Abstract
Background
Management of Rüedi-Allgöwer III or AO/OTA type C3 pilon fracture presents numerous challenges to the orthopaedic surgeon. A joint preservation technique using a large autologous ilium with periosteum in combination with internal implant fixation was reported to improve the outcome of reconstruction.
Methods
Twenty-five patients according to Tscherne/Oestern FxCO-I closed fracture and FxOI open fractures classification after Rüedi-Allgöwer III or AO/OTA type C3 pilon fracture received a large autologous ilium with periosteum for tibiotalar joint reconstruction and open reduction and internal fixation (ORIF), between March 2015 and September 2018. The visual analog scale (VAS), American Orthopaedic Foot & Ankle Society (AOFAS) score, and Burwell and Charnley criteria were used for outcome analysis.
Results
Twenty patients with an average age of 45.2 years were followed for an average of 18.3 months. The VAS and AOFAS scores, and Burwell and Charnley ratings were recorded at the last follow-up after reconstructive surgery. Two patients developed redness and swelling at the wound site, but recovered after local care and dressing changes. No patient displayed deep surgical site infection, donor site complication, non-union or local complication during the final follow-up. The average bone union time was 18.3 months (range 3–36).
Conclusions
Large autologous ilium with periosteum in combination with ORIF can be performed for tibiotalar joint reconstruction. This experimental procedure reduces the risk of post-operative complications following articular reconstruction for Rüedi-Allgöwer III or AO/OTA type C3 pilon fractures in short follow-up.
Level of evidence
Level III, retrospective cohort study.
Similar content being viewed by others
Background
Unlike common ankle fractures, pilon fractures resulting from high-energy trauma are much more complex [1], and account for approximately 5 to 7% of all tibial fractures [2]. Recent data has demonstrated that the majority of patients are unable to regain their pre-operative work status, and experience greater reduction in post-operative quality of life compared to other orthopaedic procedures [3]. Furthermore, pilon fractures are associated with a high risk of would complications, and predispose the patient to developing post-traumatic osteoarthritis of the tibiotalar joint. The management of these fractures present numerous challenges to the orthopaedic surgeon, particularly for the Rüedi-Allgöwer III or AO/OTA type C3 pilon fracture, which represents severely comminuted fractures with impaction of the distal tibia and are heterogeneous in both injury pattern and treatment [4, 5].
Various methods for the pilon fracture reconstruction have been reported, including minimally invasive plate osteosynthesis (MIPO) [6], external fixation [7], open reduction and internal fixation (ORIF) [8], and intramedullary interlocking nails [9]. For cases combined with a risk of soft tissue and osseous sepsis, reconstructive techniques included early fixation, upgrading, primary arthrodesis, staged sequential posterior and anterior fixation, acute shortening, and trans-syndesmotic fibular plating [10]. Although the risk of infection and soft tissue complications may be reduced with the use of external fixation, this method may not allow optimal reduction of the joint surface and therefore may jeopardise long-term outcomes. Classic studies have reported the use of bone grafts in treating the bony defect after fracture reduction, but this has been associated with poor prognosis [11]. Consequently, there is a paucity of studies reporting the use of a large autologous ilium with periosteum for tibiotalar joint reconstruction in pilon fractures, and long-term outcomes following such treatment.
This study reports a single-stage surgical procedure for joint reconstruction in a cohort of patients with Rüedi-Allgöwer III or AO/OTA type C3 pilon fracture. The short-term outcomes of tibiotalar joint reconstruction are evaluated following the implantation of a large autologous ilium having periosteum together with ORIF. This procedure is associated with positive post-operative outcomes, and may help reduce the risk of complications, delay joint fusion or articular arthroplasty for post-traumatic ankle osteoarthritis.
Methods
Patient characteristics
This study was performed under approval by the ethics committee of Shanxi Medical University Second Hospital (2018LL036). Twenty-five patients were initially entered into this study, but only twenty were available for evaluation at the final follow-up. Characteristics of the twenty patients included in this study are presented in Table 1. Between March 2015 and September 2018, twenty patients (15 male and 5 female) with a mean age of 45.2 years (range: 19–68) underwent tibiotalar joint reconstruction using a large autologous ilium with periosteum harvested from the iliac crest (Fig. 1). The inclusion criteria were: Rüedi-Allgöwer III or AO/OTA type C3 pilon fractures, Tscherne/Oestern FxCO-I closed fractures and FxOI open fractures [12, 13], no episodes of compartment syndrome, and no exudation or skin shrinkage. The exclusion criteria were: Rüedi-Allgöwer I, II or AO/OTA type C1, C2 pilon fractures, Tscherne/Oestern FxCOII-III closed fractures and FxOII-IV open fractures, and patients lost to follow-up.
Schematic illustration of the surgical procedure. a Rüedi-Allgöwer III or AO/OTA type C3 pilon fractures are severely comminuted fractures with impaction of the distal tibia. b A large autologous ilium with periosteum is harvested from the iliac crest. c A clear view of the entire plafond and talus is obtained after distraction of the ankle joint with the tensor and removing the fracture fragment. d The concave side of ilium with periosteum is implanted directly into the residual subchondral bone using a k-wire, guided by the articular surface of the talus as a template. Cancellous bone from the graft is used to fill the bone defect following reduction of the articular segment. e The reconstructed tibiotalar joint and plafond are fixed by anatomically locked plates
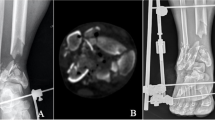
Pre-operative radiographs and 3D reconstructed computed tomography (CT) images were obtained to assess the severity of joint comminution, impaction, and displacement of fracture fragments (Fig. 2a, b). The visual analog scale (VAS) during daily activities and American Orthopaedic Foot & Ankle Society (AOFAS) [14] scores were recorded prior to surgery. These served as baseline data for comparison during follow-ups.
Surgical technique
Doppler ultrasonography was used to screen for deep vein thrombosis prior to commencing surgery. Surgery was performed under general anaesthesia or combined spinal-epidural anaesthesia in the float position under tourniquet control by a senior surgeon. The fractures were carefully protected and collected, and constructed stepwise according to procedures published by Rüedi and Allgöwer [15]. In 5 patients, ORIF was performed using an anteromedial combined with back-lateral surgical approach [16], while in the other 15 patients an anterolateral combined with back-medial approach was used [17]. Alternative and supplemental approaches were used as required depending on the fracture pattern and soft tissue situation.
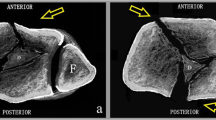
A large full-thickness autologous ilium (5 cm × 5 cm) was harvested from the patient’s iliac crest, consisting of cancellous bone with periosteal lamellae on each one side (Fig. 1b), using Wolfe-kawamoto’s technique [18]. The distance between skin bridges was maintained at larger than 7 cm. A clear view of the entire plafond and talus was obtained after distraction of the ankle joint with the tensor and removing the fracture fragment (Fig. 1c). The technique we describe here was to preserve the residual articular cartilage as much as possible, which would then be supported by the iliac crest bone graft. The concave side of ilium with periosteum (about 1 cm thickness) was implanted directly into the residual subchondral bone using a k-wire, with the articular surface of the talus as template. Cancellous bone from the graft was used to fill the bone defect for metaphyseal impaction of bone following reduction of the articular segment (Fig. 1d). In some cases where the cartilage is combined with severe comminuted fracture and cannot be distinctly recognized, the periosteal surface is used to articulate with the surface of the talus.
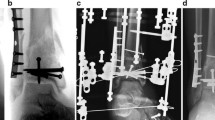
Fixation of the medial column was performed fundamentally with temporary k-wires, and small fragment screws were applied to give stability to the fracture site. The reconstructed tibiotalar joint and plafond were fixed by anatomically locked pates, which provided initial fixation and the ability to perform soft exercise (Fig. 1e). Donati vertical mattress sutures were used to close the wound [3]. Post-operative radiographs were taken on the next day of surgery and at the latest follow-up.
Post-operative management
All patients remained in splint or cast immobilisation until the wounds have healed and sutures could be removed. All patients commenced ankle motion exercises the day after operation or as soon as possible. Non-weight bearing movements were introduced thereafter, with progressively increasing amounts of weight bearing (10–15 kg) and range of motion. Patients resumed full weight bearing upon clinician recommendation based on fracture pattern and radiographic findings at follow-up. Prophylaxis for deep vein thrombosis was provided with the use of sequential compression garments and/or low molecular weight heparin throughout the time that the patient was hospitalised and during bed rest, until a maximum period of 14 days.
All patients were required to return for follow-up at 1, 3, 6 and 12 months after surgery, and each year thereafter. At follow-up, the progress of wound healing and any complications were recorded, and outcomes were evaluated using the VAS and AOFAS scores [14], the range of motion of the ankle joint, and radiographs which were used to assess the quality of fracture reduction, stability of fixation, and fracture alignment and union according to Burwell and Charnley criteria [19] (Fig. 2c). Three patients were asked to undergo MRI examination to show the integrity of the distal tibia (Fig. 2d). Implant removal was performed at 1–2 years post-operation, after the bone remodelling process was complete.
Results
Twenty patients who attended the final follow-up were included in this study. The mean operation time for the surgery was 120 min (range: 100–150), and the average wound recovery time was 16 days (range: 12–21). Two patients developed redness and swelling at the wound site, but recovered after local care and dressing changes. No patients displayed deep surgical site infection, donor site complications, non-union or extraction morbidity from the iliac donor site during follow-up. The mean follow-up duration was 18.3 months (range: 6–36), at which bone union was achieved in all patients. The mean VAS score decreased from 7.7 pre-operatively to 2.8 post-operatively, while the mean AOFAS score improved from 12 to 86. According to the Burwell and Charnley radiological criteria, 15 patients had an anatomic reduction, 4 had good reduction, and 1 had poor reduction. The healing progress of a typical case after surgery is shown in Fig. 2. Clinical outcomes of patients at the final follow-up are summarised in Table 2.
Discussion
Pilon fractures frequently lead to post-traumatic ankle osteoarthritis, with an incidence of up to 33–50% [20]. For treating Rüedi-Allgöwer III or AO/OTA type C3 pilon fractures, a consensus has not been reached in the literature regarding the optimal fixation method. The primary cause is unsatisfactory reduction of tibial plafond fractures [21], which results in elevated contract stress at the tibiotalar joint [22]. In this study, we report one experimental technique for tibiotalar joint reconstruction using large autologous ilium with periosteum that can be applied for the treatment of Rüedi-Allgöwer III or AO/OTA type C3 pilon fractures. The technique described allows for direct visualization and optimal reduction of both the articular surface and the metadiaphyseal component of the injury. Although the use of external fixation can be accomplished rapidly and limit additional soft tissue injury, this may also increase the likelihood of tibiotalar or subtalar joint stiffness [23]. Since accurate reduction of a displaced articular fracture is considered to have critical importance in minimizing the risk of developing post-traumatic osteoarthritis, we recommend that ORIF be performed after evaluating the soft tissue condition. This technique of combining an autologous ilium having periosteum with ORIF achieved satisfactory healing outcomes at greater than 6 months follow-up in all included patients, with preservation of joint function in the injured ankle and restoration of the patients’ ability to perform daily activities. In the long-term, better reconstruction may reduce the risk of developing degenerative changes in the tibiotalar joint, thus delay joint fusion or articular arthroplasty in the future.
Fresh articular allografts are frequently used for knee reconstruction following trauma, such as for fractures of the tibial plateau [24]. However, allografts are typically only indicated for young patients with significant articular defects, and their use to treat large tibiotalar defects in Rüedi-Allgöwer III or AO/OTA type C3 pilon fractures are seldomly reported. In this study, we reconstructed the tibiotalar joint using autologous ilium having periosteum harvested from the iliac crest, which are the gold standard of repair for defects with large amounts of bone loss. The success of this procedure partly depends on the time course of rehabilitation, where patients are advised to commence ankle motion exercises as soon as possible after operation. The mechanism for satisfactory articular reconstruction using concave side of ilium with periosteum is likely related to the influence of mechanical stress on joint tissue repair, which helps with the gradual transformation of granulation tissue at the defect site into bone tissue, fibrocartilage, and even hyaline cartilage. However, the characterization at 18 months in this study does not give definitive evidence of the repair tissue composition, and longer-term follow-up with noting of possible complications such as arthritic changes are necessary [24, 25]. Nevertheless, the restoration of ankle movement may introduce physiological loading that is beneficial to the healing and grinding of the articular surface, and reduce the risk of developing post-traumatic osteoarthritis [26].
Although we have demonstrated satisfactory outcomes in this study, the use of the described technique for tibiotalar joint reconstruction should be considered with caution. It has been reported that complete reduction in pilon fractures can lead to complete failure, such as non-union, avascular necrosis and osteomyelitis [27]. Some precautions that should be taken when employing this technique include: (1) the articular surface of the talus should be used as a template for reconstructing the joint relationship; (2) the residual inner and outer surrounding fractures should be restored to provide support to the bone autograft; and (3) a small bone hook can be applied to restore the vertical displacement of the joint bone fragment and recover the flatness of the articular surface. In this study, we found that a 7 cm skin bridge was required even with proper soft tissue management and appropriate timing of surgical intervention. However, other studies have suggested that the pattern of injury, rather than skin bridge dimension, should dictate the selection of surgical approach, and that a skin bridge of less than 7 cm can be used [28]. We also found that the anterolateral combined with back-medial approach was suitable for most patients and achieved good outcomes, which was in agreement with observations in other studies [17].
There were some limitations in our study. First, there was variation in the length of follow-up among the included patients, which ranged from 3 to 36 months. Combined with the small sample size, we were not able to obtain sufficient information on long-term joint status or draw definitive conclusions on the safety and efficacy of the reconstructive technique, but to assess the feasibility of our technique as a pilot study. No complications in 20 cases would give an upper 95% confidence interval of approximately 15% of not having a complication, and one poor reduction an upper 95% confidence interval of approximately 25%. The patients were also not assessed for the development or severity of post-traumatic osteoarthritis at follow-up evaluations. Second, the clinical outcomes were mainly based on subjective patient experience, as it was difficult to apply standardised objective measurements of ankle function and then to anticipate the probability of occurrence of ankle arthritis. Third, this study only included a small and selected cohort of patients with high-energy pilon fracture. The safety and efficacy of the described technique needs to be verified in a larger sample of patients across different research centers, and over consistent long-term time frames to generate more high-level evidence (by using random control trail studies) to inform its usefulness in the reconstruction of high-energy pilon fractures.
Conclusion
The use of a large autologous ilium with periosteum together with ORIF for tibiotalar joint reconstruction is an experimental technique for the treatment of Rüedi-Allgöwer III or AO/OTA type C3 pilon fractures, and may reduce post-operative complications in short-term follow-up.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ORIF:
-
Open reduction and internal fixation
- VAS:
-
Visual analog scale
- AOFAS:
-
American Orthopaedic Foot & Ankle Society
- MIPO:
-
Minimally invasive plate osteosynthesis
- CT:
-
Computed tomography
References
Jacob N, Amin A, Giotakis N, Narayan B, Nayagam S, Trompeter AJ. Management of high-energy tibial pilon fractures. Strat Trauma Limb Reconstr. 2015;10(3):137–47.
Mauffrey C, Vasario G, Battiston B, Lewis C, Beazley J, Seligson D. Tibial pilon fractures: a review of incidence, diagnosis, treatment, and complications. Acta Orthop Belg. 2011;77(4):432–40.
Zelle BA, Dang KH, Ornell SS. High-energy tibial pilon fractures: an instructional review. Int Orthop. 2019;43(8):1939–50.
Ruedi T. Fractures of the lower end of the tibia into the ankle joint: results 9 years after open reduction and internal fixation. Injury. 1973;5(2):130–4.
Fracture and dislocation compendium. Orthopaedic Trauma Association Committee for Coding and Classification. J Orthopaed Trauma. 1996;10 Suppl 1:v-ix, 1–154.
Rijal L, Sagar G, Mani K, Joshi KN, Joshi A. Minimizing radiation and incision in minimally invasive percutaneous plate osteosynthesis (MIPPO) of distal tibial fractures. Eur J Orthop Surg Traumatol. 2013;23(3):361–5.
Zhang SB, Zhang YB, Wang SH, Zhang H, Liu P, Zhang W, Ma JL, Wang J. Clinical efficacy and safety of limited internal fixation combined with external fixation for Pilon fracture: a systematic review and meta-analysis. Chin J Traumatol. 2017;20(2):94–8.
Carter TH, Duckworth AD, Oliver WM, Molyneux SG, Amin AK, White TO. Open reduction and internal fixation of distal Tibial Pilon fractures. JBJS Essent Surg Tech. 2019;9(3):e29.
Nork SE, Schwartz AK, Agel J, Holt SK, Schrick JL, Winquist RA. Intramedullary nailing of distal metaphyseal tibial fractures. J Bone Joint Surg Am. 2005;87(6):1213–21.
Kottmeier SA, Madison RD, Divaris N. Pilon fracture. Preventing complications. J Am Acad Orthop Surg. 2018;26(18):640–51.
Rüedi T, Allgower M. Fractures of the lower end of the tibia into the ankle-joint. Orthopedic Trauma Direct. 1969;7(05):25–9.
Tscherne H, Oestern HJ. A new classification of soft-tissue damage in open and closed fractures (author’s transl). Unfallheilkunde. 1982;85(3):111–5.
Oestern HJ, Tscherne H. Klassifizierung der Frakturen mit Weichteilschaden. Langenbecks Arch Chir. 1982;358(1):483.
Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994;15(7):349–53.
Ruedi TP, Allgower M. The operative treatment of intra-articular fractures of the lower end of the tibia. Clin Orthop Relat Res. 1979;138:105–10.
Leone VJ, Ruland RT, Meinhard BP. The management of the soft tissues in pilon fractures. Clin Orthop Relat Res. 1993;292:315–20.
Mehta S, Gardner MJ, Barei DP, Benirschke SK, Nork SE. Reduction strategies through the anterolateral exposure for fixation of type B and C pilon fractures. J Orthop Trauma. 2011;25(2):116–22.
Kukreja S, Raza H, Agrawal KT, Alok C. Iliac crest bone graft harvesting: prospective study of various techniques and donor site morbidity. Internet journal of orthopedic. Surgery. 2010;18:1–7.
Burwell HN, Charnley AD. The treatment of displaced fractures at the ankle by rigid internal fixation and early joint movement. J Bone Joint Surg Br. 1965;47(4):634–60.
Resch H, Pechlaner S, Benedetto KP. Long-term results after conservative and surgical treatment of fractures of the distal end of the tibia. Aktuelle Traumatol. 1986;16(3):117–23.
Liu X, An J, Zhang H, Li Y, Chen Y, Zhang W. Autologous Osteochondral graft for early posttraumatic arthritis of Tibiotalar joints after comminuted Pilon fractures in young patients. Foot Ankle Int. 2020;41(1):69–78.
Anderson DD, Van Hofwegen C, Marsh JL, Brown TD. Is elevated contact stress predictive of post-traumatic osteoarthritis for imprecisely reduced tibial plafond fractures? J Orthop Res. 2011;29(1):33–9.
Okcu G, Aktuglu K. Intra-articular fractures of the tibial plafond. A comparison of the results using articulated and ring external fixators. J Bone Joint Surg Br. 2004;86(6):868–75.
Keating JF, Simpson AH, Robinson CM. The management of fractures with bone loss. J Bone Joint Surg Br. 2005;87(2):142–50.
Hangody L, Kish G, Karpati Z, Szerb I, Udvarhelyi I. Arthroscopic autogenous osteochondral mosaicplasty for the treatment of femoral condylar articular defects. A preliminary report. Knee Surg Sports Traumatol Arthrosc. 1997;5(4):262–7.
Wu D, Peng C, Ren G, Yuan B, Liu H. Novel anterior curved incision combined with MIPO for Pilon fracture treatment. BMC Musculoskelet Disord. 2020;21(1):176.
Lee KB, Jeong SY, Kim SH, Shim DG. Complete reduction for Pilon fracture can make complete failure. J Am Podiatr Med Assoc. 2018;108(3):257–61.
Howard JL, Agel J, Barei DP, Benirschke SK, Nork SE. A prospective study evaluating incision placement and wound healing for tibial plafond fractures. J Orthop Trauma. 2008;22(5):299–305.
Acknowledgements
Not Applicable.
Funding
This study was supported by National Natural Science Foundation of China (Grant No. 81802204), China Postdoctoral Science Foundation (2020 M671453), Second Hospital of Shanxi Medical University Doctor’s Funds (No. 2017–105), Scientific and Technological Innovation Programs of Higher Education Institutions in Shanxi (2019 L0410), the Natural Science Foundation of Shanxi Province (Grant No. 201801D221117), and the Australian National Health and Medical Research Council (APP1120249).
Author information
Authors and Affiliations
Contributions
DL, JJL, and BW conceived and designed the study. DL, FSH, YYZ, and YL searched and selected relevant studies. DL, BW, and BZ extracted and interpreted data. DL, FSH, and JJL analyzed the data. DL and JJL wrote the paper. BW and BZ revised the manuscript. DL, JJL, YYZ, FSH, YL, BZ, and BW critically reviewed and approved the final manuscript. The author(s) read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was carried out with approval from the ethics committee of Shanxi Medical University Second Hospital (2018LL036). Informed consent was obtained as written form from every patient.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, D., Li, J.J., Zhu, Y. et al. Large autologous ilium with periosteum for tibiotalar joint reconstruction in Rüedi-Allgöwer III or AO/OTA type C3 pilon fractures: a pilot study. BMC Musculoskelet Disord 21, 632 (2020). https://doi.org/10.1186/s12891-020-03659-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-020-03659-7