Abstract
Background
Previously, the sagittal spinal balance in both asymptomatic and scoliotic Caucasian people has been characterized and compared. Very recently, the sagittal spino-pelvic parameters among asymptomatic Chinese adults have been studied, and the results were compared with Caucasian adults, indicating that a difference did exist. Unfortunately, the distribution of sagittal standing posture patterns among the Chinese population has not been characterized in either asymptomatic or scoliotic groups.
Methods
We conducted a radiographic comparison study to define the deviation of sagittal balance in scoliotic patients from that of an asymptomatic population. A total of 126 asymptomatic and 117 idiopathic scoliotic (IS) young adults were recruited. Radiographic data from each subject were reviewed, and sagittal spinopelvic parameters were measured. The Roussouly type was then determined, as well as the relative position of the C7 plumbline with respect to the sacrum and hip axis. Comparison analyses were undertaken between the two different groups.
Results
The IS group had a larger pelvic incidence, pelvic tilt and sacral slope, but a smaller spinal tilt than the asymptomatic group (P < 0.05), while other sagittal parameters were similar. The distribution of Roussouly types was similar between the asymptomatic and IS groups, of which 49.2% and 45.3% belonged to Roussouly Type 3, respectively. Asymptomatic males and females had a similar distribution, which was different between the two genders in the IS group (P < 0.05), with more females possessing a neutral sagittal standing posture. In addition, more IS subjects had forward displacement of the C7 plumbline than asymptomatic ones (P < 0.05), while there was no difference between the two genders in either group.
Conclusions
Although sagittal pelvic parameters were greater in the IS population, their sagittal spinal balance was maintained and there was no sagittal standing posture pattern correlated with IS. The occurrence of anterior displacement of the C7 plumbline was more common in IS patients than asymptomatic adults, but did not appear to be correlated with gender in both populations.
Similar content being viewed by others
Background
Recently, the study of sagittal spinal balance in different populations has gained importance ever since Roussouly et al. [1] proposed a four-type classification in a study of 160 normal European adults. This novel classification is mainly determined by sacral and lumbar sagittal parameters such as sacral slope (SS), lumbar lordosis (LL), the number of lumbar vertebrae in LL, inflection point and lumbar tilt (Fig. 1). However, there is a lack of literature that comprehensively analyses and compares the deviation of sagittal standing posture patterns in the scoliotic population with their normal counterparts, though previous publications have studied the difference of some sagittal spinopelvic parameters between the two populations [2, 3]. Upasani et al. [2] compared the measurements of sagittal spinopelvic parameters between scoliotic and asymptomatic adolescent subjects and found that scoliotic patients had greater pelvic incidence (PI) and pelvic tilt (PT) values than the asymptomatic population. They also found that patients with primary thoracic scoliosis had a lower thoracic kyphosis (TK) and a larger SS than the controls, whereas patients with a primary thoracolumbar scoliosis had relatively normal TK, LL and SS values. Qiu et al. [3] compared the values of sagittal spinopelvic parameters between adolescent girls with idiopathic thoracic scoliosis and asymptomatic girls and found that TK in the former group was lower, which supported the findings of Upasani et al. [2]. Other radiographic studies in this field also reported similar results [4, 5]. However, there is no published comparative study that specifically explored the difference of the whole sagittal spinal alignments and the distribution of standing posture patterns in scoliotic patients from the norm.
Representative drawings of Roussouly types. Type 1 Sacral slope (SS) < 35°, apex of lumbar lordosis (LL) at middle L5, the spine is hypolordotic and relatively normokyphotic; Type 2 SS < 35°, apex of LL at base L4, the spine is hypolordotic and hypokyphotic; Type 3 35° < SS < 45°, apex of LL at middle L4, the spine is well balanced; Type 4 SS > 45°, apex of LL at base L3, the spine is hyperlordotic and hyperkyphotic
Hu et al. [6] reported that 42.4% of scoliotic adolescents belonged to Roussouly Type 3. This proportion is considerably high when compared with that of the general population reported by previous publications [1, 7,8,9]. Thus, a question was raised regarding how the sagittal standing posture patterns of the scoliotic population deviated from the norm. Aiming to illuminate the above question, this study was designed to describe and compare the whole sagittal spinal balance and the distribution of their patterns in asymptomatic and scoliotic young adults.
Methods
Materials
Young adults with idiopathic scoliosis (IS) who visited our hospital from Jun 2006 to Dec 2013 were consecutively reviewed and screened, regardless of whether they underwent correction surgery or not. The inclusion criteria were as follows: (1) aged 18 to 34 years old; (2) diagnosed with IS with no other pathological conditions; (3) having structural curve(s) with Cobb angle(s) of 25 degrees or more on side-bending films; (4) having an entire set of films (namely, full-length posteroanterior, side-bending and lateral X-rays) taken at our hospital; (5) no previous medical intervention on spine, pelvis or low extremities. An age-matched enrolment of normal counterparts was taken among medical students, young doctors, nurses and other employees in our hospital. Their medical histories were examined, and individuals were excluded if they had (1) previous trauma or medical intervention on the spine, pelvis or low extremities; (2) any symptom suggestive of spinal or other orthopaedic diseases; (3) any radiographic anomaly during the process of imaging review, such as scoliosis, spondylolisthesis, spondylolysis, severely wedged vertebrae beyond the normal range of variation and leg discrepancy. This study was permitted by the Institutional Review Board, and informed consent was obtained from all individual participants included in the study.
Methods
Imaging protocols and parameters to measure
All X-rays included in the study were taken before brace and surgical intervention. To facilitate the comparison, an identical radiographic protocol, which was consistently adopted in our hospital, was applied to both groups. No side-bending films were used for normal subjects. Full-length posteroanterior (PA), side-bending (only for IS subjects) and lateral X-rays of the spine-pelvis complex were taken. When taking lateral films, subjects stood in an erect and comfortable position, with arms flexed 45 to 60 degrees and hands placed on adjustable supports with horizontal gaze. Exposures were taken from the base of the skull to the proximal femora. The distance from the radiographic source to the films was maintained at 180 cm, and the edges of the films were squared with respect to the horizontal and vertical axes separately. The films were digitized with a commercially available optical scanner (XR 650, GE, USA). All morphologic data were archived via Picture Archiving and Communication Systems (PACS, GE, USA). Then, the data were retrieved and measured through PACS in diagonal 20-in. screens with a resolution of 75 dpi.
First, bending films of IS subjects were retrieved for the confirmation of previous diagnoses, according to Lenke’s definition [10]. Sagittal parameters to be measured included thoracic kyphosis (TK), the angle subtended by the T1 superior endplate and T12 inferior endplate; lumbar lordosis (LL), the angle subtended by the L1 and S1 superior endplates; pelvic incidence (PI), the angle subtended by the line connecting the hip axis (HA, the midpoint of the line connecting bicoxofemoral centres) to the midpoint of the upper sacral endplate and the line perpendicular to the upper sacral endplate; pelvic tilt (PT), the angle subtended by the vertical line and the line connecting the HA to the midpoint of the upper sacral endplate (Fig. 2); sacral slope (SS), the angle subtended by the horizontal line and upper sacral endplate, and spinosacral angle (SSA), the angle subtended by the upper sacral endplate and the line from the centre of the C7 vertebral body to the midpoint of the upper sacral endplate. Moreover, spinal tilt (ST), the angle subtended by the line connecting the horizontal line and the centre of the C7 vertebral body to the midpoint of the upper sacral endplate, was calculated by the following formula: ST = SSA - SS (Fig. 2). On PA films, any significant curve was re-measured for IS subjects, while for normal subjects, any curve more than 10° was marked for exclusion. All values were measured two times by a reviewer, and the average results were obtained.
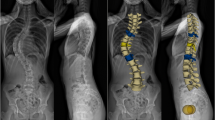
All subjects were categorized by Roussouly classification [1] according to their PI, SS, PT, thoracic and lumbar alignments (Fig. 1). In addition, the relative position of the C7 plumbline with respect to the HA and the midpoint of the sacral upper endplate was determined and divided into two subgroups [4], classified as either C7-anterior subgroup if the C7 plumbline was ahead of both the midpoint of the upper sacral endplate and the HA, or C7-posterior subgroup (Fig. 3).
Statistical analysis
Statistical analyses were conducted using IBM SPSS Statistics for Windows Version 20 (IBM Corp., Armonk, New York, USA). The precision of measurement was determined using a technical error of measurement (TEM), and the coefficient of reliability (R) was calculated [11]. Descriptive statistics were provided as the mean ± standard deviation (SD) and 95% confidence interval (95%CI). Two-tailed unpaired Student’s t-test and two-tailed Pearson’s χ2 test (or Fisher’s exact test if indicated) were utilized to compare between different groups. Statistical significance was set at 0.05.
Results
In all, 126 asymptomatic and 117 IS subjects were recruited, with an average age of 26.4 ± 3.7 and 26.3 ± 4.7 years, respectively (Table 1). The Cobb angles of coronal curves for IS adults are presented in Table 2. All sagittal parameters were normally distributed, and the reliability (R values) for all parameters was above 96%, ranging from 96.88% to 99.98%. The PI for the normal and IS groups was 41.2° ± 7.1° and 45.5° ± 10.0°, respectively. The IS group had larger PI, PT and SS but a smaller ST than the asymptomatic group (P < 0.05), while other sagittal parameters were similar (P > 0.05, Table 1). Though ST was significantly different between the two genders in the normal group (P < 0.05), other parameters were similar between males and females in either group (P > 0.05, Fig. 4).
Normal and IS groups had a comparable distribution of Roussouly classification (P > 0.05), and Type 3 was the largest for both groups, found in 49.2% and 45.3% cases, respectively (Table 1). Though the distribution of Roussouly types was similar between the two normal genders, it was different between IS males and females (P < 0.05), with more females possessing a well-balanced sagittal standing posture, namely, Type 3 (Table 3).
In all, 24.8% of IS adults belonged to the C7-anterior subgroup compared to 4.8% of normal adults (P < 0.05, Table 1). Males and females in both groups had a similar proportion of C7-anterior subgroup (P > 0.05, Table 3).
Discussion
Roussouly classification has become a valuable approach for characterizing sagittal standing posture patterns. This classification system can outline four distinct types of sagittal profiles, and each type dominates in an age range, predisposes to different spinal pathologies and even indicates for a certain surgical strategy [1, 8,9,10, 12, 13]. Thus, it is beneficial for spinal surgeons to be aware of the difference of sagittal spinal balance between normal and IS populations. Since the values of sagittal parameters are affected by many factors, recruiting strategies must be meticulously planned to maximally maintain consistency of these factors, such as age and the stance during filming. The two groups in this study had similar age modalities (Table 1). Moreover, this study seemed immune to imaging-relevant influence, since the aforementioned radiographic protocol has been consistently conducted in our hospital.
This study found that the values of some sagittal parameters in IS patients deviated from the norm (Table 1). Three pelvic parameters, PI, PT and SS, significantly increased in IS patients. PI is an important pelvic parameter that can represent the potential of pelvic compensation for the spinal malalignment caused by some spinal pathologies [5, 12, 14,15,16]. Therefore, the increased PI and PT suggested a larger retroversion of the pelvis and thus demonstrated the existence of pelvic compensation. The pelvic compensation could influence the spinal alignment, considering the excellent linear correlation between PI and LL in the normal population, which was simply formulated by the eq. LL ≈ PI + 9° (±9°) [17,18,19]. This biomechanical compensation was basically effective, which was proven by the maintenance of the distribution of Roussouly types in the IS population compared with that of the norm (Table 1).
There are few previous articles exploring the sagittal standing postures in a scoliotic population. Yu et al. [20] reported that 42.5% of the Caucasian IS population belonged to Roussouly Type 3, but his study recruited both adolescents and young adults. Therefore, the result might deviate from either the exact proportion found in adolescent IS or adult IS, considering that some sagittal parameters, including PI, PT and LL, increase with age in the growing child [21, 22]. Hu et al. [6] reported that the proportion of Roussouly Type 3 in scoliotic adolescents was 42.4%, which is lower compared to the proportion of 45.3% in scoliotic adults found in the present study (Table 1). We speculate that this difference is age-associated. As a child ages, his/her pelvis gains pelvic retroversion, which can provide a higher compensatory capacity and prevents forward displacement of the gravity axis in the case of a spinal deformity such as scoliosis. Therefore, the proportion of the well-balanced sagittal standing posture, namely, Roussouly Type 3, is maintained.
This study showed IS adults had a higher SS than normal adults (Table 1). According to Roussouly’s reports [1], higher SS in IS adults should be accompanied with higher proportions of Roussouly Type 3 and Type 4 (Fig. 1). However, this study displayed a similar distribution of Roussouly types between IS and normal populations (Table 1). We speculated that this similarity was related to less coherence of lumbar alignment, another important determinant of Roussouly classification, to the increased PI and SS in the IS population [5, 15]. Another underlying reason in addition to PI-based regulation might be the complex inter-dependence of spinal three-dimensional malalignments in IS, which was presumably associated with the joint effects of “anterior overgrowth”, vertebral rotation and spinal buckling [2, 23, 24]. Therefore, the transition of the whole spine-pelvis complex in IS is more complex than that of the normal population. In other words, higher SS is not always accompanied with higher proportions of Roussouly Type 3 and Type 4 in the IS population but is comparable or has slightly lower proportions, as shown by the findings of this study (Table 1) given the joint effects of the aforementioned factors. However, the above conclusion is not definitive and needs further study for verification.
Asymptomatic males and females demonstrated a similar distribution of Roussouly types, whereas a significant difference existed between IS males and females (Table 3). In all, 55.1% of female IS subjects belonged to Type 3, which was higher than that of IS males. IS females were prone to standing neutrally, which was somehow unexpected since female IS patients tend to have an unfavourable prognosis [5]. Whether this divergence indicated any clinical advantage for IS females could not be arbitrarily asserted, especially in the absence of longitudinal follow-ups. This study also found that normal females had increased absolute values for all parameters except TK compared with normal males, although without statistical significance, corresponding to the previous studies in normal populations [4, 21, 22]. This means that normal females tended to possess prominent lordosis and/or kyphosis, which are usually seen in Roussouly Type 3 and Type 4. This might explain the finding of higher proportions of Type 3 and Type 4 in normal females than in males, which were 68.2% versus 58.4%, respectively (Table 3). However, this was not the case for IS males and females, in whom the total proportions of Type 3 and Type 4 were quite close (64.4% versus 62.3%), although IS females were predominantly Roussouly Type 3 (Table 3). This phenomenon might be related to the aforementioned ill-matched transition of spine-pelvis complex in IS adults. Correspondingly, we found that the divergence of sagittal parameters was more trivial between the two IS genders (Fig. 4), but this finding was not unique [6,7,8]. Therefore, the sagittal balance in the IS population was more complex and affected by the two related factors, namely, the inherent malalignment of this entity and the regulation of the PI-based system.
Mac-Thiong et al. [4] stated that the relative position of C7 plumbline with respect to the sacrum and HA was an important indicator for categorizing the global sagittal balance (Fig. 3). Generally, the forward displacement of the C7 plumbline was associated with a higher risk of developing spinal pathology [4, 9, 21]. This study found that 24.8% of the IS population stood with forward displacement of the C7 plumbline, which was significantly higher compared to 4.8% in asymptomatic adults (Table 1). In other words, the anterior shifting of the whole spine was more common in the IS population. This conclusion was reinforced by the finding of a lower ST in the IS population (Table 1). In addition, the finding that the proportion of the C7-anterior subgroup was similar between males and females in both groups implied that the occurrence of the forward displacement of the C7 plumbline might not be correlated with gender.
Conclusions
In summary, this study was primarily dedicated to defining the deviation of sagittal standing postures in an IS population from the norm and found that there was no apparent correlation between specific Roussouly types and IS. However, there were some limitations. First, the source of the controls was restricted and was not from general society (see “Materials”), and these subjects had higher homogeneity in habits, lifestyle, etc., which might compromise the reliability of this study. Second, coronal deformities may affect the sagittal spinal profile, as previously reported by Hu et al. [6]. Thus, correction surgery has to restore both coronal and sagittal alignments. For example, low TK values occur in IS patients with thoracic curves, and so an effective correction of coronal curves should be accompanied with good restoration of TK. Secondary adaptation and adjustment of LL as well as pelvic sagittal parameters are then performed, and the overall sagittal balance is regained. The present study, however, mainly focused on the research of the deviation of the whole sagittal spinal balance in IS patients from the norm and did not include research and discussion regarding the effect of coronal deformity on the sagittal spinal profile.
Abbreviations
- CI:
-
Confidence interval
- HA:
-
Hip axis
- IS:
-
Idiopathic scoliosis
- LL:
-
Lumbar lordosis
- PA:
-
Posteroanterior
- PI:
-
Pelvic incidence
- PT:
-
Pelvic tilt
- SD:
-
Standard deviation
- SS:
-
Sacral slope
- SSA:
-
Spinosacral angle
- ST:
-
Spinal tilt
- TEM:
-
Technical error of measurement
- TK:
-
Thoracic kyphosis
References
Roussouly P, Gollogly S, Berthonnaud E, et al. Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine (Phila Pa 1976). 2005;30(3):346–53.
Upasani VV, Tis J, Bastrom T, et al. Analysis of sagittal alignment in thoracic and thoracolumbar curves in adolescent idiopathic scoliosis: how do these two curve types differ? Spine (Phila Pa 1976). 2007;32(12):1355–9.
Qiu Y, Liu Z, Zhu Z, et al. Comparison of sagittal spinopelvic alignment in Chinese adolescents with and without idiopathic thoracic scoliosis. Spine (Phila Pa 1976). 2012;37(12):E714–20.
Mac-Thiong JM, Roussouly P, Berthonnaud E, et al. Saggital parameters of global spinal balance: normative values from a prospective cohort of seven hundred nine Caucasian asymptomatic adults. Spine (Phila Pa 1976). 2010;35(22):E1193–8.
Mac-Thiong JM, Labelle H, Charlebois M, et al. Sagittal plane analysis of the spine and pelvis in adolescent idiopathic scoliosis according to the coronal curve type. Spine (Phila Pa 1976). 2003;28(13):1404–9.
Hu P, Yu M, Liu X. Analysis of the relationship between coronal and sagittal deformities in adolescent idiopathic scoliosis. Eur Spine J. 2016;25(2):409–16. https://doi.org/10.1007/s00586-015-3986-y.
Araujo F, Lucas R, Alegrete N, et al. Individual and contextual characteristics as determinants of sagittal standing posture: a population-based study of adults. Spine J. 2014;14(10):2373–83.
Chaleat-Valayer E, Mac-Thiong JM, Paquet J, et al. Sagittal spino-pelvic alignment in chronic low back pain. Eur Spine J. 2011;20(Suppl 5):S634–40.
Araujo F, Lucas R, Alegrete N, et al. Sagittal standing posture, back pain, and quality of life among adults from the general population. Spine (Phila Pa 1976). 2014;39(13):E782–94.
Lenke LG, Betz RR, Harms J, et al. Adolescent idiopathic scoliosis: a new classification to determine extent of spinal arthrodesis. J Bone Joint Surg Am. 2001;83(8):1169–81.
Ulijaszek SJ, Lourie JA. Intra- and inter-observer error in anthropometric measurement. In: Ulijaszek SJ, Mascie-Taylor GC, editors. Anthropometry: the individual and the population. Cambridge: Cambridge University Press; 1994. p. 30–55.
Roussouly P, Pinheiro-Franco JL. Biomechanical analysis of the spino-pelvic organization and adaptation in pathology. Eur Spine J. 2011;20(Suppl 5):609–18.
Roussouly P, Nnadi C. Sagittal plane deformity: an overview of interpretation and management. Eur Spine J. 2010;19(11):1824–36.
Lafage V, Schwab F, Patel A, et al. Pelvic tilt and truncal inclination: two key radiographic parameters in the setting of adults with spinal deformity. Spine (Phila Pa 1976). 2009;34(17):E599–606.
Legaye J, Beaupere G, Hecquet J, et al. Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J. 1998;7(2):99–103.
Vaz G, Roussouly P, Berthonnaud E, et al. Sagittal morphology and equilibrium of pelvis and spine. Eur Spine J. 2002;11(1):80–7.
Vrtovec T, Janssen MM, Likar B, et al. A review of methods for evaluating the quantitative parameters of sagittal pelvic alignment. Spine J. 2012;12(5):433–46.
Schwab F, Lafage V, Patel A, et al. Sagittal plane considerations and the pelvis in the adult patient. Spine (Phila Pa 1976). 2009;34(17):1828–33.
Le Huec JC, Faundez A, Dominguez D, et al. Evidence showing the relationship between sagittal balance and clinical outcomes in surgical treatment of degenerative spinal diseases: a literature review. Int Orthop. 2015;39(1):87–95. https://doi.org/10.1007/s00264-014-2516-6.
Yu M, Silvestre C, Mouton T, et al. Analysis of the cervical spine sagittal alignment in young idiopathic scoliosis: a morphological classification of 120 cases. Eur Spine J. 2013;22(11):2372–81.
Mac-Thiong JM, Berthonnaud E, Dimar JR, et al. Sagittal alignment of the spine and pelvis during growth. Spine (Phila Pa 1976). 2004;29(15):1642–7.
Mac-Thiong JM, Labelle H, Berthonnaud E, et al. Sagittal spinopelvic balance in normal children and adolescents. Eur Spine J. 2007;16(2):227–34.
Burwell RG, Cole AA, Cook TA, et al. Pathogenesis of idiopathic scoliosis. The Nottingham concept. Acta Orthop Belg. 1992;58(Suppl 1):33–58.
Siu King Cheung C, Tak Keung Lee W, Kit Tse Y, et al. Abnormal perpubertal anthropometric measurements and growth pattern in adolescent idiopathic scoliosis: a study of 598 patients. Spine (Phila Pa 1976). 2003;28(18):2152–7.
Acknowledgements
We thank and acknowledge the support from the National Natural Science Foundation of China (grant number: 81541122) in the process of manuscript preparation and language improvement.
Funding
This study received no financial funding.
Availability of data and materials
The datasets used in the present study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
PH and MY reviewed the radiological films, performed measurements, analysed and interpreted the harvested data, and wrote and revised the manuscript. They contributed equally to the article and share the first authorship. XL, ZC and ZL analysed and interpreted the harvest data. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The present study was approved by the Institutional Research Board (IRB) of Peking University Third Hospital (registration number: IRB00006761–2012033), and informed consent for participation and publication was obtained from the participants.
Consent for publication
Not Applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Hu, Pp., Yu, M., Liu, Xg. et al. How does the sagittal spinal balance of the scoliotic population deviate from the asymptomatic population?. BMC Musculoskelet Disord 19, 36 (2018). https://doi.org/10.1186/s12891-018-1954-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-018-1954-5