Abstract
Background
People with intellectual and developmental disability (IDD) have poor oral health and need support to maintain optimal oral health outcomes. Little is known about how, when and where to intervene for this population. Thus the aim of this review was to summarise the existing evidence surrounding improving oral health outcomes for people with IDD.
Methods
A scoping literature review was conducted focusing on ‘oral health’ and ‘intellectual disability’. Systematic searches of five electronic databases were conducted in line with the study aims and two authors independently examined all records for relevance, with consensus achieved by a third author.
Results
A small number of approaches and interventions were identified to support people with IDD to independently maintain optimal oral hygiene. Identified studies highlighted that caregivers play a vital role in the provision of oral health support, emphasising the effectiveness of educational interventions for caregivers. However, there was uncertainty regarding the efficacy of specific tooth brushing interventions for people with IDD. In cases of more severe IDD and/or dental-related behavioural problems, dental treatment under general anaesthesia was often both a necessary and effective method of oral health care provision. The findings also identified outreach and exclusive oral health services as successful strategies for increasing the limited access of people with IDD to oral care services.
Conclusions
A uniform approach to supporting oral health for people with IDD is unlikely to succeed. A system-based approach is needed to address the diverse needs of the population of people with IDD, their caregivers and service context. Further high quality evidence is required to confirm these findings.
Similar content being viewed by others
Background
Recent evidence has highlighted the existence of health inequalities between people with intellectual and developmental disability (IDD) and people without IDD [1,2,3]. Of particular concern is the oral health of people with IDD, with research showing that this population has poorer oral health than those without IDD [4, 5]. In addition, a systematic review by Anders and Davis [4] has specifically shown that people with IDD have a higher prevalence of periodontal disease and untreated dental caries compared with people without IDD. The implications of poor oral health are substantial, with emerging research highlighting the impact poor oral health can have on general health, including significant associations with aspiration pneumonia and major chronic diseases such as cardiovascular disease, diabetes, respiratory disease and stroke [6,7,8,9,10,11,12]. Oral health also has an important influence on an individual’s psychological and social health. For example, poor oral health can lead to toothache, associated anxiety, difficulty performing daily activities, impaired social interactions and reduced nutritional intake [13,14,15,16,17,18,19].
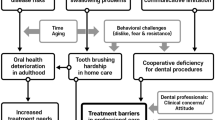
People with IDD are particularly vulnerable to poor oral health and have more complex oral health care needs than people without IDD [20, 21]. This disparity is due to myriad risk factors that people with IDD may experience including barriers to accessing quality health care, the need for assistance with core activities such as oral hygiene, behavioural challenges, communication challenges, a higher prevalence of enteral feeding, and a higher likelihood of having lower educational and income levels when compared to people without IDD [22,23,24].
Caregivers, including paid care staff and family members, play a vital role in maintaining the oral health of people with IDD, particularly when they require assistance with core activities [4]. In recent years, following the shift from institutionalisation of people with IDD to community-based support, caregivers for people with IDD are often family members or support workers rather than trained health professionals [25]. Studies also revealed that lower caregiver education was associated with greater caregiver burden and less preventative dental care use [26]. Caregivers’ attitude towards oral health of special needs patients was found relatively unsatisfactory even though their knowledge was adequate [27]. If interventions to improve the oral health of people with IDD are to be implemented effectively, barriers faced by caregivers should be identified and carefully considered in the investigation and evaluation of these interventions. Likewise, barriers faced by mainstream oral health services also need to be an integral part of the solutions.
Some studies have identified a number of the barriers to oral health care as perceived by caregivers. Although a Cochrane review of oral health interventions published after our search was concluded reported low to very low certainty with all reported interventions [28], and another review explored indications for treatment under GA [29], there has been no broad-based review that also summarises and incorporates the range of barriers to effective oral health care as perceived by caregivers. Given the reported low to very low certainty in evidence, there remains a significant gap in our knowledge of when and how to intervene, given the heterogeneity of the population of people with IDD at different life stages.
The aim of this review was to compile current evidence regarding the promotion of better oral health in people with IDD in order to provide insight into the requirements of enhancing oral health outcomes for people with IDD. The objectives were to:
-
i)
identify any published novel intervention studies and how they sought to provide solutions to poor oral health -for different people with IDD;
-
ii)
explore the literature regarding the types of issues facing people with IDD, their caregivers and dental professionals
-
iii)
identify non-clinical oral health care service contexts that are likely to be embedded in future practices
Methods
Design
A scoping review methodology was implemented to explore current studies, synthesise knowledge of the topic and identify gaps in the literature. This design was best suited to address the broad aims of the study and our desire to look beyond the small number of fully controlled interventions [28] in this area, and also because this design can incorporate a broad range of qualitative and quantitative studies [30].
Search strategy
All articles relevant to the two study objectives were reviewed in this study using the following databases: Science Direct, PubMed, CINAHL, Scopus and Cochrane. Due to the differences in indexing between databases, each database had its own search strategy developed, including a combination of keywords used in conjunction with various Boolean operators, phrase searching, truncation and Medical Subject Headings. Key words used included: oral health, dental, caries, mental retardation, intellectual disability, learning disability, developmental disability, cognitive disability, intellectual impairment, mental deficiency, mentally defective, and psychosocial retardation.
Selection process
All records relating to the study aims published between January, 2000 and March, 2019, and written in English, were selected. Articles reporting on individuals with physical disability only were excluded from analysis. Descriptive studies including dental screening studies and oral health surveys that only reported on oral health status were also excluded. Articles were distributed among the team and independently reviewed for inclusion by pairs of investigators using a summary table, and in the case of conflicting opinions, a third reviewer was involved to achieve consensus. Although definitions varied, articles that reported on people with intellectual disability, learning disability, developmental disability, or IDD were all included provided the majority of participants were reported to have a primary diagnosis of IDD. An overview of this process using the PRISMA flowchart [31] is provided in Fig. 1.
Results
In total, 41 papers were included in this scoping review; key information regarding authors, year of publication, study design, objectives/outcome measures, and key findings were extracted from each article and are summarised in Table 1. Most of the studies were from Europe (n = 12) followed by North America (n = 11), Asia/Arabia (n = 10), the UK (n = 3), Australia (n = 2), South America (n = 2), and Africa (n = 1). Using the Centre for Evidence-based Medicine’s research design flowchart [71], the majority of the studies used observational (n = 25) with the remainder using experimental designs. Studies are grouped into three categories to present a meaningful overview of the literature:
-
Category 1: Interventions – technical and educational
-
1a) tooth brushing
-
1b) caregiver oral health education programs
-
1c) dental care procedures, utilisation of general anaesthesia (GA), and sedation
-
1d) dental clinic setting
-
-
Category 2: Perspectives – people with IDD, caregivers, and contexts.
-
2a) perspectives of people with IDD
-
2b) perspectives of caregivers
-
2c) perspectives of dentists
-
-
Category 3: Non-clinical service delivery contexts
Category 1: interventions – technical and educational
This category explored
1a). Tooth brushing interventions (N = 3)
Shin and Saeed [33] explored which aspects of tooth brushing were more difficult for people with IDD than for people without IDD and whether instructions could improve their technique. They highlighted that the hardest tooth brushing steps were those requiring greater dexterity and comprehension, specifically brushing the front teeth (inside and outside) and removing plaque when identified from disclosing solution [33]. Although most of the instruction focussed on wrist rotation to better access brushing of all tooth surfaces, this did not significantly impact plaque index (PlI) and gingival index (GI). García-Carrillo et al. [32] compared the effect on PlI and GI using electronic versus manual toothbrushes, however found no significant differences in PlI and GI despite the sample with mild IDD reported to have appropriate fine motor skills [33]. Zhou et al. [34] examined if a visual-verbal integration model (VVIM) was effective at teaching children with IDD to dispense a pea-sized amount of fluoridated toothpaste. Their intervention showed that combining both visual and verbal prompts was effective in training parents and children with greater adaptive behaviour skills to dispense a pea-sized amount of toothpaste.
1b). Caregiver oral health education programs (N = 6)
The study by Binkley et al. [35] used four strategies to capacity build paid caregivers, including: 1) agreed caregiver action using behavioural contracts; 2) capacity building through didactic (video and Powerpoint®) and observational (demonstration of teeth cleaning with a client) training; 3) environmental changes such as providing equipment and creating a calm atmosphere; and 4) ongoing coaching and reinforcement from a dental hygienist. In addition to a 50% decrease in the PlI, there was a positive change to caregivers’ oral hygiene supervision of people with IDD and their use of environmental adaptations. Faulks and Hennequin [36] involved both the client and the caregiver in their study. The program consisted of an oral presentation for paid caregivers about dental pathologies and the effect of plaque. This was followed by three repeated practical workshops where a dentist identified the presence of any plaque in each individual with IDD and then provided instructions on the best ways to support the oral health of that person with IDD. The results showed a significant increase in the amount of times teeth were brushed each day and in the caregivers’ ability to brush both the anterior and posterior teeth.
Fickert & Ross [37] used an existing education program where a dental hygienist spent four hours delivering a population-specific workshop, followed by a live demonstration and opportunities for the caregivers to practice their skills. At post-test and follow-up, there was a significant increase in caregiver knowledge and an improvement in oral health skills and compliance. The two Irish studies [38, 39] used a “train-the-trainer” model where managerial staff were trained by dental professionals; the managers then trained their staff. The training consisted of an oral presentation followed by practical workshops on plastic dummies and volunteers, and role-plays about complex oral health scenarios. At post-test, there was a significant increase in caregiver knowledge but no significant difference in caregiver self-efficacy between the intervention and control groups. The study by Phlypo et al. [40], reported on a dental student developed oral health program where the intervention group were provided with booklets, an information session and advice on appropriate toothbrushes and toothpaste. The only significant difference was in post-test GI between the intervention and the control group.
1c). Dentist intervention: dental care procedures, utilisation of general anaesthesia (GA), and sedation (N = 9)
Two studies were based on dental procedures that were only available with access to a dentist (using glass cement on teeth and using a mechanical teeth cleaning/polishing tool) and, although reportedly beneficial to oral health, have few implications outside a dental setting [45, 49]. One study reported on dentists who were provided with background information about their patients with IDD to see if that improved the level of cooperation for more effective treatment, and whether they could better support the special needs of their clients throughout the dental consultation [43].
The other six studies provided insights into the factors that could affect dental routines and treatment procedures for people with IDD, including one that examined the appropriateness of implementing GA in dental treatment [41], four that focussed on the depth of sedation or GA administered [42, 44, 46, 47], as well as one retrospective study on the feasibility of propofol sedation for dental care [48].
Dental treatment under sedation or GA remains a treatment facilitator of choice for people with IDD and severe behavioural problems related to dental examination and treatment. A study conducted in Japan used the International Classification of Functioning (ICF) as a means to measure tolerability for dental procedures as a way of determining the suitability of a person for dental treatment under GA [42]. The study by Vaessen et al. [48] evaluated the safety and effectiveness of propofol sedation during dental treatment (n = 124); propofol sedation is effective providing its flexibility in addressing individual patient needs in combination with low-dose propofol [48]. Silva et al. [47] found that bispectral index (BIS) detected by a bilateral sensor placed on patient’s forehead may be able to reflect anaesthetic depth in patients undergoing dental treatment under GA. Despite the relatively small sample size, monitoring of BIS could potentially benefit some patients with IDD considering the difficulties faced by dentists in interpreting clinical signs of their neurological conditions under anaesthesia. Two of the Japanese studies sought to identify the ideal sedative dose for people with IDD; one study showed the sedative dose for people with IDD was consistently higher than in people without IDD [44], while the other study, using a measurement of the depth of sedation (BIS) in combination with a controlled infusion (TCI) of the sedative drug, reduced the overall amount of sedative drugs needed [46]. The study by Chang et al. [41] adapted the Child Oral Health Impact Profile (COHIP) and the Family Impact Scale (FIS) into short forms COHIP-14 and FIS-12 to examine the impact of dental treatment under GA, with a preoperative questionnaire administered on the day of scheduled treatment and a postoperative questionnaire completed within 1 week to 1 months’ time by caregivers of patients with IDD. Their findings highlighted that dental treatment under GA was worthwhile given the improvement of carer-perceived Oral Health-related Quality of Life (OHRQoL), despite reported restrictions on time and the known additional costs of procedures under a GA.
1d). Dental clinic setting (N = 4)
A sensory adapted dental environment (SADE) is where the provision of sensory modifications within the clinical context is modified to reduce dental anxiety for people with IDD. The crossover Randomised Controlled Trial (RCT) by Shapiro et al. [50], modified visual, tactile, somatosensory and auditory stimuli in a dental clinic for 16 children with IDD and 19 typically developing children. They revealed that children with IDD showed higher levels of relaxation and cooperation in the SADE compared with routine dental environment (RDE). Similarly, two other recent studies observed the efficacy of SADE on dental anxiety of children with IDD (n = 22) [50] and adults with IDD (n = 41) [51]. Potter et al. [51] added to the evidence with both reduced frequency and duration of agitated behaviours in the SADE condition, whereas Shapiro et al. [52] only recorded the duration. The study by Kim et al. [50] involved pre-appointment sensory/behaviour assessment and individualised sensory modifications, which also received positive feedback from the participants. It is also important for health care workers to be able to identify the verbal and non-verbal cues of emotional distress of these patients promptly. Zhou et al. [53] used the Verona coding definitions of emotional sequences (VR-CoDES) to assess distress in the dental context, through reviewing 14 dental consultation videos from patients with varying degree of IDD. Their findings indicate that VR-CoDES is a potentially reliable tool for understanding and managing emotional distress of dental patients with complex communication needs.
Category 2: perspectives – people with IDD, caregivers, and context
2a). The perspectives of people with IDD (N = 3)
Mac Giolla Phadraig et al. [56] explored, using a Delphi process, what people with IDD viewed as being the most important components of a dental visit. Having an informed dental workforce with insight into the issues facing people with IDD was ranked as the most important and cost was the lowest ranked issue. This group of people with IDD were potentially disempowered in their interactions with dental services about their dental care as they either did not, or perhaps could not, complain if unhappy with the services and who were unlikely to have the means or capacity to choose alternative services. Suggestions to improve access to and the quality of services included both services and people with IDD being involved in shared decision-making and having access to more meaningful information.
Lees et al. [55] conducted individual semi-structured interviews with adults with IDD (n = 4) and their carers (n = 6) to explore their community dental services experiences. Although the level of satisfaction across multiple dental service domains was high, the communication problems in the movement from child to adult services were noted. The focus group study by Blaizot et al. [54] first analysed interviews with people with IDD (n = 8) to generate themes and subsequently used the emergent themes to organise information from the other two focus groups: family caregivers (n = 6) and paid caregivers (n = 6). Both studies highlighted the discrepancies in communication competencies of dental professionals, as well as barriers to accessing affordable dental services.
2b). Caregiver perspectives and suggestions to improve oral health (N = 11).
Barriers reported by caregivers included factors associated with the person with IDD, such as lack of comprehension regarding why oral care is essential [57], noncompliance with oral hygiene care [61,62,63] and to alleviate anxiety around oral care [57, 64]. Suggestions for improving oral health outcomes included the provision of specialised dental clinics in disability services [59], access to specific support for culturally negative attitudes towards IDD [60] and training for unpaid caregivers, using tools such as the Dental Discomfort Questionnaire (DDQ) to help identify dental pain earlier [60], and individualised training that targets specific behavioural challenges [63].
Other suggestions were associated with social and environmental support for caregivers. Four studies reported that caregivers recognised the importance of delivery of oral care, but also their self-reported incompetence and lack of training [57, 58, 60, 61]. In the USA, paid caregivers were reported to be more confident in providing oral health care and support when compared to unpaid caregivers [61] and in Australia, people with IDD were more likely to have regular dental visits if they lived in residential services compared to people with IDD living at home [23]. Lack of access to skilled dentists working with adults with IDD was another significant factor [23]. Finances, employment and time burdens were also reported to hinder the oral care practices from these caregivers [63, 66]. The national survey by Wiener et al. [66] analysed responses from caregivers of children with Autism Spectrum Disorder, Developmental Disability and Mental Health Conditions (CASD/DD/MHD) (n = 16,323) in the USA, which reported the association between unmet needs of preventive dental care and financial burdens of the caregivers.
2c). Perspectives of dentists or other health professionals (N = 2).
Byrappagari et al. [67] examined the perspectives of dentists (n = 291) in Michigan, USA of providing care to people with IDD. The results indicated the following barriers: 1) behaviour management problems; 2) inadequate training/experience; 3) severity of patient’s condition; 4) inadequately trained staff; and 5) the additional time required to treat versus inadequate reimbursement. This study reflected the support needed for general dentists in providing better dental care for people with IDD and could potentially contribute to continuing education for practising dentists. Grant et al. [68] reviewed a number of professional viewpoints on how to best achieve better oral health outcomes for people with IDD. Noted strategies were consistent personnel over time, positive verbal feedback to the person with IDD, and adapting a more patient communication style.
Category 3: non-clinical service delivery context (N = 3)
Two studies reported on school-based programs [72, 70] and one on a community outreach program [69]. The school-based dental programs not only reduced many of the access barriers to seeing a dentist, but also improved PlI and GI in children with IDD [72, 70]. Access barriers were also addressed in the outreach program in Hong Kong where repeat visits in the future were requested [69].
Discussion
This study is the first to examine in detail reported strategies to counteract the poor oral health of people with IDD. It has highlighted several aspects of oral health care for people with IDD. One is that the efficacy of specific toothbrushing interventions for people with IDD is yet to be established. Another is that the role of caregivers in the provision of oral health support is vital. Further, for people with more severe IDD and/or dental-related behavioural problems, dental treatment under GA is often both a necessary and effective means of providing oral health care and of improving oral health. Access to services and educational supports remains difficult for people with IDD and their caregivers, however outreach and exclusive services appear to be successful strategies for increasing access. Finally, a range of educational interventions for caregivers are reportedly effective. However, unpaid caregivers do not always have immediate access to these. The remaining gaps in our knowledge are: 1) ideally, where and when should health professionals intervene in oral health care for people with IDD, 2) how should intervention differ when supporting different sub-populations of people with IDD, different caregiver groups, and different service contexts, and 3) how should people with IDD who present to specialised services with severe intolerance to oral health support be best cared for?
Insights into interventions
This review highlighted two types of educational interventions; those that were designed for people with IDD and those designed for paid caregivers. That there were no significant differences in oral health outcomes between the manual and electronic toothbrushes in the study by García-Carrillo et al. [32] suggesting, at least for this sample of people with mild IDD, that technique was not the issue. What was unclear in the literature reviewed was an identification of specific variations between a procedural intervention (e.g., how to approach the task of teeth cleaning conceptually and how to remember to clean one’s teeth) and a technical intervention (e.g., how to technically execute the task of holding a toothbrush and cleaning one’s teeth). That is, the interventions reported were about technique and did not include any strategy for promoting independence, for example, by providing daily reminders or visual toothbrushing charts as suggested for children [73].
It is likely that most toothbrushing interventions would be best targeted at people with the capacity to understand and follow instructions without any associated physical disability that preclude task performance. There would also be the sub-population of people with IDD who had the potential to be semi-independent and would likely require a combination of oral health supports such as toothbrushing interventions and the employment of caregivers trained in the provision of oral health support. Although contributory factors to independence are not clearly reported in the literature, the paper by Maeda et al. [46] about using the ICF as a functional framework to identify differing levels of tolerance to dental procedures is one potential starting point for identifying how to target interventions to individuals.
The interventions reported for paid caregivers all described significant outcomes and were broadly based on two principles; those of enhancing theoretical knowledge and providing opportunitities for caregivers to practice alongside an expert, and offering regular reinforcement over time [35,36,37,38,39]. Two things remain unclear however: i) the length of time the effects of the educational interventions last; and ii) how unpaid family caregivers could access these educational opportunities. The first issue is vital; just because caregivers know how to clean teeth, does not mean that they know the value of oral hygiene [27]. Staff motivation to provide support that is enabling and of high quality differs depending on organisational culture [74, 75]. Disability services require their staff to undertake mandatory training in a range of different areas. The opportunity might exist for oral health educational interventions to be embedded into annual mandatory staff training to promote the value of and potential for better oral health outcomes.
Answers that might identify how to best help unpaid family caregivers access and pay for oral health training are not clear from this review; different funding and service access structures across the world means that overcoming these barriers would be country-specific. In the Australian context, the new National Disability Insurance Scheme (NDIS) has shifted funding to the individual and although it has raised a number of issues around workforce development [76]. For the first time this change offers a concrete way for family caregivers, theoretically, to access specific training in matters of health care such as oral health. As far as we are aware, however, no such training actually exists in Austalia. Nevertheless, the provision of funding codes related to health procedure training for caregivers holds promise, and should be explored further [77]
Insights into service contexts
Some dental interventions for people with IDD can only be provided in the context of a specialised disability dental clinic with GA facilities [41] and where behavioural support options have been exhausted. However, these are a specialised and expensive service option that realistically can only be provided in larger hospital/clinic settings where appropriate perioperative supports are available.
One unintended consequence of the provision of exclusive and specialised dental services could be that limited resources are allocated to providing extreme supports leaving gaps in other mainstream services. Mainstream oral health services should ideally be positioned to make whatever reasonable adjustments are necessary to promote access and inclusion of people with IDD [78]. The use of sensory adpated environments and increasing the knowledge base of dentists and their ancillary staff about IDD, are both important capacity-building strategies that should be implemented more widely [52]. Indeed, people with IDD want to access dental services which have an appreciation of their unique needs [56]. In addition, specialist dental outreach services [69] provide one example of a systems-based approach where adapting centre-based clinical models of dental care in partnership with community-based services, improves access and improves outcomes. This outreach model also mirrors the decentralised “hub and spoke” model for community therapy services (OT, speech, physiotherapy) for people with IDD in rural Australia where the main therapy teams are based in a major centre, but provide outreach services in smaller towns [79].
Implications for research and practice
The authors have not clearly identified at which point intervention is likely to be most beneficial and cost-effective for the promotion of oral health amongst people with IDD. A combination of effectve interventions might have to be developed for implementation at the differing degrees of function, caregiver type, and with dental health professionals to maximise the likelihood that oral health can be maintained and improved. The promising educational interventions suggest that an opportunity exists for researchers, clinicians, and caregivers to collaborate on a standardised, yet adaptable, education program for caregivers in various contexts of care delivery. An example of the types of interventions we are referring to include nurse-led oral health support and training programs for the caregivers of people with IDD who also have chronic and complex health problems that directly impact upon the provision of daily oral hygiene. For instance, oral health support to a person with IDD who has a tracheostomy or is at risk of aspiration. Another could be led by a dental officer and targeted at people with milder degrees of IDD and the potential to be independent with their daily oral hygiene. A third example could be led by a health worker who provides home-based early intervention training for the families of people with IDD who present with behavioural challenges impacting upon their oral health. Although specific to the Australian context, such interventions would fit within the current schedule of services as defined by the NDIS [79].
What is less clear from our review, however, is how the causes of poor oral hygiene, and subsequent interventions to resolve the same, vary within and between contexts. In particular, the sheer range of different systems and eligibility criteria for dental services across the world makes it almost impossible to generalise. Nevertheless, a systems-based approach to oral hygiene for people with IDD that incorporates procedural, behavioural and educational elements and that is adaptable enough to be applied in a variety of client care contexts needs to be developed through an ongoing program of rigorous research.
Limitations
This is a small and diverse body of work and while the review has highlighted a small number of potential areas to focus future interventions, more questions arise. Nevertheless, it presents a starting point for an applied research agenda in this area using the published peer reviewed literature from the selected databases. Another limitation is the use by some authors of vague disability identifiers, such as ‘special needs’ and ‘learning difficulty’ that were excluded as it was not certain the study was about people with IDD. Further, the inability to compare participant groups across studies due to different definitions, demographic profiles and support needs is limiting. The lack of a critical appraisal of included studies represents another limitation, however, the lack of controlled intervention studies in this area, the diverse range of methods, and different types of papers published meant that such a review would offer little to our conclusions. The exclusion of grey literature is another limitation, however adding government and professional reports of guidelines from around the globe is not feasible in a review of this nature.
Conclusion
People with IDD have poor oral health and there is no clear systems-based approach or intervention framework that takes full account of the diverse support needs of the population. What is clear is that a one-size-fits-all approach is unlikely to be effective at maintaining or improving the oral health of people with IDD who are least able to participate in their own care. While educational and technical interventions can be developed and implemented with support from caregivers to people with milder degress of IDD, the problem of caring for the oral health of people with more severe IDD, who are dependent, and who have an aversion to oral health care interventions as fundamental as regular teeth cleaning, remains unresolved. People with IDD, service providers, and paid and unpaid carers need to balance the distribution of educational and technical resources amongst people with IDD who are most able, those who are least able, and all those who fit in between.
Availability of data and materials
All data generated or analysed during this study are included in this published article (and its supplementary information files).
Abbreviations
- BIS:
-
Bispectral Index
- CASD/DD/MHD:
-
Children with Autism Spectrum Disorder, Developmental Disability and Mental Health Conditions
- COHIP:
-
Child Oral Health Impact Profile
- DDQ:
-
Dental Discomfort Questionnaire
- FIS:
-
Family Impact Scale
- GA:
-
General Anaesthesia
- GI:
-
Gingival Index
- ICF:
-
International Classification of Functioning
- IDD:
-
Intellectual and Developmental Disability
- OHRQoL:
-
Oral Health-Related Quality of Life
- PlI:
-
Plaque Index
- RDE:
-
Routine Dental Environment
- SADE:
-
Sensory Adapted Dental Environment
- VR-CoDES:
-
Verona Coding Definitions of Emotional Sequences
- VVIM:
-
Visual-Verbal Integration Model
References
Allerton LA, Welch V, Emerson E. Health inequalities experienced by children and young people with intellectual disabilities: a review of literature from the United Kingdom. J Intellect Disabil. 2011;15(4):269–78.
Emerson E, Baines S. Health inequalities and people with learning disabilities in the UK. Tizard Learn Disabil. 2011;16(1):42–U59.
Merrick J, Merrick E. Equal Treatment: Closing the Gap. A Formal Investigation into Physical Health Inequalities Experienced by People with Learning Disabilities and/or Mental Health Problems. J Policy Pract Intellect Disabil. 2007;4(1):73.
Anders PL, Davis EL. Oral health of patients with intellectual disabilities: a systematic review. Spec Care Dentist. 2010;30(3):110–7.
Wilson NJ, Lin Z, Villarosa A, George A. Oral health status and reported oral health problems in people with intellectual disability: a literature review. J Intellect Develop Disabil. 2019:44(3):292–304. https://doi.org/10.3109/13668250.2017.1409596.
Aida J, Kondo K, Yamamoto T, Hirai H, Nakade M, Osaka K, et al. Oral health and cancer, cardiovascular, and respiratory mortality of Japanese. J Dent Res. 2011;90(9):1129–35.
Cohen W, Rose LF, Minsk L. The periodontal–medical risk relationship. 2001;22(2 Spec No):7–11.
Genco RJ, Glurich I, Haraszthy V, Zambon J, DeNardin E. Overview of risk factors for periodontal disease and implications for diabetes and cardiovascular disease. Compend Contin Educ Dent (Jamesburg, NJ : 1995). 2001;22(2 Spec No):21–23.
Joshipura KJ, Hung H-C, Rimm EB, Willett WC, Ascherio A. Periodontal disease, tooth loss, and incidence of ischemic stroke. Stroke. 2003;34(1):47–52.
Jung SH, Ryu JI, Jung DB. Association of total tooth loss with socio-behavioural health indicators in Korean elderly. J Oral Rehabil. 2011;38(7):517–24.
Tada A, Miura H. Prevention of aspiration pneumonia (AP) with oral care. Arch Gerontol Geriatr. 2012;55(1):16–21.
Walls AW, Steele JG. Geriatric oral health issues in the United Kingdom. Int Dent J. 2001;51(3 Suppl):183–7.
Alves NS, Gavina VP, Cortellazzi KL, Antunes LA, Silveira FM, Assaf AV. Analysis of clinical, demographic, socioeconomic, and psychosocial determinants of quality of life of persons with intellectual disability: a cross-sectional study. Spec Care Dentist. 2016;36(6):307–14.
Couto P, Pereira PA, Nunes M, Mendes RA. Oral health-related quality of life of Portuguese adults with mild intellectual disabilities. PLoS One. 2018;13(3):e0193953.
Hillebrecht AL, Hrasky V, Anten C, Wiegand A. Changes in the oral health-related quality of life in adult patients with intellectual disabilities after dental treatment under general anesthesia. Clin Oral Investig. 2019:1–9.
Locker D. In: GD Slade, editor, Measuring Oral Health and Quality of Life. Concepts of oral health, disease and the quality of life. Deaprtment of Dental Ecology, School of Dentistry. University of North Carolina; 1997. p. 11–24. https://www.adelaide.edu.au/arcpoh/downloads/publications/reports/miscellaneous/measuring-oral-health-and-quality-of-life.pdf.
Zucoloto ML, Maroco J, Campos JA. Impact of oral health on health-related quality of life: a cross-sectional study. BMC Oral Health. 2016;16(1):55.
McGrath C, Zhou N, Wong HM. A systematic review and meta-analysis of dental plaque control among children and adolescents with intellectual disabilities. J Appl Res Intellect Disabil. 2019;32(3):522–32.
Zhou N, Wong HM, Wen YF, McGrath C. Oral health status of children and adolescents with intellectual disabilities: a systematic review and meta-analysis. Dev Med Child Neurol. 2017;59(10):1019–26.
NSW Ministry of Health. Centre for Oral Health Strategy. Oral health 2020: A strategic framework for dental health in NSW. Sydney NSW Minist Health. 2013. p. 10–11.
Horwitz SM, Kerker BD, Owens PL, Zigler E. The health status and needs of individuals with mental retardation. New Haven: Yale University; 2000.
Kavanagh A, Krnjacki L, Kelly M. Disability and health inequalities in Australia: research summary. Victoria: Victorian Health Promotion Foundation; 2012.
Pradhan A, Slade GD, Spencer AJ. Access to dental care among adults with physical and intellectual disabilities: residence factors. Aust Dent J. 2009;54(3):204–11.
Slack-Smith L, Ree M, Leonard H. Oral health and children with an intellectual disability: a focus group study of parent issues and perceptions. J Disabil Oral Health. 2010;11(4):171–9.
Glassman P, Miller CE. Effect of preventive dentistry training program for caregivers in community facilities on caregiver and client behavior and client oral hygiene. N Y State Dent J. 2006;72(2):38–46.
Chi DL, McManus BM, Carle AC. Caregiver burden and preventive dental care use for US children with special health care needs: a stratified analysis based on functional limitation. Matern Child Health J. 2014;18(4):882–90.
Shah AH, Naseem M, Khan MS, Asiri FYI, AlQarni I, Gulzar S, et al. Oral health knowledge and attitude among caregivers of special needs patients at a comprehensive rehabilitation Centre: an analytical study. Annali Di Stomatologia. 2018;8(3):110–6.
Waldron C, Nunn J, Mac Giolla Phadraig C, Comiskey C, Guerin S, van Harten MT, Donnelly-Swift E, Clarke MJ. Oral hygiene interventions for people with intellectual disabilities. Cochrane Database Syst Rev. 2019;(5):CD012628. https://doi.org/10.1002/14651858.CD012628.pub2.
Dougherty N. The dental patient with special needs: a review of indications for treatment under general anesthesia. Spec Care Dentist. 2009;29(1):17–20.
Colquhoun HL, Levac D, O'Brien KK, Straus S, Tricco AC, Perrier L, et al. Scoping reviews: time for clarity in definition, methods, and reporting. J Clin Epidemiol. 2014;67(12):1291–4.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
Garcia-Carrillo A, Jover A, Pla R, Martorell A, Sota C, Gomez-Moreno G, et al. Manual versus sonic powered toothbrushing in patients with intellectual disability: a cluster-randomized clinical trial. J Clin Periodontol. 2016;43(8):684–93.
Shin CJ, Saeed S. Toothbrushing barriers for people with developmental disabilities: a pilot study. Spec Care Dentist. 2013;33(6):269–74.
Zhou N, Wong HM, McGrath C. Effectiveness of a visual-verbal integration model in training parents and their preschool children with intellectual and developmental disabilities to dispense a pea-sized amount of fluoridated toothpaste. J Appl Res Intellect Disabil. 2019;32(3):657–65.
Binkley CJ, Johnson KW, Abadi M, Thompson K, Shamblen SR, Young L, et al. Improving the oral health of residents with intellectual and developmental disabilities: an oral health strategy and pilot study. Eval Program Plann. 2014;47:54–63.
Faulks D, Hennequin M. Evaluation of a long-term oral health program by carers of children and adults with intellectual disabilities. Spec Care Dentist. 2000;20(5):199–208.
Fickert NA, Ross D. Effectiveness of a caregiver education program on providing oral care to individuals with intellectual and developmental disabilities. Intellect Dev Disabil. 2012;50(3):219–32.
Mac Giolla Phadraig C, Guerin S, Nunn J. Train the trainer? A randomized controlled trial of a multi-tiered oral health education programme in community-based residential services for adults with intellectual disability. Community Dent Oral Epidemiol. 2013;41(2):182–92.
Mac Giolla Phadraig C, Guerin S, Nunn J. Should we educate care staff to improve the oral health and oral hygiene of people with intellectual disability in residential care? Real world lessons from a randomized controlled trial. Spec Care Dentist. 2015;35(3):92–8.
Phlypo I, De Tobel J, Marks L, De Visschere L, Koole S. Integrating community service learning in undergraduate dental education: a controlled trial in a residential facility for people with intellectual disabilities. Spec Care Dentist. 2018;38(4):201–7.
Chang J, Patton LL, Kim HY. Impact of dental treatment under general anesthesia on the oral health-related quality of life of adolescents and adults with special needs. Eur J Oral Sci. 2014;122(6):363–71.
Maeda S, Kita F, Miyawaki T, Takeuchi K, Ishida R, Egusa M, et al. Assessment of patients with intellectual disability using the international classification of functioning, disability and health to evaluate dental treatment tolerability. J Intellect Disabil Res. 2005;49(Pt 4):253–9.
Meurs D, Rutten M, de Jongh A. Does information about patients who are intellectually disabled translate into better cooperation during dental visits? Spec Care Dentist. 2010;30(5):200–5.
Miyawaki T, Kohjitani A, Maeda S, Egusa M, Mori T, Higuchi H, et al. Intravenous sedation for dental patients with intellectual disability. J Intellect Disabil Res. 2004;48(Pt 8):764–8.
Mori Y, Amano A, Akiyama S, Morisaki I. Effects of short professional mechanical tooth-cleaning (PMTC) program in young adults with mental disabilities. Spec Care Dentist. 2000;20(1):18–22.
Sakaguchi M, Higuchi H, Maeda S, Miyawaki T. Dental sedation for patients with intellectual disability: a prospective study of manual control versus Bispectral index-guided target-controlled infusion of propofol. J Clin Anesth. 2011;23(8):636–42.
Silva A, Amorim P, Felix L, Abelha F, Mourao J. Analysis of electroencephalogram-derived indexes for anesthetic depth monitoring in pediatric patients with intellectual disability undergoing dental surgery. J Dent Anesth Pain Med. 2018;18(4):235–44.
Vaessen HH, Schouten AN, van der Hoeve H, Knape JT. The feasibility of office-based propofol sedation for dental care in patients with intellectual disability by sedation practitioners. Spec Care Dentist. 2017;37(2):93–8.
Yeganegi KS, Tandon S. Tooth surface protection for individuals who are mentally disabled. Spec Care Dentist. 2008;28(1):32–8.
Kim G, Carrico C, Ivey C, Wunsch PB. Impact of sensory adapted dental environment on children with developmental disabilities. Spec Care Dentist. 2019;39(2):180–7.
Potter CN, Wetzel JL, Learman KE. Effect of sensory adaptations for routine dental care in individuals with intellectual and developmental disabilities: a preliminary study. J Intellect Develop Disabil. 2018;44(3):305–14.
Shapiro M, Sgan-Cohen HD, Parush S, Melmed RN. Influence of adapted environment on the anxiety of medically treated children with developmental disability. J Pediatr. 2009;154(4):546–50.
Zhou Y, Black R, Freeman R, Herron D, Humphris G, Menzies R, et al. Applying the Verona coding definitions of emotional sequences (VR-CoDES) in the dental context involving patients with complex communication needs: an exploratory study. Patient Educ Couns. 2014;97(2):180–7.
Blaizot A, Hamel O, Folliguet M, Herve C, Meningaud JP, Trentesaux T. Could ethical tensions in Oral healthcare management revealed by adults with intellectual disabilities and caregivers explain unmet Oral health needs? Participatory research with focus groups. J Appl Res Intellect Disabil. 2017;30(1):172–87.
Lees C, Poole H, Brennan M, Irvine F. Adults with learning disabilities experiences of using community dental services: service user and carer perspectives. Brit J Learn Disabil. 2017;45(2):114–20.
Mac Giolla Phadraig C, Dougall A, Stapleton S, McGeown D, Nunn J, Guerin S. What should dental services for people with disabilities in Ireland be like? Agreed priorities from a focus group of people with learning disabilities. Brit J Learn Disabil. 2016;44(4):259–68.
Chadwick D, Chapman M, Davies G. Factors affecting access to daily oral and dental care among adults with intellectual disabilities. J Appl Res Intellect Disabil. 2018;31(3):379–94.
Eijsink AM, Schipper G, Vermaire JH. A Q-methodology study among caregivers of people with moderate intellectual disabilities on their clients' health care: an example in oral health. J Appl Res Intellect Disabil. 2018;31(5):915–26.
Gerreth K, Borysewicz-Lewicka M. Access barriers to dental health Care in Children with disability. A questionnaire study of parents. J Appl Res Intellect Disabil. 2016;29(2):139–45.
Kahabuka FK, Ndalahwa M. Parental oral health care of mentally retarded children in Ilala municipality, Dar Es Salaam, Tanzania. Int J Dent Hyg. 2006;4(3):145–9.
Minihan PM, Morgan JP, Park A, Yantsides KE, Nobles CJ, Finkelman MD, et al. At-home oral care for adults with developmental disabilities: a survey of caregivers. J Am Dent Assoc (1939). 2014;145(10):1018–25.
Oliveira AC, Paiva SM, Pordeus IA. Parental acceptance of restraint methods used for children with intellectual disabilities during dental care. Spec Care Dentist. 2007;27(6):222–6.
Thole K, Chalmers J, Ettinger RL, Warren J. Iowa intermediate care facilities: an evaluation of care providers' attitudes toward oral hygiene care. Spec Care Dentist. 2010;30(3):99–105.
Versloot J, Hall-Scullin E, Veerkamp JSJ, Freeman R. Dental discomfort questionnaire: its use with children with a learning disability. Spec Care Dentist. 2008;28(4):140–4.
Weckwerth SAM, Weckwerth GM, Ferrairo BM, Chicrala GM, Ambrosio AMB, Toyoshima GHL, Bastos JRMB, Pinto EC, Velasco SRM, Bastos RS, (2016) Parents'. perception of dental caries in intellectually disabled children. Special Care in Dentistry 36(6):300–6.
Wiener RC, Vohra R, Sambamoorthi U, Madhavan SS. Caregiver burdens and preventive dental Care for Children with autism Spectrum disorder, developmental disability and/or mental health conditions: National Survey of CSHCN, 2009-2010. Matern Child Health J. 2016;20(12):2573–80.
Byrappagari D, Jung Y, Chen K. Oral health care for patients with developmental disabilities: a survey of Michigan general dentists. Spec Care Dentist. 2018;38(5):281–90.
Grant E, Carlson G, Cullen-Erickson M. Oral health for people with intellectual disability and high support needs: positive outcomes. Spec Care Dentist. 2004;24(2):70–9.
Lo EC, Luo Y, Dyson JE. Outreach dental service for persons with special needs in Hong Kong. Spec Care Dentist. 2004;24(2):80–5.
York JA, Holtzman JM. Designing and implementing a school-based dental program for students with developmental disabilities. Spec Care Dentist. 2004;24(6):308–12.
Grimes DA, Schulz KF. An overview of clinical research: the lay of the land. Lancet. 2002;359(9300):57–61.
Shyama M, Al-Mutawa SA, Honkala S, Honkala E. Supervised toothbrushing and oral health education program in Kuwait for children and young adults with Down syndrome. Spec Care Dentist. 2003;23(3):94–9.
Pine CM, McGoldrick PM, Burnside G, Curnow MM, Chesters RK, Nicholson J, et al. An intervention programme to establish regular toothbrushing: understanding parents' beliefs and motivating children. Int Dent J. 2000;50(S6_Part1):312–23.
Bigby C, Beadle-Brown J. Culture in better group homes for people with intellectual disability at severe levels. Intellect Dev Disabil. 2016;54(5):316–31.
Bigby C, Beadle-Brown J. Improving quality of life outcomes in supported accommodation for people with intellectual disability: what makes a difference? J Appl Res Intellect Disabil. 2018;31:e182–200.
Dowse L, Wiese M, Dew A, Smith L, Collings S, Didi A. More, better, or different? NDIS workforce planning for people with intellectual disability and complex support needs. J Intellect Develop Disabil. 2016;41(1):81–4.
Ryan R, Stanford J. A portable training entitlement system for the disability support services sector. Canberra: The Australia Institute; 2018.
Giuntoli G, Newton B, Fisher KR. Current models of health service delivery for people with intellectual disability – Literature review. Sydney: Social Policy Research Centre, UNSW Australia; 2015. Contract No.: SPRC Report 12/2015.
Dew A, Veitch C, Lincoln M, Brentnall J, Bulkeley K, Gallego G, et al. The need for new models for delivery of therapy intervention to people with a disability in rural and remote areas of Australia. J Intellect Develop Disabil. 2012;37(1):50–3.
Acknowledgements
We acknowledge Luke Warren, the liaison librarian for the School of Nursing and Midwifery, Western Sydney University for his support with the literature search and for training Zhen Lin in literature search techniques.
Funding
This research was supported by a competitive student scholarship under the Western Sydney University Undergraduate Summer Research Program funded between 1st December 2016 and 24th February 2017. The Program appointed a student (ZL) to work with the primary authors (NJW and AG) on the nominated literature review where the student was expected to learn research skills in designing, conducting, analysing, interpreting, and writing up a literature reivew.
Author information
Authors and Affiliations
Contributions
AG, NJW and ZL conceived the idea. NJW and ZL screened the articles. All authors (NJW, ZL, AV, PL, PP, BS, & AG) worked together to review the articles until agreement was reached. All authors then created the table of papers. NJW, PL and ARV led the writing. NJW and PL checked and revised the text. BS and PP led the final editing stages of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Wilson, N.J., Lin, Z., Villarosa, A. et al. Countering the poor oral health of people with intellectual and developmental disability: a scoping literature review. BMC Public Health 19, 1530 (2019). https://doi.org/10.1186/s12889-019-7863-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-019-7863-1