Abstract
Background
Occipitocervical (OC) fusion is indicated for OC instability and other conditions. Surgical complications include infection, malunion, and instrument failure.
Case presentation
We described a patient who underwent OC fusion and subsequently developed complication of cerebellar abscess and obstructive hydrocephalus. A 63-year-old male patient had been suffering from long-term neck pain and limb numbness and weakness. Cervical spine examination revealed tight stenosis at C1 level and instability in the C1-C2 joints. A C1 laminectomy with OC fusion was performed, and the patient was discharged. Unfortunately, a few days later, he went to the emergency department and complained of persistent dizziness, vomiting, and unsteady gait. Computed tomography (CT) and magnetic resonance imaging (MRI) images revealed a suspicious cerebellar abscess formation and hydrocephalus. Furthermore, CT images indicated that the left screw was loose, and the diameter of the right screw hole was much larger than the size of the screw. Besides, inappropriate length of the screw penetrated the occipital bone and may cause the disruption of dura mater. The patient underwent external ventricular drainage first, followed by abscess drainage and C1-C2 fixation a few days later. He was discharged without any further neurological deficits or infectious problems. The patient recovered with intact consciousness, full muscle strength, and improved numbness throughout the extremities, with a Nurick grade of 1. A follow-up magnetic resonance imaging at 3 months after surgery revealed near total resolution of the abscess. Inform consent was obtained from this patient.
Conclusions
Carefully conducting the procedure using the most tailored approach is essential to successful surgery, but this rare complication should always be kept in mind.
Similar content being viewed by others
Background
For C1-C2 instability, C1-C2 fixation is a common and well-developed technique. However, this procedure is more challenging and has higher incidence of the risk of damaging vertebral artery (VA) due to the complexity of C1-C2 [1,2,3]. Instead, some surgeons will choose occipito-cervical (OC) fixation and skip C1-C2 instead of C1-C2 instrumentation to avoid the high risk of injury to the VA. There are some postoperative disadvantages of OC fixation, such as reduced cervical mobility, difficulty in swallowing, postoperative neck stiffness, etc. [4,5,6,7,8]. Possible complications of OC fixation includes VA injury, screw loosening, neurological deterioration, bone fusion failure, cerebellar infraction, nerve or cord injury, and wound infection [9,10,11]. To the best of our knowledge, OC fusion complicated by cerebellar abscess formation has not been reported thus far. Thus, we reported a patient who underwent OC fusion for C1-C2 subluxation, and subsequently resulted in cerebellar abscess and hydrocephalus complications.
Case presentation
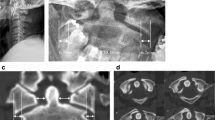
A 63-year-old male patient had been suffering from long-term neck pain and limb numbness. The dynamic flexion-extension view revealed the C1-C2 instability, and magnetic resonance imaging (MRI) of the cervical spine revealed hypertrophic ossification at the odontoid process, resulting in tight stenosis at C1 level and spinal cord edema (Fig. 1). C1 laminectomy and OC fixation using the screw-rod system were performed by an orthopedic surgeon in another hospital. To avoid the risk of VA injury, the surgeon chose occipito-C3-C4 fixation instead of C1-C2 fixation. The patient was discharged after 1 week, but a few days later, he began to experience persistent intolerable dizziness and vomiting. He went to the emergency department of our hospital. Physical examination revealed that his consciousness was clear and alert and had no change in muscle power compared to the status before surgery. He had no fever. However, the blood test showed a slight increase in leukocytosis (11,800 per mm3) and C-reactive protein level (< 5 mg/dl), indicating that the infection was in the early stage. Furthermore, the patient has symptoms of unsteady gait and right-sided dysmetria, suggesting that the patient may have a cerebellar lesion. Computed tomography (CT) further revealed a significant signal enhancement around the occipital screw (arrow in Fig. 2a) and a hypodense lesion in right cerebellar hemisphere (circled area in Fig. 2b-d). Although the presence of the screw interfered with CT image, it is still found that the position of the screw was the origin of brain abscess. In addition, the screw of inappropriate length were observed to penetrate through the occipital bone (Supplementary Figure 1). Since the CT image showed only a mild patchy enhancement, the lesion is more likely to be a cerebritis rather than a neoplasm. Therefore, we speculated that it should be a central nervous system (CNS) infection, and the patient was initially prescribed broad-spectrum antibiotics, including Vancomycin and Ceftazidime. Although the local metallic implants interfered with the interpretation of MRI, subsequent MRI confirmed the lesion as a 2.5 cm faint ring-enhanced cerebellar abscess based on the T1-weighted images with contrast medium and on the diffusion weighted imaging sequences (Fig. 3). A few days later, the patient became drowsier, so we decided to perform emergent external ventricular drainage (EVD) first to divert CSF and release intracranial pressure. When the wall of abscess is firmly formed, a second stage of suboccipital craniectomy will be performed to drain the brain abscess, and the implants will also be readjusted at the same time. One week after EVD surgery, the patient underwent an elective operation to drain the cerebellar abscess, debride the necrotic tissue, and inspect and readjust the hardware. Preoperative CT angiography (CTA) was conducted to evaluate the relationship between the VA and the planned trajectory, and it excluded a high-riding VA, demonstrating a safe trajectory for bilateral C2 transpedicular screws. In addition, the CTA scan also revealed that additional surgical changes in the positions of the left C3 and C4 screws may not be appropriate as it may breach the transverse foramen and damage the VA (Fig. 4). Moreover, the CT sagittal images further showed dislodgement of the occipital screw (Fig. 5a) and oversized diameter of the screw hole (Fig. 5b), indicating the failure of the instruments. Considering that the infectious status was limited to only around the occipital and cerebellar area and the persistent C1-C2 instability, therefore, in addition to the debridement and drainage of the abscess, the next step is to remove the previous hardware and reintroduce the C1 lateral mass and C2 transpedicular screws. In order to avoid the risk of VA injury when removing C3 and C4 screws, we left these screws in position. Next, we enlarged the hole of the right occipital screw and confirmed the abscess by echography. No purulent discharge was found, but necrotic tissue was found and debrided. The C1 lateral mass and C2 transpedicular screws were safely introduced under fluoroscopic guidance without VA damage (Fig. 6). The postoperative course was uneventful, and the symptoms of dizziness, unsteady gait, and dysmetria improved gradually. A few days later, the EVD was removed. No pathogens were detected from the final tissue and CSF cultures, antibiotics were prescribed for the patient for 8 weeks, and the patient was discharged uneventfully. An MRI examination at 3 months postoperatively revealed that the cerebellar abscess almost completely subsided (Fig. 7).
The axial images of four continuous CT of the patient with cerebellar abscess. The four continuous CT images from a to d represented continuous section from the base of the skull to top. The arrow in (a) indicated the position where the screw penetrates the dura mater. Circled area was indicated as brain abscess
CT sagittal images of the failure of the OC fusion instruments. (a) The arrow showed the dislodgement of the occipital screw and the screw hole. The screw was loose and not in their original position. (b) The arrow indicated the oversized diameter of the screw hole. The diameter of the screw hole is much larger than the size of the screw, indicating that the screw has no fixing effect
Discussion and conclusion
OC fusion is indicated for OC instability and some cases of C1-C2 subluxation, and it promises a satisfactory fusion rate and neurologic improvement [9]. The related complications include pneumonia, deep venous thrombosis of the lower extremity, wound infection, CSF leakage (dural injury), malunion, instrument failure, and VA injury [9, 12,13,14]. In the literature review, we found a report of intracranial infections and brain abscesses in patient using the Halo jacket for cervical spine fixation [15]. However, to date, no cerebellar abscess has been reported due to OC fixation. In our patient with true C1-C2 instability, the orthopedic surgeon did not first arrange a CTA study to evaluate the feasibility of C1-C2 instrumentation. Instead, he chose a simpler OC fusion procedure that eventually resulted in rare serious complications of cerebellar abscess and caused obstructive hydrocephalus, screw loosening, and inappropriate trajectory and position on the left-sided C3 and C4 screws. Furthermore, the postoperative plain film revealed that the occipital plate did not fit the curve of the occiput, which may have been the cause of the screw loosening (Supplementary Figure 2). Moreover, the length of the original right occipital screw seemed to be too long and penetrated the dura mater of the posterior fossa (Fig. 5b and Supplementary Figure 1), resulted in an increased risk of intracranial infection and eventually abscess formation.
OC fusion provides satisfactory arthrodesis and biomechanical stability to treat degenerative diseases, trauma, tumors, and inflammatory processes. The screw-rod system has more favorable outcomes and less adverse complications than other fusion techniques [16]. However, no matter which system is used, it is obvious that OC fusion techniques are much more easily and quickly performed than C1-C2 fusion when considering the risk of VA injury. Nevertheless, compared to OC fusion, C1-C2 instrumentation is the most straightforward procedure for C1-C2 subluxation and provides the most powerful rigid fixation without sacrificing too much range of motion. However, no matter which fusion technique is performed clinically, familiarization with every step of instrumentation is the most critical part of dealing with high cervical surgical procedures. This also includes determining the optimal and safe trajectory by intraoperative fluoroscope, choosing the appropriate length and type of screws, and avoiding infection at the surgical site. Furthermore, in addition to reduce surgery-related complications, we recommend the most appropriate surgical approach should be adopted based on the comprehensive acquisition and evaluation of the patient’s preoperative information.
In conclusion, OC fusion complicated with cerebellar abscess and resultant obstructive hydrocephalus has never been reported. Choosing the most tailored approach and being familiar with each surgical step are essential to avoid major complications.
Availability of data and materials
All data generated or analysed during this study are included in this published article and its supplementary information files.
Abbreviations
- CNS:
-
Central nervous system
- CSF:
-
Cerebrospinal fluid
- CT:
-
Computed tomography
- CTA:
-
CT angiography
- EVD:
-
External ventricular drainage
- MRI:
-
Magnetic resonance imaging
- OC:
-
Occipitocervical
- VA:
-
Vertebral artery
References
Gluf WM, Brockmeyer DL. Atlantoaxial transarticular screw fixation: a review of surgical indications, fusion rate, complications, and lessons learned in 67 pediatric patients. J Neurosurg Spine. 2005;2(2):164–9.
Gluf WM, Schmidt MH, Apfelbaum RI. Atlantoaxial transarticular screw fixation: a review of surgical indications, fusion rate, complications, and lessons learned in 191 adult patients. J Neurosurg Spine. 2005;2(2):155–63.
Yoshida M, Neo M, Fujibayashi S, Nakamura T. Comparison of the anatomical risk for vertebral artery injury associated with the C2-pedicle screw and atlantoaxial transarticular screw. Spine (Phila Pa 1976). 2006;31(15):E513–7.
Hong J, Lim S. Dysphagia after Occipitocervical fusion. N Engl J Med. 2017;376(22):e46.
Hamblen DL. Occipito-cervical fusion. Indications, technique and results. J Bone Joint Surg Br. 1967;49(1):33–45.
Martinez-Del-Campo E, Turner JD, Kalb S, Rangel-Castilla L, Perez-Orribo L, Soriano-Baron H, Theodore N. Occipitocervical fixation: a single Surgeon's experience with 120 patients. Neurosurg. 2016;79(4):549–60.
Hu Y, Yuan ZS, Kepler CK, Dong WX, Sun XY, Zhang J. Comparison of occipitocervical and atlantoaxial fusion in treatment of unstable Jefferson fractures. Indian J Orthop. 2017;51(1):28–35.
Bhimani AD, Chiu RG, Esfahani DR, Patel AS, Denyer S, Hobbs JG, Mehta AI. C1-C2 fusion versus Occipito-cervical fusion for high cervical fractures: a multi-institutional database analysis and review of the literature. World Neurosurg. 2018;119:e459–66.
Choi SH, Lee SG, Park CW, Kim WK, Yoo CJ, Son S. Surgical outcomes and complications after occipito-cervical fusion using the screw-rod system in craniocervical instability. J Korean Neurosurg Soc. 2013;53(4):223–7.
Tauchi R, Imagama S, Ito Z, Ando K, Hirano K, Muramoto A, Matsui H, Kato F, Yukawa Y, Sato K, et al. Complications and outcomes of posterior fusion in children with atlantoaxial instability. Eur Spine J. 2012;21(7):1346–52.
Christensson D, Saveland H, Rydholm U. Cervical spine surgery in rheumatoid arthritis. A Swedish nation-wide registration of 83 patients. Scand J Rheumatol. 2000;29(5):314–9.
Cappuccio M, De Iure F, Amendola L, Paderni S, Bosco G. Occipito-cervical fusion in post-traumatic instability of the upper cervical spine and cranio-cervical junction. Eur Spine J. 2013;22(Suppl 6):S900–4.
Lieberman IH, Webb JK. Occipito-cervical fusion using posterior titanium plates. Eur Spine J. 1998;7(4):308–12.
Zhao D, Wang S, Passias PG, Wang C. Craniocervical instability in the setting of os odontoideum: assessment of cause, presentation, and surgical outcomes in a series of 279 cases. Neurosurg. 2015;76(5):514–21.
Hioki A, Miyamoto K, Inoue T, Hosoe H, Shinoda J, Iwama T, Shimizu K. Successful antibiotic treatment for subdural empyema and seizure due to methicillin-resistant Staphylococcus aureus as a complication of halo orthosis usage: a case report. Eur J Orthop Surg Traumatol. 2012;22(Suppl 1):25–8.
Winegar CD, Lawrence JP, Friel BC, Fernandez C, Hong J, Maltenfort M, Anderson PA, Vaccaro AR. A systematic review of occipital cervical fusion: techniques and outcomes. J Neurosurg Spine. 2010;13(1):5–16.
Acknowledgments
None.
Funding
This work was supported by the Department of Neurosurgery, Chang gung Memorial Hospital, Taoyuan, Taiwan.
Author information
Authors and Affiliations
Contributions
CCL designed the concept of this study, collect and analyzed the clinical data, and drafted the manuscript. YTL developed the concept of this study, analyzed and interpreted the data, drafted the manuscript, and provided approval of the investigation. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
All authors declare they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1: Figure S1.
Arrow indicates image evidence of improper length of screws penetrating occipital bone after initial OC fusion.
Additional file 2: Figure S2.
A postoperative plain film of the initial OC fusion indicated that the occipital plate did not conform to the occipital curve.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lee, CC., Liu, YT. Occipitocervical fusion complicated with cerebellar abscess: a case report. BMC Musculoskelet Disord 21, 129 (2020). https://doi.org/10.1186/s12891-020-3157-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-020-3157-0