Abstract
Background
To describe the experience of combination therapy with extracorporeal membrane oxygenation(ECMO), high-frequency oscillatory ventilation(HFOV) and prone positioning in treating severe respiratory failure caused by community acquired methicillin resistant Staphylococcus aureus(CA-MRSA).
Case presentation
A 30-year-old female presented with fever and dyspnea for 3 days. She was diagnosed CA-MRSA pneumonia complicated by severe respiratory failure, pneumothorax and neutropenia. Venovenous ECMO was applied within 8 h of the pneumothorax diagnosis. For amelioration of ventilator-induced lung injury, HFOV and prone positioning were combined with ECMO. The patient’s condition improved considerably. ECMO was weaned on day 19, and she was discharged on day 48 with good lung recovery.
Conclusions
To the best of our knowledge, this was the first case in which ECMO was combined with HFOV and prone positioning to treat severe necrotic CA-MRSA pneumonia complicated with pneumothorax. This combination therapy may provide safe respiratory support, may minimize the risk of barotrauma, and provide better drainage of secretions in patients with necrotizing pneumonia.
Similar content being viewed by others
Background
Pneumonia caused by Staphylococcus aureus (SA) is usually characterized by lobar consolidation and pneumatoceles, with rapid progression to severe respiratory failure. Barotrauma may lead to pneumothoraces despite a lung-protective ventilation strategy, thus causing more severe hypoxemic respiratory failure and a greater challenge for conventional mechanical ventilation [1]. Community-acquired methicillin-resistant S. aureus (CA-MRSA) pneumonia, a community-acquired infection that predominantly affects young people, has a mortality rate > 70% despite aggressive conventional management [2]. Panton-Valentine leukocidin (PVL) is a pore-forming toxin secreted by strains epidemiologically-associated with CA-MRSA and lethal necrotizing pneumonia [3].
Due to the high mortality and frequency of pneumothoraces, in the necrotic lungs of patients with CA-MRSA pneumonia, non-conventional respiratory support strategies, such as extracorporeal membrane oxygenation (ECMO), high-frequency oscillatory ventilation (HFOV), prone positioning, and extracorporeal carbon dioxide removal (ECCO2R), have been used [1, 2]. When patients are supported with ECMO and safe oxygenation is reached, HFOV may help re-open the collapsed lung and prone positioning may provide good drainage of necrotic secretions in the lung, which together may lead to rapid recovery and prevent or help heal the pneumothoraces. Although each strategy has been reported independently in previous studies [1, 2], there is very little information in the literature regarding the management of patients with PVL-producing CA-MRSA pneumonia and combination support with ECMO,HFOV, and the prone positioning.
Case presentation
A 30-year-old female with no medical history was admitted to a local hospital with fever, cough, and dyspnea for 3 days. She was neutropenic with a white cell count of 1.2 × 109/L and the C-reactive protein was 124 mg/L on admission to the outside hospital (from now on considered as day 1 for the case timeline). A Gram stain of sputum revealed MRSA on day 4. Antibiotic therapy included meropenem, moxifloxacin, and teicoplanin.Rapid clinical deterioration prompted intubation and mechanical ventilation (day 2). After 3 days of conventional management with ventilation at a peak inspiratory pressure (PIP) of 30 cm H2O, positive end expiratory pressure (PEEP) of 18 cm H2O, and a FiO2 of 1.0, she developed a right lung pneumothorax and the oxygenation could not be maintained despite a right-sided intercostal chest drain (day 5; Fig. 1). The arterial blood gas was as follows: pH 7.36, PaO2 57 mmHg, PaCO2 39 mmHg. She was referred to our hospital, the Beijing Chao-Yang Hospital Respiratory Intensive Care Unit (RICU), for ECMO support on day 5. Venovenous ECMO (VV-ECMO) was established through the right internal jugular and right femoral vein at the bedside of the local hospital, and she was transferred to the RICU with an ambulance across a distance of 290 km.
Upon arrival at our RICU (day 5), ventilation was at a very low pressure and low FiO2 lung protective settings (PIP 10 cmH2O, PEEP 0 cmH2O, and FiO2 0.4). The diagnosis of PVL-expressing CA-MRSA pneumonia after influenza was confirmed by culture and influenza A nucleic acid PCR during support with ECMO. PVL genes was detected with polymerase chain reaction method, as described in previous reports by Lina et al. [4]. The procalcitonin level was 44 ng/mL; MRSA was also cultured from the right thorax drainage fluid, and empyema was diagnosed. The antibiotic regimen was changed to imipenem/cilastatin, vancomycin (1.0 g every 8 h). Because aspergillosis was reported in influenza patients in recent study [5], and positive galocomannan was detected in her serum and bronchoalveolar fluid samples, voriconazole was used at her admission to our RICU. The serum trough vancomycin levels were monitored two days after its initial dose was given. The trough vancomycin levels range from 4.8 to 8.9 mg/L for 5 days (from day 7 to day 12); vancomycin was thus changed to linezolid on day 13. As Acinetobacter baumannii was cultured from her sputum on day 16, tigecycline and cefoperazone/sulbactam was started to used on days 17 and 30, respectively.
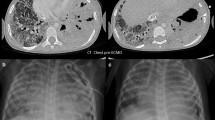
Chest computed tomography showed bilateral necrotic pneumonia with massive consolidation, especially in the right lung (day 7; Fig. 2). Because of a persistent air leak from the right lung, ventilation was converted to HFOV at a mean airway pressure of 15 cmH2O and amplitude of 50 cmH2O (day 7). HFOV was used for 23 h per day, and the patient was changed to PCV (PIP of 10 cmH2O, PEEP of 0 cmH2O) for less than an hour to evaluate her respiratory mechanics, such as tidal volume. Bedside bronchoscopy was performed daily and demonstrated a large amount of necrotic secretions from the left and right main bronchus. The tidal volume was evaluated daily on conventional mechanical ventilation, and showed <100 ml. The patient was deeply sedated, thus a spontaneous cough for sputum was unavailable. Bronchoscopic suction did not fully clear the accumulated necrotic secretion in the bilateral lower lobes. For better drainage of the secretions from the lower lobe of the consolidated lung, the patient was placed in the prone position with ECMO and HFOV(day 6); 8 h daily for 12 days. The prone positioning was arranged by a trained respiratory therapist team with nurses (Fig. 3). The air leak was closed and the tidal volume subsequently improved to 200 ml. The consolidated lung was re-opened by HFOV and the prone position, as evidenced by a chest X-ray 2 days after combination therapy was initiated (day 9; Fig. 4). No adverse and unanticipated events was observed.
ECMO was weaned on day 19 and mechanical ventilation was weaned on day 25. She was discharged home on day 48. CT scans on days 16, 27, 41, and she was followed up after 1 year of discharge showed a rapid repair of the necrotic lung (Fig. 2). A time line of the events, antibiotics, and ventilation modes is illustrated in Fig. 5.
a. Day 1, admission in the local hospital. b. The patient was intubated and ventilated with PCV on day 2. c. The sputum culture yielded MRSA on day 4. d. Complicating with right pneumothorax, the patient accepted VV-ECMO to maintain oxygenation and transferred to our RICU for further support. HFOV, prone position and PSV with protective strategy were used for promoting lung recovery and removal of secretion. e. On day 13, insufficient vancomycin drug concentration urge the change to linezolid. The chest tube was also pulled out on this day. f. Nosocomial Acinetobacter baumannii infection was detected, tigecycline was used for strengthening the antibiotic therapy on day 17. g. VV-ECMO was weaned on day 19. h. The patient was extubated on day 25. i. Cefoperazone/sulbactam was used for extensive drug resistant Acinetobacter baumannii infection on day 30. j. Candida albicans infection was detected, itraconazole was added. k. The patient was discharged home on day 48. Vancomycin and imipenem: Day 6–12; voriconazole: Day 6–20; linezolid: day 13–48; tigecycline: day 17–39; cefoperazone:day 30–42; itraconazole: day 43–48. Abbreviations: MRSA, methicillin resistant Staphylococcus aureus; ECMO, extracorporeal membrane oxygenation; HFNC, high flow nasal catheter; HFOV, high frequency oscillatory ventilation; PSV, pressure support ventilation; PCV, pressure control ventilation
Review of cases from the literature
As shown in Table 1, five previously published case series and the current case with PVL-producing CA-MRSA pneumonia supported with ECMO were reviewed. A total of 20 cases were reported, including 4 adults and 16 children or adolescent patients. Pneumothoraces occured in 60% of the patients with severe CA-MRSA pneumonia. ECMO was established in 70% of patients with most severe ARDS. HFOV was combined with ECMO in 3 cases. A lateral position was reported in one case for better drainage, but prone positioning was not reported in combination with ECMO before the current case. The survival rate of the whole case series was 70%, and 64% in patients supported with ECMO.
Discussion
PVL-producing CA-MRSA has now been established as a pathogen responsible for a rapidly progressive, frequently fatal disease manifested as necrotizing pneumonia. CA-MRSA pneumonia requires early suspicion, especially in young otherwise healthy individuals with rapidly evolving clinical features, including cavitary consolidation, bilateral infiltrates, pleural effusion, and hemoptysis [6]. Although primary infection can occur in young, healthy, immunocompetent patients, there is increasing evidence to suggest that PVL-MRSA pneumonia may occur secondarily after influenza infection, thus raising concern about possible outbreaks of PVL-MRSA pneumonia during influenza epidemics [7]. Additionally, a number of patients with severe CA-MRSA pneumonia complicated pneumothoraces, can be attributed to barotrauma with a high level of ventilator pressure settings and the underlying pathology of lung necrosis. When single or bilateral pneumothoraces occur, lung function dramatically deteriorates, thus causing refractory hypoxemia and hypercapnia [1]. Indeed, a mortality rate > 70% has been reported after conventional intensive care even though most of the patients were previously healthy, young individuals [6]. As the cases we reviewed, pneumothoraces occurred in 60% of the patients with severe CA-MRSA pneumonia.
VV-ECMO is increasingly recognized as a valuable respiratory support modality in patients with severe ARDS caused by MRSA [8], especially those patients complicated by barotrauma and in need of ultra-protective ventilation to treat the air leak. VV-ECMO support with conventional ventilation, however, has some limitations in the treatment of necrotic pneumonia. First, low pressure, low tidal volume ventilation cannot help the relatively normal lung region re-open. Second, a persistent supine position hinders the drainage of necrotic secretions which have accumulated in the lower lobe. These two factors may lead to prolonged recovery or even a negative outcome. In some centers where ECMO is unavailable, HFOV and prone positioning have been combined for patients with refractory hypoxemia ARDS [9].
In recent years, based on the sufficient oxygenation provided by ECMO, the combination of prone positioning has become feasible in patients with severe ARDS. Guervilly reported that, patients with severe hypoxemia (PaO2 to FiO2 ratio < 70) despite maximal oxygenation, injurious ventilation parameters with a plateau pressure > 32 cmH2O or a failed attempt to wean ECMO after at least 10 days on ECMO support were considered for prone positioning combined with ECMO [10]. Despite repeated bronchoscopic suctioning, effective drainage of necrotic secretions was not possible in our deeply sedated patient on ECMO. Therefore, we propose the prone position by recruiting the dorsal regions of the consolidated lungs and draining the dorsal regions with necrotic secretion accumulation, which could thus exert beneficial effects during ECMO therapy [11]. In our review of literature, 100% of adult patients were treated with ECMO, and only 62.5% of pediatric patients were on ECMO.
Currently, HFOV may still be considered as a rescue therapy option in patients with refractory hypoxemia after the use of ventilation in the prone position, recognizing that prone patients may be oscillated [12]. The combination of HFOV may be useful in patients with persistent severe hypoxemia despite VV-ECMO full support, especially in the 2.4% - 21% of patients with pneumothoraces [1, 2, 13]. Four of 5 reported patients with CA-MRSA pneumonia were supported by ECMO complicated with pneumothoraces, 3 patients had an operative intervention, and 2 patients were changed to HFOV from conventional ventilation [1, 2]. Successful use of HFOV to overcome a persistent air leak with underlying lung collapse and associated refractory hypoxemia eliminating the need for operative intervention has been reported [14,15,16]. The major problems associated with a persistent air leak in a ventilated patient are persistent lung collapse, ineffective delivery of tidal volume and inability to apply PEEP. The goal of controlling the air leak, reducing the flow from the fistula, and permitting the air leak to heal is not achieved despite the best possible conventional ventilator strategy, thus leading to a refractory air leak and an operative intervention. HFOV generates a high continuous distending pressure, which is reduced from the ventilator to the distal trachea. HFOV prevents the repeated opening–closing phenomenon of alveoli and may recruit collapse of unstable alveolar units more efficiently than conventional ventilation. This mechanism might have played a role, at least in part, in the successful management of our patient [14]. Moreover, HFOV should be viewed only as a rescue maneuver and not as a mainstay in ARDS management. Two recent RCTs on HFOV have shown either neutral or negative results.
Our case has limitations. First, from the first 24–48 h of presentation to the outside hospital, the patient should have been prone and on neuromuscular blocking agents (2 established interventions for severe ARDS). Because the patient was rescued in the local hospital, she was probably not managed ideally from the beginning. Second, the patient did not receive toxin-inhibiting drugs such as clindamycin at the early stage in the local hospital. This two points should be noted, which may lead to her deterioration and pneumothorax. Moreover, in young patients even severe MRSA pneumonias with associated pneumothoraces can recover without ECMO or HFOV was reported [17].
Conclusions
To the best of our knowledge, this was the first case in which ECMO was combined with HFOV and prone positioning to treat severe necrotic CA-MRSA pneumonia complicated with pneumothorax. This combination therapy may provide safe respiratory support, may minimize the risk of barotrauma, and provide better drainage of secretions in patients with necrotizing pneumonia.
Abbreviations
- ARDS:
-
Acute respiratory distress syndrome
- CA-MRSA:
-
Community acquired methicillin resistant Staphylococcus aureus
- ECMO:
-
Extracorporeal membrane oxygenation
- HFOV:
-
High frequency oscillatory ventilation
- PEEP:
-
Positive end expiratory pressure
- PIP:
-
Peak inspiratory pressure
- PVL:
-
Panton-Valentine leukocidin
- RICU:
-
Respiratory intensive care unit
References
Stroud MH, Okhuysen-Cawley R, Jaquiss R, Berlinski A, Fiser RT. Successful use of extracorporeal membrane oxygenation in severe necrotizing pneumonia caused by Staphylococcus Aureus. Pediatr Crit Care Med. 2007;8(3):282–7.
Noah MA, Dawrant M, Faulkner GM, Hill AM, Harvey C, Hussain A, Jenkins DR, Nichani S, Peek GJ, Sosnowski AW, et al. Panton-valentine leukocidin expressing Staphylococcus Aureus pneumonia managed with extracorporeal membrane oxygenation: experience and outcome. Crit Care Med. 2010;38(11):2250–3.
Labandeira-Rey M, Couzon F, Boisset S, Brown EL, Bes M, Benito Y, Barbu EM, Vazquez V, Hook M, Etienne J, et al. Staphylococcus aureus Panton-Valentine leukocidin causes necrotizing pneumonia. Science. 2007;315(5815):1130–3.
Lina G, Piemont Y, Godail-Gamot F, Bes M, Peter MO, Gauduchon V, Vandenesch F, Etienne J. Involvement of Panton-valentine leukocidin-producing Staphylococcus Aureus in primary skin infections and pneumonia. Clin Infect Dis. 1999;29(5):1128–32.
Wauters J, Baar I, Meersseman P, Meersseman W, Dams K, De Paep R, Lagrou K, Wilmer A, Jorens P, Hermans G. Invasive pulmonary aspergillosis is a frequent complication of critically ill H1N1 patients: a retrospective study. Intensive Care Med. 2012;38(11):1761–8.
Gillet Y, Issartel B, Vanhems P, Fournet JC, Lina G, Bes M, Vandenesch F, Piemont Y, Brousse N, Floret D, et al. Association between Staphylococcus Aureus strains carrying gene for Panton-valentine leukocidin and highly lethal necrotising pneumonia in young immunocompetent patients. Lancet. 2002;359(9308):753–9.
Roberts JC, Gulino SP, Peak KK, Luna VA, Sanderson R. Fatal necrotizing pneumonia due to a Panton-valentine leukocidin positive community-associated methicillin-sensitive Staphylococcus Aureus and influenza co-infection: a case report. Ann Clin Microbiol Antimicrob. 2008;7:5.
Creech CB, Johnson BG, Bartilson RE, Yang E, Barr FE. Increasing use of extracorporeal life support in methicillin-resistant Staphylococcus Aureus sepsis in children. Pediatr Crit Care Med. 2007;8(3):231–5. quiz 247
Ng D, Klein W, Tran R, Riddle-Branske D, Luna PJ, Nguyen HB. Combination therapy with high-frequency oscillatory ventilation, neuromuscular blockade, inhaled nitric oxide and prone position in acute respiratory distress syndrome with refractory hypoxaemia. Anaesth Intensive Care. 2012;40(5):898–9.
Guervilly C, Hraiech S, Gariboldi V, Xeridat F, Dizier S, Toesca R, Forel JM, Adda M, Grisoli D, Collart F, et al. Prone positioning during veno-venous extracorporeal membrane oxygenation for severe acute respiratory distress syndrome in adults. Minerva Anestesiol. 2014;80(3):307–13.
Gattinoni L, Taccone P, Carlesso E, Marini JJ. Prone position in acute respiratory distress syndrome. Rationale, indications, and limits. Am J Respir Crit Care Med. 2013;188(11):1286–93.
Demory D, Michelet P, Arnal JM, Donati S, Forel JM, Gainnier M, Bregeon F, Papazian L. High-frequency oscillatory ventilation following prone positioning prevents a further impairment in oxygenation. Crit Care Med. 2007;35(1):106–11.
Ip T, Mehta S. The role of high-frequency oscillatory ventilation in the treatment of acute respiratory failure in adults. Curr Opin Crit Care. 2012;18(1):70–9.
Soni KD. Aggarwal R, Gupta a, Sharma P: is the use of high frequency oscillatory ventilator beneficial in managing severe chest injury with massive air leak? BMJ Case Rep. 2014;2014. doi:10.1136/bcr-2014-204284.
Jeng MJ, Lee YS, Tsao PC, Soong WJ. Neonatal air leak syndrome and the role of high-frequency ventilation in its prevention. J Chin Med Assoc. 2012;75(11):551–9.
Galvin I, Krishnamoorthy R, Saad RS. Management of advanced ARDS complicated by bilateral pneumothoraces with high-frequency oscillatory ventilation in an adult. Br J Anaesth. 2004;93(3):454–6.
Tsangaris I, Paramythiotou E, Tsaknis G, Argentos S, Antoniadou A, Kopterides P, Armaganidis A. Ovarian hyperstimulation syndrome complicated by severe community-acquired pneumonia due to methicillin-resistant Staphylococcus Aureus positive for Panton-valentine leukocidin. J Obstet Gynaecol Res. 2012;38(2):476–8.
Panchabhai TS, Khabbaza JE, Raja S, Mehta AC, Hatipoglu U. Extracorporeal membrane oxygenation and toilet bronchoscopy as a bridge to pneumonectomy in severe community-acquired methicillin-resistant Staphylococcus Aureus pneumonia. Ann Thorac Med. 2015;10(4):292–4.
Schwartz KL, Nourse C. Panton-valentine leukocidin-associated Staphylococcus Aureus necrotizing pneumonia in infants: a report of four cases and review of the literature. Eur J Pediatr. 2012;171(4):711–7.
Castaldo ET, Yang EY. Severe sepsis attributable to community-associated methicillin-resistant Staphylococcus Aureus: an emerging fatal problem. Am Surg. 2007;73(7):684–7. discussion 687-688.
Acknowledgements
No acknowledgement.
Funding
Not applicable.
Availability of data and materials
The original data of this case can be found in the record system of Beijing Chao-Yang Hospital. Once published, the data can be found on the website of the Journal.
Author information
Authors and Affiliations
Contributions
All authors made substantial contributions to conception and design, or acquisition of data, or analysis and interpretation of data; reviewed and approved the final manuscript; and contributed significantly to this study. HH takes full responsibility for the integrity of the submission and publication, and was involved in study design. BS, HW and HH had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis, and was responsible for data verification, analysis and drafting of the manuscript. ZT had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. XT, RW and XL were responsible for the microbiological examination and data collection. All authors read and appprove the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
We did not commence any experimental use of a novel procedure or tool in this case, and each of the procedures of ECMO, HFOV and prone positioning was approved by an ethics committee of our hospital, informed consents for each procedure was obtained from the next of kin of the patient.
Consent for publication
Consent to publish her data and pictures was obtained from the patient and submitted as a supplement with the manuscript.
Competing interests
All authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
He, H., Wang, H., Li, X. et al. Successful rescue combination of extracorporeal membrane oxygenation, high-frequency oscillatory ventilation and prone positioning for the management of severe methicillin-resistant Staphylococcus aureus pneumonia complicated by pneumothorax: a case report and literature review. BMC Pulm Med 17, 103 (2017). https://doi.org/10.1186/s12890-017-0445-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-017-0445-z