Abstract
Background
With an estimated 13,000 newly diagnosed patients per year, nasopharyngeal carcinoma (NPC) is one of the most common types of cancer in males in Indonesia. Moreover, most patients are diagnosed at an advanced stage of the disease. This study aimed to explore the health behaviors of patients diagnosed with NPC and the possible causes of patient delay in NPC diagnosis.
Methods
A qualitative research method was used to gain better insight into patient behaviors. Twelve patients were interviewed using semi-structured interview guidelines. All interviews were recorded, transcribed verbatim and analyzed according to a standard content analysis framework.
Results
Most patients had limited knowledge regarding NPC and its causes. Fifty percent of the patients had a delay of six months from the onset of symptoms to diagnosis. The main reason for this delay was the lack of awareness among the patients, which was influenced by their environment, economic status, family, culture, and religion. The perceived barriers to seeking medical help included direct non-medical costs not covered by health insurance, complex and time-consuming insurance and referral systems, and negative experiences in the past. Health insurance did motivate people to seek medical help.
Conclusion
This study provides additional insight into patients’ motivations to delay seeking medical help and can facilitate the design of NPC education programs. To improve awareness of the abovementioned causes for delay, community-based education programs are highly warranted and should focus on the recognition of NPC symptoms and possible solutions to overcome the main barriers at an earlier disease stage.
Similar content being viewed by others
Background
Cancer mortality is rising in middle- and low-income countries, while increased numbers of cancer survivors can be found in high-income countries [1]. Moreover, a delayed diagnosis of cancer is more often found in middle- and low-income countries due to the limited availability and accessibility of health care. Patients’ ability and willingness to undertake action, which depends on their social-economic status, attitude, financial situation, culture, and religion, also play a role [2,3,4,5]. In addition, patients are often embarrassed to discuss abnormalities [4, 6] or lack trust in medical consultation [7].
Nasopharyngeal carcinoma (NPC), with over 13,000 newly diagnosed patients per year, is one of the most frequently encountered types of cancer in Indonesia, especially in males, and is associated with high mortality [8]. Early symptoms of NPC are nonspecific and mimic a normal upper airway infection, making it a difficult disease to recognize for general practitioners working in primary health care centers. A previous study conducted in Yogyakarta, Indonesia, showed that most patients were diagnosed with an advanced stage of NPC and had a median overall survival of less than 2 years [9].
In Javanese culture, health is seen as a requirement to complete daily activities, and as long as the Javanese are not hindered in their daily activities, they consider themselves to be healthy [5]. Javanese men are the breadwinners of the family and the decision-makers after consulting family members and considering their partner’s opinion. Women, on the other hand, take care of the health of the family [5]. The ability of patients in Indonesia to seek medical help often depends on the role of the family [10, 11]. The importance of the family is reflected in the following proverb: ‘mangan ora mangan waton kumpul’ (even if there is no food to eat, being together is the most important thing) [12].
Delay in diagnosis can occur in the form of patient delay, doctor delay, or system delay. Poor health literacy influences patient behavior and often plays a role in delayed diagnosis and poor treatment outcomes [13, 14]. A systematic review and an integrative review investigated patient delay in patients with head and neck cancer [7] and oral cancer [15]. However, the studies described by Goy et al. focused on the relation between diagnostic delay and stage at diagnosis and did not examine possible explanations for this delay [7]. Additionally, NPC is often excluded in these studies, which mainly report patient delay in high-income countries. To the best of our knowledge, qualitative research exploring health behaviors in patients diagnosed with NPC in Indonesia has not been reported.
Therefore, the aim of this qualitative study was to explore and understand health behaviors and the possible causes of patient delay in the diagnosis of NPC. By better understanding this context and environment, we believe that community-based interventions focused on minimizing patient delay in NPC diagnosis and better treatment outcomes can be efficient.
Methods
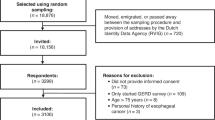
Participants and procedure
Between March 2014 and June 2014, patients newly diagnosed with NPC at the Ear, Nose and Throat Department of Dr. Sardjito Hospital were recruited. The inclusion criteria were age older than 18 years, having histopathologically confirmed NPC, currently waiting for radiotherapy, and understanding and speaking Bahasa Indonesian or Javanese. Patients who had a psychiatric treatment history or were too ill to complete the interview were excluded (one interviewed patient was excluded in retrospect). The Medical and Health Research Ethics Committee of Gadjah Mada University, Yogyakarta, Indonesia approved the study.
Data collection
The in-depth, semi-structured interview design was based on the health belief model (HBM). The failure of individuals to enter interventions that prevent diseases is well-explained by the HBM [16]. The HBM predicts the behavior of individuals based on two variables: the values of the individual and the perception of the individual that an action will result in achieving a particular goal [17]. The HBM consists of the following categories: perceived susceptibility, perceived severity, perceived benefits, perceived barriers, and cues to action [18]. In this study, the HBM may reflect the perception of NPC patients of an NPC diagnosis and the delay in diagnosis of NPC patients. Therefore, this model was chosen to form a conceptual model, which was used as the basis for the development of the sub-questions in our study. Based on the HBM categories, sub-questions and main topics were discussed (AB, RF, FD, and SS) and adapted if needed. Pathway to diagnosis was defined as date from the onset of symptoms until histological proven date of diagnosis.
All eligible patients received a short oral explanation of the study while visiting the outpatient clinic. The anonymity of the respondents was guaranteed, and all patients provided informed consent. Each interview lasted approximately 60 min and was conducted in Bahasa Indonesian or Javanese. To ensure that the patients were at ease, a trained interviewer conducted the interviews at the patients’ homes. Participants were asked about their demographic characteristics, including age, religion, insurance status, level of education, and employment status. These questions were followed by an in-depth, semi-structured interview on topics related to NPC.
Each interview was recorded, transcribed verbatim, translated into English, subsequently reviewed by a bilingual team member (AB), and coded using content analysis using MaxQDA11. Following the emergent design, the coding scheme was jointly developed by FD and SS to decide on new probing questions and the saturation of answers according to theoretical saturation. Saturation was reached after 12 interviews. Participant inclusion ended when no new concepts arose from the last two interviews. The key themes were pre-determined (i.e., perceived susceptibility and severity, perceived benefits and barriers, cues to action, and the influence of culture and religion). All codes derived from the interviews were compiled into categories and merged into the main themes using MAXQDA11. This process was conducted in two steps: after six interviews and at the end of data collection. Inter-coder agreement of 85% was measured over a sample of interviews, and differences were discussed until a consensus was reached. Final coding and categorization were performed by two researchers (RF and AB). Trustworthiness was achieved through different cultural backgrounds within our research team. Having team members with different cultural background ensured that culturally embedded barriers were revealed. Additionally, by interviewing patients in their homes, patients were more likely to be at ease, resulting in less social desirability bias.
Results
Characteristics of the participants
This study was based on data from 12 interviewed NPC patients. For two patients, a relative of the patient participated during the interview because the patient insisted on it. Two-thirds of the patients were male, their mean age was 44 years, and all participants were Muslim and of Javanese origin (Table 1). Six participants had a low educational level. Most patients had insurance for (borderline) lower income individuals. All patients had an advanced stage of disease, and two of them already had distant metastasis at diagnosis. For ten patients, the delay in diagnosis after the first symptoms was more than three months. Most patients visited multiple health care institutions before their appointment at the Ear, Nose and Throat Department of Dr. Sardjito Hospital. One patient even visited eleven different health care institutions.
Perceived susceptibility and severity (quotes 1–9; Table 2)
Most patients (n = 10) had never heard of NPC before their diagnosis or said they had limited, basic knowledge of NPC and its causes (n = 8). When patients were asked about the perceived causes for their illness, they often did not know. However, having cancer frightened the patients, and they wanted to start curative treatment. In addition, they stated that they only received oral information from the doctor directly after diagnosis, and no written information was available. Some patients gathered information on the symptoms and the risk factors through their doctor, family, friends, or the internet. However, not all patients were interested in obtaining knowledge about the disease. Several patients changed their lifestyle (e.g., quit smoking), family lifestyle, and/or food consumption (e.g., not using flavor enhancers like MSG and minimizing the consumption of salty fish).
Most respondents waited several months before seeking medical help, and some did not realize that delaying the diagnosis could worsen the disease. The median delay before seeking medical help was 5.5 months (range 1–12), during which time the respondents observed that their symptoms became more severe. The patients did not recognize the first symptoms of NPC; these symptoms were often considered to be harmless because they did not hinder the patients in their daily activities. The symptoms described by the patients as mild included a ringing sound in the ear, headache, runny nose, nose bleeds, double vision, and symptoms of the common flu. Some patients described the pain or the mass in their neck as mild and not severe, although a neck mass is one of the symptoms of more advanced stages of the disease. When symptoms like a headache and enlarged neck lymph nodes did not disappear over time, it was a trigger to seek medical help. One patient, who described severe pain in the bones, was later diagnosed with distant metastasis.
Perceived benefits and barriers (quotes 10–15; Table 2)
Most patients were unaware of the severity of their disease and mainly expected to get rid of their symptoms as they would a headache. The primary motivation for patients to seek medical help was to get healthy again.
Although many patients mentioned positive experiences with the health care system, all patients shared negative experiences with health care services resulting in a barrier to seeking medical help. Patients often encountered physicians who were unaware of the disease, resulting in misdiagnosis and time-consuming referrals, followed by long queues due to limited treatment capacity. In addition, while waiting, patients often encountered more severe cancer patients, which frightened the patients even more. All of these experiences ultimately formed barriers for the patients to continue visiting health care providers, and they often looked for alternatives.
Medical costs often resulted in patients postponing medical treatment. Although insurance covered most of the costs, patients only started applying for this insurance once the need for medical help was inevitable. Applying for insurance is time consuming, and the insurance does not cover costs like transportation. Frequently, patients had to travel long distances and had to rent a car. In addition, not all patients wanted to use the insurance because they felt that the treatment and service was different when they paid themselves.
Lack of awareness and fear of the side effects of the treatment made patients reluctant to be diagnosed or even start treatment. Experiences in their surroundings (e.g., family or friends) of chemotherapy and radiotherapy scared the patients.
Cues to action (quotes 16–19; Table 2)
Patients stated that if they would have been more aware of the severity of the disease and the need for treatment from the onset of the first symptoms, they would have sought medical help at an earlier stage. Some patients suggested creating community-based awareness using printed media, such as folders and flyers about the symptoms and risk factors of NPC and how changes in lifestyle may minimize the risk of developing NPC. In addition, improving the referral system and queuing system for registration would help patients to overcome these barriers and seek medical help at an earlier time point.
Although transportation costs are still not covered by health insurance and can be seen as a barrier to seeking medical help, the introduction of health insurance did motivate patients to take action. In the past, treatment was unaffordable for some patients, but the introduction of an insurance system has changed this situation.
Culture and religion (quotes 20–25; Table 2)
The participants were strongly bound to Javanese culture and religion, and for that reason, these two aspects were added to the HBM (Fig. 1). Religion and the support of family members to get diagnosed or undergo treatment play a large role in Indonesian culture. In addition, family support is needed to cover possible extra costs. With support from family and friends, most patients start with traditional, complementary, and alternative medicine (TCAM) before seeking medical treatment. The main motivation for using TCAM was to minimize symptoms, as patients were unaware of the underlying disease. Patients often stated that TCAM was easier to obtain and more affordable. However, they also stated that a limited reduction in symptoms was experienced.
Health Believe Model according to Hochbaum, Rosenstock and Kegels [15] with of culture and religion added as modifying factors by the authors
The one-way style of communication of health care providers instead of a partnership communication style, as is present in Indonesian culture, often creates a barrier for the patient. The dominant role of the doctor hinders the patients from asking questions, and patients are too modest to ask for more information or to question the treatment options.
Moreover, all patients in this study were Muslim. Their strong beliefs in God ensured that they accepted the consequences of the disease, resulting in more passive health behaviors.
Discussion
This study addressed the health behaviors of Indonesian patients newly diagnosed with NPC before they received medical treatment. The following factors were found to influence the patients’ health behaviors: environment, economic status, the complex and time-consuming insurance and referral system, lack of awareness, negative experience in the past, family, culture, and religion. Culture-embedded barriers are often difficult to distinguish from one’s own culture. It was a great asset that our research team was multicultural and the phenomena could be examined from different angles. In this way, culturally based barriers were discovered. By adding cultural and religious aspects to the HBM, the model became more representative of the different factors associated with the delay in diagnosis of people experiencing the first symptoms of NPC.
In a Malaysian study by Prasad et al., patients with NPC presented themselves to a doctor within a reasonable time, but for one-third of the patients, it took more than six months to receive a diagnosis [19]. In our study, we specifically looked at the time between the onset of symptoms and the diagnosis instead of the time until the first visit to a doctor. We investigated this time period because all patients except one visited multiple health care providers before being diagnosed at the ENT department at Dr. Sardjito Hospital. We found that for 50 % of the patients, it took more than six months to receive a diagnosis.
Although NPC has a high incidence in Indonesia, participants were not aware of the causes or severity of the disease. This lack of knowledge regarding NPC seemed to influence the stage at diagnosis and the patients’ perceptions of their susceptibly to and the severity of the disease. These findings confirmed that knowledge is a key predictor in patient delay, which is in concordance with other studies of patient delay for breast cancer diagnosis in developing countries [20,21,22,23]. Most participants reported the first symptoms of NPC as harmless and compared them to symptoms of the common flu. As a result, all patients were diagnosed with an advanced stage of the disease accompanied by enlarged lymph nodes in the neck. The misinterpretation of cancer symptoms is a problem that has been reported elsewhere [24, 25]. Additionally, patients were not aware of the consequences of a delay in diagnosis.
The costs of treatment, if not covered by insurance, and the cost of transportation to the hospital caused major treatment-related delays. This finding is in line with other studies that examined treatment outcomes for childhood cancer in Indonesia [26, 27]. Although insurance stimulated patients to seek medical help, patients still struggled with direct non-medical costs.
Indonesian culture often shows hierarchical respect towards people with a higher social status and the elderly, and maintaining harmony between people is seen as important [28]. This respect towards medical staff often leads to unmet information needs and low satisfaction with the provided information. This low satisfaction may lead to unfavorable outcomes, reduced understanding of the illness, and lower health-related quality of life [29,30,31,32].
Limitations
Because theoretical saturation was achieved after 12 interviews, no new patients were included, resulting in a relatively small study population. However, the sample size was adequate because the research scope was narrow, and the study population was homogenous [33]. Thus, one can argue that the sample size was large enough to represent patients diagnosed with NPC in Indonesia. Additionally, we should note that there might have been some recall bias. All patients were diagnosed with an advanced stage of the disease. Although their condition was good enough to participate, one can imagine that it may have been difficult for the patients to remember their onset of symptoms and exact referral path. Often, the recollection of patients was based on a public holiday or other event. However, the level of detail the patients could recall suggested the validity of the interviews. However, for that reason, in the pathway to diagnosis we did not make any further distinguish between the appraisal and help-seeking intervals suggested by others [34,35,36]. In the period from the onset of symptoms and diagnosis also other factors influences the delay e.g. the doctor’s delay and primary care and diagnostic interval [37].
The HBM is a theory used to describe or predict behavior at an individual level. This theory illustrates one’s willingness to act on perceived threats and possible outcome of the actions, based on logical reasoning. We used HBM to understand why an individual suffering from the symptoms of NPC, delays seeking help and still considers the illness as a mild condition with low benefits for early treatment and faces high barriers to seek help. At a later stage in the pathway to diagnosis, the HBM theory is no longer applicable, as the disease has been perceived as life-threatening, not only requiring immediate treatment, but also, requiring more actions from the individual beyond his abilities. Therefore, culture and religion will play a more important role in individuals’ way to handle the problem.
Conclusions
Half of the patients with NPC were diagnosed more than six months after the onset of symptoms, and all patients had an advanced stage of the disease. The main reason for this delay was the lack of awareness of the patients, which was influenced by their environment, economic status, family, culture, and religion. The complex and time-consuming insurance and referral system, negative experiences in the past and direct non-medical costs not covered by health insurance were the greatest barriers to seeking treatment. Improved and varied information services in combination with more effective referrals are important goals to minimize the delay in diagnosis for NPC patients. Community-based education is needed and should focus on the recognition of NPC symptoms and possible solutions to overcome the main barriers at an earlier stage of disease.
Abbreviations
- NPC:
-
Nasopharyngeal carcinoma
- TCAM:
-
Traditional Complementary and Alternative Medicine
References
Jemal A, Center MM, DeSantis C, Ward EM. Global patterns of cancer incidence and mortality rates and trends. Cancer Epidemiol Biomarkers Prev. 2010;19:1893–907.
Freitas AGQ, Weller M. Patient delays and system delays in breast cancer treatment in developed and developing countries. Cien Saude Colet. 2015;20:3177–89. ABRASCO - Associação Brasileira de Saúde Coletiva
Levesque J-F, Harris MF, Russell G. Patient-centred access to health care: conceptualising access at the interface of health systems and populations. Int J Equity Health. 2013;12:1–1.
Siminoff L, Thomson M, Dumenci L. Factors associated with delayed patient appraisal of colorectal cancer symptoms. Psychooncology. 2014;23:981–8.
Dewi FST, Weinehall L, Ohman A. “maintaining balance and harmony”: Javanese perceptions of health and cardiovascular disease. Glob Health Action. 2010;3:4660. doi:10.3402/gha.v3i0.4660.
Öztürk Ç, Fleer J, Hoekstra HJ, JEHM H-W. Delay in diagnosis of testicular cancer; a need for awareness programs. PLoS One. 2015;10:e0141244. Public Library of Science
Goy J, Hall SF, Feldman-Stewart D, Groome PA. Diagnostic delay and disease stage in head and neck cancer: a systematic review. Laryngoscope. 2009;119:889–98. Wiley Subscription Services, Inc., A Wiley Company
Ferlay J, Soerjomataram I, Ervik M, Dikshit R, Eser S. GLOBOCAN 2012 v1. 0, Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 11. 2013, International Agency for Research on Cancer. http://globocan.iarc.fr; 2014.
Wildeman MA, Fles R, Herdini C, Indrasari RS, Vincent AD, Tjokronagoro M, et al. Primary treatment results of nasopharyngeal carcinoma (NPC) in Yogyakarta, Indonesia. PLoS One. 2013;8:e63706.
Effendy C, Vissers K, Tejawinata S, Vernooij-Dassen M, Engels Y. Dealing with symptoms and issues of hospitalized patients with cancer in Indonesia: the role of families, nurses, and physicians. Pain Pract. 2014;15:441–6.
Anggraeni MD, Ekowati W. Family role in the achievement of post radical mastectomy self integrity patients. Int J Public Health Res. 2011;1:163–8.
Subandi MA. Family expressed emotion in a Javanese cultural context. Cult Med Psychiatry. 2011;35:331–46. Springer US
Mancuso L. Overcoming health literacy barriers: a model for action. J Cult Divers. 2011;18:60–5.
Husson O, Mols F, Fransen MP, van de Poll-Franse LV, Ezendam NPM. Low subjective health literacy is associated with adverse health behaviors and worse health-related quality of life among colorectal cancer survivors: results from the profiles registry. Psychooncology. 2014;24:478–86.
Noonan B. European Journal of Oncology nursing. Eur J Oncol Nurs. 2014;18:118–24. Elsevier Ltd
Baum A. Cambridge handbook of psychology, health and medicine. 1997.
Janz NK, Becker MH. The health belief model: a decade later. Health Educ Q. 1984;11:1–47.
Glanz K, Rimer BK, Viswanath K. Health behavior and health education. 4 ed. San Francisco: Jossey-Bass Publisher. 2008. pp. 1–590.
Prasad U, Pua KC. Nasopharyngeal carcinoma: a delay in diagnosis. Med J Malaysia. 2000;2:1–6.
Agarwal G, Ramakant P, Forgach ERS, Rendón JC, Chaparro JM, Basurto CS, et al. Breast cancer care in developing countries. World J Surg. 2009;33:2069–76. Springer-Verlag
Iskandarsyah A, de Klerk C, Suardi DR, Soemitro MP, Sadarjoen SS, Passchier J. Psychosocial and cultural reasons for delay in seeking help and nonadherence to treatment in Indonesian women with breast cancer: a qualitative study. Health Psychol. 2014;33:214–21.
Memon ZA, Shaikh AN, Rizwan S, Sardar MB. Reasons for Patient's delay in diagnosis of breast carcinoma in Pakistan. Asian Pac J Cancer Prev. 2013;14:7409–14.
Taib NA, Yip CH, Low WY. Recognising symptoms of breast cancer as a reason for delayed presentation in Asian women--the psycho-socio-cultural model for breast symptom appraisal: opportunities for intervention. Asian Pac J Cancer Prev. 2011;12:1601–8.
Brouha XDR, Tromp DM, de Leeuw JRJ, Hordijk G-J, Winnubst JAM. Laryngeal cancer patients: analysis of patient delay at different tumor stages. Head Neck. 2005;27:289–95.
Hall N, Birt L, Banks J, Emery J, Mills K, Johnson M, et al. Symptom appraisal and healthcare-seeking for symptoms suggestive of colorectal cancer: a qualitative study. BMJ Open. 2015;5:e008448. British Medical Journal Publishing Group
Mostert S, Gunawan S, Wolters E, van de Ven P, Sitaresmi M, Dongen JV, et al. Socio-economic status plays important roles in childhood cancer treatment outcome in Indonesia. Asian Pac J Cancer Prev. 2012;13:6491–6.
Sitaresmi MN, Mostert S, Schook RM, Sutaryo, AJP V. Treatment refusal and abandonment in childhood acute lymphoblastic leukemia in Indonesia: an analysis of causes and consequences. Psychooncology. 2010;19:361–7. John Wiley & Sons, Ltd
Claramita M, Nugraheni MDF, Van Dalen J, Van der Vleuten C. Doctor–patient communication in Southeast Asia: a different culture? Adv Health Sci Educ. 2012;18:15–31. Springer Netherlands
Davies NJ, Kinman G, Thomas RJ, Bailey T. Information satisfaction in breast and prostate cancer patients: implications for quality of life. Psychooncology. 2008;17:1048–52.
Husson O, Thong MSY, Mols F, Oerlemans S, Kaptein AA, van de Poll-Franse LV. Illness perceptions in cancer survivors: what is the role of information provision? Psychooncology. 2013;22:490–8. John Wiley & Sons, Ltd
Llewellyn CD, Horne R, McGurk M, Weinman J. Development and preliminary validation of a new measure to assess satisfaction with information among head and neck cancer patients: the satisfaction with cancer information profile (SCIP). Head Neck. 2006;28:540–8.
Llewellyn CD, McGurk M, Weinman J. How satisfied are head and neck cancer (HNC) patients with the information they receive pre-treatment? Results from the satisfaction with cancer information profile (SCIP). Oral Oncol. 2006;42:726–34.
Guest G, Bunce A, Johnson L. How many interviews are enough? Field methods, vol. 18. Thousand Oaks: Sage Publications; 2016. p. 59–82.
Scott SE, Walter FM, Webster A, Sutton S, Emery J. The model of pathways to treatment: conceptualization and integration with existing theory. Br J Health Psychol. 2013;18:45–65. Blackwell Publishing Ltd
Walter F, Webster A, Scott S, Emery J. The Andersen model of Total patient delay: a systematic review of its application in cancer diagnosis. J Health Serv Res Policy. 2012;17:110–8. SAGE Publications
Weller D, Vedsted P, Rubin G, Walter FM, Emery J, Scott S, et al. The Aarhus statement: improving design and reporting of studies on early cancer diagnosis. Br J Cancer. 2012;106:1262–7. Nature Publishing Group
Olesen F, Hansen RP, Vedsted P. Delay in diagnosis: the experience in Denmark. Br J Cancer. 2009;101:S5–8. Nature Publishing Group
Acknowledgements
The authors would like to thank all patients who participated in this study.
Funding
This research was supported by the Dutch Cancer Society (KWF 2012-5423).
Availability of data and materials
The datasets of the current study are available from the corresponding author on request.
Authors’ contributions
Conceived and designed the study: RF, S, IBT, SMH, MKS, and FSTD. Coordinated interviews and translation: EW and DR. Analyzed the data: RF, ACRKB, S, and FSTD. Drafted the manuscript: RF and ACRKB. Critically reviewed several drafts of the article: RF, ACRKB, S, IBT, MKS, and FSTD. All authors have read and approved this manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The medical ethical committee of Dr. Sardjito Hospital, Yogyakarta, Indonesia approved this qualitative study. All participants signed informed consent.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Fles, R..., Bos, A.C.R.K., Supriyati et al. The role of Indonesian patients’ health behaviors in delaying the diagnosis of nasopharyngeal carcinoma. BMC Public Health 17, 510 (2017). https://doi.org/10.1186/s12889-017-4429-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-017-4429-y