Abstract
Background
Influenza generates a significant societal impact on morbidity, mortality, and associated costs. The study objective was to identify factors associated with influenza-like-illness (ILI) episodes during seasonal influenza epidemics among the general population.
Methods
A prospective study was conducted with the GrippeNet.fr crowdsourced cohort between 2012/13 and 2017/18. After having completed a yearly profile survey detailing socio-demographic, lifestyle and health characteristics, participants reported weekly data on symptoms. Factors associated with at least one ILI episode per influenza epidemic, using the European Centre for Disease Prevention and Control case definition, were analyzed through a conditional logistic regression model.
Results
From 2012/13 to 2017/18, 6992 individuals participated at least once, and 61% of them were women (n = 4258). From 11% (n = 469/4140 in 2013/14) to 29% (n = 866/2943 in 2012/13) of individuals experienced at least one ILI during an influenza epidemic. Factors associated with higher risk for ILI were: gender female (OR = 1.29, 95%CI [1.20; 1.40]), young age (< 5 years old: 3.12 [2.05; 4.68]); from 5 to 14 years old: 1.53 [1.17; 2.00]), respiratory allergies (1.27 [1.18; 1.37]), receiving a treatment for chronic disease (1.20 [1.09; 1.32]), being overweight (1.18 [1.08; 1.29]) or obese (1.28 [1.14; 1.44]), using public transport (1.17 [1.07; 1.29]) and having contact with pets (1.18 [1.09; 1.27]). Older age (≥ 75 years old: 0.70 [0.56; 0.87]) and being vaccinated against influenza (0.91 [0.84; 0.99]) were found to be protective factors for ILI.
Conclusions
This ILI risk factors analysis confirms and further completes the list of factors observed through traditional surveillance systems. It indicates that crowdsourced cohorts are effective to study ILI determinants at the population level. These findings could be used to adapt influenza prevention messages at the population level to reduce the spread of the disease.
Similar content being viewed by others
Background
Seasonal influenza represents a major cause of morbidity and mortality worldwide, responsible for 3 to 5 million of serious illnesses [1], and for 290,000 to 650,000 deaths annually, according to recent updates from the World Health Organization and the United States Centers for Disease Control and Prevention [2]. Clinical manifestations occur through influenza-like-illness (ILI) with sudden onset of fever, myalgia and respiratory signs [3].
Documented influenza risk factors are related to (i) individual characteristics, such as age (higher risk of infection for young age, higher risk of complication and mortality for older age) [4, 5], immunodeficiency [1], pregnancy [6], chronic underlying medical conditions and respiratory diseases [7]; (ii) individual’s household features, such as living with children [8]; or (iii) individual’s profession like having contacts with children [9] or infected individuals [10]. However, the number of factors analyzed per study is often limited and mainly identified through traditional surveillance systems based on healthcare professionals [6, 7] or households follow-up [5, 8, 10].
Risk factors identified through healthcare systems or household studies may not be generalized to the general population, as they pertain more severe cases, or individuals selected based on their influenza susceptibility. Exploring risk factors for influenza directly from the general population can help to have a better knowledge of a larger spectrum of infections, including milder infections. Targeting message to individuals at risk of influenza and not only to those at risk of severe influenza may contribute to help limiting the spread of the disease in the population and potentially reducing the associated costs. An influenza epidemic in France is estimated to cost around $2.6 billion, with $0.3 billion of direct costs of medical care and $2.3 billion of indirect costs due to loss of productivity, leading to 2.9 (±2.5) days of work lost per influenza episode and person [11, 12].
Risk factors analyses based on the general population have been already addressed, but most were implemented during the 2009 A/H1N1pdm09 pandemic [13]. Since 2009, a participatory syndromic surveillance system for influenza, called Influenzanet, is operational in Europe [14, 15]. The system allows fine scale data collection among the general population enabling detailed risk factors analyses [16]. Here we focus on six consecutive influenza seasons, from 2012/13 to 2017/18, to estimate ILI frequency among the GrippeNet.fr (GN) cohort in France and identify the factors associated with ILI infections.
Methods
GrippeNet.fr data collection
GN is a crowdsourced surveillance system operating each year from November to April in mainland France since 2012. It is part of a broader European platform Influenzanet, where ten countries are involved [15]. Individuals from the GN cohort report their influenza-related symptoms through a dedicated website (https://www.grippenet.fr). Consent is informed and implied through registration and voluntarily completing a profile survey. This profile survey can be updated throughout the season, and covers socio-demographic (gender, age, household composition, occupation, place of residency); lifestyle (having pets, daily contacts, daily transportation means, smoking habit); and health-related characteristics (height and weight to estimate the body mass index (BMI), chronic treatments for at least one comorbidity including asthma, diabetes, immunosuppression, heart, kidney or pulmonary diseases, influenza vaccination status for the current and past seasons, respiratory allergies) [17, 18]. After the profile completion, symptoms data are collected on a weekly basis [14,15,16]. If symptoms are reported (from a list of 19 symptoms), further questions are asked to detail them and the participant behavior [19]. The profile and weekly symptoms surveys were published elsewhere (profile survey [17] and symptoms survey [19]). Participants can also answer to profile surveys and weekly symptoms surveys for other household members through multi-user accounts to facilitate for example participation and report of children and elderly. Each participant added in this way has all her/his individual information filled in the platform and was considered as an individual participant in our analyses.
Although GN participants were not representative of the French general population in terms of age and gender (overrepresentation of middle-aged individuals and women), all age classes were represented (data from 2011/12 season [17]). The GN population was also found to be more frequently employed, with a higher education level. No significant difference was found regarding chronic conditions, such as asthma and diabetes.
Study period
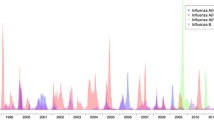
The analysis was conducted on six GN seasons from 2012/13 to 2017/18.
Study participants
Each season, GN participants who provided regular information were included in the current study. Regular information was defined as having filled at least one profile survey and three weekly symptoms surveys for a given season. At least one symptoms survey should have been completed before, another during and one after the influenza epidemic period as stated by the French national surveillance network in primary care, called Sentinelles network [20]. A similar inclusion criterion was used in a previous work conducted at the European level [16]. Individuals included in the study may have participated in one to six GN seasons.
ILI case definitions
Different case definitions have been built from symptoms declared on GN [19]. For the risk factors analyses, we considered the ILI definition of the European Centre for Disease Control and Prevention (ILIECDC), which is often used by other Influenzanet studies [16, 21, 22]. ILI is defined as (i) the sudden onset of symptoms, AND (ii) at least one of the following four systemic symptoms (fever or feverishness, malaise, headache or myalgia), AND (iii) at least one of the three respiratory symptoms (cough, sore throat, shortness of breath) [23]. The analyses were also conducted on a much more specific definition, closer to the one used by the French general practitioners (GP) Sentinelles network, stated as GNILI- and defined by (i) sudden onset of symptoms, AND (ii) fever ≥38 °C or fever (when the body temperature level was not available) AND pain or headache, AND (iii) sore throat or cough or shortness of breath [19]. The latter was computed as a sensitivity analysis, in order to clarify the ILI risk factors found.
As demonstrated in previous research, ILI represents a good proxy for influenza estimates [3, 24]. As no influenza virological confirmation was available, we took only into account ILI occurring during the influenza epidemic period identified by the Sentinelles network.
Statistical analyses
Characteristics of the study participants between 2012/13 to 2017/18 were described depending on the last profile survey completed over the study period. As GN is an observational cohort, most of the participants are returning participants season after season, and so one participant can be counted in the study from one to six times. A person-season was defined as an individual having participated in the study during one season. Determinants associated with having at least one ILI episode during a follow-up season were estimated through a conditional logistic regression model, using the generalized estimated equations for longitudinal correlated data, based on the person-seasons. Explanatory variables (season, socio-demographic, geographic, health-related and lifestyle characteristics) were tested in univariate analyses. All covariates with a p-value below 0.2 were tested in multivariate analyses. Covariates were selected through a backward stepwise selection. The final model included all covariates associated with having at least one ILI episode with a p-value below or equal to 0.05. Same analyses were conducted using the more specific definition (GNILI-). All statistical analyses were performed using the R software (3.2.5 version) and the geepack package [25, 26].
Results
Participation
Participation description is available in Table 1. Overall, there were 6992 individuals who participated at least once over the study period from 2012/13 to 2017/18. The 6992 individuals represented 24,653 person-seasons over the 6 year follow-up. An individual participated on average three seasons from 2012/13 to 2017/18. The mean number of participants per season was 4109 (min = 2943 in 2012/13 and max = 4780 in 2015/16). Individuals filled a mean number of 19 weekly symptoms surveys per season over the 6 years follow-up, with seasons lasting from 19 to 23 weeks.
Description of the participants
Socio-demographic, lifestyle and health-related characteristics of the 6992 participants included in the study were described in Table 2. Overall, participants were mostly women (61%, n = 4258), living in urban area (81%, n = 5637), and having a mean age of 51 years old. Regarding daily contacts, 32% (n = 2268) were in contact with groups of ≥10 individuals, 26% (n = 1788) with children (beyond their own ones), 10% (n = 728) with patients and 10% (n = 721) with elderly. Vaccination against influenza for the current season was done in 36% (n = 2517) of the individuals followed (min = 29% in 2013/14, and max = 42% in 2017/18). Concerning the underlying health conditions, 22% (n = 1504) of the participants were treated for at least one comorbidity (as known as asthma, diabetes, immunosuppression, heart, kidney and pulmonary diseases). One third (n = 2413) had respiratory allergies and 11% (n = 766) were smokers. Further details are available in Table 2. The description of the participants for the six seasons from 2012/13 to 2017/18 did not show any difference between seasons. Full results are detailed in Additional file 1.
Estimations of ILI episodes
Depending on GN season, from 11% (469/4140 in 2013/14) to 29% (866/2943 in 2012/13) of individuals experienced at least one ILIECDC episode during the influenza epidemic. Using the more specific GNILI- definition, this range reduced from 3% (111/4140 in 2013/14) to 8% (231/2943 in 2012/13) (Table 1).
Risk factor analyses: univariate and multivariate analyses
In the univariate analysis, factors associated with having at least one ILIECDC episode during the influenza epidemic period with a p-value below 0.2 were: gender, age, household composition, occupation, use of public transport, pets at home, contacts with patients, contact with a group of individuals, contact with children, influenza vaccination status regarding the current and past seasons, being treated for health comorbidities, respiratory allergy, and body mass index (Table 3).
In the final multivariate model (Table 3), women tended to have more ILIECDC episodes with respect to men (OR = 1.29, [1.20; 1.40]). Children experienced more ILIECDC episodes compared to adults from 45 to 64 (OR = 3.12 [2.05; 4.68] for children from 0 to 4, and OR = 1.53 [1.17; 2.00] for children from 5 to 14). Individuals using public transport (OR = 1.17 [1.07; 1.29]), having pets at home (OR = 1.18 [1.09; 1.27]), treated for health comorbidities (OR = 1.20 [1.09; 1.32]), having respiratory allergy (OR = 1.27 [1.18; 1.37]), or being overweight or obese (OR = 1.18 [1.08; 1.29] and OR = 1.28 [1.14; 1.44], respectively) were also more prone to experience an ILIECDC episode. On the contrary, individuals aged 75 years or older tended to have fewer ILIECDC episodes compared to those in the range of 45 to 64 (OR = 0.70 [0.56; 0.87]). Individuals vaccinated for the current season were also found to be at lower risk (OR = 0.91 [0.84; 0.99]).
The sensitivity analysis conducted with the more specific GNILI- definition showed similar results (see Additional file 2).
Discussion
This study allowed us to identify factors associated with ILI directly from the general population. Some health determinants already described in the literature were found, such as having a young age or health comorbidities. We also found more debated risk factors, such as sex and the use of public transport, or rather unexpected ones, such as living with pets.
In our analyses, women were found to be at higher risk for ILI, independently of the case definition used (either ILIECDC or GNILI- definitions). Female vs. male differences regarding influenza have been previously evaluated: at younger (< 20 years) and older (> 80) ages, morbidity rates seem to be higher for males than females, however during the reproductive age (from 20 to 49 age group) women were found to have higher morbidity rates [27,28,29]. The observed differences are thought to be based on various factors that can affect both sex (e.g. genetic, immunological, and hormonal differences) and gender (i.e. behavioural) characteristics [27, 29, 30]. Here, the increased risk for women is found even adjusting for behavioural determinants such as living or having contacts with children. Further investigations should be implemented to understand better the biological and behavioural impacts.
Taking public transport is associated in our study with an increased risk for ILI. Only few studies addressed this association. One found that public transport used within 5 days of symptoms onset was associated with an increased risk of consulting for acute respiratory infection [31]. Previous Influenzanet works did not find an association between public transport and influenza [16, 21, 32], likely because of lack of statistical power due to the consideration of one season only [16, 21] or due to methodological differences based on the public transport covariate definition [32]. In this last article, the public transport covariate was defined using three categories (bicycle/foot, car and public transport), whereas here we opted for two categories (private vs. public transports) in order to better observe any impact of public transports with respect to other modes of daily locomotion, where individuals do not have close contacts.
Individuals who had pets at home had a higher chance of experiencing ILI as well. This result confirms previous findings obtained in the Influenzanet platform [16, 32], though it still remains unexplained. It would be interesting to further explore additional factors that can impact this small increased risk observed, such as the lifestyle of individuals living with pets and the contacts they establish.
In addition to the risk factor analysis, we estimated here the average fraction of individuals presenting at least one ILI episode during a season, ranging from 5% (GNILI-) to 19% (ILIECDC). International studies have provided estimates in the same ballpark (2.8 to 10.9% in the US [33], 10 to 25% in Canada [34]), however the comparison can be difficult as influenza impact depends on the specific season but also on the surveillance system and the case definition. In France, an average 3.4% of the population was estimated to have an ILI requiring a medical consultation from general practitioners surveillance data [20], a lower value compared to our GN estimate that can be explained by the limited fraction of illnesses leading to health-seeking behavior (56.7% of GNILI- episodes, 32.6% with the ILIECDC definition) [35].
The strength of this study is the identification of ILI determinants in the general population. Fine scale data have been collected through a large panel of individuals during several seasons allowing the evaluation of a wide range of ILI determinants. Little-known risk factors for ILI were identified in addition to well-known factors indicating that GrippeNet.fr is effective to study ILI determinants at the population level. However, a few limitations can be highlighted. First, the cohort was not representative of the French population as it is a crowdsourced system. Nevertheless, all ages and gender were represented. Second, no virological confirmation was available to ensure influenza follow-up. Thus, risk factors found here were not specifically associated with influenza infection but with a broader set of respiratory viruses causing similar symptoms. To limit the impact of this aspect, we decided to include only ILI episodes occurring during the influenza epidemic period, and also to explore two ILI case definitions, namely a more sensitive one (ILIECDC) and a more specific one (GNILI-).
Conclusion
The identification of risk factors from the general population performed in this study confirms and further completes the list of factors observed through traditional surveillance systems. These findings can help target specific communication and influenza prevention campaigns at the population level aimed at reducing the spread of the disease. Some ILI risk factors, as gender, public transport use and having pets are still debated, they should be further investigated.
Availability of data and materials
GrippeNet.fr databases used in this study are not publicly available, in accordance with the authorization we have from the French National Commission on Informatics and Liberty (CNIL, authorization DR-2012-024). The datasets used and/or analysed during the current study are available from the authors on reasonable request.
Abbreviations
- BMI:
-
body mass index
- ECDC:
-
European Centre for Disease Prevention and Control
- GN:
-
GrippeNet.fr
- ILI:
-
influenza-like-illness
References
World health organization: influenza (seasonal) - fact sheet http://www.who.int/mediacentre/factsheets/fs211/en/ (2018). Accessed 15 Nov 2018.
Iuliano AD, Roguski KM, Chang HH, Muscatello DJ, Palekar R, Tempia S, Cohen C, Gran JM, Schanzer D, Cowling BJ, et al. Estimates of global seasonal influenza-associated respiratory mortality: a modelling study. Lancet. 2018;391:1285–300.
Casalegno JS, Eibach D, Valette M, Enouf V, Daviaud I, Behillil S, Vabret A, Soulary JC, Benchaib M, Cohen JM, et al. Performance of influenza case definitions for influenza community surveillance: based on the French influenza surveillance network GROG, 2009-2014. Euro Surveill. 2017;22:14.
Fiore AE, Uyeki TM, Broder K, Finelli L, Euler GL, Singleton JA, Iskander JK, Wortley PM, Shay DK, Bresee JS, et al. Prevention and control of influenza with vaccines: recommendations of the advisory committee on immunization practices (ACIP), 2010. MMWR Recomm Rep. 2010;59(RR-8):1–62.
Riley S, Kwok KO, Wu KM, Ning DY, Cowling BJ, Wu JT, Ho LM, Tsang T, Lo SV, Chu DK, et al. Epidemiological characteristics of 2009 (H1N1) pandemic influenza based on paired sera from a longitudinal community cohort study. PLoS Med. 2011;8(6):e1000442.
Sappenfield E, Jamieson DJ, Kourtis AP. Pregnancy and susceptibility to infectious diseases. Infect Dis Obstet Gynecol. 2013;2013:752852.
Jain S, Kamimoto L, Bramley AM, Schmitz AM, Benoit SR, Louie J, Sugerman DE, Druckenmiller JK, Ritger KA, Chugh R, et al. Hospitalized patients with 2009 H1N1 influenza in the United States, April-June 2009. N Engl J Med. 2009;361(20):1935–44.
Viboud C, Boelle PY, Cauchemez S, Lavenu A, Valleron AJ, Flahault A, Carrat F. Risk factors of influenza transmission in households. The British journal of general practice: the journal of the Royal College of General Practitioners. 2004;54(506):684–9.
Marchbanks TL, Bhattarai A, Fagan RP, Ostroff S, Sodha SV, Moll ME, Lee BY, Chang CC, Ennis B, Britz P, et al. An outbreak of 2009 pandemic influenza a (H1N1) virus infection in an elementary school in Pennsylvania. Clin Infect Dis. 2011;52(Suppl 1):S154–60.
France AM, Jackson M, Schrag S, Lynch M, Zimmerman C, Biggerstaff M, Hadler J. Household transmission of 2009 influenza a (H1N1) virus after a school-based outbreak in new York City, April-may 2009. J Infect Dis. 2010;201(7):984–92.
Szucs T. The socio-economic burden of influenza. J Antimicrob Chemother. 1999;44(Suppl B):11–5.
Carrat F, Sahler C, Rogez S, Leruez-Ville M, Freymuth F, Le Gales C, Bungener M, Housset B, Nicolas M, Rouzioux C. Influenza burden of illness: estimates from a national prospective survey of household contacts in France. Arch Intern Med. 2002;162(16):1842–8.
Delabre RM, Lapidus N, Salez N, Mansiaux Y, de Lamballerie X, Carrat F. Risk factors of pandemic influenza a/H1N1 in a prospective household cohort in the general population: results from the CoPanFlu-France cohort. Influenza Other Respir Viruses. 2015;9(1):43–50.
Paolotti D, Carnahan A, Colizza V, Eames K, Edmunds J, Gomes G, Koppeschaar C, Rehn M, Smallenburg R, Turbelin C, et al. Web-based participatory surveillance of infectious diseases: the Influenzanet participatory surveillance experience. Clin Microbiol Infect. 2014;20(1):17–21.
Influenzanet: https://www.influenzanet.eu/ (2013). Accessed 25 Apr 2013.
Guerrisi C, Turbelin C, Blanchon T, Hanslik T, Bonmarin I, Levy-Bruhl D, Perrotta D, Paolotti D, Smallenburg R, Koppeschaar C, et al. Participatory syndromic surveillance of influenza in Europe. J Infect Dis. 2016;214(suppl_4):S386–s392.
Debin M, Turbelin C, Blanchon T, Bonmarin I, Falchi A, Hanslik T, Levy-Bruhl D, Poletto C, Colizza V. Evaluating the feasibility and participants’ representativeness of an online nationwide surveillance system for influenza in France. PLoS One. 2013;8(9):e73675.
Cantarelli P, Debin M, Turbelin C, Poletto C, Blanchon T, Falchi A, Hanslik T, Bonmarin I, Levy-Bruhl D, Micheletti A, et al. The representativeness of a European multi-center network for influenza-like-illness participatory surveillance. BMC Public Health. 2014;14:984.
Guerrisi C, Turbelin C, Souty C, Poletto C, Blanchon T, Hanslik T, Bonmarin I, Levy-Bruhl D, Colizza V. The potential value of crowdsourced surveillance systems in supplementing sentinel influenza networks: the case of France. Euro Surveill. 2018;23:25.
Souty C, Amoros P, Falchi A, et al. Influenza epidemics observed in primary care from 1984 to 2017 in France: A decrease in epidemic size over time. Influenza Other Respi Viruses. 2019;13:148-157. https://doi.org/10.1111/irv.12620.
Adler AJ, Eames KT, Funk S, Edmunds WJ. Incidence and risk factors for influenza-like-illness in the UK: online surveillance using Flusurvey. BMC Infect Dis. 2014;14:232.
Kjelso CGM, Bang H, Ethelberg S, Grove Krause T. Influmenter - an online tool for self-reporting of influenza-like illness in Denmark. Infectious Diseases. 2015;48(4):322–7.
European Commission. Amending decision 2002/253/EC laying down case definitions for reporting communicable diseases to the community network under decision no 2119/98/EC of the European Parliament and of the council. In. Official Journal of the European Union; 2012.
Aguilera JF, Paget WJ, Mosnier A, Heijnen ML, Uphoff H, van der Velden J, Vega T, Watson JM. Heterogeneous case definitions used for the surveillance of influenza in Europe. Eur J Epidemiol. 2003;18(8):751–4.
Yan J, Fine J. Estimating equations for association structures. Stat Med. 2004;23(6):859–74; discussion 875-857,879-880.
Halekoh UHS, Yan Y. The R package geepack for generalized estimating equations. J Stat Softw. 2006;15(2).
World Health Organization: Sex, gender and influenza http://whqlibdoc.who.int/publications/2010/9789241500111_eng.pdf?ua=1 (2010). Accessed 20 Jan 2018.
Wang XL, Yang L, Chan KH, Chan KP, Cao PH, Lau EH, Peiris JS, Wong CM. Age and sex differences in rates of influenza-associated hospitalizations in Hong Kong. Am J Epidemiol. 2015;182(4):335–44.
Klein SL, Hodgson A, Robinson DP. Mechanisms of sex disparities in influenza pathogenesis. J Leukoc Biol. 2012;92(1):67–73.
vom Steeg LG, Klein SL. SeXX matters in infectious disease pathogenesis. PLoS Pathog. 2016;12(2):e1005374.
Troko J, Myles P, Gibson J, Hashim A, Enstone J, Kingdon S, Packham C, Amin S, Hayward A, Nguyen Van-Tam J. Is public transport a risk factor for acute respiratory infection? BMC Infect Dis. 2011;11:16.
van Noort SCC, Koppeschaar C, Van Ranst M, Paolotti D, Gomes G. Ten-year performance of Influenzanet: ILI time series, risks, vaccine effects, and care-seeking behaviour. Epidemics. 2015;13:28–36.
Rolfes Melissa A, Foppa Ivo M, Shikha G, Brendan F, Lynnette B, Singleton James A, Erin B, Daniel J, Olsen Sonja J, Joseph B, et al. Annual estimates of the burden of seasonal influenza in the United States: a tool for strengthening influenza surveillance and preparedness. Influenza Other Respir Viruses. 2018;12(1):132–7.
Santé Canada et l’Agence de santé publique du Canada: La grippe https://www.ctf-fce.ca/Research-Library/Issue2_Article6_FR.pdf Accessed 15 Nov 2018.
Ariza M, Guerrisi C, Souty C, Rossignol L, Turbelin C, Hanslik T, Colizza V, Blanchon T. Healthcare-seeking behaviour in case of influenza-like illness in the French general population and factors associated with a GP consultation: an observational prospective study. BJGP Open. 2017;1:4.
Acknowledgements
We thank all current and former participants and members of the GrippeNet.fr system.
Funding
This work was supported by public funds from Sorbonne Université, Inserm, Santé publique France and the French National Research Agency (ANR). The funding was not specific for the study described in this article. The funder had no role in study design, data collection, data analysis, data interpretation, writing of the report, or in the decision to submit this article for publication. All researchers’ decisions have been entirely independent from funders.
Author information
Authors and Affiliations
Contributions
CG, TB designed and analyzed the results from the prevalence and risk factor analyses. CG, ME, CS, LR, CT, MD, TG, PYB, TH, VC, TB interpreted the results. CG, TB wrote the manuscript. CG, ME, CS, LR, CT, MD, TG, PYB, TH, VC, TB read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The consent procedure was informed and implied through the voluntary and anonymous registration of participants on a dedicated website: https://www.grippenet.fr, to complete a profile survey. Only an email address is required to participate. Information on confidentiality and data security as well as ethics approval are publicly available on the GrippeNet.fr website (https://www.grippenet.fr/fr/grippenet/confidentialite-et-securite-des-donnees/). Even though ethics approval is not required by the French law for epidemiological data collection in the setting of non-interventional biomedical research, GrippeNet.fr was reviewed and approved by the French Advisory Committee for research on information treatment in the field of health (i.e. CCTIRS, authorization 11.565), and by the French National Commission on Informatics and Liberty (i.e. CNIL, authorization DR-2012-024).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional files
Additional file 1:
Socio-demographic, exposure and health characteristics of GrippeNet.fr participants from seasons 2012/13 to 2017/18. This table represents the description of the participants for each of the six seasons studied. (DOCX 26 kb)
Additional file 2:
Factors associated with at least one ILI episode (GNILI-) during six influenza epidemic periods, GrippeNet.fr. This table highlights the factors associated with an ILI episode using a more specific definition. (DOCX 25 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Guerrisi, C., Ecollan, M., Souty, C. et al. Factors associated with influenza-like-illness: a crowdsourced cohort study from 2012/13 to 2017/18. BMC Public Health 19, 879 (2019). https://doi.org/10.1186/s12889-019-7174-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-019-7174-6