Abstract
Background
Non-specific neck pain and headache are major economic and individual burden in office-workers. The aim of this study is to investigate the effect of a multi-component intervention combining workstation ergonomics, health promotion information group workshops, neck exercises, and an app to enhance intervention adherence to assess possible reductions in the economic and individual burden of prevalent and incident neck pain and headache in office workers.
Methods/design
This study is a stepped wedge cluster-randomized controlled trial. Eligible participants will be any office-worker aged 18–65 years from two Swiss organisations in the Cantons of Zurich and Aargau, working more than 25 h a week in predominantly sedentary office work and without serious health conditions of the neck. One hundred twenty voluntary participants will be assigned to 15 clusters which, at randomly selected time steps, switch from the control to the intervention group. The intervention will last 12 weeks and comprises workstation ergonomics, health promotion information group workshops, neck exercises and an adherence app. The primary outcome will be health-related productivity losses (presenteeism, absenteeism) using the Work Productivity and Activity Impairment Questionnaire. Secondary outcomes are neck disability and pain (measured by the Neck Disability Index, and muscle strength and endurance measures), headache (measured by the short-form headache impact test), psychosocial outcomes (e.g. job-stress index, Fear-Avoidance Beliefs Questionnaire), workplace outcomes (e.g. workstation ergonomics), adherence to intervention, and additional measures (e.g. care-seeking). Measurements will take place at baseline, 4 months, 8 months, and 12 months after commencement. Data will be analysed on an intention to treat basis and per protocol. Primary and secondary outcomes will be examined using linear mixed-effects models.
Discussion
To the authors’ knowledge, this study is the first that investigates the impact of a multi-component intervention combining current evidence of effective interventions with an adherence app to assess the potential benefits on productivity, prevalent and incident neck pain, and headache. The outcomes will impact the individual, their workplace, as well as private and public policy by offering evidence for treatment and prevention of neck pain and headache in office-workers.
Trial registration
ClinicalTrials.gov, NCT04169646. Registered 15 November 2019 - Retrospectively registered.
Similar content being viewed by others
Background
Non-specific neck pain (NP) is a major burden in industry due to lost productivity in terms of absenteeism and presenteeism as well as personal suffering from pain, disability, or reduced quality of life [1]. Moreover, NP has a high tendency for persistence and recurrence [1]. In 2010, a Swiss federal directive indicated that 68% of office-workers experienced NP on at least 1 day per year, while a recent study examining representative Zurich-based young and middle-aged adults indicates NP prevalence between 18 and 55%; both percentages appear at the upper end of global estimates [2, 3]. In another study, 13% of symptomatic office-workers reported reduced work productivity due to NP of nearly 22% [4].
In a Swiss survey, 35% of more than twelve thousand office-workers complained about having at least one headache episode within the last 4 weeks [3]. The 12-month-population prevalence for headache was approximately 34% for Switzerland, leading to a second rank for all health-related complaints [5]. In women in particular, headache ranked first in Switzerland (37%) [5]. These figures have been confirmed by a European census including 27 states (n = 28,079), which also comprises data from Switzerland (n = 871). However, these data relate not only to office-workers [5].
The workplace is increasingly becoming the arena for many health initiatives not only because of the amount of time an individual spends at the workplace, but also due to the strong link between work and health, and between health and productivity [6, 7]. Most current workplace-based strategies for the prevention and management of NP in office-workers fall into two broad categories: ergonomic-based interventions targeting the workstation or environment, and exercise-based interventions targeting the workers’ capacity to do their job [8, 9]. Recent studies examined the effect of workplace ergonomics, neck exercise, or health promotion on the individual burden of pain and disability as summarized below.
Three studies showed a positive effect of an ergonomic intervention on economic burden (productivity), but no effect on the individual burden of pain or disability [10,11,12]. A systematic review and meta-analysis by Chen et al. [13] questioned the value of stand-alone workstation ergonomic interventions in the office for people with NP which, is supported by strong evidence of no effect. One study was in favour of a multi-component ergonomic intervention, and another in favour of low monitor angles [14, 15]. Despite this contradictory and underwhelming evidence supporting workstation ergonomics, it is generally considered best practice for the work environment and most companies now provide workstations that can be adjusted to suit each employee [16]. However, a worker’s use or non-use of these often expensive items has not been sufficiently explored.
Health promotion is a broad field inclusive of interventions targeting the physical and psychosocial aspects of the individual and the workplace. Two systematic reviews showed a positive effect of health promotion intervention on work productivity [17, 18].
Exercise is a common treatment for office-workers suffering from musculoskeletal disorders [19, 20]. Likewise, in office-workers exercises may alleviate headache [21]. A systematic review and meta-analysis showed that strengthening exercises should be favoured to endurance and stretching exercise for the treatment of NP in office-workers [22]. An Australian study examined the impact of neck exercises on workplace productivity in monetary terms specific to office-workers within participating companies [23]. This study found evidence that neck strengthening exercises and best-practice ergonomics positively influence productivity and pain [23]. Other recent studies show improved productivity with exercise-based interventions [24,25,26,27,28].
Independent of the mode of the intervention (neck exercise, workstation ergonomics, health promotion), adherence to an intervention still remains a huge problem. Different studies observed greater effect with higher participation, which points to a need for an intervention that additionally encourages adherence [23, 29, 30]. A way to enhance exercise adherence is the use of an exercise app [31]. Main benefits of an app are the constant availability of the exercise program and an interactive technology with feedback and reminder.
To the authors’ knowledge, no research project has investigated the effect of a multi-component intervention, that includes all current evidenced aspects, and tested it against ‘as usual’ practise to assess the economic burden (work productivity) of prevalent and incident NP. Thus, the aim of this study is to investigate the impact of a multi-component intervention for office-workers that combines the evidence-based interventions of workstation ergonomics, health promotion, neck exercise, and an app to enhance adherence to intervention with regard to productivity, prevalent and incident NP, and headache. The overarching hypothesis is that work productivity will be improved by empowering workers to reduce NP- and headache-related presenteeism and absenteeism. Furthermore, NP, headache and/or disability (primary and secondary prevention) will be reduced and job stress and health-related quality of life will be improved.
Methods / design
Study design
A stepped wedge cluster-randomized controlled trial (RCT) with a multi-component intervention group is planned for 2020. In a stepped wedge cluster RCT, each participant completes a control and intervention period [24, 32].
This study protocol was written according to the SPIRIT (Standard Protocol Items for Randomized Trials) recommendations [33].
Participants
Study setting and eligibility criteria
Participants will be recruited from two Swiss organisations in the Cantons of Zurich and Aargau towards the end of 2019. Inclusion criteria will be Swiss office-workers, who suffer from NP or want to take prevention of neck pain or headache, aged 18–65 years, working more than 25 h per week (0.6 full-time equivalent) in predominantly sedentary office work and have provided written informed consent. In addition, participants will have to be able to communicate in German (written, spoken). Exclusion criteria are in alignment with European taskforce (EUTF) recommendations and will be health conditions such as previous trauma or injuries to the neck (NP grade 4 [34]), specific diagnosed pathologies (e.g., congenital cervical abnormalities stenosis, fracture, radiculopathy) or inflammatory condition (e.g., rheumatoid arthritis), any history of cervical spine surgery or if exercise is contraindicated (e.g., medical advice, own beliefs) [35]. Participants who anticipate prolonged absence from work (more than four consecutive weeks) during the study intervention period and / or pregnant women will be excluded.
Recruitment
The project coordinator will distribute information (e-mail, flyer, announcement) to participating organisations to forward to employees. To enhance recruitment, short presentations about the study will be offered as required in each organisation. Employees willing to participate will be directed to the study website for further information about the research and to register their interest. Screening of interested employees will be completed in person.
Allocation to cluster and group
The project coordinator will allocate eligible participants to a cluster (de-identified) until the required number is reached for each intake. A senior statistician blinded to the identity of individuals will randomise clusters to a sequence within the period of data collection when clusters change from the control to the intervention condition (group 1 to 3). A cluster is defined as a group of seven office-workers located on the same floor, room or work group. Fifteen clusters will be required to achieve a sample size of 120. The study coordinator will notify individuals of their allocation, collect baseline data, and communicate between participants and the intervention health professional to organize assessments.
Timeline
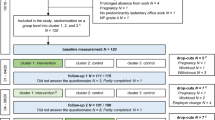
The study duration for each participant is approximately 1 year. After recruitment, screening, and confirmation of eligibility, clusters will be randomly assigned to the groups. The study intervention will start according to their cluster affiliation (Fig. 1). Every 16 weeks, they will be asked to complete follow-up assessments including online-surveys and physical examinations. Each participant will receive the intervention within their cluster at the time point scheduled by the randomization procedure.
Intervention
The multi-component intervention will last for 12 weeks and will combine four existing evidence-based interventions. Each participant will receive all four interventions.
-
Workstation ergonomics: Participants’ workstation ergonomics will be assessed using an observation-based ergonomics assessment checklist for office-workers adapted to Swiss guidelines [36]. Based on the initial assessment, best practice ergonomics will be applied individually using existing infrastructure [23]. Topics will include for example the adjustment of the chair, desk, and monitor.
-
Health promotion: Participants will attend health promotion information group workshops for approximately 1 h per week for 12 weeks. Content will include: attitudes to health and elements of success (including sleep); basic anatomical knowledge; behaviour change towards success; common workplace mental health issues; conflict management and resilience in the workplace; job stress and how to deal with it; keeping active (sit less, move more); keeping up the momentum and motivation; practical healthy eating; role of digital media; self-esteem; stress and relaxation workshop; and text-neck and how to avoid it [23, 37]. ‘Text-neck’ describes mechanical exposures on the neck, including static loading, non-neutral postures, and repetitive motions, associates with viewing portable devices over prolonged periods of time. The topics were selected in consultation with the organisations and on the basis of previous studies [23].
-
Neck exercise: Participants will receive an individual progressive exercise programme aimed at conditioning the muscles of the neck and shoulder girdle. The exercises will be performed in groups (maximum of 12 per group) at the workplace in a dedicated room, for approximately 1 h (3 × 20 minutes) per week; once per week supervised by a physiotherapist, a human movement scientist, or a health scientist, and twice per week self-administrated. A standard sequence of exercises will be prescribed to all participants, but their implementation and progression will be within the specific capabilities of the individual considering potential age- and gender-specific requirements. Participants will perform shoulder girdle exercises (bilateral shoulder shrugs; bilateral scapular raise; bilateral incline shoulder external rotation in squat position; bilateral shoulder extension; shoulder row; bench dips; incline push-ups), progressing from un-resisted to resisted utilising variable resistance bands, and neck exercises (using the hand to apply resistance during neck flexion, extension and rotation) [38, 39]. Training load for each individual will be based on their one-repetition maximum (1-RM) that will be assessed during physical examination of the neck and regularly re-evaluated [40, 41]. Training sessions will start with ten repetitions at 50% of 1-RM warm-ups, followed by two to three sets of 10–15 repetitions of exercise at 60–80% of 1-RM corresponding to 10-RM. Adequate breaks will be taken between sets to avoid overexertion. Warm-up exercises (bilateral shoulder circling; upper body rotation) once each for 20 s, and cool-down exercises (lateral neck stretch; neck extensor stretch; seated side stretch; self-massage of shoulder and neck with spiky ball) for three times 20 s will complete the program [20, 42].
-
Adherence to intervention: Workshop session attendance will be recorded as an indication of adherence to health promotion. Adherence to neck exercises will be recorded with the Physitrack® app (London, United Kingdom). Participants will maintain a record of exercise frequency, intensity, time, and type (F.I.T.T principles) [43]. A detailed instruction of each exercise technique (video), load intensity, and details regarding the number of sets and repetitions are recorded for each participant on the app enabled on their smartphone, tablet, or desk-top computer. Training reminder and feedback will be provided by the app.
Outcomes
Primary outcome
NP-related productivity loss (economic outcome) will be measured in percentages of the working time, using the Work Productivity and Activity Impairment Questionnaire for Specific Health Problem (WPAI-SHP, German version) and converted into monetary units using individual earnings [44,45,46].
The WPAI questionnaire is composed of five questions with a recall time frame of the past 7 days: Q1 = currently employed; Q2 = hours missed due to NP; Q3 = hours missed due to other reasons (e.g., vacation); Q4 = hours actually worked; Q5 = degree to which NP affected productivity while working (using a 0 to 10 Visual Analogue Scale) [47, 48].
NP-related impairment percentages will be calculated following the scoring rules of the developers of the WPAI (percentage absenteeism = Q2/(Q2 + Q4), percentage presenteeism = (1-Q2/(Q2 + Q4))*Q5/10)). The total NP-related work productivity loss is obtained by adding the percentage absenteeism and presenteeism (percentage NP-related work productivity loss = (Q2/(Q2 + Q4) + (1-Q2/(Q2 + Q4))*Q5/10) [47, 48]. The monetary value for the lost productivity will be calculated for each individual by multiplying the percentages by the individual gross wage [47, 48].
Secondary outcomes
Several secondary outcomes will be measured, which can be divided into the following subsections:
-
Physical and health outcomes including self-assessment of NP and headache (extent / pain drawings, occurrence, frequency, intensity, duration, Neck Disability Index, short-form headache impact test), physical examination of the neck (muscle strength, muscle endurance, mobility, local pain pressure threshold), physical activity level (International Physical Activity Questionnaire) and health related quality of life (EuroQoL Five Dimension) [49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71].
-
Psychosocial outcomes as the job-stress index, job satisfaction, and health beliefs (Fear-Avoidance Beliefs Questionnaire) [47, 72,73,74].
-
Workplace outcomes as workstation ergonomics (observation-based ergonomics assessment checklist for office-workers adapted to Swiss guidelines), workplace implementation, psychosocial workplace factors (Copenhagen Psychosocial Questionnaire), work breaks, and daily use of personal smartphone [36, 75].
-
Adherence to intervention
Additional measures
-
Participants’ global impression of change on an 11 points scale [74, 76].
-
Individual characteristics (e.g. gender, care-seeking) are collected as predictor or control variable.
Data management
Study personnel
All measurements and interventions will be delivered by qualified and experienced health care professionals. Physiotherapists, health scientist, human movement scientists, and psychologists involved in data collection and delivering the interventions will receive prior training from nationally accredited experts in order to maintain standardised methodologies. A study on interrater reliability with the actual staff was conducted at the end of 2019.
Blinding
After assignment to the intervention condition, the administrators of online-surveys will be blinded to the identity of the individuals through an encoded login of participants. The outcome assessors of the physical examination will be blinded to group allocation and previous test results of the participants. Data analysts will be blinded to the identity of the individuals.
Data collection
Physical examination of the neck will be recorded in paper-based report forms, which will be digitalized afterwards. Data entry for electronic data will be double-checked for typos and missing data. UNIPARK© (Berlin, Germany) will be used for the online questionnaire.
Data analysis
The effect of the intervention in reducing the productivity loss over the study period will be examined using linear mixed-effects models, similar to the one used in the simulation-based power calculation. Moreover, the broader category of generalized linear mixed-effects models will be used for the analyses of secondary outcomes. We will also investigate the distribution of gender and symptom characteristics (like persistence) across different groups at baseline. In case of uneven distributions, these factors will be included in the model to adjust for their potential confounding effects. If required, we will also adjust for other potential confounding effects in the analyses, such as age, occupation, adherence, psychosocial factors, health beliefs, job satisfaction, and physical activity at baseline.
All statistical analyses will be performed using Stata® (Texas, USA) or R® (Boston, USA) statistical software. Significance level was set at alpha = 0.05. Missing data will be examined to determine its randomness and addressed with multiple imputations, if required. The results of the mixed-effects modelling will be presented in outcome specific effect sizes and their 95% confidence intervals. The data will be analysed on an intention to treat and per protocol basis. Drop-outs before study commencement will be replaced by recruitment of new subjects.
Data deposition and curation
All anonymized study data will be archived at Zurich University of Applied Sciences (ZHAW) for a minimum of 10 years after study termination or premature termination of the clinical trial on restricted data pools and fire-proofed lockers, respectively with access only by study personnel.
Sample size calculation
Based on the baseline results of an Australian study, we assumed a baseline productivity of 90% and an intervention attributable increase in productivity of 5% [23]. Also, in line with the Australian study, the cluster size was set to seven subjects. In order to test the sensitivity of the sample size calculations, we used varying cluster-specific and subject-specific intraclass correlations (Rho [1] = 0.1 or 0.2 and Rho [2] = 0.2 and 0.3 respectively) as well as varying number of steps (three or four steps). The underlying statistical model that was used in the simulations was a standard closed cohort mixed effects model comprising a random effect for the clusters, a random effect for the repeated measurements on the same cohort of individuals, a fixed effect to account for time trends, and a fixed effect representing the treatment effect [77, 78]. The linear mixed effect method from the R-package lme4 was used to estimate the models [79]. Furthermore, the acceptable probability for a Type I Error to occur was set to alpha = 0.05 and the acceptable probability for a Type II Error to occur was set to beta = 0.20 (Power = 0.80). From the four assessed scenarios, the solution with 72 participants, 12 clusters and three steps are optimal in the sense that three steps put much less burden on participants than four steps, i.e., there are less measurements per subject.
An Australian study reported an attrition rate of nearly 20%. In order to prevent the risk to under-power our study, we will increase the number of clusters from 12 to 15 (> 20%) and the number of subjects per cluster from 6 to 8 (> 20%) [23]. Consequently, we aim to enrol and follow 120 participants in 15 clusters over four measurements (one baseline and three steps from the control to the intervention arm of the study) which yields a total of 420 observations.
Discussion
Summary
NP is a major burden in Swiss office-workers. To the authors’ knowledge, this study is the first that investigates the effect of a multi-component intervention combining the current evidence of workstation ergonomics, health promotion, neck exercises, and an adherence app to impact the economic and individual burden of NP and headache in this population.
Considerations and issues
Study design
As in many intervention studies, drop-outs and non-attendances are anticipated [13, 23]. Therefore, the sample size calculation is adjusted and adherence to intervention may be optimized using an app. In addition, the intervention will take place at the workplace and, depending on the organisation, almost the whole time needed for the intervention can be counted as working time. As not all participants will receive the intervention at the same time, a contamination of intervention may occur. To minimize this effect, people working on the same floor, in the same room or work group will be in the allocated to the same cluster.
Ethical approval
As every subject will eventually receive the intervention, ethical concerns of negligence should be regarded as unwarranted. The stepped wedge design helps to achieve a similar study power while requiring fewer participants, although more measurement from each [24, 32].
Safety
No risks of the intervention, except from some temporary muscle soreness due to the exercise intervention and testing have been reported in earlier studies [27, 29, 80]. Participants suffering from NP or headache may feel an immediate benefit during the study and not only during their working hours. These effects especially depend on adherence to the exercise programme, but also on the feedback to study personnel regarding any longer lasting discomfort or pain due to the interventional programme. A brief worsening of the symptoms may occur at the start of intervention period due to muscular change [38].
Monitoring and auditing
At minimum of four visits will be conducted by a monitor who is independent of the study (informed consent, data collection and case report forms, data entry, data analysis). Monitoring visits at the investigator’s site prior to the start and during the course of the study will help to follow up the progress of the clinical study, to assure utmost validity of the data and to detect possible errors at an early time point.
Dissemination plan
After the statistical analysis of this trial, the NEXpro (neck exercise productivity) team will publish data in top-ranking journals in medicine and health sciences. In particular, the following publications beyond the study protocol are planned: primary outcome (productivity analysis), studies on secondary and additional outcomes (e.g., neck pain analysis, headache analysis).
Potential implication
It is expected that the study will impact the individual, their place of work, as well as private and public policy and practice regarding healthy behaviours of office-workers. This research will address an unmet organisational need by exploring the impact of an evidence-based intervention over the course of a year.
Availability of data and materials
Not applicable.
Change history
25 July 2020
An amendment to this paper has been published and can be accessed via the original article.
Abbreviations
- AA:
-
Andrea Aegerter
- AE:
-
Achim Elfering
- BASEC:
-
Business Administration System for Ethics Committees
- BB:
-
Beatrice Brunner
- Dec:
-
December
- EuroQoL:
-
European Quality of Life (Community)
- EUTF:
-
European taskforce
- Fig.:
-
Fig
- F.I.T.T. :
-
Exercise principles (frequency, intensity, time, and type)
- GS :
-
Gisela Sjøgaard
- HL:
-
Hannu Luomajoki
- ICH-GCP:
-
International Conference on Harmonisation-Good Clinical Practice
- MD:
-
Manja Deforth
- ME:
-
Markus Ernst
- MM:
-
Markus Melloh
- NEXpro:
-
Neck exercise productivity
- NP:
-
Neck pain
- RCT:
-
Randomized-controlled trial
- SPIRIT:
-
Standard Protocol Items for Randomized Trials
- TV:
-
Thomas Volken
- VJ:
-
Venerina Johnston
- WPAI-SHP:
-
Work Productivity and Activity Impairment Questionnaire for Specific Health Problem
- ZHAW:
-
Zurich University of Applied Sciences
- 12-RM:
-
Twelve-repetition maximum
References
Hoy D, March L, Woolf A, Blyth F, Brooks P, Smith E, et al. The global burden of neck pain: estimates from the global burden of disease 2010 study. Ann Rheum Dis. 2014;73(7):1309–15.
Angst F, Angst J, Ajdacic-Gross V, Aeschlimann A, Rossler W. Epidemiology of Back pain in young and middle-aged adults: a longitudinal population cohort survey from age 27-50 years. Psychosomatics. 2017;58(6):604–13.
Amstutz S, Monn C, Vanis M, Schwehr P, Kündig S, Bossart R, et al. Schweizerische Befragung in Büros (SBiB-Studie) In: Eidgenössisches Volkswirtschaftsdepartement Staatssekretariat für Wirtschaft SECO, editor. Schweizerische Eidgenossenschaft 2010.
Hagberg M, Tornqvist EW, Toomingas A. Self-reported reduced productivity due to musculoskeletal symptoms: associations with workplace and individual factors among white-collar computer users. J Occup Rehabil. 2002;12(3):151–62.
Krieger R, Graf M, Vanis M. Sechste Europäische Erhebung über die Arbeitsbedingungen 2015 Ausgewählte Ergebnisse zu den Schweizerischen Arbeitsbedingungen der abhängig Erwerbstätigen. In: Eidgenössisches Departement für Wirschaft BuFW, editor.: Staatssekretariat für Wirtschaft SECO, Direktion für Arbeit/Arbeitsbedingungen; 2017.
Loeppke R, Taitel M, Haufle V, Parry T, Kessler RC, Jinnett K. Health and productivity as a business strategy: a multiemployer study. J Occup Environ Med. 2009;51(4):411–28.
Schultz AB, Edington DW. Employee health and presenteeism: a systematic review. J Occup Rehabil. 2007;17(3):547–79.
Aas RW, Tuntland H, Holte KA, et al. Workplace interventions for neck pain in workers. Cochrane Database Syst Rev. 2011;2011(4):CD008160. https://doi.org/10.1002/14651858.CD008160.pub2.
Van Eerd D, Munhall C, Irvin E, Rempel D, Brewer S, van der Beek AJ, et al. Effectiveness of workplace interventions in the prevention of upper extremity musculoskeletal disorders and symptoms: an update of the evidence. Occup Environ Med. 2016;73(1):62–70.
Martimo KP, Shiri R, Miranda H, Ketola R, Varonen H, Viikari-Juntura E. Effectiveness of an ergonomic intervention on the productivity of workers with upper-extremity disorders--a randomized controlled trial. Scand J Work Environ Health. 2010;36(1):25–33.
Shiri R, Martimo KP, Miranda H, Ketola R, Kaila-Kangas L, Liira H, et al. The effect of workplace intervention on pain and sickness absence caused by upper-extremity musculoskeletal disorders. Scand J Work Environ Health. 2011;37(2):120–8.
Kennedy CA, Amick BC 3rd, Dennerlein JT, Brewer S, Catli S, Williams R, et al. Systematic review of the role of occupational health and safety interventions in the prevention of upper extremity musculoskeletal symptoms, signs, disorders, injuries, claims and lost time. J Occup Rehabil. 2010;20(2):127–62.
Chen X, Coombes BK, Sjogaard G, Jun D, O'Leary S, Johnston V. Workplace-based interventions for neck pain in office workers: systematic review and meta-analysis. Phys Ther. 2018;98(1):40–62.
Mekhora K, Liston CB, Nanthavanij S, Cole JH. The effect of ergonomic intervention on discomfort in computer users with tension neck syndrome. Int J Ind Ergon. 2000;26(3):367–79.
Fostervold KI, Aarås A, Lie I. Work with visual display units: long-term health effects of high and downward line-of-sight in ordinary office environments. Int J Ind Ergon. 2006;36(4):331–43.
Hoe VCW, Urquhart DM, Kelsall HL, Sim MR. Ergonomic design and training for preventing work-related musculoskeletal disorders of the upper limb and neck in adults. Cochrane Database Syst Rev. 2012;2012(8):CD008570-CD.
Cancelliere C, Cassidy JD, Ammendolia C, Cote P. Are workplace health promotion programs effective at improving presenteeism in workers? A systematic review and best evidence synthesis of the literature. BMC Public Health. 2011;11:395.
Kuoppala J, Lamminpaa A, Husman P. Work health promotion, job well-being, and sickness absences--a systematic review and meta-analysis. J Occup Environ Med. 2008;50(11):1216–27.
Marley J, Tully MA, Porter-Armstrong A, Bunting B, O'Hanlon J, Atkins L, et al. The effectiveness of interventions aimed at increasing physical activity in adults with persistent musculoskeletal pain: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2017;18(1):482.
Shariat A, Lam ET, Kargarfard M, Tamrin SB, Danaee M. The application of a feasible exercise training program in the office setting. Work (Reading, Mass). 2017;56(3):421–8.
Gram B, Andersen C, Zebis MK, Bredahl T, Pedersen MT, Mortensen OS, et al. Effect of training supervision on effectiveness of strength training for reducing neck/shoulder pain and headache in office workers: cluster randomized controlled trial. Biomed Res Int. 2014;2014:693013.
Louw S, Makwela S, Manas L, Meyer L, Terblanche D, Brink Y. Effectiveness of exercise in office workers with neck pain: A systematic review and meta-analysis. S Afr J Physiother. 2017;73(1):392.
Pereira M, Comans T, Sjøgaard G, et al. The impact of workplace ergonomics and neck-specific exercise versus ergonomics and health promotion interventions on office worker productivity: a cluster-randomized trial. Scand J Work Environ Health. 2019;45(1):42–52. https://doi.org/10.5271/sjweh.3760.
Christensen JR, Bredahl TV, Hadrevi J, Sjogaard G, Sogaard K. Background, design and conceptual model of the cluster randomized multiple-component workplace study: FRamed intervention to decrease occupational muscle pain – “FRIDOM”. BMC Public Health. 2016;16(1):1116.
Justesen JB, Sogaard K, Dalager T, Christensen JR, Sjogaard G. The effect of intelligent physical exercise training on sickness Presenteeism and absenteeism among office workers. J Occup Environ Med. 2017;59(10):942–8.
Puig-Ribera A, Bort-Roig J, Gine-Garriga M, Gonzalez-Suarez AM, Martinez-Lemos I, Fortuno J, et al. Impact of a workplace ‘sit less, move more’ program on efficiency-related outcomes of office employees. BMC Public Health. 2017;17(1):455.
Sihawong R, Janwantanakul P, Jiamjarasrangsi W. Effects of an exercise programme on preventing neck pain among office workers: a 12-month cluster-randomised controlled trial. Occup Environ Med. 2014;71(1):63–70.
Grimani A, Aboagye E, Kwak L. The effectiveness of workplace nutrition and physical activity interventions in improving productivity, work performance and workability: a systematic review. BMC Public Health. 2019;19(1):1676.
Andersen CH, Andersen LL, Pedersen MT, Mortensen P, Karstad K, Mortensen OS, et al. Dose-response of strengthening exercise for treatment of severe neck pain in women. J Strength Cond Res. 2013;27(12):3322–8.
Pedersen MT, Andersen LL, Jorgensen MB, Sogaard K, Sjogaard G. Effect of specific resistance training on musculoskeletal pain symptoms: dose-response relationship. J Strength Cond Res. 2013;27(1):229–35.
Voth EC, Oelke ND, Jung ME. A Theory-Based Exercise App to Enhance Exercise Adherence: A Pilot Study. JMIR Mhealth Uhealth. 2016;4(2):e62-e.
Zhan Z. Evaluation and analysis of stepped wedge designs: application to colorectal cancer follow-up. Groningen: Rijksuniversiteit Groningen; 2018.
Chan AW, Tetzlaff JM, Altman DG, Dickersin K, Moher D. SPIRIT 2013: new guidance for content of clinical trial protocols. Lancet. 2013;381(9861):91–2.
Misailidou V, Malliou P, Beneka A, Karagiannidis A, Godolias G. Assessment of patients with neck pain: a review of definitions, selection criteria, and measurement tools. J Chiropr Med. 2010;9(2):49–59.
Haldeman S, Carroll L, Cassidy JD, Schubert J, Nygren A, Bone, et al. The Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders: executive summary. Spine (Phila Pa 1976). 2008;33(4 Suppl):S5–7.
Pereira MJ, Straker LM, Comans TA, Johnston V. Inter-rater reliability of an observation-based ergonomics assessment checklist for office workers. Ergonomics. 2016;59(12):1606–12.
Wanous JP, Poland TD, Premack SL, Davis KS. The effects of met expectations on newcomer attitudes and behaviors: a review and meta-analysis. J Appl Psychol. 1992;77(3):288–97.
Andersen LL, Kjaer M, Sogaard K, Hansen L, Kryger AI, Sjogaard G. Effect of two contrasting types of physical exercise on chronic neck muscle pain. Arthritis Rheum. 2008;59(1):84–91.
Jull G, Sterling M, Falla D, Treleaven J, O’Leary S. Chapter 14 - Therapeutic Exercise for Cervical Disorders: Practice Pointers. Whiplash, Headache, and Neck Pain. Edinburgh: Churchill Livingstone; 2008. p. 207–29.
Kraemer WJ, Adams K, Cafarelli E, Dudley GA, Dooly C, Feigenbaum MS, et al. American College of Sports Medicine position stand. Progression models in resistance training for healthy adults. Med Sci Sports Exerc. 2002;34(2):364–80.
Gao Y, Kristensen LA, Grøndberg TS, Murray M, Sjøgaard G, Søgaard K. Electromyographic evaluation of specific elastic band exercises targeting neck and shoulder muscle activation. Appl Sci. 2020;10(3):756.
Shariat A, Cleland JA, Danaee M, Kargarfard M, Sangelaji B, Tamrin SBM. Effects of stretching exercise training and ergonomic modifications on musculoskeletal discomforts of office workers: a randomized controlled trial. Brazilian J Phys Ther. 2018;22(2):144–53.
Alexander JC, Joshi GP. Smartphone applications for chronic pain management: a critical appraisal. J Pain Res. 2016;9:731–4.
Reilly MC, Zbrozek AS, Dukes EM. The validity and reproducibility of a work productivity and activity impairment instrument. PharmacoEconomics. 1993;4(5):353–65.
Reilly MC, Gooch KL, Wong RL, Kupper H, van der Heijde D. Validity, reliability and responsiveness of the Work Productivity and Activity Impairment Questionnaire in ankylosing spondylitis. Rheumatology (Oxford). 2010;49(4):812–9.
Lambert J, Hansen BB, Arnould B, Grataloup G, Guillemin I, Hojbjerre L, et al. Linguistic validation into 20 languages and content validity of the rheumatoid arthritis-specific work productivity and activity impairment questionnaire. Patient. 2014;7(2):171–6.
Igic I, Keller A, Luder L, Elfering A, Semmer NK, Brunner B, et al. Job-stress-index 2015. Bern: Gesundheitsförderung Schweiz; 2015.
Pereira MJ, Johnston V, Straker LM, Sjogaard G, Melloh M, O'Leary SP, et al. An investigation of self-reported health-related productivity loss in office workers and associations with individual and work-related factors using an Employer's perspective. J Occup Environ Med. 2017;59(7):e138–e44.
Barbero M, Fernandez-de-Las-Penas C, Palacios-Cena M, Cescon C, Falla D. Pain extent is associated with pain intensity but not with widespread pressure or thermal pain sensitivity in women with fibromyalgia syndrome. Clin Rheumatol. 2017;36(6):1427–1432. doi: 10.007/s10067-017-3557-1. Epub 2017 Feb 4.
Swanenburg J, Humphreys K, Langenfeld A, Brunner F, Wirth B. Validity and reliability of a German version of the neck disability index (NDI-G). Man Ther. 2014;19(1):52–8.
Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35(8):1381–95.
Stark RG, Reitmeir P, Leidl R, Konig HH. Validity, reliability, and responsiveness of the EQ-5D in inflammatory bowel disease in Germany. Inflamm Bowel Dis. 2010;16(1):42–51.
Leoni D, Falla D, Heitz C, Capra G, Clijsen R, Egloff M, et al. Test-retest reliability in reporting the pain induced by a pain provocation test: further validation of a novel approach for pain drawing acquisition and analysis. Pain Pract. 2017;17(2):176–84.
Palacios-Cena M, Barbero M, Falla D, Ghirlanda F, Arend-Nielsen L, Fernandez-de-Las-Penas C. Pain extent is associated with the emotional and physical burdens of chronic tension-type headache, but not with depression or anxiety. Pain Med. 2017;18(10):2033–9. https://doi.org/10.1093/pm/pnx047.
Müller B, Baum A, Holzhausen M, Grittner U, Hilgendorf I, Martus P, et al. Der Rostocker Kopfschmerzfragen-Komplex: Validierung einer schnellen diagnostischen Hilfe bei der Einordnung primaerer Kopfschmerzen. Fortschr Neurol Psychiatr. 2014;82(03):145–8.
Fritsche G, Hueppe M, Kukava M, Dzagnidze A, Schuerks M, Yoon M-S, et al. Validation of a German language questionnaire for screening for migraine, tension-type headache, and trigeminal autonomic Cephalgias. Headache. 2007;47(4):546–51.
Madsen BK, Sogaard K, Andersen LL, Skotte JH, Jensen RH. Neck and shoulder muscle strength in patients with tension-type headache: a case-control study. Cephalalgia. 2016;36(1):29–36.
O'Leary S, Hoogma C, Molland Oystein S, Sundberg S, Pedler A, van Wyk L. Comparative strength and endurance parameters of the craniocervical and cervicothoracic extensors and flexors in females with and without idiopathic neck pain. J Appl Biomech. 2019;35(3):209–15.
Domenech MA, Sizer PS, Dedrick GS, McGalliard MK, Brismee JM. The deep neck flexor endurance test: normative data scores in healthy adults. PM R. 2011;3(2):105–10.
Castien RF, van der Wouden JC, De Hertogh W. Pressure pain thresholds over the cranio-cervical region in headache: a systematic review and meta-analysis. J Headache Pain. 2018;19(1):9.
Yoon M-S, Obermann M, Fritsche G, Slomke M, Dommes P, Schilf C, et al. Population-based validation of a German-language self-administered headache questionnaire. Cephalalgia. 2008;28(6):605–8.
Kuorinka I, Jonsson B, Kilbom A, Vinterberg H, Biering-Sorensen F, Andersson G, et al. Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. Appl Ergon. 1987;18(3):233–7.
Sjogaard G, Sogaard K, Hermens HJ, Sandsjo L, Laubli T, Thorn S, et al. Neuromuscular assessment in elderly workers with and without work related shoulder/neck trouble: the NEW-study design and physiological findings. Eur J Appl Physiol. 2006;96(2):110–21.
Oesch P, Hilfiker R, Keller S, Kool J, Luomajoki H, Schädler S, et al. Assessments in der Rehabilitation - Band 2: Bewegungsapparat. Bern: Hans Huber Verlag; 2017.
Rutten A, Ziemainz H, Schena F, Stahl T, Stiggelbout M, Auweele YV, et al. Using different physical activity measurements in eight European countries. Results of the European physical activity surveillance system (EUPASS) time series survey. Public Health Nutr. 2003;6(4):371–6.
Ernst MJ, Crawford RJ, Schelldorfer S, Rausch-Osthoff AK, Barbero M, Kool J, et al. Extension and flexion in the upper cervical spine in neck pain patients. Man Ther. 2015;20(4):547–52.
Sahrmann S. Movement system impairment syndromes of the extremities, cervical and thoracic spines - E-book. Bern: Elsevier Health Sciences; 2010.
Satpute K, Nalband S, Hall T. The C0-C2 axial rotation test: normal values, intra- and inter-rater reliability and correlation with the flexion rotation test in normal subjects. J Man Manipulative Ther. 2019;27(2):92–8.
Luedtke K, Basener A, Bedei S, Castien R, Chaibi A, Falla D, et al. Outcome measures for assessing the effectiveness of non-pharmacological interventions in frequent episodic or chronic migraine: a Delphi study. BMJ Open. 2020;10(2):e029855.
Martin M, Blaisdell B, Kwong JW, Bjorner JB. The short-form headache impact test (HIT-6) was psychometrically equivalent in nine languages. J Clin Epidemiol. 2004;57(12):1271–8.
Luedtke K, Boissonnault W, Caspersen N, Castien R, Chaibi A, Falla D, et al. International consensus on the most useful physical examination tests used by physiotherapists for patients with headache: a Delphi study. Man Ther. 2016;23:17–24.
Wanous JP, Reichers AE, Hudy MJ. Overall job satisfaction: how good are single-item measures? J Appl Psychol. 1997;82(2):247–52.
Pfingsten M, Kroner-Herwig B, Leibing E, Kronshage U, Hildebrandt J. Validation of the German version of the Fear-Avoidance Beliefs Questionnaire (FABQ). European journal of pain (London). 2000;4(3):259–66.
Igic I, Semmer NK, Elfering A. Manual S-Tool: Online – Stressbefragungsinstrument für die Unternehmen. Bern, Lausanne: Gesundheitsförderung Schweiz; 2012.
Nubling M, Stossel U, Hasselhorn HM, Michaelis M, Hofmann F. Measuring psychological stress and strain at work - Evaluation of the COPSOQ Questionnaire in Germany. Psycho-Soc Med. 2006;3:Doc05.
Hurst H, Bolton J. Assessing the clinical significance of change scores recorded on subjective outcome measures. J Manip Physiol Ther. 2004;27(1):26–35.
Baio G, Copas A, Ambler G, Hargreaves J, Beard E, Omar RZ. Sample size calculation for a stepped wedge trial. Trials. 2015;16:354.
Barker D, McElduff P, D'Este C, Campbell MJ. Stepped wedge cluster randomised trials: a review of the statistical methodology used and available. BMC Med Res Methodol. 2016;16:69.
Bates D, Mächler M, Bolker B, Walker S. Fitting Linear Mixed-Effects Models Using lme4. J Stat Softw. 2015;67(1):1–48.
Andersen CH, Andersen LL, Zebis MK, Sjogaard G. Effect of scapular function training on chronic pain in the neck/shoulder region: a randomized controlled trial. J Occup Rehabil. 2014;24(2):316–24.
Acknowledgements
The following are members of the NEXpro collaboration group: Andrea M. Aegerter (Switzerland), Marco Barbero (Switzerland), Beatrice Brunner (Switzerland), Jon Cornwall (New Zealand), Yara Da Cruz Pereira (Switzerland), Manja Deforth (Switzerland), Oliver Distler (Switzerland), Julia Dratva (Switzerland), Holger Dressler (Switzerland), Tobias Egli (Switzerland), Achim Elfering (project co-lead, Switzerland), Markus J. Ernst (Switzerland), Irene Etzer-Hofer (Switzerland), Deborah Falla (United Kingdom), Michelle Gisler (Switzerland), Michelle Haas (Switzerland), Venerina Johnston (Australia), Sandro Klaus (Switzerland), Gina M. Kobelt (Switzerland), Hannu Luomajoki (Switzerland), Kerstin Lüdtke (Germany), Markus Melloh (project lead, Switzerland), Corinne Nicoletti (Switzerland), Seraina Niggli (Switzerland), Salome Richard (Switzerland), Nadine Sax (Switzerland), Katja Schülke (Switzerland), Gisela Sjøgaard (Denmark), Lukas P. Staub (Australia), Thomas Volken (Switzerland), and Thomas Zweig (Switzerland).
Funding
This work was financially supported by the Swiss National Science Foundation grant number 32003B_182389. The authors acknowledge Rebecca J. Crawford for her significant work on the funding application.
Author information
Authors and Affiliations
Consortia
Contributions
AA and MD wrote the study protocol. ME, HL, and BB revised the study protocol. VJ, GS, and AE designed the study and revised the study protocol. MM, JD, and TV wrote the funding application, designed the study and revised the study protocol. TV performed the sample size calculations, designed the statistical analysis and revised the study protocol. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study has been approved by the Ethical Commission of the Canton of Zurich, Switzerland (swissethics No. 2019–01678). Written informed consent will be obtained from study participants.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Aegerter, A.M., Deforth, M., Johnston, V. et al. On-site multi-component intervention to improve productivity and reduce the economic and personal burden of neck pain in Swiss office-workers (NEXpro): protocol for a cluster-randomized controlled trial. BMC Musculoskelet Disord 21, 391 (2020). https://doi.org/10.1186/s12891-020-03388-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-020-03388-x