Abstract
Background
Staphylococcal aureus (S. aureus) has become the leading causative pathogen of Prosthetic Joint Infection (PJI), which is the most devastating complication after arthroplasty surgeries. Due to the biofilm formation ability and emergence of multiple-drugs resistance strains of S. aureus, it has become an urgency to find new anti-staphylococcal agents to establish effective prophylaxis and treatment strategy for PJI. Extracted from a traditional Chinese herb, berberine is proved active in inhibiting S. aureus, while whether it exerts the same effect on PJI-related S. aureus remains unknown. This study aims to investigate the antimicrobial activity of berbrine against clinical derived PJI-related S. aureus and whether its inhibiting efficacy is associated with subtypes of S. aureus.
Methods
Eighteen PJI-associated S. aureus were collected and their Multi-locus Sequence Types (MLST) and susceptibility to berberine both in planktonic and biofilm form were investigated. Additionally, one S. aureus strain (ST1792) was selected from the group and its transcriptomic profiling in berberine incubation was performed. The statistical analyses were conducted using Student’s t-test with SPSS 24.0(SPSS, IBM, USA). The data were expressed as the means ± standard deviation. Values of p < 0.05 were considered statistically significant.
Results
It was found out that the Minimum Inhibitory Concentration values of PJI-related S. aureus varied in a broad range (from 64 to 512 μg/ml) among different MLST subtypes and the bacteria were able to regain growth after 24 h in berberine of MIC value or higher concentrations. In addition, sub-inhibitory concentrations of berberine surprisingly enhanced biofilm formation in some S. aureus strains.
Conclusion
Traditional medicine is utilised by a large number of individuals, which provides abundant resources for modern medical science. In our study, berberine was found bactericidal against PJI related S. aureus, however, its antibacterial property was impacted by the MLST subtypes of the bacteria, both in planktonic and biofilm growth forms.
Similar content being viewed by others
Background
Prosthetic joint infection (PJI) is a disastrous complication after arthroplasty surgeries which causes great burden to both patients and surgeons, as well as social economy [1,2,3,4]. Staphylococcus aureus (S. aureus) is one of the leading causative pathogens of PJI [5,6,7,8]. Due to its array of virulence and the ability to form biofilm [7, 9,10,11,12,13], S. aureus-induced PJI is particularly difficult to combat. Furthermore, in recent years, the increasing occurrence of high morbidity and mortality of PJI has been proved associated with multidrug-resistant S. aureus [14, 15]. Therefore, finding new antimicrobial agents to help establish effective treatment and prophylaxis against S. aureus associated PJI has become a major concern in the surgeons’ community.
Berberine is an isoquinoline alkaloid extracted from a traditional Chinese herb named Huang-Lian (Coptis chinensis) and has been used for decades as an OTC (Over the Counter) drug to treat diarrhea and bowl disorder in China. Studies have found a lot more biological activities of berberine, such as antitumor [16, 17], antidiabetic [18,19,20], antiviral [21, 22], antifungal [23] and antibacterial in particular [24,25,26,27,28]. Robert et al. tested the antimicrobial effect of berberine against Coagulase-Negative staphylococcus standard strains [29]. Chu et al. demonstrated that berberine is active in killing Methicillin-Resistant S. aureus (MRSA) [30]. Guo et al. proved berberine was effective in inhibiting growth of S. aureus both in planktonic and biofilm cultures [31]. However, the strains tested in these studies were either not S. aureus strains or non-clinical strains. And the clinical S. aureus strains tested by Guo et al. were not associated with PJI. Further, the MLST types of the clinical S. aureus were not determined while different subtypes of S. aureus could have vastly different sensitivity to the same antimicrobial agents. These disadvantages may hinder the way of applying berberine into clinical PJI control. Therefore, in this study, we collected eighteen PJI-associated clinical S. aureus strains, determined their MLST types and tested the inhibitory effect of berberine against S. aureus in planktonic and biofilm status. Besides, to investigate the underlying mechanisms of berberine inhibiting S. aureus, transcriptomic profile of S. aureus treated with berberine was investigated by transcriptome sequencing of a clinical PJI-related S. aureus strain. And bioinformatics analysis including DEGs (Differentially Expressed Genes) selection, GO (Gene Ontology Consortium) functional enrichment and pathway significance enrichment were conducted.
Methods
Bacteria strains, media and reagents
In all, 18 isolates of staphylococcal aureus were collected from the cultures of PJI patients in joint surgery department, Shanghai Sixth people’s Hospital, Shanghai, China. After collection, the bacteria were given a series number from A to R and stored in Tryptic Soy Broth (TSB) medium with 20% of glycerol at − 80 °C for further use. Mueller–Hinton broth II (MHB II) and Tryptic soy broth (TSB) were purchased from Sangon Biotech (Shanghai, China). The berberine chloride (C20H18ClNO4, molecular weight 371.81) was purchased from Sigma-Aldrich (St Louis, MO, USA) and stock solutions at various concentrations were made in 1% dimethyl sulfoxide (DMSO) (Sangon Biotech) [32].
MLST determination and Berberine MICs test
Bacterial MLST was determined by the PCR amplification and sequencing of seven housekeeper genes (arc, aro, glp, gmk, pta, tpi, yqd) and referring the results to the database online. The MIC values of berberine against eighteen PJI-related S. aureus strains were determined using twofold serial dilutions in MHB II according to CLSI/NCCLS M100-S15 (CLSI, 2005) in triplicate. The MICs were defined as the lowest concentrations at which no visible growth was observed after 24 h.
Biofilm assay
Berberine was added to the TSB broth containing 1% glucose in 96-well plates (Corning Co., NY, USA) to reach a final volume of 100 μl and a series of concentrations (2, 4, 8, 16, 32, 64, 128, 256, and 512 μg/ml was only made when testing strain ST39). The cultures were then inoculated with 100 μl seed culture of S. aureus (5 × 10^5 CFU/mL). After incubating for 24 h at 37 °C, the supernatant was completely removed and the wells were washed three times with phosphate buffered saline (PBS) (pH 7.2). Then 200 μl methanol was used to stabilize the biofilm for 30 min and then dried at 60 °C. After that, the biofilm was stained with 200 μl of 0.1% crystal violet for 15 min. Unbound crystal violet was rinsed by PBS for three times. After drying 200 μl of 95% ethanol was added to each well and the plates were shaken for 1 h to release the stain from the biofilm. The absorbance of the biofilm was measured at 600 nm for three times. Wells containing 1% DMSO and bacteria was the bacterial growth control (GC).
Growth kinetics test
A suspension of 100 μl bacterial cultures (5 × 10^5 CFU/mL) in TSB was added to 100 μL of serially diluted berberine (0.5, 1, 2, 4, 8, 16, 32, 64, 128, 256, and 512 μg /mL) in 96-well plates (Corning Co., NY, USA). Microplates were incubated at 37 °C for 2, 6, 12 and 24 h, and the bacterial growth was evaluated by measuring the optical density of cultures at 600 nm wavelength with a Multiskan EX microplate reader (Thermo Electron Corp., Vantoa, Finland). Wells Molecules containing 1% DMSO with bacterial inoculum served as the bacterial growth control (GC).
Treatment with berberine
Staphylococcus aureus strain ST1792 was grown overnight in 4 mL of TSB at 37 °C. Two 15 ml test tubes containing 10 mL of TSB were inoculated with an overnight culture with an initial OD600 of 0.05. The bacteria were grown at 37 °C at 220 rpm to an OD600 of 0.3~0.4. Then, 500 μl of 1280 μg/mL berberine stock solution was added to the experiment tube, and DMSO solution was added to the control tube. The final concentration of berberine in the experimental tube was 1/2 MIC (64 μg/ml). The final concentration of DMSO in each culture was 1%, and such amounts of DMSO did not change the pH of the medium. The experimental and control cultures were incubated for a further 45 min at 37 °C, and then bacterial cells were collected and RNA isolation was performed. Three independent experiments were performed.
Total RNA isolation
The collected bacterial cells were placed in the RNA-protect Bacteria Reagent (QIAGEN GmbH, Germany) and incubated for 5 min at room temperature to stabilize the mRNA. After that, the cell suspensions were centrifuged at 8000×g for 5 min and the supernatant was discarded. Total RNA was purified using RNeasy Mini Kit (Qiagen) according to the manufacturer’s protocol. RNA quantity was measured using Agilent 2100 bioanalyzer.
Enrichment and sequencing of mRNA
A total of 10 μg of each RNA sample was subjected to further purification to enrich the mRNA using a MICROB Express Kit (Ambion) according to the manufacturer’s instructions. The mRNA sample was suspended in 25 μl RNA storage solution and the quality of mRNA was determined using Agilent 2100 Bioanalyzer. Bacterial mRNA was fragmented and the fragments were achieved in the size range of 200–250 bp using the Illumina TruSeq Stranded Kit (Illumina, USA), which was also used to generate the double-stranded cDNA to prepare RNA-seq library. All of the samples were sequenced using the Hiseq2000 (Illumina, USA) sequencer at Beijing Genomics Institute at Shenzhen.
Transcriptome assembly and annotation
Reads were aligned to Staphylococcus aureus subsp. aureus ST1792 (Genome sequenced before, data not shown) using the HISAT (Hierarchical Indexing for Spliced Alignment of Transcripts) [33]. The RNA-seq data analysis included the following steps. (1) If the pair-end reads satisfied N > 2% and low quality (quality value < 20) > 50%, the reads were removed. In addition, if the terminal 20 bp consisted of N or was of low quality, the reads were removed. Clean data were produced using the above quality control (QC) standards. (2) The clean data were aligned to S. aureus ST1792 using BWA. (3) Reads that could not be mapped or had incorrect alignment were removed. Quality control (QC) of alignment was produced on the standard above. (4) The commonly used fragments per kilo-base of transcript per million mapped fragments (FPKM) incorporate normalization steps to ensure that expression levels for different genes and transcripts are comparable across runs [34]. Based on FPKM normalization, analyses of distribution, coverage and differentially expressed genes were also performed.
Identification of differentially expressed genes
Differentially expressed genes were identified using DESeq2, which calculated expression in two or more samples and tested the statistical significance of each observed expression changes between them. Genes with an adjusted P value < 0.05, FDR ≤ 0.01 and fold change ≥2 were identified as differentially expressed. Finally, heat map and volcano plot were used to visualize and integrate the data produced by DESeq2 analysis.
Quantitative real-time RT-PCR used to validate RNA-seq data
Nine genes (icaA, icaR, fnbA, lrgA, lrgB, cidA, srrB, spa, nuc) that were significantly differential transcribed (P < 0.05, FDR < 0.01) under berberine treatment and related to the production of three types of biofilm matrix were selected for qRT-PCR to validate RNA-seq data. Gene information and primer used were shown in Table 1. RNA was reverse transcribed into cDNA using the PrimeScript™ RT reagent Kit with gDNA Eraser (TaKaRa, Japan) according to the manufacturer’s instructions. The qRT-PCR was performed in a 20 μ L volume using SYBR Green qPCR Master Mix (TaKaRa, Japan) as recommended by the manufacturer. The cDNA was subjected to real-time RT-PCR using the primer pairs listed in Table 2. Cycling conditions were 48 °C for 30 min and 95 °C for 15 min, followed by 40 cycles of 95 °C for 15 s and 60 °C for 1 min, and a dissociation step of 95 °C for 15 s, 60 °C for 30 s, and 95 °C for 15 s. Fold change between treatment samples and controls was calculated using 2–ΔΔCt method. All samples were analyzed in triplicate and housekeeping gene pyk was used as the internal reference to obtain basis of normalization [35, 36].
Statistical analysis
At least three independent replicates of each 96-well plate experiment were performed. The statistical analyses were conducted using Student’s t-test with SPSS 24.0(SPSS, IBM, USA). The data were expressed as the means ± standard deviation. Values of p < 0.05 were considered statistically significant.
Results
The MIC values to berberine of 18 S. aureus isolates varied among different MLST types
The MLST test showed that 18 PJI-related S. aureus isolates fell into eleven sub-types, with 1 each into ST15, ST17, ST188, ST39, ST1792, ST88, ST8, 2 into ST1281 and 3 into ST630, ST7, ST239 (Table 3), respectively. Among the 11 S. aureus sequence types, MIC values of berberine varied from 64 to 512 μg/ml. The highest MIC value was 512 μg/ml for ST 39 and the lowest was 64 μg/ml for ST239. The other 9 MLST types of S. aureus displayed the same berberine MIC value of 12 μg/ml (Table 3).
Berberine exerted excellent inhibiting effect on PJI-related S. aureus strains in planktonic form
Within 2 h of incubation, no significant growth of all tested S. aureus was detected (Fig. 1a and b). After 6 h of incubation, all tested strains showed an essential decrease in the number of bacteria (evidenced by OD value changes) when compared to control group (1% DMSO, Fig. 1c). After 12 h of incubation, within the range of berberine concentration from 32 to 512 μg/mL, a dramatic reduction in the number of bacteria was detected and a total growth inhibition was observed in some strains (Fig. 1d). After 24 h of the study, though some growth could be seen, substantial decreases were noticed in the number of bacteria within the range of berberine concentration from 32 to 512 μg/mL. At the concentrations of 256 and 512 μg/mL, growth of some strains was completely inhibited as the OD (Optical Density) value showed no change (Fig. 1e). The data from S. aureus ST39 showed that for all tested berberine concentrations lower than 512 μg/mL, this strain displayed substantial growth which indicated a relatively resistance to berberine compared to the other strains.
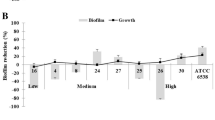
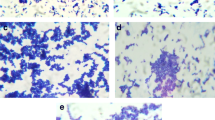
Sub-inhibitory concentrations of berberine promoted biofilm formation in some PJI-related S. aureus strains
Biofilm assay showed that for all 18 PJI related S. aureus strains, berberine yielded excellent anti-biofilm effect at concentrations of MIC or higher as the biofilm biomass was significantly lower than the control group (Fig. 2). However, at low concentrations, the anti-biofilm effect of berberine worked in two distinct modes. For the strains in group 2 (Fig. 2), the biofilm formation reduced as the concentration of berberine increased, which was in accordance with the findings of previous study [30]. However, for the strains in group 1 (Fig. 2), the biofilm formation surprisingly increased along with the concentration of berberine until meeting a sharp drop at 64 μg/ml (ST15, ST17, ST188 and ST630) or 32 μg/ml (ST1281 and ST39) indicating that low concentration of berberine enhanced biofilm formation of these S. aureus strains.
Berberine greatly impacted on global gene transcription of S. aureus ST1792
Transcriptomics analysis reveal the 795 significantly differentially expressed genes in S. aureus ST1792 treated with berberine, with 336 genes being up-regulated and 459 down-regulated (Fig. 3a). Volcano-plot map visualized the distribution of 2596 detectable differentially expressed genes, with the red plots representing 336 significantly up-regulated (log2 Fold-change ≥ 1 or P-value ≤ 0.05) genes, blue plots representing 459 significantly down-regulated (log2 Fold-change ≥ 1 or P-value ≤ 0.05) genes and grey representing 1801 non-significantly regulated (log2 Fold-change < 1 or P-value > 0.05) genes (Fig. 3b).
Inhibitory effects of berberine on clinical S.aureus biofilm formation. S. aureus strains were inoculated into TSB and cultured with different concentrations of berberine. Wells containing 1% DMSO and bacteria was the bacterial growth control (GC). Data are presented as mean ± standard deviation. *Significance was determined at P < 0.05 with comparison to the control group
Berberine induced great differentially expressions of major pathogenic genes in S. aureus ST1792
The pathogenesis of S. aureus in PJI is modulated by the expressions of its abundant pathogenic genes. Transcriptome sequencing revealed the changes in the expressions of major pathogenic genes in S. aureus ST1792 caused by berberine, as listed in Table 2 and Fig. 4. The biofilm of S. aureus is composed of different matrix including PIA (Polysaccharide Intercellular Adhesin), proteins and eDNA (Extracellular DNA) [37,38,39,40] involving different genes, respectively. Unexceptionally, the expressions pf positive regulators (icaA/B [41, 42], srrB [43], fnbA/B, spa [44], sasG [45], nuc [46], cidA [47]) of Staphylococcal biofilm were all up-regulated while negative regulators (icaR [48], spxA [49], lrgA/B [50]) down-regulated. Notably, two important biofilm regulator of S. aureus, the agr operon [51, 52] and sigB [53,54,55], were not differentially expressed in berberine.
Differentially expressed genes in berberine group compared to TSB control group. a Totally 795 significantly differentially expressed genes were detected, of which 336 were up-regulated and 459 were down-regulated (Significance: log2 Fold-change≥1 and P-value < 0.05). b Volcano-plot map of 2596 detectable differentially expressed genes Red: significantly up-regulated genes; blue: significantly down-regulated genes, grey: non- significantly regulated genes (log2 Fold-change < 1 or P-value> 0.05). Wells containing 1% DMSO and bacteria was the bacterial growth control (GC)
RNA-seq results were verified by qRT-PCR
The Log2 (Fold-change) of gene expression in berberine treatment group compared to control group revealed by RNA-seq and qRT-PCR are shown in Table 4. Although there is a slight difference in the exact fold change for each gene between qRT-PCR and RNA-seq, the differences were minor and the gene expression shares a similar trend in qRT-PCR with RNA-seq, which suggested the relatively high consistency between RNA-seq and qRT-PCR.
Discussion
The S. aureus is leading pathogen of prosthetic joint infection, imposing great challenges for PJI control, especially with the increasing occurrence of multi-drug resistant S. aureus recently due to inappropriate use of antibiotics [56]. Thus, species identification of the pathogen is widely acknowledged the key to right use of antibiotics and avoidance of drug resistance and have been strongly addressed in the clinical practice of orthopedic surgeons. However, it has been found that within the same species of bacteria, subtype strains could present distinct sensitivities to antimicrobials which hasn’t drawn enough attention in clinical practice. As berberine has been proved affective inhibiting wide range of microbes including S. aureus [30, 57], it holds a great potential to be a complementary antimicrobial agent for S. aureus induced PJI control. Our study first tested the sensitivity of eighteen PJI-related S. aureus to berberine and particularly investigated the differences among the MLST subtypes of S. aureus and. It was found that eighteen PJI relevant S. aureus showed eleven MLST subtypes and berberine presented significant antibacterial activity against all eleven PJI-associated S. aureus MLST subtypes, surprisingly however, the MIC values of berberine were quite diverse among different MLST types, as the highest MIC value was 512 μg/ml in ST 39 and the lowest was 64 μg/ml in ST239. The great diversity of MIC values among different MLST subtypes of S. aureus reveals the importance of determining the MLST subtypes and accordingly choose the appropriate dosage when applying berberine into clinical S. aureus induced PJI control.
Growth kinetics test of eighteen PJI-related S. aureus in berberine was conducted and significant planktonic growth inhibition was observed. Consistent with MIC test results, the growth kinetics test also revealed a MLST subtype-depend sensitivities to berberine of S. aureus relevant to PJI. Notably, after 24 h, all tested S. aureus strains except for ST39 showed remarkable growth in berberine concentrations over their MIC values. Similar results were observed when Robert et al. tested the antimicrobial effect of berberine against coagulase-negative staphylococcus strains in 2014 [29]. Giving these, we propose the reason could be that berberine does not exert antimicrobial efficacy against staphylococci by direct killing, but rather, by inhibiting the bacteria. Thus, certain amount of bacteria is able to survive and persist in high berberine concentration environment, and as berberine gradually depletes the survivors regain a favorable environment. This infers that although berberine displays excellent inhibiting effects against S. aureus while used alone berberine is not sufficient to control S. aureus infections. Therefore, we suggest that berberine be used as an ancillary drug in combination with other antibiotics in S. aureus related PJI control, since berberine shows remarkable synergy effects with a wide range of antibiotics [27, 29, 58, 59]. For example, a study by Zuo et al. revealed that berberine significantly lowered the MIC values of a series of antibiotics against S. aureus including MRSA [59]. Furthermore, since local host immunity is often impaired in PJI patients [60] and berberine has been proved able to improve host immunity [61,62,63], it is a promising candidate for clinical PJI control.
Biofilm plays an essential role in the pathogenesis of S. aureus-induced PJI [12, 13]. Berberine showed excellent anti-biofilm effect at concentrations of MIC or higher for all tested PJI related S. aureus strains, while unexpectedly, at sub-inhibiting concentrations berberine enhanced biofilm formation in a concentration-depend manner for nine strains (ST15, ST17, ST188, ST630, ST1281 and ST39). This was further confirmed by the transcriptome sequencing that at half MIC berberine concentration, the expression of genes responsible for producing three types of biofilm matrix in S. aureus were all up-regulated. This is likely to be due to the bacterial adaptation to the highly-stressed environment produced by berberine since under environmental stress, S. aureus tend to live in a biofilm-form instead of planktonic-form [64, 65]. This of acting mode of berberine on PJI-related S. aureus biofilm formation infers that the concentration of berberine must reach an ‘instant peak’ like an elevator when used in clinic for PJI control since slow concentration growth like an escalator may improve bacterial biofilm formation. However, oral administration of berberine shows poor absorption [66, 67] and berberine is toxic [68] when given through venous injection. Therefore, we recommend berberine be locally administrated when used in PJI control, for instance, contained in bone cement [69] in combination with other antibiotics. As a result, an ‘instant peak’ of berberine concentration is achieved and co-administration of berberine and antibiotics produces synergic antimicrobial effects and immune enhancement [27, 29, 58, 59, 70].
Conclusion
Our work showed the antimicrobial ability and the MLST type-dependent action mode of berberine against S. aureus related to PJI, which might provide reference for future application of berberine for controlling S. aureus induced PJI.
Availability of data and materials
The datasets generated and analysed during the current study are not publicly available due to its future use in our further studies including investigating the mechanisms of inconsistent antimicrobial effects of berberine against different S. aureus subtypes based on the RNA-seq profiles but are available from the corresponding author on reasonable request.
Abbreviations
- DEGs:
-
Differentially Expressed Genes
- DMSO:
-
Dimethyl sulfoxide
- eDNA:
-
Extracellular DNA
- GO:
-
Gene Ontology Consortium
- MHB II:
-
Mueller–Hinton Broth II
- MIC:
-
Minimum Inhibitory Concentration
- MLST:
-
Multi-locus Sequence Types
- MRSA:
-
Methicillin-Resistant S. aureus
- OD:
-
Optic Degree
- OTC:
-
Over the Counter
- PBS:
-
Phosphate Buffered Saline
- PIA:
-
Polysaccharide Intercellular Adhesin
- PJI:
-
Prosthetic Joint Infection
- RNA-seq:
-
RNA sequencing
- S. aureus :
-
Staphylococcal aureus
- TSB:
-
Tryptic Soy Broth
References
Zimmerli W. Clinical presentation and treatment of orthopaedic implant-associated infection. J Intern Med. 2014;276(2):111–9.
Tande AJ, Osmon DR, Greenwood-Quaintance KE, Mabry TM, Hanssen AD, Patel R. Clinical characteristics and outcomes of prosthetic joint infection caused by small colony variant staphylococci. MBio. 2014(5, 5):e01910–4.
Barrett L, Atkins B. The clinical presentation of prosthetic joint infection. J Antimicrob Chemother. 2014;69(Suppl 1):i25–7.
Legout L, Senneville E: Periprosthetic joint infections: clinical and bench research. Sci World J 2013, 2013:549091.
Holleyman RJ, Baker PN, Charlett A, Gould K, Deehan DJ. Analysis of causative microorganism in 248 primary hip arthroplasties revised for infection: a study using the NJR dataset. Hip Int. 2016;26(1):82–9.
Aggarwal VK, Bakhshi H, Ecker NU, Parvizi J, Gehrke T, Kendoff D. Organism profile in periprosthetic joint infection: pathogens differ at two arthroplasty infection referral centers in Europe and in the United States. J Knee Surg. 2014;27(5):399–406.
Fernandes A, Dias M. The microbiological profiles of infected prosthetic implants with an emphasis on the organisms which form biofilms. J Clin Diagn Res. 2013;7(2):219–23.
Nickinson RS, Board TN, Gambhir AK, Porter ML, Kay PR. The microbiology of the infected knee arthroplasty. Int Orthop. 2010;34(4):505–10.
Teterycz D, Ferry T, Lew D, Stern R, Assal M, Hoffmeyer P, Bernard L, Uckay I. Outcome of orthopedic implant infections due to different staphylococci. Int J Infect Dis. 2010;14(10):e913–8.
Otto M. Staphylococcus aureus toxins. Curr Opin Microbiol. 2014;17:32–7.
Arciola CR, Visai L, Testoni F, Arciola S, Campoccia D, Speziale P, Montanaro L. Concise survey of Staphylococcus aureus virulence factors that promote adhesion and damage to peri-implant tissues. Int J Artif Organs. 2011;34(9):771–80.
Gbejuade HO, Lovering AM, Webb JC. The role of microbial biofilms in prosthetic joint infections. Acta Orthop. 2015;86(2):147–58.
Dastgheyb S, Parvizi J, Shapiro IM, Hickok NJ, Otto M. Effect of biofilms on recalcitrance of staphylococcal joint infection to antibiotic treatment. J Infect Dis. 2015;211(4):641–50.
Foster TJ. Antibiotic resistance in Staphylococcus aureus. Current status and future prospects. FEMS Microbiol Rev. 2017;41(3):430–49.
McCarthy H, Rudkin JK, Black NS, Gallagher L, O'Neill E, O'Gara JP. Methicillin resistance and the biofilm phenotype in Staphylococcus aureus. Front Cell Infect Microbiol. 2015;5:1.
Sun Y, Xun K, Wang Y, Chen X. A systematic review of the anticancer properties of berberine, a natural product from Chinese herbs. Anti-Cancer Drugs. 2009;20(9):757–69.
Wang CY, Bai XY, Wang CH. Traditional Chinese medicine: a treasured natural resource of anticancer drug research and development. Am J Chin Med. 2014;42(3):543–59.
Tang LQ, Wei W, Chen LM, Liu S. Effects of berberine on diabetes induced by alloxan and a high-fat/high-cholesterol diet in rats. J Ethnopharmacol. 2006;108(1):109–15.
Zhang H, Wei J, Xue R, Wu JD, Zhao W, Wang ZZ, Wang SK, Zhou ZX, Song DQ, Wang YM, et al. Berberine lowers blood glucose in type 2 diabetes mellitus patients through increasing insulin receptor expression. Metabolism. 2010;59(2):285–92.
Zhang Q, Xiao X, Li M, Li W, Yu M, Zhang H, Ping F, Wang Z, Zheng J. Berberine moderates glucose metabolism through the GnRH-GLP-1 and MAPK pathways in the intestine. BMC Complement Altern Med. 2014;14(188):1–10.
Bodiwala HS, Sabde S, Mitra D, Bhutani KK, Singh IP. Synthesis of 9-substituted derivatives of berberine as anti-HIV agents. Eur J Med Chem. 2011;46(4):1045–9.
Hayashi K, Minoda K, Nagaoka Y, Hayashi T, Uesato S. Antiviral activity of berberine and related compounds against human cytomegalovirus. Bioorg Med Chem Lett. 2007;17(6):1562–4.
Xiao C-W, Ji Q-A, Wei Q, Liu Y, Bao G-L. Antifungal activity of berberine hydrochloride and palmatine hydrochloride against Microsporum canis -induced dermatitis in rabbits and underlying mechanism. BMC Complem Altern Med. 2015;15(177):1–15.
Slobodnikova L, Kost'alova D, Labudova D, Kotulova D, Kettmann V. Antimicrobial activity of Mahonia aquifolium crude extract and its major isolated alkaloids. Phytother Res. 2004;18(8):674–6.
Yan D, Jin C, Xiao XH, Dong XP. Antimicrobial properties of berberines alkaloids in Coptis chinensis Franch by microcalorimetry. J Biochem Biophys Methods. 2008;70(6):845–9.
Fan D-L, Xiao X-H, Ma X-J. Calorimetric study of the effect of protoberberine alkaloids in Coptis chinensis Franch on Staphylococcus aureus growth. Thermochim Acta. 2008;480(1–2):49–52.
Yu HH, Kim KJ, Cha JD, Kim HK, Lee YE, Choi NY, You YO. Antimicrobial activity of berberine alone and in combination with ampicillin or oxacillin against methicillin-resistant Staphylococcus aureus. J Med Food. 2005;8(4):454–61.
Cernáková MKD. Antimicrobial activity of berberine--a constituent of Mahonia aquifolium. Folia Microbiol. 2002;47(4):375–8.
Wojtyczka RD, Dziedzic A, Kepa M, Kubina R, Kabala-Dzik A, Mularz T, Idzik D. Berberine enhances the antibacterial activity of selected antibiotics against coagulase-negative Staphylococcus strains in vitro. Molecules. 2014;19(5):6583–96.
Chu M, Zhang MB, Liu YC, Kang JR, Chu ZY, Yin KL, Ding LY, Ding R, Xiao RX, Yin YN, et al. Role of Berberine in the treatment of methicillin-resistant Staphylococcus aureus infections. Sci Rep. 2016;6:24748.
Guo N, Zhao X, Li W, Shi C, Meng R, Liu Z, Yu L. The synergy of berberine chloride and totarol against Staphylococcus aureus grown in planktonic and biofilm cultures. J Med Microbiol. 2015;64(8):891–900.
Wang D, Yu L, Xiang H, Fan J, He L, Guo N, Feng H, Deng X. Global transcriptional profiles of Staphylococcus aureus treated with berberine chloride. FEMS Microbiol Lett. 2008;279(2):217–25.
Kim D, Langmead B, Salzberg SL. HISAT: a fast spliced aligner with low memory requirements. Nat Methods. 2015;12(4):357–60.
Trapnell C, Roberts A, Goff L, Pertea G, Kim D, Kelley DR, Pimentel H, Salzberg SL, Rinn JL, Pachter L. Differential gene and transcript expression analysis of RNA-seq experiments with TopHat and cufflinks. Nat Protoc. 2012;7(3):562–78.
Theis T, Skurray RA, Brown MH. Identification of suitable internal controls to study expression of a Staphylococcus aureus multidrug resistance system by quantitative real-time PCR. J Microbiol Methods. 2007;70(2):355–62.
Tan X, Qin N, Wu C, Sheng J, Yang R, Zheng B, Ma Z, Liu L, Peng X, Jia A. Transcriptome analysis of the biofilm formed by methicillin-susceptible Staphylococcus aureus. Sci Rep. 2015;5:11997.
Flemming HC, Wingender J. The biofilm matrix. Nat Rev Microbiol. 2010;8(9):623–33.
Jabbouri S, Sadovskaya I. Characteristics of the biofilm matrix and its role as a possible target for the detection and eradication of Staphylococcus epidermidis associated with medical implant infections. FEMS Immunol Med Microbiol. 2010;59(3):280–91.
Arciola CR, Campoccia D, Speziale P, Montanaro L, Costerton JW. Biofilm formation in Staphylococcus implant infections. A review of molecular mechanisms and implications for biofilm-resistant materials. Biomaterials. 2012;33(26):5967–82.
O'Neill E, Pozzi C, Houston P, Humphreys H, Robinson DA, Loughman A, Foster TJ, O'Gara JP. 34 a novel Staphylococcus aureus biofilm phenotype mediated by the fibronectin-binding proteins, FnBPA and FnBPB. J Bacteriol. 2008;190(11):3835–50.
O'Gara JP. Ica and beyond: biofilm mechanisms and regulation in Staphylococcus epidermidis and Staphylococcus aureus. FEMS Microbiol Lett. 2007;270(2):179–88.
Arciola CR, Campoccia D, Ravaioli S, Montanaro L. Polysaccharide intercellular adhesin in biofilm: structural and regulatory aspects. Front Cell Infect Microbiol. 2015;5:7.
Ulrich M, Bastian M, Cramton SE, Ziegler K, Pragman AA, Bragonzi A, Memmi G, Wolz C, Schlievert PM, Cheung A, et al. The staphylococcal respiratory response regulator SrrAB induces Ica gene transcription and polysaccharide intercellular adhesin expression, protecting Staphylococcus aureus from neutrophil killing under anaerobic growth conditions. Mol Microbiol. 2007;65(5):1276–87.
Merino N, Toledo-Arana A, Vergara-Irigaray M, Valle J, Solano C, Calvo E, Lopez JA, Foster TJ, Penades JR, Lasa I. Protein A-mediated multicellular behavior in Staphylococcus aureus. J Bacteriol. 2009;191(3):832–43.
Geoghegan JA, Corrigan RM, Gruszka DT, Speziale P, O'Gara JP, Potts JR, Foster TJ. Role of surface protein SasG in biofilm formation by Staphylococcus aureus. J Bacteriol. 2010;192(21):5663–73.
Beenken KE, Spencer H, Griffin LM, Smeltzer MS. Impact of extracellular nuclease production on the biofilm phenotype of Staphylococcus aureus under in vitro and in vivo conditions. Infect Immun. 2012;80(5):1634–8.
Rice KC, Mann EE, Endres JL, Weiss EC, Cassat JE, Smeltzer MS, Bayles KW. The cidA murein hydrolase regulator contributes to DNA release and biofilm development in Staphylococcus aureus. Proc Natl Acad Sci U S A. 2007;104(19):8113–8.
Jefferson KK, Pier DB, Goldmann DA, Pier GB. The teicoplanin-associated locus regulator (TcaR) and the intercellular adhesin locus regulator (IcaR) are transcriptional inhibitors of the Ica locus in Staphylococcus aureus. J Bacteriol. 2004;186(8):2449–56.
Pamp SJ, Frees D, Engelmann S, Hecker M, Ingmer H. Spx is a global effector impacting stress tolerance and biofilm formation in Staphylococcus aureus. J Bacteriol. 2006;188(13):4861–70.
Mann EE, Rice KC, Boles BR, Endres JL, Ranjit D, Chandramohan L, Tsang LH, Smeltzer MS, Horswill AR, Bayles KW. Modulation of eDNA release and degradation affects Staphylococcus aureus biofilm maturation. PLoS One. 2009;4(6):e5822.
Le KY, Otto M. Quorum-sensing regulation in staphylococci-an overview. Front Microbiol. 2015;6:1174.
Boles BR, Horswill AR. Agr-mediated dispersal of Staphylococcus aureus biofilms. PLoS Pathog. 2008;4(4):e1000052.
Lauderdale KJ, Boles BR, Cheung AL, Horswill AR. Interconnections between sigma B, agr, and proteolytic activity in Staphylococcus aureus biofilm maturation. Infect Immun. 2009;77(4):1623–35.
Pane-Farre J, Jonas B, Forstner K, Engelmann S, Hecker M. The sigmaB regulon in Staphylococcus aureus and its regulation. Int J Med Microbiol. 2006;296(4–5):237–58.
Rachid S, Ohlsen K, Wallner U, Hacker J, Hecker M, Ziebuhr W. Alternative transcription factor sigma(B) is involved in regulation of biofilm expression in a Staphylococcus aureus mucosal isolate. J Bacteriol. 2000;182(23):6824–6.
Post V, Wahl P, Uckay I, Ochsner P, Zimmerli W, Corvec S, Loiez C, Richards RG, Moriarty TF. Phenotypic and genotypic characterisation of Staphylococcus aureus causing musculoskeletal infections. Int J Med Microbiol. 2014;304(5–6):565–76.
Imenshahidi M, Hosseinzadeh H. Berberis Vulgaris and Berberine: An Update Review. Phytother Res. 2016;30(11):1745–64.
Zhou X, Yang C, Li Y, Liu X, Wang Y. Potential of berberine to enhance antimicrobial activity of commonly used antibiotics for dairy cow mastitis caused by multiple drug-resistant Staphylococcus epidermidis infection. Genet Mol Res. 2015;14(3):9683–92.
Zuo GY, Li Y, Han J, Wang GC, Zhang YL, Bian ZQ. Antibacterial and synergy of berberines with antibacterial agents against clinical multi-drug resistant isolates of methicillin-resistant Staphylococcus aureus (MRSA). Molecules. 2012;17(9):10322–30.
Wagner C, Obst U, Hansch GM. Implant-associated posttraumatic osteomyelitis: collateral damage by local host defense? Int J Artif Organs. 2005;28(11):1172–80.
Aziz M, Ghareeb D, Eweda S, Hussien H, Demellawy ME. Immunomodulatory effect ofBerberis vulgarisextracts on murine splenocytes and enrichment of dendritic cellsin vitro. Biotechnol Biotechnol Equip. 2015;29(6):1149–55.
Li H, Li XL, Zhang M, Xu H, Wang CC, Wang S, Duan RS. Berberine ameliorates experimental autoimmune neuritis by suppressing both cellular and humoral immunity. Scand J Immunol. 2014;79(1):12–9.
Tsang MS, Jiao D, Chan BC, Hon KL, Leung PC, Lau CB, Wong EC, Cheng L, Chan CK, Lam CW, et al. Anti-inflammatory activities of Pentaherbs formula, Berberine, Gallic acid and Chlorogenic acid in atopic dermatitis-like skin inflammation. Molecules. 2016;21(4):519.
Leimer N, Rachmuhl C, Palheiros Marques M, Bahlmann AS, Furrer A, Eichenseher F, Seidl K, Matt U, Loessner MJ, Schuepbach RA, et al. Nonstable Staphylococcus aureus small-Colony variants are induced by low pH and sensitized to antimicrobial therapy by Phagolysosomal Alkalinization. J Infect Dis. 2016;213(2):305–13.
Li T, Wang G, Yin P, Li Z, Zhang L, Liu J, Li M, Zhang L, Han L, Tang P. Effect of negative pressure on growth, secretion and biofilm formation of Staphylococcus aureus. Antonie Van Leeuwenhoek. 2015;108(4):907–17.
Zhang X, Qiu F, Jiang J, Gao C, Tan Y. Intestinal absorption mechanisms of berberine, palmatine, jateorhizine, and coptisine: involvement of P-glycoprotein. Xenobiotica. 2011;41(4):290–6.
Pan G, Wang G, Liu X, Fawcett J, Xie Y. The involvement of P-glycoprotein in berberine absorption. Pharmacol Toxicol. 2002;91(4):193–7.
Kheir MM, Wang Y, Hua L, Hu J, Li L, Lei F, Du L. Acute toxicity of berberine and its correlation with the blood concentration in mice. Food Chem Toxicol. 2010;48(4):1105–10.
Zou Q, Li Y, Zhang L, Zuo Y, Li J, Li J. Antibiotic delivery system using nano-hydroxyapatite/chitosan bone cement consisting of berberine. J Biomed Mater Res A. 2009;89(4):1108–17.
Wang Y, Wang F, Yang D, Tang X, Li H, Lv X, Lu D, Wang H. Berberine in combination with yohimbine attenuates sepsis-induced neutrophil tissue infiltration and multiorgan dysfunction partly via IL-10-mediated inhibition of CCR2 expression in neutrophils. Int Immunopharmacol. 2016;35:217–25.
Acknowledgements
Not applicable.
Funding
This study was supported by grant from The National Natural Science Funds of China (No.81772364 and No.81472108). The funders had no role in study design, data collection and interpretation, or the decision to submit the work for publication.
Author information
Authors and Affiliations
Contributions
JQ T: made substantial contributions to conception and design, acquisition and analysis and interpretation of data; involved in drafting the manuscript; given final approval of the version to be published. JW, CY, CZ Z, GY G: each partially helped in the acquisition and all given final approval of the version to be published. HS, JT: made contributions to conception and design; involved in revising it critically for important intellectual content; given final approval of the version to be published.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Tan, J., Wang, J., Yang, C. et al. Antimicrobial characteristics of Berberine against prosthetic joint infection-related Staphylococcus aureus of different multi-locus sequence types. BMC Complement Altern Med 19, 218 (2019). https://doi.org/10.1186/s12906-019-2558-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12906-019-2558-9