Abstract
Background
Predictors of bone deterioration after hip fracture have not been well characterized. The aim of this study was to examine the associations of physical function and lean body mass (LBM) with loss of bone density and strength in older people recovering from a hip fracture.
Methods
A total of 81 over 60-year-old, community-dwelling men and women operated for a hip fracture participated in this 1-year prospective follow-up study. Distal tibia total volumetric bone mineral density (vBMDTOT, mg/cm3) and compressive strength index (BSI, g2/cm4) and mid-tibia cortical vBMD (vBMDCO, mg/cm3) and bending strength index (SSI, mm3) were assessed in both legs by peripheral quantitative computed tomography (pQCT) at baseline (on average 10 weeks after fracture) and at 12 months. At baseline, LBM was measured with a bioimpedance device and physical function with the Short Physical Performance Battery (SPPB) and perceived difficulty in walking outdoors. Robust multivariable linear regression models were used to estimate the associations of physical function and LBM with the change in bone parameters at 12-months.
Results
The mean change in distal tibia vBMDTOT and BSI in both legs ranged from − 0.9 to − 2.5%. The change in mid-tibia vBMDCO and SSI ranged from − 0.5 to − 2.1%. A lower SPPB score, difficulty in walking outdoors and lower LBM predicted greater decline in distal tibia vBMDTOT in both legs. A lower SPPB score and difficulty in walking outdoors were also associated with a greater decline in distal tibia BSI in both legs. At the midshaft site, a lower SPPB score and lower LBM were associated with greater decline in SSI on the fractured side.
Conclusions
Older hip fracture patients with low physical function and lower LBM may be at risk for greater decline in tibia bone properties during the first post-fracture year. Acknowledgement of the risk factors could assist in developing interventions and care to promote bone health and overall recovery.
Trial registration
ISRCTN, ISRCTN53680197. The trial was registered retrospectively but before the recruitment was completed. Registered March 3, 2010.
Similar content being viewed by others
Background
Substantial decrements in physical function and muscle occur after hip fracture [1, 2], and less than half of these patients recover their pre-fracture level of function [3, 4]. In addition, hip fracture is followed by accelerated and long-term decline in bone structure, density and strength [5,6,7,8,9], especially in the leg on the fractured side [6, 10]. Together with the loss of physical function, bone deterioration increases the risk for a subsequent fracture [11, 12]. Post-hip fracture bone loss can probably be explained in part by disuse, but to date systematic exploration of the factors contributing to post-fracture bone deterioration has been rather scarce.
Low level of physical function is a risk factor for poorer recovery after hip fracture [13]. With the present study population, we have previously shown better recovery of physical function in patients with less difficulty in their post-discharge ability to walk outdoors [13]. A low level of physical function may also prevent effective loading of the bones and could be related to reduced bone-loading physical activity. Moreover, owing to the strong relationship between bone and muscle [14], lower LBM could also contribute to the increase in post-hip fracture bone loss. The positive relationship between bone and muscle can be traced to several biochemical (myokines and osteokines) and biomechanical factors, including gravitational loading on weight-bearing bones and the associated effect of muscle contraction [15], which places the greatest load on bones [14]. In older men, higher LBM has also been associated with better functional recovery after hip fracture [16].
The few studies that have explored the factors contributing to bone loss after hip fracture [2, 17] have not reported either measures of bone strength or outcomes for the leg on the fractured side. The aim of this study was to examine whether physical function, measured with SPPB and perceived difficulty in walking outdoors, and LBM predict the change at 12 months in the bone density and strength of both legs in older men and women recovering from a recent hip fracture.
Methods
Design and participants
This study utilizes data from a randomized controlled trial (ISRCTN53680197) investigating the effects of a yearlong home-based rehabilitation program compared to standard care on mobility recovery among over 60-year-old, ambulatory and community-dwelling older people with a recent hip fracture [18]. The design and recruitment procedure have been reported in detail earlier [19]. Briefly, all men and women who had been operated for a femoral neck or pretrochanteric fracture (ICD code S72.0 or S72.1) in the Central Finland Central Hospital (Jyväskylä, Finland) between 1.3.2008 and 31.12.2010, and fulfilling the inclusion criteria were informed about the study (n = 269). Of these, 161 were interested and further informed on the study. After preliminary assessment of eligibility, 136 persons were invited to the baseline measurements. Patients suffering from severe memory problems (Mini Mental State Examination, MMSE < 18), alcoholism, a severe cardiovascular or pulmonary condition or some other progressive disease, and severe depression (Beck Depression Inventory BDI-II > 29) were excluded from the study. Thereafter, 81 eligible patients participated in the study.
After the baseline measurements, conducted on average 10 weeks post fracture, the participants were randomized into an intervention (n = 40) and a standard care control (n = 41) group using a computer-generated group allocation list generated by a blinded statistician, who was not involved in either the recruitment or data collection process. Blocks of 10, stratified by gender and surgical procedure (internal fixation vs arthroplasty), were used. Follow-up measurements were arranged at 3, 6, and 12 months after the baseline measurements. All assessments were conducted at the research laboratory, and all outcome assessors were blinded to the treatment-group assignment. For the present analyses, data from the rehabilitation and standard care control groups were pooled, since the intervention had no effect on bone properties [10], and only baseline and 12-month follow-up bone data were utilized.
The sample size calculations have been reported in detail before [18, 19]. Briefly, an a priori sample size calculation was performed for the primary outcome, mobility limitation, based on previously published longitudinal data on mobility recovery after a hip fracture [20]. Based on calculations, a minimum of 44 participants were needed in each group (in total 88 participants) to detect the expected difference between the study groups at a level of significance of α = 0.05 and β = 0.20. Sample size was calculated using an online sample size calculator (DSS researcher’s toolkit).
Intervention and control condition
All participants received standard care from the hospital. In addition, the intervention group received a year-long, physical rehabilitation program aimed at restoring mobility and physical functional capacity to the pre hip fracture level [18, 19]. The individually tailored program comprised an evaluation and modification of environmental hazards, guidance for safe walking, non-pharmacological pain management, motivational physical activity counselling and a progressive home exercise program. The intervention took place in the participants’ homes and included five to six home visits by a physiotherapist. The progressive home exercise program comprised strengthening exercises for the lower limb muscles using resistance bands, balance training in the standing position, stretching, and functional exercises including walking, reaching, turning in different directions and stair climbing [10, 18].
Peripheral quantitative computed tomography (pQCT)
Bone scans from the distal tibia (5% of measured tibial length proximal to the distal end plate) and tibial shaft (55%) of both legs were obtained by pQCT (XCT-2000, Stratec Medizintechnik, Pforzheim, Germany) according to methods described earlier [10]. The pQCT scans were analyzed with an automated threshold-free cortical bone detection method [the outer boundary detection and subsequent shrinking (OBS) procedure, OBS cortical bone detection 2.1] [21, 22]. The outcome variables for the distal tibia were total volumetric bone mineral density (vBMDTOT, mg/cm3) and compressive bone strength index (BSI, g2/cm4 = vBMDTOT2 × CSATOT) [8, 9]. For the midshaft site, the variables were cortical vBMD (vBMDCO) and a strength-strain index (SSI, mm3; density-weighted polar section modulus) reflecting the bone’s resistance to bending and torsional loads. The root mean square coefficient of variation (CVRMS) for the BMD and strength index measurements in our laboratory ranges from 0.4 to 1.6% [23].
Physical function
Physical function at baseline was measured using the Short Physical Performance Battery (SPPB) test, which includes habitual walking speed, chair rise and standing balance tests [24]. A higher score (range, 0–12) indicates better performance. Perceived difficulty in walking outdoors was assessed by a questionnaire with the following response categories: 1) no difficulties, 2) some difficulties, 3) a great deal of difficulties, 4) manage only with help, and 5) unable to manage even with help.
Lean body mass
Lean body mass (kg) was assessed with a bioimpedance device with eight polar electrodes (BC-418; TANITA, Tokyo, Japan). Participants were instructed to avoid caffeine for 2 h, alcohol for 36 h and physical exercise for 24 h before testing.
Health, fracture status and anthropometry
The presence of chronic conditions, use of prescription medications, fracture date and status, and type and date of surgery were assessed by means of a pre-structured questionnaire, current prescriptions and medical records and confirmed in a medical examination performed by a research nurse and a physician. Contraindications for the physical performance assessments were evaluated according to ACSM guidelines [25]. Body height and weight were measured using standard procedures, and body mass index was calculated as body weight divided by height squared (kg/m2). Fat percentage was assessed with bioimpedance device. Serum concentrations of 25-hydroxyvitamin D (25OHD, nmol/L) and parathyroid hormone (PTH, ng/L) were determined according to methods described earlier [10]. Smoking status was assessed by questionnaire and categorized as current, former and never smokers.
Statistical analysis
Mean values and standard deviations (SD) were calculated using standard procedures. To alleviate problems resulting from extreme outliers, we used the robust linear regression approach [26] to estimate the associations of the predictor variables with each dependent variable. The mean percentage changes in vBMD and the bone strength indices, used as outcome variables, were calculated as [(follow-up – baseline)/baseline × 100]. Baseline LBM, SPPB score and ability to walk outdoors were entered in the models at the same time as predictors. The SPPB scores were recoded into a single binary variable: 0) high performance (score ≥ 7) or 1) low performance (score < 7). A score below 7 indicates a high risk for disability [27]. The categories of perceived difficulty in walking outdoors were recoded as 0) major difficulties or unable (categories 3–5), or 1) no difficulties or minor difficulties (categories 1–2). Predictive mean matching of the ‘mice’ package [28] in the R programming environment was used to impute missing values in LBM for three subjects. The models were adjusted for potential confounders: age, gender, surgical procedure (internal fixation vs hemiarthroplasty vs total arthroplasty), number of chronic diseases and use of bisphosphonate medication (yes/no) at baseline. The study group was not included in the models, as no differences were observed in baseline characteristics between the groups and the intervention had no effect on bone properties [10]. The main reasons for missing bone data were inability to perform the measurements, inaccurate positioning of the leg, a technically invalid pQCT scan, substantial movement artifacts, and metal in tissues in the scanned region. For the distal tibia, a total of 154 valid scans were obtained at baseline, and 130 at 12 months. For the midshaft site, the corresponding numbers were 156 and 130. Descriptive analyses were performed using SPSS 24.0 software (IBM, NY, USA) and the robust linear regression models were analyzed using R version 3.5.1 (R core team, Vienna, Austria) with the significance level set at 5%. The study power, calculated for the main outcome, mobility limitation, was 78%.
Results
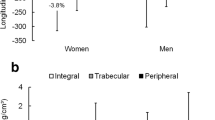
Baseline characteristics of the participants are shown in Table 1. During the 12-month study, three participants dropped out for personal reasons, and one participant died unrelated to the research procedures. The mean change from baseline to 12 months in distal tibia vBMDTOT was − 1.5 (SD 4.6) % on the fractured and − 0.9 (3.7) % on the non-fractured side. The corresponding changes for BSI were − 2.1 (8.8) % and − 2.5 (7.0) %, respectively. At the midshaft site, the mean change in vBMDCO was − 1.3 (2.3) % on the fractured and − 0.5 (1.6) % on the non-fractured side. The corresponding changes for SSI were − 2.1 (4.4) % and − 1.5 (3.4) %.
In the adjusted multivariable regression analyses, a lower SPPB score, difficulty in walking outdoors and lower LBM at baseline predicted greater decline in distal tibia vBMDTOT both on the fractured and non-fractured sides (Table 2). A lower SPPB score and difficulty in walking outdoors were also predictive of a greater decline in the distal tibia BSI on both sides. At the midshaft site, a lower SPPB score and lower LBM were associated with a greater decline in the SSI on the fractured side.
Discussion
In this 12-month follow-up study of older, community-dwelling men and women operated for a hip fracture, we found that lower physical function and lower LBM predicted greater decline in distal tibia bone density during the year following the fracture. Lower physical function was also associated with a greater decline in distal tibia bone strength. At the midshaft site, a lower SPPB score and lower LBM were predictive of a greater decline in bone strength on the fractured side.
Despite the large body of research on the factors contributing accelerated bone loss in aging people, very few have been conducted on hip fracture patients [2, 17] and none have examined potential predictors of the changes in bone properties over time. As in our previous studies [6, 10], bone deterioration was more pronounced in the leg on the fractured side, a finding which may partly be explained by disuse. No between-side differences in the predictors were, however, found except for mid-tibia SSI. At the midshaft site, a lower SPPB score and lower LBM were predictive of greater decline in the SSI on the fractured side only. Neither the decline in SSI on the non-fractured side nor the decline in cortical vBMD on both sides was associated with any of the factors studied, suggesting that the mid-tibia may not be equally sensitive to differences in the predictors used.
In the present study, a lower SPPB score (under 7) and major difficulty in the ability to walk outdoors predicted greater deterioration in distal tibia volumetric bone density and strength. This is in line with our previous findings indicating better functional recovery in patients with better function [13] and supports our hypothesis of better bone recovery in patients with a better capacity to load their bones. In old age, walking outdoors has also been associated with a greater amount of objectively measured physical activity [29]. Furthermore, our results are in line with previous studies suggesting better post-fracture functional recovery [16] and reduced age-related bone loss [30] for men with higher LBM. Moreover, in older, often frail and undernourished, hip fracture patients, higher LBM may also reflect better resources to cope with a prolonged catabolic state and the hip fracture-related stresses.
This study has its limitations. The study reports the results of a secondary analysis of an RCT, and the observational design demonstrates only associations, not causal relationships. Because of missing data and a relatively small sample size, we had to limit the number of possible confounders included in the analyses. Down-weighting the influence of outliers in the regression analyses further reduced the sample size but yielded more reliable regression coefficients. Moreover, the participants were community-living, and therefore the results may not be generalizable to all hip fracture patients. Furthermore, DXA or MRI would have provided more accurate LBM results. Finally, constraints related to the imaging method used, such as scan resolution, partial volume effect and beam hardening should be considered when interpreting the results. The strengths of the study include a population-based clinical study sample, a 3D imaging modality to assess changes in volumetric bone mineral density and estimated strength in the leg on the fractured side, and a longitudinal follow-up of sufficient length to detect changes in bone properties.
Conclusions
In conclusion, low physical function and lower LBM may increase the risk for accelerated bone deterioration in older hip fracture patients. Attention should be paid to patients at greater risk for poorer recovery, and more effective, multidimensional and individualized interventions and care should be provided to promote bone health and overall recovery. Due to limited possibilities to prevent bone deterioration after hip fracture, attention should be paid to physical function, muscle mass preservation and fall prevention before as well as after fracture occurrence.
Availability of data and materials
The datasets used and analyzed during the current study are available from SS on reasonable request.
Abbreviations
- 25OHD:
-
25-hydroxyvitamin D
- BSI:
-
Compressive bone strength index
- LBM:
-
Lean body mass
- OBS:
-
Outer boundary detection and subsequent shrinking procedure
- pQCT:
-
Peripheral quantitative computed tomography
- PTH:
-
Parathyroid hormone
- SPPB:
-
Short Physical Performance Battery
- SSI:
-
Strength-strain index
- vBMDCO :
-
Cortical volumetric bone mineral density
- vBMDTOT :
-
Total volumetric bone mineral density
References
Fox KM, Magaziner J, Hawkes WG, Yu-Yahiro J, Hebel JR, Zimmerman SI, et al. Loss of bone density and lean body mass after hip fracture. Osteoporos Int. 2000;11(1):31–5.
Wehren LE, Hawkes WG, Hebel JR, Orwig DL, Magaziner J. Bone mineral density, soft tissue body composition, strength, and functioning after hip fracture. J Gerontol A Biol Sci Med Sci. 2005;60(1):80–4.
Vochteloo AJ, Moerman S, Tuinebreijer WE, Maier AB, de Vries MR, Bloem RM, et al. More than half of hip fracture patients do not regain mobility in the first postoperative year. Geriatr Gerontol Int. 2013;13(2):334–41.
Handoll HH, Sherrington C, Mak JC. Interventions for improving mobility after hip fracture surgery in adults. Cochrane Database Syst Rev. 2011;(3):CD001704. https://doi.org/10.1002/14651858.CD001704.pub4.
Magaziner J, Wehren L, Hawkes WG, Orwig D, Hebel JR, Fredman L, et al. Women with hip fracture have a greater rate of decline in bone mineral density than expected: another significant consequence of a common geriatric problem. Osteoporos Int. 2006;17(7):971–7.
Mikkola T, Sipila S, Portegijs E, Kallinen M, Alen M, Kiviranta I, et al. Impaired geometric properties of tibia in older women with hip fracture history. Osteoporos Int. 2007;18(8):1083–90.
Reider L, Beck TJ, Hochberg MC, Hawkes WG, Orwig D, YuYahiro JA, et al. Women with hip fracture experience greater loss of geometric strength in the contralateral hip during the year following fracture than age-matched controls. Osteoporos Int. 2010;21(5):741–50.
Rathbun AM, Shardell M, Orwig D, Hebel JR, Hicks GE, Beck TJ, et al. Difference in the trajectory of change in bone geometry as measured by hip structural analysis in the narrow neck, intertrochanteric region, and femoral shaft between men and women following hip fracture. Bone. 2016;92:124–31.
Rathbun AM, Shardell M, Orwig D, Hebel JR, Hicks GE, Beck T, et al. Differences in the trajectory of bone mineral density change measured at the total hip and femoral neck between men and women following hip fracture. Arch Osteoporos. 2016;11:9–6 Epub 2016 Feb 4.
Suominen TH, Edgren J, Salpakoski A, Arkela M, Kallinen M, Cervinka T, et al. Effects of a home-based physical rehabilitation program on tibial bone structure, density, and strength after hip fracture: a secondary analysis of a randomized controlled trial. JBMR Plus. 2019;3(6):e10175.
Berry SD, Samelson EJ, Hannan MT, McLean RR, Lu M, Cupples LA, et al. Second hip fracture in older men and women: the Framingham study. Arch Intern Med. 2007;167(18):1971–6.
Lonnroos E, Kautiainen H, Karppi P, Hartikainen S, Kiviranta I, Sulkava R. Incidence of second hip fractures. A population-based study. Osteoporos Int. 2007;18(9):1279–85.
Sipilä S, Salpakoski A, Edgren J, Sihvonen SE, Turunen K, Pesola M, et al. Recovery of lower extremity performance after hip fracture depends on prefracture and postdischarge mobility: a subgroup analysis of a randomized rehabilitation trial. J Am Geriatr Soc. 2016;64(9):25.
Burr DB. Muscle strength, bone mass, and age-related bone loss. J Bone Miner Res. 1997;12(10):1547–51.
Cianferotti L, Brandi ML. Muscle-bone interactions: basic and clinical aspects. Endocrine. 2014;45(2):165–77.
Di Monaco M, Vallero F, Di Monaco R, Tappero R, Cavanna A. Muscle mass and functional recovery in men with hip fracture. Am J Phys Med Rehabil. 2007;86(10):818–25.
Wehren LE, Hawkes WG, Hebel JR, Orwig D, Zimmerman SI, Fox KM, et al. Predictors of bone loss after hip fracture. Osteoporos Int. 2004;15(2):125–31.
Salpakoski A, Tormakangas T, Edgren J, Kallinen M, Sihvonen SE, Pesola M, et al. Effects of a multicomponent home-based physical rehabilitation program on mobility recovery after hip fracture: a randomized controlled trial. J Am Med Dir Assoc. 2014;15(5):361–8.
Sipila S, Salpakoski A, Edgren J, Heinonen A, Kauppinen MA, Arkela-Kautiainen M, et al. Promoting mobility after hip fracture (ProMo): study protocol and selected baseline results of a year-long randomized controlled trial among community-dwelling older people. BMC Musculoskelet Disord. 2011;12:277.
Visser M, Harris TB, Fox KM, Hawkes W, Hebel JR, Yahiro JY, et al. Change in muscle mass and muscle strength after a hip fracture: relationship to mobility recovery. J Gerontol A Biol Sci Med Sci. 2000;55(8):434.
Cervinka T, Hyttinen J, Sievanen H. Threshold-free automatic detection of cortical bone geometry by peripheral quantitative computed tomography. J Clin Densitom. 2012;15(4):413–21.
Cervinka T, Sievanen H, Lala D, Cheung AM, Giangregorio L, Hyttinen J. A new algorithm to improve assessment of cortical bone geometry in pQCT. Bone. 2015;81:721–30.
Rantalainen T, Heinonen A, Komi PV, Linnamo V. Neuromuscular performance and bone structural characteristics in young healthy men and women. Eur J Appl Physiol. 2008;102(2):215–22.
Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49(2):85.
Haskell WL, Lee IM, Pate RR, Powell KE, Blair SN, Franklin BA, et al. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007;39(8):1423–34.
Venables WN, Ripley BD. Modern applied statistics with S-PLUS. 3rd ed. New York: Springer; 1999.
Guralnik JM, Ferrucci L, Simonsick EM, Salive ME, Wallace RB. Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. N Engl J Med. 1995;332(9):556–61.
van Buuren S, Groothuis-Oudshoorn K. Mice: multivariate imputation by chained equations in R. J Stat Softw. 2011;45(3):1–67.
Portegijs E, Tsai L, Rantanen T, Rantakokko M. Moving through life-space areas and objectively measured physical activity of older people. PLoS One. 2015;10(8):e0135308.
Kim KM, Lim S, Oh TJ, Moon JH, Choi SH, Lim JY, et al. Longitudinal changes in muscle mass and strength, and bone mass in older adults: gender-specific associations between muscle and bone losses. J Gerontol A Biol Sci Med Sci. 2018;73(8):1062–9.
Acknowledgments
The authors sincerely thank all the participants of this study. We would also like to thank the personnel of the Physiotherapy Department of the Central Finland Health Care District for their work in the recruitment of the participants and data collection. Additionally, we are also grateful to various persons who assisted in data collection: Veera Farin, Suoma Korhonen, Hanna-Maija Lapinkero, Katri Turunen, Mervi Matero, Tuovi Nykänen, Jenni Rouhiainen, Emma Takkinen, and Leena Tulla. We express our warmest gratitude to physicians Jukka Vanhatalo and Pirkko Jäntti for medical screening and Professor Urho Kujala for medical surveillance during the measurements.
CONSORT statement
This study adheres the CONSORT guidelines.
Funding
The study was supported by grants from the Ministry of Education and Culture (SS, Grants Dnro 43/627/2007, 63/627/2008, 79/627/2009) and Kela (the Social Insurance Institution of Finland) (SS, Grant Dnro 24/26/2007). TT was funded by the Academy of Finland (grant no. 286536) and TR was an Academy Research Fellow during the preparation of this manuscript (Academy of Finland grant numbers 321336 and 328818). The funders had no role in the study design, data collection, analyses, or interpretation, or in writing the manuscript.
Author information
Authors and Affiliations
Contributions
Study design: SS, AH, MK. Study conduct: SS, JE, AS, MK. Data collection: SS, JE, AS, MK. Data analysis: THS, TC, TT. Data interpretation: THS, TR, TT, AH, SS. Drafting manuscript: THS. Revising manuscript content: THS, JE, AS, MK, TC, TR, TT, AH, SS. Approving final version of manuscript: THS, JE, AS, MK, TC, TR, TT, AH, SS. THS, TC, TT, SS take responsibility for the integrity of the data analysis.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All participants gave their written informed consent and permission to review their medical records prior to participation in the study. The study was approved by the Ethics Committee of the Central Finland Health Care District (Dnro56/2007) and conformed with the principles of the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Suominen, T.H., Edgren, J., Salpakoski, A. et al. Physical function and lean body mass as predictors of bone loss after hip fracture: a prospective follow-up study. BMC Musculoskelet Disord 21, 367 (2020). https://doi.org/10.1186/s12891-020-03401-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-020-03401-3