling of chemotherapy cycles, and supporting workflow [10,11,12,13,14,15,16]. Conversely, CPOE can introduce new types of error and have unexpected negative consequences on work practices [1, 17]. It can also be challenging to implement CPOE for chemotherapy [15, 16, 18, 19], with every chemotherapy protocol having to be entered in the system and then kept up to date [15, 20]. Adoption of CPOE for chemotherapy can thus lag behind adoption of CPOE systems for other medications or in other clinical areas [15].
The literature suggests that design of CPOE for chemotherapy is ‘confronted with problems’ [21] and that CPOE alone is not sufficient to eliminate chemotherapy errors. Other safety strategies generally co-exist, including error surveillance systems [22, 23], checking of patient regimens against standard protocols [22, 24], and interventions to improve situational awareness [12, 22]. The literature remains unclear on how CPOE relates to such strategies, especially with regard to management of interdependencies. This gap in knowledge may hinder efforts to improve CPOE design and implementation, and thus improve patient safety.
This study aimed to fill this gap by investigating how CPOE for chemotherapy relates to other safety strategies in use in a paediatric clinical oncology unit, with a focus on the management of interdependencies. Our objectives were to identify the strategies clinicians apply to safely manage the interdependencies inherent in paediatric chemotherapy, and whether/how CPOE affects these.
For this study, we drew on theoretical and practical insights from Vincent and Amalberti’s research on safety strategies ‘in the real world’, and the three main safety models they propose - ultra-safe, high-reliability organisations (HROs) and ultra-adaptive [3, 25, 26]. We briefly explain their framework in the next section, as we describe our methods and provide definitions.
Methods
Analytical framework
Vincent and Amalberti [3] explain the different ‘real world’ safety strategies applied in different sectors or organisations for dealing with risks. Such strategies may involve, for example: 1. eliminating exposure to risk by defining ‘no go’ contexts for operations (following Amalberti, we refer to this as ‘Plan A’ [25] – in aviation, equivalent to grounding all flights when a volcano erupts) and applying rigid standard operating procedures; 2. introducing barriers to risks by engineering optimisation of work processes (including by introducing technology); 3. dealing with risks by improving organisational capacity for monitoring, adaptation and response (e.g. by maintaining ‘sensitivity to operations’ [27], or awareness of how one’s actions affect others); and 4. developing professional expertise for extreme situations. We considered these strategies as different ways, at different levels, to manage risks associated with interdependencies. These strategies also approximately correspond to three models of safety in organisations (Fig. 1)– the ultra-safe (examples 1 and 2 above), high reliability organisation (HRO) (example 3) and ultra-adaptive (example 4) [3, 25]. Different healthcare contexts have a different combination of the three models, with some working more often than others as ultra-safe, HRO, and/or ultra-adaptive, along a continuum. Thus, it may be expected that: ‘A healthcare team might, in one afternoon, work in an ultra-safe manner at some points, such as when a care pathway is clearly defined and entirely appropriate for the patient; they may work in a high-reliability mode for the main part and, for short periods, in an ultra-adaptive mode.’ [3]
Three models of safety and examples of associated risk strategies. Elaboration of Vincent and Amalberti text and figures [3, 25], with additional reference to collective mindfulness – typical of high reliability organisations models of safety [27]. Collective mindfulness manifests when people on the frontline collectively show preoccupation with failure (ongoing wariness that errors are possible), reluctance to simplify interpretations of unexpected events (questioning assumptions, uncovering blind spots), sensitivity to operations (having an integrated understanding of current situation, e.g. awareness of how one’s actions affect others), commitment to resilience (awareness that it is impossible to anticipate all situations, needs for adaptation) and deference to expertise (persons with expertise to make decisions regardless of hierarchy) [27]
Building on Thompson’s Organization in Action [28], we define interdependency as the relation between tasks or activities, where related tasks/activities must all be completed in a timely fashion, reliably, and/or safely, to achieve safe processes and/or outcomes. While many interdependencies are sequential (one task contributing to the next; a task cannot be completed unless other tasks have been completed first), others may be reciprocal (one task contributing to the other and vice-versa), or pooled (each activity independently contributing to the whole) [28]. For example, nurses’ chemotherapy administration depends on doctors’ prescribing, which may depend on pathologists’ reporting results (sequential tasks); supplying medications in hospital pharmacies on a just-in-case basis, contributes to doctors prescribing medications to patients, while doctors prescribing also calls for medications being stored in pharmacy on a just-in-case basis (reciprocal relationship between activities); repeated administration of chemotherapy doses to a patient cumulates towards a safe maximum level (pooled activities). We define time dependencies as those where safety in management of the interdependency requires attention to timeliness or timing of related tasks (e.g. administration of sequential doses at specific time intervals).
Setting and design
The study took place in the oncology unit of a 350-bed tertiary paediatric hospital in New South Wales (Australia) between September 2018 and June 2019. The oncology unit is the largest children’s cancer unit in the State, with up to 150 new referrals each year. The unit has an inpatient ward plus an outpatient clinic run as an ‘open door’ service where patients and their families can be seen without an appointment. Doctors are routinely called to see patients not under their regular care.
Eighteen months prior to this study, the hospital had implemented hospital-wide CPOE (Cerner [29]) for prescribing and administration of medications, test orders and results, as part of an electronic medical record system. The oncology unit made use of CPOE functionality for linking orders (‘PowerPlan’) to incorporate chemotherapy regimens into the system and to prescribe and administer chemotherapy for individual patients. A chemotherapy PowerPlan team was responsible for building chemotherapy protocol templates in the CPOE and training oncology clinicians in use of the system.
We carried out a qualitative, interpretative study combining incident report analysis and interviews. Analysis of the incident reports informed the interview questions, and the insights gained through the interviews fed back to further analysis of the events described in the incident reports.
Data collection
Incident reports were submitted by staff through the hospital online incident reporting system. Any event that resulted in (or had potential to lead to) injury, damage or other loss is required to be reported. The hospital provided us with all incident reports concerning oncology patients recorded in the period 15 August 2016 to 15 February 2018 (the first 18 months following CPOE implementation in oncology), whether or not these were specifically related to medications or CPOE.
Interviews were carried out by a researcher (VL) with a background in health informatics and qualitative research. All clinicians in the oncology unit and members of the chemotherapy PowerPlan team were invited to participate as we were seeking to maximise variety of levels of seniority and CPOE expertise. Access to participants was facilitated by the unit coordinator. We sought participants for interviews until we reached code and meaning saturation [30]. Interviews were semi-structured, using questions (Additional file 1) aimed to uncover how clinicians deal with interdependencies in the medication process, and whether the CPOE supported their work. With participants’ written consent, interviews were audio recorded and professionally transcribed.
Data analysis
We carried out a qualitative content analysis [31] of the text narratives of the incident reports (fields for Incident description and Contributing factors) and the interview transcripts. Analysis was carried out with support of NVivo v.11, by one researcher in discussion with co-investigators. The free text fields from incident reports were treated as narrative accounts of events from frontline clinicians [32, 33]. All reports were included, but only those related to direct patient care coded. We took both a conventional (inductive) content analysis approach, with open codes derived from the data, and a directed (deductive) approach with our objectives providing higher level categories for grouping the open codes.
Analysis of interview transcripts was carried out iteratively. First, an in-depth detailed understanding of the data was gained through careful reading and line by line coding. Open codes were applied through both conventional and directed approaches, to address study objectives and capture significant aspects of the context. Chemotherapy medication processes, as described by clinicians in the unit, were represented in flowcharts to better understand interdependencies in workflow. This analysis was done concurrently with, and soon after, data collection. A framework analysis approach [34] was then applied using categories from Vincent and Amalberti’s model.
Throughout the analysis process, discrepant findings were sought. Findings from incident analysis were triangulated with those from interviews to enrich understanding [35]. The head of the oncology unit (LDP) checked ‘the “fit” between respondents’ views and the researcher’s representation of them’ [36] (credibility).
Results
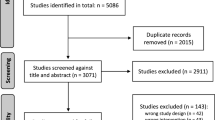
A dataset of 827 incidents were received from the hospital and included in the analysis. Incidents not concerning direct patient care were then excluded (n = 73). (Details of the 827 incidents are given in Additional file 2 and elsewhere [37]). In the analysis of the incidents, the CPOE appeared to be both a mechanism for safety and a contributing factor for incidents.
Twenty interviews were conducted with 19 participants (Table 1). Interviews lasted about 30 min.
We integrated results from interviews and incidents analysis and structured these around interdependencies and risks to medication safety, strategies to deal with these risks, and the role of the CPOE for each strategy. We identified quotes from interview transcripts by interview number (idX), but do not provide details on interviewees’ roles to protect their anonymity. We refer to incident reports by their row in the dataset (iX).
Interdependencies and risks to safety with chemotherapy
Work practices related to paediatric chemotherapy treatments were rich in interdependencies. Across interviews and incidents, we identified two interrelated overarching types of interdependencies that characterised chemotherapy prescribing and administration: first, those related to the organisation of clinical activities, in particular the medication workflow involving doctors, nurses and pharmacy staff, and its interplay with a variety of hospital services (e.g. intensive care, pathology, imaging, as well as other hospitals), and second, interdependencies inherent to chemotherapy regimens that dictated combinations of medications and tests. Time dependencies were especially apparent, such as precise time gaps between administration of successive doses.
Both types of interdependencies (organisational and regimen-related) were identified in incident reports and often involved CPOE. For example, an incorrect date in a CPOE prescription and a delay in documentation of the patient being ‘ready for chemotherapy’ (organisational dependency-medication workflow) delayed administration due to the medication requiring pre-medication (a regimen dependency), which further cascaded into requiring monitoring of the patient ‘after hours’, leading to increased risks for the patient and costs to the hospital (organisational dependency).
[...] Patient due rituximab and MTX [methotrexate] today, date for chemotherapy was incorrect and not ‘ready for chemotherapy’ documented [in the CPOE]. This delayed chemotherapy administration until 11am. [...] [medications] will need to be reordered. The first medication requires premedication and the patient is at risk of anaphylaxis with this drug (needs to be given in business hours) and MTX requires blood monitoring levels and if given outside set hours adds significant cost [...] [i150]
Ultra-safe risk strategies applied to chemotherapy processes
Chemotherapy safety risks were reported to be managed through a range of strategies based on the application of rules and multiple safety checks. These appeared more typical of the ultra-safe model of safety [3] than the HRO model.
Specifically, participants spoke of rigid rules regarding who was authorised to prescribe chemotherapy (on CPOE) and the content of medication orders as per chemotherapy protocols. Continuing with a regimen (e.g. progressing to the next cycle) was organised around the principle of withholding treatment until the patient recovers (comparable to ‘Plan A’ in the ultra-safe model).
Participants reported multiple checks during the medication process. In particular, nurses were tasked with checking each dose against the protocol to alert doctors to any discrepancy. This was ‘an institution specific practice’ (id16) that was maintained after CPOE implementation, despite the use of pre-set CPOE templates that would (or should) support doctors to produce orders matching the corresponding protocol.
...when I am ordering it [on CPOE], it looks fine to me. [But] The nurses [would] say, “Well, can’t do that because it is out of sequence,” or, “you have pushed this onto that.” [...] Or they will say, “The protocol mandates 120% of this and you are giving 110% or 150%.” And they are just simply saying, “Is this what you want me to do?” ... (id16)
Sometimes the patient’s condition led to clinicians deciding to deviate from the protocol – such as when ‘this child has such a high-risk disease that no matter what I’m going to go ahead’ (id16) despite test results not reaching the threshold indicated by the protocol. This kind of judgement – highly dependent on individual clinical expertise - typically belongs to the ultra-adaptive model of safety. However, in this context – where the doctor had to communicate the decision to the nurses and to other doctors in order to act on it – it is perhaps suggestive of a HRO approach to dealing with risks.
Does CPOE support an ultra-safe model of safety with chemotherapy?
CPOE supported strategies typical of the ultra-safe model through hard and soft mechanisms, namely through automation, access to information and standardisation of the semantics of protocols (disambiguation) (Table 2).
In terms of automation, the CPOE provided clinicians with all required medications pre-built in templates, to reduce the possibility of medications being omitted by mistake, which were also linked with appropriate time dependencies (if doctors delayed one, the others would be automatically delayed for a corresponding period). The CPOE provided automatic dose calculations and warnings based on embedded rules, and ‘exposed’ unreliable patient weight and height data used for dose calculation, by displaying trends and normal ranges.
... you can see patients with a weight here and a height up here [on the CPOE chart] [...] three months for a baby of four kilos you can go to eight kilos, you can change dramatically the dose. [...]. Now, in paper land [...] [doctors] might go six months without checking the height and weight. It happened before, but here it’s exposing it. (id1)
CPOE automation also limited prescribing and administration rights through different users’ profiles; the embedded workflow management system automatically routed the orders to the authorised person. The CPOE paused the workflow proceeding forward to administration until the system had been notified via a checkbox that the patient was ‘ready for chemo’.
However, these CPOE contributions towards an ultra-safe approach to chemotherapy were challenged by the perceived complexity of operating the system (especially when protocol templates were not available in the system to prescribe a patient’s regimen), and difficulties in identifying ‘where the patient is at’ in the protocol.
In terms of ‘soft’ mechanisms, we identified two aspects of CPOE that supported use of ultra-safe risk strategies. All clinicians had access both to patient information and the relevant chemotherapy protocol; previously, paper-based protocols were kept in drawers and not easily accessible across place and time. In addition, the process of converting paper-based protocols into electronic versions brought to the surface previously invisible ambiguities in their rules. To automate these rules, these had to be clarified and uniquely defined so that all clinicians would interpret the protocol in the same way.
HRO strategies - management of uncertainties and ‘usual hazards’ through adaptation and different time horizons
The application of the principle of withholding treatment until the patient recovers (‘plan A’) meant that planned doses or cycles often needed to be rescheduled. Thus, for any patient there would be uncertainty about when exactly the treatment would be given. This scheduling – or rescheduling - of the treatment must also take into account the constraints posed by the hospital’s resources (organisational interdependencies), for example ‘our general anaesthetic days are Monday and Thursday’ (id16), or over holidays, ‘services aren’t working quite as well’ (id1). The patient and family may also pose constraints on suitable dates – such as wanting to avoid school photo day.
Clinicians reported that it was challenging to plan cycles, tests and doses much in advance. Although the CPOE theoretically allowed clinicians to prescribe a whole regimen in advance, given these uncertainties, interviewees indicated that they would only schedule about a month ahead in practice.
Researcher: the doctors might schedule the entire one year of treatment in advance? Participant: [...] they probably wouldn’t. [...] we would chart chemotherapy, kind of, a month out, because [children] can grow so much in such a short time, the doses need to change. Other things can happen as well that they may start to not recover as well, so we need to modify the dose, it was too big for them, so we need to back off [...]. (id7)
Doctors therefore made use of time as a risk management strategy [25] to deal with the uncertainties. More specifically, we identified three time horizons used to approach a patient’s chemotherapy regimen – a life-long view, the whole regimen view, and the ‘here and now’. CPOE automation better supported the ‘here and now’ than the longer time views (Table 3). For example, clinicians reported difficulties with finding and collating information to calculate a patient cumulative dose (a life-long view), and with the fragmented electronic display of the whole regimen.
Sensitivity to operations and CPOE
We found that a combination of situation awareness, organisational awareness and CPOE awareness was perceived as essential for safe and efficient CPOE use (Fig. 2). Clinicians had to maintain (and act on) situational awareness to understand ‘where is the patient at’ in their specific regimen and with respect to the corresponding protocol. Several interviewees referred to this information need – ‘where patients are up to’ (id1, id5, id7, id8–12). Clinicians also had to maintain (and act on) organisational awareness. For example, they had to act on the system with awareness of self and others ‘down the line’ (Table 4). They had to be aware of CPOE, learning to be watchful of its automated behaviour such as automated recording of times and dates. With use, clinicians learned that, for a variety of reasons, time and dates in the system may not accurately reflect the times when medication activities took place. This had repercussions for regimen time dependencies, which were also encoded in the templates.
...sometimes when [the CPOE] says, it’s the start date, it’s not really been the start date, because it’s been delayed [...]. That stays as the estimated start date [...] when you come to [prescribe], they’re due next week, for example, but if you look at the chemotherapy, [...], they’re due in two weeks. [...] just [automatically] ticks over [...] (id3)
Sensitivity to operations in chemotherapy prescribing (with examples). CPOE = Computerized Provider Order Entry system. We refer to Endsley’s definition of situation awareness [38] as “the perception of the elements in the environment within a volume of time and space, the comprehension of their meaning and the projection of their status in the near future”, applied to a patient. With organisation awareness we refer to the understanding of how roles and services fit within the organisational structure, institutional practices and rules, and how to operate within these practices to achieve desired effects. This definition includes individual awareness of local teams and workflows, or of the wider hospital organisation, within or beyond individual’s control. CPOE awareness is knowledge on how the technology works/how to make it work/the effects it produces and acting on this knowledge. We take sensitivity to operations (at individual or collective level) as any and all of the three types of awareness at any one time
Discussion
We studied a paediatric oncology unit using a hospital-wide CPOE system, and identified two inter-related overarching types of interdependencies associated with chemotherapy: those related to the organisation of clinical activities, and those inherent to chemotherapy regimens in terms of dictating precise combinations of medications, and combinations of medications and tests. Time dependencies were especially apparent across both interdependency types. The time dependencies in a patient regimen were dealt with through a cognitive strategy known as ‘fragmentation’ (‘allowing shorter horizon planning’ [39]) and a practice of temporary plans and constant adjustments. These we associate with ‘adaptation’ strategies typical of HRO models of safety.
CPOE automation seemed to better support the small scale, short-time regimen dependencies that are largely under control of the team, rather than the scheduling of services where organisational dependencies are not under their control. It is possible that the small scale, short-time regimen dependencies were mainly sequential interdependencies (e.g. administration of different medications as sequential steps), while the organisational dependencies were also relational or pooled, and that sequential interdependencies are easier to automate in workflow management systems.
Both ultra-safe and HRO strategies were used to address chemotherapy risks and interdependencies. CPOE automation supported application of ultra-safe strategies in chemotherapy such as compliance with protocols’ rules and ‘no-go’ contexts for proceeding with chemotherapy. CPOE support mechanisms for an ultra-safe model of care were both ‘hard’ (automation) and ‘soft’ (information availability/disambiguation). However, prescribing regimens with CPOE was difficult when protocol templates were not readily available; it was difficult to track medication data across screens, and a summary display of the whole regimen (showing protocol variations, if any) was not available; automated time-stamps of medication administration were not always accurate, with repercussions for subsequent time-dependent doses. Therefore, in addition to situational awareness at the level of the patient [38] and awareness of the organisation’s teams and services [27], clinicians had to maintain awareness of the technology (‘CPOE awareness’), its limitations and consequences. We propose a definition of CPOE awareness as knowledge of how the technology works, how to make it work, and the effects it produces, and acting on this knowledge.
The finding that ‘CPOE awareness’ was needed in this setting is consistent with other CPOE chemotherapy implementations that required significant investment of time and resources to enable clinicians to gain necessary familiarity with all the nuances of CPOE workflows [19]. Our finding that CPOE automation supported application of ultra-safe strategies in chemotherapy is in line with existing literature that shows how CPOE may improve compliance with chemotherapy protocols [17]. However, prescribed regimens are subject to change and in need of adaptation, also due to application of ultra-safe rules (typically, waiting for patient recovery before proceeding with treatment). In the late 1990s, medical sociologists Timmermans and Berg explained how standardisation of patient care with (paper-based) oncology protocols was achieved through clinicians’ ‘active (not mindless) support [...] to maintain the protocol’s trajectory on course’ [40]. In their account, adaptation was an enabler, rather than opposer, to standardisation. We posit that active (not mindless) adaptation requires situational awareness (knowledge of ‘where is the patient at’ in relation to a prescribed regimen and underlying protocol), which must be facilitated by CPOE displaying interdependent elements of regimens over different time horizons (in chemotherapy, known as ‘roadmaps’ [12]). This is also supported by recent research suggesting that chemotherapy errors with CPOE may be prevented with knowledge of a patient’s chemotherapy history and in-depth knowledge of protocols [41]. Nurses’ and/or pharmacists’ routine checks of CPOE orders against protocols [22, 24] – also reported in the unit we studied - are one way to address CPOE limitations by automatically monitoring variations to protocols, and may also be facilitated by the availability of electronic roadmap displays.
Strengths of this study include multiple sources of data - interviews and incident reports - and analysis informed by theory. A limitation is that we did not observe the activities described. Instead, we relied on participants as ‘their own ethnographers’ [42]. We had limited nurse participation. We identified ultra-safe and HRO strategies; we did not find any strategy from the ultra-adaptive safety model possibly because we did not observe activities. Patient safety incident reports were brief and provided only limited information; incidents related to multiple aspects of patient care, not exclusively chemotherapy. We took a qualitative approach to incident analysis given the limitations of analysing these quantitatively; reported incidents are likely to represent only a fraction of the incidents that occur and thus numbers of incidents cannot be relied on to establish frequency [43]. The CPOE system investigated was a general system adapted for chemotherapy, rather than a bespoke chemotherapy system; it is not known whether the findings generalise across other organisations and other systems.
Ultra-safe services ‘are highly standardized and rely heavily on automation and information technology’ [3]. Implementation of CPOE in chemotherapy appears to be a move towards ultra-safe, but our findings suggest that CPOE design must be improved. In such a complex and high-risk setting, CPOE design should facilitate clinicians’ decision-making processes, rather than add difficulties. Lessons can be learned for design of chemotherapy CPOE that better supports the management of interdependencies in regimens and workflows [21]. This might include affording a variety of visualisation displays over different time horizons and capturing more accurate timestamps of activities, tracking protocol variations and cumulative effects over time. CPOE implementations also need to support learning processes for clinicians to gain the awareness needed to use CPOE systems safely. For this, sufficient enabling resources (e.g. staff/patient ratio, CPOE training and assistance, quiet time for prescribing) must be in place at the point of roll-out and maintained throughout staff turnover [19].
To our knowledge, this is the first study to apply Vincent and Amalberti’s models of safety and related risk strategies [3] to evaluate a technology implementation in a healthcare setting. The study has been able to identify mechanisms by which CPOEs can mitigate or exacerbate medication safety risks.
Patients and families may have different priorities or values about medication safety and compliance with rules, that may vary during the long period of chemotherapy treatments. Future research in paediatric oncology should investigate whether/how patients and families’ priorities or values change the way clinicians use the CPOE for chemotherapy regimens, and how they approach the different time frames: the ‘here and now’, ‘whole treatment’ and ‘life-long’. Further research with CPOE for chemotherapy should also investigate time dependencies in regimens in more detail – including how nurses manage administration times between doses and automated timestamping of activities.
Conclusions
CPOE appears to affect the ‘mix’ of risk strategies in place in an oncology unit. It can drive ultra-safe models of safety and protocol mandated care, but operating ultra-safe strategies embedded in the CPOE and staying on protocol also requires HRO strategies including ‘sensitivity to operations’ in CPOE use. CPOE implementations need to support the processes of learning required for clinicians to gain such collective awareness, and shortcomings in CPOE design must be addressed for it to fully contribute to the ultra-safe.
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available. The hospital has not consented to the sharing of patient safety incidents data beyond the project team. Research participants did not consent to interview transcripts being made publicly available.
Abbreviations
- CPOE:
-
Computerized provider order entry
- HRO:
-
High-reliability organisations
References
Weingart SN, Zhang L, Sweeney M, Hassett M. Chemotherapy medication errors. Lancet Oncol. 2018;19(4):e191–e9.
Small MD, Barrett A, Price GM. The impact of computerized prescribing on error rate in a department of Oncology/hematology. J Oncol Pharm Pract. 2008;14(4):181–7.
Vincent C, Amalberti R. Safer healthcare: strategies for the real world. Cham: Springer International Publishing; 2016.
Carrington C, Stone L, Koczwara B, Searle C, Siderov J, Stevenson B, et al. The Clinical Oncological Society of Australia (COSA) guidelines for the safe prescribing, dispensing and administration of cancer chemotherapy. Asia Pacific J Clin Oncol. 2010;6(3):220–37.
Fani Pakdel A, Mousavi M, Roohani M, Elyasi S, Kooshyar M. 113P Chemotherapy administration safety standards for preventing medication errors and adverse drug reactions in patients with breast cancers. Ann Oncol. 2016;27(suppl_9).
Neuss MN, Gilmore TR, Belderson KM, Billett AL, Conti-Kalchik T, Harvey BE, et al. 2016 updated American Society of Clinical Oncology/Oncology Nursing Society chemotherapy administration safety standards, including standards for pediatric oncology. J Oncol Pract. 2016;12(12):1262–71.
Coccia PF, Pappo AS, Beaupin L, Borges VF, Borinstein SC, Chugh R, et al. Adolescent and young adult oncology, version 2.2018, NCCN clinical practice guidelines in oncology. J Natl Compr Cancer Netw. 2018;16(1):66–97.
Pfeiffer Y, Gut SS, Schwappach DL. Medication safety in oncology care: mapping checking procedures from prescription to Administration of Chemotherapy. J Oncol Pract. 2018;14(4):e201–e10.
Franklin BD, Panesar SS, Vincent C, Donaldson LJ. Identifying systems failures in the pathway to a catastrophic event: an analysis of national incident report data relating to vinca alkaloids. BMJ Q Safety. 2014;23(9):765–72.
Ferranti JM, Horvath MM, Jansen J, Schellenberger P, Brown T, DeRienzo CM, et al. Using a computerized provider order entry system to meet the unique prescribing needs of children: description of an advanced dosing model. BMC Med Inform Decis Mak. 2011;11(1):14.
Gandhi S, Tyono I, Pasetka M, Trudeau M. Evaluating an oncology systemic therapy computerized physician order entry system using international guidelines. J Oncol Pract. 2014;10(2):e14–25.
Allen SW, Hayashi RJ, Jones SJ, Drozda MH, Brown RL, Lackey IT, et al. Development of electronic chemotherapy roadmaps for pediatric oncology patients. J Pediatr Oncol Nurs. 2018;35(5):314–9.
Elsaid K, Truong T, Monckeberg M, McCarthy H, Butera J, Collins C. Impact of electronic chemotherapy order forms on prescribing errors at an urban medical center: results from an interrupted time-series analysis. Int J Q Health Care. 2013;25(6):656–63.
Hoffman JM, Baker DK, Howard SC, Laver JH, Shenep JL. Safe and Successful Implementation of CPOE for Chemotherapy at a Children's Cancer Center. J Nat Compr Canc Netw. 2011;9(Suppl 3):S-36–50.
Martin DB, Kaemingk D, Frieze D, Hendrie P, Payne TH. Safe implementation of computerized provider order entry for adult oncology. Appl Clin Inform. 2015;6(4):638–49.
Whalen K, Lynch E, Moawad I, John T, Lozowski D, Cummings BM. Transition to a new electronic health record and pediatric medication safety: lessons learned in pediatrics within a large academic health system. J Am Med Inform Assoc. 2018;25(7):848–54.
Rahimi R, Moghaddasi H, Rafsanjani KA, Bahoush G, Kazemi A. Effects of chemotherapy prescription clinical decision-support systems on the chemotherapy process: a systematic review. Int J Med Inform. 2019;122:20–6.
Wagner S, Beckmann MW, Wullich B, Seggewies C, Ries M, Bürkle T, et al. Analysis and classification of oncology activities on the way to workflow based single source documentation in clinical information systems. BMC Med Inform Decis Mak. 2015;15(1):107.
Chung C, Patel S, Lee R, Fu L, Reilly S, Ho T, et al. Implementation of an integrated computerized prescriber order-entry system for chemotherapy in a multisite safety-net health system. Am J Health Syst Pharm. 2018;75(6):398–406.
Crespo A, Redwood E, Vu K, Kukreti V. Improving the safety and quality of systemic treatment regimens in computerized prescriber order entry systems. J Oncol Pract. 2018;14(6):e393–402.
Rahimi R, Kazemi A, Moghaddasi H, Rafsanjani KA, Bahoush G. Specifications of computerized provider order entry and clinical decision support systems for cancer patients undergoing chemotherapy: a systematic review. Chemotherapy. 2018;63:162–71.
Weiss BD, Scott M, Demmel K, Kotagal UR, Perentesis JP, Walsh KE. Significant and sustained reduction in chemotherapy errors through improvement science. J Oncol Pract. 2017;13(4):e329–e36.
Call RJ, Burlison JD, Robertson JJ, Scott JR, Baker DK, Rossi MG, et al. Adverse drug event detection in pediatric oncology and hematology patients: using medication triggers to identify patient harm in a specialized pediatric patient population. J Pediatr. 2014;165(3):447–52.e4.
Baldwin A, Rodriguez ES. Improving patient safety with error identification in chemotherapy orders by verification nurses. Clin J Oncol Nurs. 2016;20(1):59–65.
Amalberti R. Navigating safety: necessary compromises and trade-offs - theory and practice: springer; 2013.
Amalberti R, Vincent C. Managing risk in hazardous conditions: improvisation is not enough. BMJ Q Safety. 2019; Published Online First: 09 July 2019:bmjqs-2019-009443.
Weick KE, Sutcliffe KM, Obstfeld D. Organizing for High Reliability: Processes of Collective Mindfulness. In: Sutton RS, Staw BM, editors. Research in Organizational Behavior. Volume 1. Stanford: Jai Press; 1999. p. 81–123.
Thompson JD. Organizations in action: social science bases of administrative theory: McGraw Hill; 1967.
Cerner Corporation: https://www.cerner.com/. Accessed 10 Aug 2020.
Hennink MM, Kaiser BN, Marconi VC. Code saturation versus meaning saturation:how many interviews are enough? Qual Health Res. 2017;27(4):591–608.
Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–88.
Waring JJ. Constructing and re-constructing narratives of patient safety. Soc Sci Med. 2009;69(12):1722–31.
Iedema R, Flabouris A, Grant S, Jorm C. Narrativizing errors of care: critical incident reporting in clinical practice. Soc Sci Med. 2006;62(1):134–44.
Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol. 2013;13:117.
Salkind N. Triangulation. In: Encyclopedia of research design. Thousand Oaks: SAGE Publications; 2012.
Nowell LS, Norris JM, White DE, Moules NJ. Thematic analysis: striving to meet the trustworthiness criteria. Int J Qual Methods. 2017;16(1):1609406917733847.
Lichtner V, Baysari M, Gates P, Dalla-Pozza L, Westbrook JI. Medication safety incidents in paediatric oncology after electronic medication management system implementation. Eur J Cancer Care. 2019;28(6):e13152.
Endsley MR. Situation awareness in aviation systems. Handbook of aviation human factors; 1999. p. 257–76.
Daniel R, Schuck NW, Niv Y. How to divide and conquer the world, one step at a time. Proc Natl Acad Sci. 2015;112(10):2929–30.
Timmermans S, Berg M. Standardization in action: achieving local universality through medical protocols. Soc Stud Sci. 1997;27(2):273–305.
Reinhardt H, Otte P, Eggleton AG, Ruch M, Wohrl S, Ajayi S, et al. Avoiding chemotherapy prescribing errors: analysis and innovative strategies. Cancer. 2019;125(9):1547–57.
Mol A. The body multiple: ontology in medical practice: Duke University press; 2002.
Westbrook JI, Ling L, Elin C, Lehnbom M, Baysari T, Braithwaite J, et al. What are incident reports telling us? A comparative study at two Australian hospitals of medication errors identified at audit, detected by staff and reported to an incident system. Int J Q Health Care. 2015;27(1):1–9.
Acknowledgements
We are grateful to the hospital staff who gave their time to participate in this study.
Funding
This study received funding from the European Union’s Horizon 2020 research and innovation programme under the Marie-Skłodowska Curie Grant Agreement number 740131. This paper represents independent research supported by the NIHR Imperial Patient Safety Translational Research Centre. The funding bodies had no role in the design of the study and collection, analysis, and interpretation of data and in writing the paper. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health and Care. The European Commission and its Research Executive Agency are not responsible for any use that may be made of the information this paper contains.
Author information
Authors and Affiliations
Contributions
VL conceived the study, collected the data, lead data analysis and drafted the manuscript. LDP assisted with data collection. BDF, JW and LDP contributed to data analysis and to the writing of the paper. All authors read and approved the final manuscript.
Authors’ information
VL is currently researching the impact of technology for medications on collective mindfulness and medication safety. LDP is oncology specialist and head of the cancer centre in the hospital we studied.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study received ethics approval from the hospital’s human research ethics committee (Ref HREC/15/SCHN/370). Hospital incident reports were de-identified prior to review and analysis. Interview participants provided written informed consent. Data from interviews were anonymised at the point of data collection.
Consent for publication
Not applicable.
Competing interests
Professor Franklin supervises a PhD student who is part funded by Cerner, outside the submitted work. All other authors have no conflicts of interest to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1: Appendix 1:
Interview guide.
Additional file 2.
Incident analysis - methods and summary of findings.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lichtner, V., Franklin, B.D., Dalla-Pozza, L. et al. Electronic ordering and the management of treatment interdependencies: a qualitative study of paediatric chemotherapy. BMC Med Inform Decis Mak 20, 193 (2020). https://doi.org/10.1186/s12911-020-01212-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12911-020-01212-z