Abstract
Background
Diabetes is one of the most common chronic illnesses worldwide. This study was to assess whether the incidence risk of type 2 diabetes mellitus between female nurses and female non-nurses.
Methods
Study data were obtained from the Longitudinal Health Insurance Research Database, and nurses were sampled from the Registry for medical personnel. Nurses and non-nurses with similar traits and health conditions were selected via 1:1 propensity score matching. A total of 111,670 subjects were selected (55,835 nurses and 55,835 non-nurses). Stages of diabetes development were monitored until December 31, 2009. The Cox proportional hazards model was used to discuss risks and influencing factors related to diabetes. Poisson distribution methods were used to examine the incidence rate of diabetes per 1,000 person-years.
Results
The propensity matching results show that on average, female nurses who were diagnosed with diabetes were younger compared with the non-nurses (46.98 ± 10.80 vs. 48.31 ± 10.43, p <0.05). However, the results of the Cox proportional hazards model show that the nurses showed a lower risk of developing diabetes compared with the non-nurses (Adj. HR = 0.84, 95 % CI: 0.79–0.90). Factors influencing diabetes development risks among the nurses include advanced age and high Charlson Comorbidity Index levels.
Conclusion
The low degree of diabetes development among the nurses may be attributable to the fact that nurses possess substantial knowledge on health care and on healthy behaviors. The results of this study can be used as a reference to assess occupational risks facing nursing staff, to prevent diabetes development, and to promote health education.
Similar content being viewed by others
Background
Nurses work on the front lines in the medical industry and account for 45.2 % of all professional medical personnel in Taiwan [1]. Numerous medical orders and procedures rely on the work of nurses; therefore, nursing care is highly correlated with care quality levels and with patient treatment outcomes, and nurses play a crucial role in the medical industry.
Ongoing care services are essential to the medical industry. Shift work creates certain occupational problems for nurses [2, 3]. Relevant studies have shown that in addition to causing an increasing number of accidents [4] and higher rates of disease and cancer development [5], engagement in shift work increases one’s likelihood of developing metabolic diseases [6, 7]. Previous studies have revealed that individuals working in occupations that involve shift work show higher risks of developing diabetes compared with those who do not work shifts [8–10].
Diabetes is one of the most common chronic illnesses worldwide. Statistics [11] show that approximately 366 million people worldwide were diagnosed with diabetes in 2011. This number is estimated to increase to 552 million by 2030, accounting for 4.4 % of the global population. In the United States, research has been conducted on the health status of 67,420 nurses from 1976 to 1996, and the results show that 7,401 (11 %) of the nurses were diagnosed with type 2 diabetes mellitus (DM) [12]. Since 2003, diabetes has ranked third among the top 10 causes of death among women in Taiwan [13]. Nurses are exposed to an occupational environment that may be detrimental to their health, which may affect the quality of medical care. The present study compares type 2 DM development risk levels among female nurses to those of the general female citizen population to further identify influencing factors. These data may serve as a foundation for future discussions on occupational health in relation to health promotion, prevention and protection.
Methods
Study design
A retrospective and longitudinal method was adopted in this study, and data were sourced from the National Health Insurance Research Database. To comply with privacy measures, personal information was removed from the collected data.
The Taiwanese government created a compulsory National Health Insurance (NHI) system in 1995, a governmental insurance system that all citizens are mandated to be insured under. Since the end of 2012, the NHI coverage rate reached to as high as 99.85 % [14]. The NHI covers costs for outpatient procedures; emergency procedures; and inpatient prescriptions, treatments, and examinations. The NHI database details all medical claims records for the insured, including treatments for chronic illnesses such as diabetes [15, 16].
Data sources and study participants
Data were sourced from the Longitudinal Health Insurance Research Database of 2000 published by the NHI, which included one million population randomly selected to be representative of whole population in Taiwan and a sample of nurses was selected from the nationwide Registry for Medical Personnel published by the NHI. We used female nurses and female non-nurses as the study participants. Nurses were defined as the nurses were listed in the Registry for Medical Personnel before December 31, 2000. Non-nurses were defined as the participants who had not registered as a licensed medical professional, such as physicians, dentists, physical therapists, nutritionists, and so on before the end of study observation. Participants younger than 20 years and older than 90 years and those diagnosed with type 2 DM prior to December 31, 2000 were excluded. Male nurses were excluded from the study, as most nurses in Taiwan are female (98.92 %) [17]. A total of 374,173 participants were selected, 70,675 of whom were nurses and 303,498 of whom were female non-nurses.
To objectively compare diabetes development risks among female nurses and female non-nurses, 1:1 propensity score matching was used to control for selection bias, and participants with similar characteristics and health conditions were selected from the two groups. After propensity score matching, we assigned 55,835 nurses to the observation group and 55,835 non-nurses to the control group (Table 1). Patterns of diabetes development were monitored until December 31, 2009, covering an average of 9.68 ± 1.06 years (9.72 ± 0.92 and 9.64 ± 1.19 y for nurses and non-nurses, respectively).
Variables description
In this study, the type 2 diabetes mellitus was defined as a primary or secondary diagnosis with ICD-9-CM: 250 or A-code: A181 and the patients had made 3 or more clinic visits or been hospitalized at least once within 365 days [18], and this study excluded other types DM patients. We categorized residence areas into 7 levels, and level 1 was the most urbanized [19]. We used the modified Charlson Comorbidity Index (CCI) to classify the severity of comorbidity [20]. The CCI involved 17 comorbidities weighted based on severity. Higher score denoted greater comorbidity. Presence of catastrophic illnesses was defined as yes or no. The catastrophic illnesses or injuries were defined by National Health Insurance Administration in Taiwan including 30 categories of major illnesses (e.g., cancer, stroke, hemophilia, type I diabetes, autoimmune diseases, end-stage renal disease etc.) for which patients were exempted from copayment and thus avoided financial hardship [21].
Data analysis
A descriptive analysis was conducted to examine demographical traits of the research population (e.g., age, monthly salary, and CCI) and to classify the participants as nurses and non-nurses. Propensity matching (PS) methods were used, and a Chi-square test was subsequently employed to compare variations in diabetes development risks for the two groups. The Cox proportional hazards model was used to discuss relative risks and influencing factors related to diabetes. Hazard ratios (HRs) and 95 % CIs were derived from Cox proportional hazards models. Poisson distribution methods were employed to examine diabetes incidence rates for 1,000 person-years for the two groups. In this study, statistic significance was set at p < 0.05.
Results
Participants demographics
The data prior to propensity matching revealed significant differences (p <0.05) between age, monthly salary, and CCI levels for the two groups (Table 1). Before propensity score matching, the average age of the nurses was 31.23 ± 8.48 years, whereas that of the non-nurses was younger by 10.97 ± 7.00 years at 42.20 ± 15.48 years. Most of the nurses (34.35 %) earned a salary of NT$ 36,301–NT$ 45,800, and the non-nurses earned NT$ 17,281–NT$ 22,800 (44.25 %) on average. The CCI scores for the nurses and non-nurses were 2.93 ± 2.89 and 3.48 ± 3.43, respectively.
After performing the propensity score matching tasks, we did not find any significant differences in terms of age, monthly salaries, residence area urbanization levels, CCI levels, and in other catastrophic illness levels between the two groups (Table 1).
Stratified analysis on the risk of diabetes for the nurses and non-nurses
In the Table 2, the results of the bivariate analysis revealed a lower incidence of diabetes among the nurses (2.68 %) compared with that of the non-nurses (3.13 %), revealing a statistically significant difference (p <0.05). After controlling for other factors, Cox proportional hazards models were used to identify the risk of diabetes for the nurses and non-nurses (Table 3). The results of the nurses showed a lower risk of developing diabetes compared with the non-nurses (Adj. HR = 0.84, 95 % CI: 0.79–0.90). For age, in the 35–44- and 45–54-year age groups, the nurses exhibited a significantly lower risk of diabetes compared with the non-nurses (Adj. HR: 0.82 and 0.75, respectively). For the income groups of less than NT$ 17,280, NT$ 22,801–NT$ 28,800, and NT$ 36,301–NT$ 45,800, nurses presented significantly lower risks of diabetes development compared with those of the non-nurses (Adj. HR: 0.65, 0.77, 0.86, respectively). Regarding urbanization variables, with the exception of participants residing in Levels 4 and 5 urbanization areas, no significant differences in diabetes development risk were found between the nurses and non-nurses (p <0.05). In less urbanized regions, nurses showed lower risks of diabetes development than non-nurses (p <0.05).
An analysis on the comorbidity of other catastrophic illnesses indicated that risks of diabetes development facing those nurses who did not have other catastrophic illnesses were significantly lower than those of non-nurses (Adj. HR: 0.84; p <0.05). While risks of diabetes development among the nurses with catastrophic illnesses were lower than those for the non-nurses, the results were non-significant (p <0.05). The results of the CCI analysis show that the nurses presented significantly lower susceptibility to diabetes development overall compared with the non-nurses (p <0.05).
Relative factors and the incidence of diabetes among nurses
The analysis results presented in Table 4 show that age and CCI serves as critical factors that influence diabetes development risks among nurses. Regarding age variables, a 10-year period was used as an interval to create age groups. The older nurses presented relatively higher risks of diabetes development compared with the nurses of less than 25 years (Adj. HR: 1.56–16.85). Nurses who were older than 65 years of age showed a 16.85-fold higher risk of developing diabetes compared with nurses who were younger than 25 years of age (95 % CI: 11.47–24.75).
CCI significantly influences diabetes development risks among nurses. The analysis results indicate that those nurses with a higher CCI were at a higher risk of developing diabetes than the reference group (CCI = 0). Those nurses with a CCI of ≧10 presented 28.48-fold higher relative risks of diabetes development than the reference group (95 % CI: 15.51–52.29). The research results shown in Table 5 indicate that diabetes incidence rates per 1,000 person-years for the nurses were lower than those of the non-nurses (2.76 ‰ vs. 3.25 ‰). The analysis results on the various variables reveal that with the exception of the ≦25-year age group, the incidence rate of diabetes per 1,000 person-years for nurses of all of the age groups was lower than that of the non-nurses.
Discussion
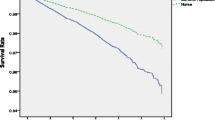
After the research population was collected from the NHI database, 1:1 propensity score matching was employed. The results of the bivariate analysis shown in Table 2 indicate that the nurses presented a lower risk of diabetes development than the non-nurses (2.68 % vs. 3.13 %), which is consistent with that of the Cox proportional hazards model (Table 3 and Fig. 1; Adj. HR: 0.83, 95 % CI: 0.78–0.89).
Previous studies [8–10] have determined that individuals who work in professions that require shift work present higher risks of developing diabetes. After propensity score matching, our nurses cohort and non-nurses control group were similar in terms of demographics, socioeconomic status, and health conditions. However, the nurses showed lower risks of developing diabetes than the non-nurses, and this may be attributed to nurses’ medical knowledge and educational training. Furthermore, nurses are assume health promotion and education responsibilities [22] and are thus likely to live healthy lifestyles and to invest in their long-term health. This phenomenon is known as the healthy worker effect [23, 24]. Nurses must be in excellent health to achieve effective performance; therefore, nurses are generally healthier than non-nurses.
The aforementioned results may be correlated with knowledge, attitudes, and practice (KAP) theory principles [25, 26]. Self-care levels depend on patient behaviors, and a patient’s knowledge influences his or her attitudes, thereby affecting his or her practices. Acquiring correct knowledge about a disease and adopting positive and proactive attitudes are essential for motivating self-care behaviors, which directly or indirectly affect health outcomes. Nurses are equipped with comprehensive medical knowledge and thus possess a favorable view of personal health and diseases and a positive attitude toward medical care, resulting in superior self-care [27]. However, further study is needed to examine the effect of KAP theory on the nurses’ incidence risk of developing diabetes.
The results presented in Tables 3 and 4 show that for the entire sample population, age and CCI variables most heavily influenced diabetes development risks. The older participants presented higher risks of diabetes development than the reference group (<25 y), complementing the results of previous studies [28–30], and this shows that glucose tolerance levels decrease with age; therefore, diabetes development risks increase rapidly among individuals who are older than 45 years of age. As shown in Table 5, a rapid increase in the incidence rate of diabetes per 1,000 person-years was observed among both nurses and non-nurses of 45 years of age and older. As shown in Tables 3 and 4, a higher CCI involves an increased relative risk of diabetes development, complementing the results of Huang [31] and Monami et al. [32]. Thus, CCI serves as a critical variable for predicting diabetes development risks.
Study limitations
There are several limitations to our analyses. According to the International Statistical Classification of Diseases (ICD), DM diagnosis is based on an ICD-9 diagnosis code. Therefore, clinical diagnostic data could not be acquired and verified. To optimize the accuracy of this study while compensating for this limitation, diabetes occurrence was identified when patients visited an outpatient department three times or when they were hospitalized more than once within 365 days of receiving a primary or secondary diabetes diagnosis (ICD-9-CM: 250 or A-code: A181) [17]. Some risk factors are not present in analysis. For instance, information on lifestyle, health behaviors and clinical testing data were not available and thus could not be used in variable analyses. So, we used the propensity score matching to control for selection bias. The propensity score adjustment is an important statistical technique to reduce the bias from confounding variables in observational studies and mimic the results of a randomized controlled trial [33]. In addition, the long follow-up and national design provided adequate power.
Conclusion
This study is the first to use a nationwide database to compare risks of diabetes development among female nurses and female non-nurses. The results show that nurses present a lower risk of developing diabetes than non-nurses. This result may be attributable to the fact that nurses possess superior medical knowledge and thus have lower incidence risk of developing diabetes.
Abbreviations
CCI, Charlson Comorbidity Index; CI, confidence interval; DM, diabetes mellitus; HR, hazard ratio; ICD, International Statistical Classification of Diseases; KAP, knowledge, attitudes, and practice; NHI, National Health Insurance; NT$, New Taiwan Dollar; PS, propensity score.
References
National Statistic , R.O.C (Taiwan). Health, Medical Facilities and Medical Personnel. 2013. http://eng.stat.gov.tw/mp.asp?mp=5. Accessed 20 May 2015.
Triolo P. Occupational health hazards of hospital staff nurses. Part I: Overview and psychosocial stressors. AAOHN J. 1989;37(6):232–7.
Triolo P. Occupational health hazards of hospital staff nurses. Part II: Physical, chemical, and biological stressors. AAOHN J. 1989;37(7):274–9.
Plaimee P, Mititraporn R, Nuangjumnong W, Johns NP, Johns J. Comparison of Melatonin Levels, Sleep Quality and Alertness between Nurses Working Night Shift and Day Shift. Srinagarind Med J. 2013;27(4):393–400.
Schernhammer ES, Feskanich D, Liang G, Han J. Rotating night-shift work and lung cancer risk among female nurses in the United States. Am J Epidemiol. 2013;178(9):1434–41.
Sookoian S, Gemma C, Fernandez Gianotti T, Burgueno A, Alvarez A, Gonzalez C, Pirola C. Effects of rotating shift work on biomarkers of metabolic syndrome and inflammation. J Intern Med. 2007;261(3):285–92.
Esquirol Y, Bongard V, Mabile L, Jonnier B, Soulat J-M, Perret B. Shift work and metabolic syndrome: respective impacts of job strain, physical activity, and dietary rhythms. Chronobiol Int. 2009;26(3):544–59.
Pan A, Schernhammer ES, Sun Q, Hu FB. Rotating night shift work and risk of type 2 diabetes: two prospective cohort studies in women. PLoS Med. 2011;8(12):e1001141.
Karlsson B, Knutsson A, Lindahl B. Is there an association between shift work and having a metabolic syndrome? Results from a population based study of 27 485 people. Occup Environ Med. 2001;58(11):747–52.
Suwazono Y, Sakata K, Okubo Y, Harada H, Oishi M, Kobayashi E, Uetani M, Kido T, Nogawa K. Long-term longitudinal study on the relationship between alternating shift work and the onset of diabetes mellitus in male Japanese workers. J Occup Environ Med. 2006;48(5):455–61.
Whiting DR, Guariguata L, Weil C, Shaw J. IDF diabetes atlas: global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract. 2011;94(3):311–21.
Al-Delaimy WK, Willett WC, Manson JE, Speizer FE, Hu FB. Smoking and Mortality Among Women With Type 2 Diabetes The Nurses’ Health Study cohort. Diabetes Care. 2001;24(12):2043–8.
Ministry of Health and Welfare. 2012 statistics of causes of death. 2014. http://www.mohw.gov.tw/EN/Ministry/Statistic. Accessed 31 Dec 2015.
National Health insurance Administration, Ministry of Health and Welfare. Statistics & Surveys. 2013. http://www.nhi.gov.tw. Accessed 13 May 2015.
Cheng T-M. Taiwan’s new national health insurance program: genesis and experience so far. Health Aff. 2003;22(3):61–76.
Lu J-FR, Hsiao WC. Does universal health insurance make health care unaffordable? Lessons from Taiwan. Health Aff. 2003;22(3):77–88.
Hsu Y, Tang W, Chang Y, Maa S. [A preliminary study of the work values of male nurses in Taiwan and related factors]. Hu Li Za Zhi. 2013;60(2):50–60.
Chang C, Shau W, Jiang Y, Li H, Chang T, H‐H Sheu W, Kwok C, Ho L, Chuang L. Type 2 diabetes prevalence and incidence among adults in Taiwan during 1999–2004: a national health insurance data set study. Diabet Med. 2010;27(6):636–43.
Liu C-Y, Hung Y, Chuang Y, Chen Y, Weng W, Liu J, Liang K. Incorporating development stratification of Taiwan townships into sampling design of large scale health interview survey. J Health Manag. 2006;4(1):1–22.
Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613–9.
National Health insurance Administration, Ministry of Health and Welfare. Reglations governing the exemption of the national heaelth insurance beneficiaries from co-payment. 2015. http://www.nhi.gov.tw. Accessed 20 Apr 2016.
Carpenter, H. Nurses. Role models, advocates and educators of health, safety, and wellness. Paper presented at the 141st APHA Annual Meeting (November 2-November 6, 2013). Boston.
Naimi AI, Richardson DB, Cole SR. Causal Inference in Occupational Epidemiology: Accounting for the Healthy Worker Effect by Using Structural Nested Models.American journal of epidemiology. 2013. doi:10.1093/aje/kwt215.
Radon K, Goldberg M, Becklake M. Healthy worker effect in cohort studies on chronic bronchitis. Scand J Work Environ Health. 2002;28(5):328–32.
Bhargava A, Mishra B, Thakur A, Dogra V, Loomba P, Gupta S. Assessment of knowledge, attitude and practices among healthcare workers in a tertiary care hospital on needle stick injury. Int J Health Care Qual Assur. 2013;26(6):549–58.
Tobin EA, Okojie P-W, Isah EC. Community knowledge and attitude to pulmonary tuberculosis in rural Edo state, Nigeria. Ann Afr Med. 2013;12(3):148.
Andersen R, Newman JF. Societal and individual determinants of medical care utilization in the United States. Milbank Q. 2005;83(4). doi:10.1111/j.1468-0009.2005.00428.x.
Campbell AJ, Busby WJ, Horwath CC, Robertson MC. Relation of age, exercise, anthropometric measurements, and diet with glucose and insulin levels in a population aged 70 years and over. Am J Epidemiol. 1993;138(9):688–96.
Mizuno S, Nakai Y, Isayama H, Yanai A, Takahara N, Miyabayashi K, Yamamoto K, Kawakubo K, Mohri D, Kogure H. Risk factors and early signs of pancreatic cancer in diabetes: screening strategy based on diabetes onset age. J Gastroenterol. 2013;48(2):238–46.
International Diabetes Federation. About diabetes. Risk factors. 2014. http://www.idf.org. Accessed 2 Jan 2015.
Huang Y-Q, Gou R, Diao Y-S, Yin Q-H, Fan W-X, Liang Y-P, Chen Y, Wu M, Zang L, Li L. Charlson comorbidity index helps predict the risk of mortality for patients with type 2 diabetic nephropathy. Science B. 2014;15(1):58–66.
Monami M, Vitale V, Lamanna C, Bartoli N, Martelli D, Zannoni S, Antenore A, Toffanello G, Marchionni N, Mannucci E. HbA1c levels and all-cause mortality in type 2 diabetic patients: Epidemiological evidence of the need for personalised therapeutic targets. Nutr Metab Cardiovasc Dis. 2013;23(4):300–6.
Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivar Behav Res. 2011;46(3):399–424.
Acknowledgments
We are grateful for use of the National Health Insurance Research Database provided by the National Health Research Institutes. The interpretations and conclusions contained herein do not represent those of the Ministry of Health and Welfare, Taiwan, R.O.C.
Funding
This study was supported by the grant (CMU102-ASIA-12) from China Medical University and Asia University as well as the grant (DOH 10216) from Ministry of Health and Welfare.
Availability of data and materials
Data are available from the National Health Research Institutes (NHRI), Taiwan. All interested researchers can obtain the databases published and managed by the NHRI. All researchers are allowed to use the databases for their studies if they are interested in using the data. Before using the databases for research, all studies should get the IRB permission.
Authors’ contributions
HLH and WCT drafted the manuscript. WCT and PTK designed the study. CCP, SMW, PTK and WYC collected data. HLH, PTK and WCT were responsible for study conceptualization and developing the analytical plan. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics statement
The institutional review board of China Medical University approved this study (IRB No.: CMUH 20130326C).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Huang, HL., Pan, CC., Wang, SM. et al. The incidence risk of type 2 diabetes mellitus in female nurses: a nationwide matched cohort study. BMC Public Health 16, 443 (2016). https://doi.org/10.1186/s12889-016-3113-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-016-3113-y