Abstract
Background
Over the past decades research has shown that employment has a positive impact on quality of life, global functioning and recovery in individuals with schizophrenia. However, access to vocational rehabilitation services for this group is limited and unemployment rates remain high. In this study we explore the potential cost-effectiveness of a novel vocational rehabilitation program (The Job Management Program – JUMP) earmarked for individuals with schizophrenia in Norway.
Methods
The JUMP study was a vocational rehabilitation program augmented with either cognitive behaviour therapy or cognitive remediation. In addition to the JUMP protocol, we extracted treatment cost data from comprehensive and mandatory health and welfare registers. The costs over a two-year follow-up period were compared with the costs over the two-year period prior to inclusion in the study. We also compared the cost-effectiveness of JUMP with a treatment as usual group (TAU).
Results
We identified significant reductions in inpatient services in the JUMP group, both for those who obtained employment and those who did not. Significant reductions were also found in the TAU group, but adjusted for baseline differences the total cost for JUMP participants were € 10,621 lower than in the TAU group during the follow-up period.
Conclusion
In addition to supporting individuals with schizophrenia obtain employment, JUMP appears to have reduced the reliance on mental health services, which should be of interest to stakeholders.
Trial registration
ClinicalTrials.gov Identifier: NCT01139502. Retrospectively registered on 6 February 2010.
Similar content being viewed by others
Background
Employment is associated with improved quality of life and global functioning, and is an important part of recovery for individuals with schizophrenia [1,2,3,4]. Nevertheless, unemployment rates remain high [5, 6], and in Norway only 10% of the population with schizophrenia is employed [7]. This rate is stable across age groups, and the transition rate from disability benefits into employment is close to zero [8].
Supported employment programs have proven superior compared to sheltered workshops or day service programs in supporting individuals with severe mental illnesses attain competitive employment [9,10,11,12,13]. Benefits of employment include social integration, increased quality of life, higher self-esteem, and improved global functioning [4, 14,15,16]. A few cost-effectiveness analyses have also been undertaken showing a favourable effect of supported employment in terms of increased employment rates and reduced health service costs [10, 17,18,19]. However, due to large variations in costs of health and welfare services and income levels between countries it is difficult to generalise these results [20]. Thus, before implementation can be recommended, the cost-effectiveness of an intervention needs to be evaluated in its intended setting.
Vocational rehabilitation (VR) services in Norway are primarily provided by enterprises that offer both sheltered work and supported employment. These services are funded through the Norwegian Labour and Welfare Administration (NAV) and are typically combined with welfare schemes such as NAV paying the individuals’ salary for extended periods, or work placement with no salary beyond disability benefits [16, 21]. This practice has been described as the “benefit trap” [8], and is likely contributing to the high unemployment among individuals with schizophrenia in Norway [7, 8, 21]. Due to the ineffectiveness and limited access to these services for individuals with schizophrenia spectrum disorders, the Job Management Program (JUMP) was established as a VR program for this group with the primary aim of supporting participants obtain competitive employment. A secondary aim was to explore the effect of augmenting VR with cognitive behaviour therapy (CBT) or cognitive remediation (CR). At two-year follow-up 21.2% of the participants in the JUMP study had obtained competitive employment. A further 25.3% had work placements in competitive workplaces, and an additional 13.7% had sheltered work. Both intervention groups (CR and CBT) improved on global functioning, self-esteem, neurocognitive functioning and depression during the follow-up period [16, 22, 23].
Aims
The objective of the current study was to explore the potential cost-effectiveness of the JUMP intervention compared to a treatment as usual (TAU) group in terms of mental health service costs and effectiveness.
Methods
The JUMP study
The JUMP study was a multi-site VR program for adults with schizophrenia spectrum disorders conducted in six Norwegian counties. The program provided 10 months of standard VR services in competitive or sheltered workplaces, which involved assessments, writing job applications, and preparing for interviews. When required, participants also practiced skills, and had job tasks adapted to accommodate for difficulties at the workplace. In addition to the standard VR services the JUMP protocol included three add-ons: (1) there was a formalised collaboration between VR enterprises, NAV and the mental health services to ensure coordinated and ongoing support; (2) participants, collaborators, and in some cases employers received psychoeducation on common elements associated with schizophrenia spectrum disorders; and (3) either CR or use of CBT techniques provided by trained employment specialists twice a week for a 6 month period. Three counties were randomised to CR and three to CBT. Participants were given the intervention provided in their catchment area [16, 22, 24].
Participants
Participants were recruited from within the mental health services, NAV, and through self-referral in the six counties that were involved in the JUMP study. All participants provided written informed consent. Inclusion criteria were: age between 18 and 65; a diagnosis within the broad schizophrenia spectrum disorders (schizophrenia, schizoaffective disorder, psychotic disorder not otherwise specified and delusional disorder) [25]; sufficient understanding of the Norwegian language; and an IQ above 70. Individuals with neurological disorders, head trauma with more than ten minutes of unconsciousness, and medical conditions that interfered with cognitive function were excluded from the study. Also, individuals who displayed high risk of violent behaviour or severe suicidal ideation, and individuals with ongoing alcohol or substance abuse were not permitted to participate [16, 22, 26,27,28,29].
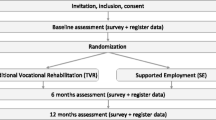
A total of 148 participants were included in the JUMP study between August 2009 and March 2012, 84 and 64 respectively allocated to the CBT and CR interventions [16, 28] (Fig. 1).
Economic evaluation
The economic evaluation was carried out from the perspective of the health and social care system. This included calculating the cost of mental health services, community care services, social security services, medications and primary health care services, in addition to the costs of the CR and CBT interventions. In accordance with the Norwegian Directorate of Health’s guidelines for economic evaluations in the health sector [30], the number of months employed were converted into quality adjusted life years (QALYs) and served as the measure of effectiveness for the cost-effectiveness analysis. Costs were summarised for two 24-month periods: T0 = the last 2 years prior to inclusion in the study and T1 = from inclusion in the study to two-year follow-up. Intervention costs were included in T1.
We examined the intervention costs and health- and welfare costs for T0 and T1. The mental health service costs in the JUMP group were compared to a control group that received treatment as usual (TAU). Effectiveness was measured in terms of QALYs gained during T1 as compared to T0.
Data sources
Data on services and costs were obtained from comprehensive health and welfare registers: The Norwegian Patient Register (NPR); The Norwegian Prescription Database (NorPD); The Norwegian Health Economics Administration (HELFO); The Individual-based Register of Care Services (IPLOS); and The Norwegian Labour and Welfare Administration’s (NAV) registers on social security benefits, sick leave payments, disability benefits, and competitive employment. The registers are described in detail elsewhere [7]. All data were collected based on the participants’ unique personal identification number. The cost-effectiveness analyses were not part of the original design of the JUMP study, thus a separate consent for extraction of register data after completion of the program was required. Participants were contacted during July – September 2014.
Intervention costs
The intervention costs included costs of employment specialists, a coordinator from the mental health services at each of the six sites, and overhead costs. Each participant was allocated 6 h of the employment specialists’ time per week, including 2 h of CR or CBT in addition to VR services and collaboration with other involved parties.
Treatment as usual
The TAU group was drawn from the NPR. Upon approval of extracting data from the NPR, all JUMP participants (n = 148) were excluded from the draw based on personal identification numbers. Statisticians at the NPR drew a random sample of 100 individuals with a primary diagnosis of schizophrenia that was matched with the JUMP group on age and sex categories (Table 2). The data were annualised for the period 2010–2012. Only individuals in active treatment in the specialised mental health services (Hospitals, Community Mental Health Centres, and private Psychiatrists and Psychologists with a provider licence) are included in the NPR.
Currency conversions
All costs were converted to 2015 Norwegian Kroner (NOK) based on the average consumer price index [31]. Costs are reported in €. For currency conversions we used The Central Bank of Norway’s average annual exchange rate for 2015 (8.95 NOK = 1 €) [32].
Employment data
Employment status for JUMP participants was recorded weekly by employment specialists during the intervention period. Employment status between the end of the intervention period and two-year follow-up were obtained through interviews with the participants and confirmed against NAV’s employee register. Baseline (T0) employment data were obtained through NAV’s employee register. No employment data was available for the TAU group as we did not have approval to merge the NPR with the employment register for this sample. Thus we assumed a stable employment rate of 10.2% for this group based on the national employment rate identified for individuals with schizophrenia in past studies using data from 2012 [7, 8, 33,34,35].
Quality adjusted life years
Cost-effectiveness studies commonly use quality-adjusted life-years (QALYs) as a generic outcome measure [36]. QALYs are estimated on the bases of health related quality of life measures. Quality of life measures were not part of the JUMP protocol, thus QALYs were calculated by multiplying months of employment and unemployment with quality of life tariff scores associated with paid employment (0.87) and unemployment (0.79) from the Schizophrenia Health Outcomes (SOHO) study [2]. These scores were based on EuroQol-5D (EQ-5D) scores in individuals who had received 3 years of continuous treatment for schizophrenia. Paid employment was defined as part-time or full-time employment in competitive workplaces. Twenty-one (30.4%) of the JUMP participants (n = 69) had paid employment during the two-year follow-up period, and sixteen (23.2%) were employed at the time of the two-year follow-up.
Analyses
IBM SPSS Statistics version 21.0 [37] and Stata version 13.1 [38] were used for statistical analyses. All tests were two-tailed with a significance level of 5%. In order to examine group differences, baseline comparisons were conducted with Bootstrap Students t-tests or Chi-square tests. Generalized Linear models (GLM) with gamma family and identity link with baseline costs as a covariate were used to compare costs between groups during the two-year follow-up period. Cost data are often skewed as they are always > 0 and the variance is likely to increase with higher expected costs, and thus violate normality assumptions. The GLM approach provides robust estimates of the mean by accommodating for skewness in the data via 3 components: the random component (cost); the systematic component (treatment group); and the link function (relationship between the random and systematic components). In the gamma family the variance of cost is assumed to be proportional to the square of the mean, which gives a better fit than the normal distribution [39, 40]. To adjust for potential bias due to the lack of randomisation, we performed propensity score adjustments with age, sex, and baseline day treatment, inpatient and outpatient care as potential bias variables. The propensity score was included as a covariate in the GLM. In health economic evaluations, it is recommended to perform probabilistic sensitivity analysis to assess the uncertainty of the resulting cost-effectiveness. We performed probabilistic sensitivity analysis on resulting costs and effects and combined these to provide an estimate of the probability of JUMP being cost-effective compared to TAU.
Results
Baseline analysis
Sixty-nine (46.6%) participants from the JUMP study consented to extraction of register data for this study. There were no significant differences between those who consented and those who declined on key variables (diagnosis, age, sex, units of DDD of antipsychotic medication, psychotic symptoms, education, previous work experience, employment outcome (Table 1) at two-year follow-up, thus we assume the results are fairly representative for the participants in the JUMP study.
All JUMP participants had primary diagnoses in the schizophrenia spectrum (87% schizophrenia) while subjects in the TAU group had schizophrenia as their primary diagnosis. There were no significant differences in sex or age (Table 2).
Costs and service utilization
The mean cost of the JUMP intervention was € 9131 (SD 2123) per participant. The mean duration of the intervention was 26.52 weeks (SD 5.89).
There were significant reductions in inpatient services from T0 to T1 for both the JUMP participants (mean = € -90,944; 95CI -137,781, − 46,165; p < .012) and the TAU group (mean = € -78,116; 95% CI -126,941, − 33,275; p = .010). Combining inpatient and outpatient costs gives a mean reduction of € 87,809 in the JUMP group and € 76,386 in the TAU group (median: € -1335 and € 13,263 respectively). The reduction in the JUMP group was significant both for those who gained paid employment (n = 21; mean = € -80,776; 95% CI -140,112, − 21,467; p = .010) and for those who had work placement or sheltered work (n = 42; mean = € -90,885; 95% CI -153,873, − 27,897; p = .006). No significant changes were found for other health or welfare costs. Mean and median costs for each 24 - month period; T0 and T1 (inclusive of intervention costs) are detailed in Table 3.
In terms of utilisation of mental health services, the JUMP group had significantly more outpatient visits during both T0 and T1 compared to TAU. At T1 the JUMP group had significantly fewer days of hospitalisation than the TAU group (Table 4). Bootstrap paired samples t-tests revealed significant reductions in inpatient days for both JUMP (mean − 63.0; 95% CI -96.2, − 33.3; p = .006) and for TAU (mean − 53.8; 95% CI -87.5, − 23.1; p = .004). We found no significant differences in change scores between JUMP and TAU through bootstrap independent samples t-test (mean 9.2; 95% CI -39.9, 58.5; p = .71).
We performed a generalized linear regression with costs at T0, group (JUMP/TAU) and the propensity score as covariates using gamma family and identity link to examine group differences in total costs at T1 (Table 5). We tested the assumptions with a linktest which was non-significant, indicating that the assumptions are reasonable. Total mean costs for the JUMP group (inclusive of intervention costs and adjusted for baseline differences) were € 10,621 lower than for TAU (95% CI: -29,979, 8735; p = .282). Costs at T0 was a significant predictor of costs at T1 (Table 5).
Cost-effectiveness
When assessing whether a program is cost-effective it is useful to use the cost-effectiveness plane (Fig. 2). If the mean value of the new program is more effective and less costly than the reference program, it is cost-effective and is typically denoted as a dominant strategy. Likewise, if the new program is less effective and more costly it is dominated [41]. New programs in the two other quadrants of the plane are evaluated against a cost-effectiveness threshold value suggested by the Norwegian Directorate of Health which is € 62,000 per QALY gained [42].
The cost-effectiveness plane [48]
In terms of exploring the cost effectiveness of an intervention the effect is usually estimated as a general measure of gained health related quality of life from the new intervention compared to existing treatment, which is converted into quality adjusted life years (QALY).
The mean months of competitive employment in the JUMP group were 3.10 (N = 69, SD 7.27) at T0 and 4.30 (N = 69, SD 7.33) at T1 with corresponding QALYs being .8003 (SD .024) at T0 and .8043 (SD .024) at T1. Thus the incremental QALYs for competitive employment were .004 (SD .026; 95%CI −.002, .010) in the JUMP group, while we assumed a stable 10.2% employment rate in the TAU group.
Dividing the aggregate difference in average specialised mental health service costs (€ 10,621) by the aggregated improvement in QALYs yields a negative incremental cost-effectiveness ratio, which places the JUMP group in the bottom right quadrant of the cost-effectiveness plane (more effective and less costly) (Fig. 2). Although the difference is not significant there is a trend towards the JUMP program being more cost-effective. This is also the case if using incremental months of work as the effect measure. JUMP generated more months of employment than TAU at a lower cost. Probabilistic analyses indicate an 85% probability that JUMP is cost-effective compared to TAU.
Discussion
This study found reduced mental health service costs during a novel vocational rehabilitation program (JUMP) for individuals with schizophrenia spectrum disorders in Norway. Compared to a TAU group the mean mental health costs, adjusted for baseline differences (T0), were € 10,621 lower in the JUMP group (inclusive of intervention costs) during the two-year follow-up period (T1). Due to skewed data we also provided median costs for specialised mental health services. The median costs for the JUMP group reduced slightly from T0 to T1, while the median cost for the TAU group increased by € 13,261. This is further evidence in favour of the JUMP intervention [43]. A large mean reduction in mental health service use was also identified in the TAU group. One potential explanation for this reduction may be that only patients in active treatment within the specialised mental health services are registered in the NPR. Hence, the reduced reliance on mental health services in the TAU group is likely an effect of therapeutic interventions beyond our control. The service use variation was also greater in the TAU group with the median group difference being greater than the mean.
We also found that competitive employment during 24 months in the JUMP group increased from a mean 3.1 months at T0 to 4.3 months at T1. When including all types of employment the mean months of employment at T1 was 15.14 months. The assumed duration of competitive employment in the TAU group (based on previous studies [7, 8, 33,34,35]) was 2.35 months. The incremental QALYs related to competitive employment were .006 higher in the JUMP group than the TAU group at T1. Despite the costly intervention, mental health service costs were reduced in the JUMP group and there was an increased effect measured in both QALYs and months worked.
The cost reductions in the current study were driven by a large reduction in inpatient care at T1. Similar reduced reliance on inpatient care for individuals who gain employment have also been documented in other studies [44,45,46]. A commonly used argument for such results is that work in itself facilitates symptom improvement and enhanced self-esteem [4, 14, 15, 46], which in turn is likely to reduce hospitalisations. This is probably one of several factors in play, and some studies have displayed somewhat different results. In a study comparing supported employment with traditional VR across six European cities, Knapp and colleagues found that participants in the supported employment group utilised significantly less inpatient services than participants in the traditional VR group during the first 12 months of the study, while there was no difference during the six months thereafter [19]. In contrast, the current study found the reliance of inpatient care to remain significantly lower than in the TAU group throughout the 24 - month follow-up period. In a recent study comparing supported employment to traditional VR in Norway, Reme and colleagues found that supported employment did not have a significant effect on inpatient care [47]. Notably this study had broader inclusion criteria, thus the results are not directly comparable.
An interesting point when comparing the current study with supported employment studies is that we found no significant differences between those who gained competitive employment and those who had work placements or sheltered work in terms of reliance on mental health services. This is important as it indicates that vocational rehabilitation programs for individuals with schizophrenia can have positive health effects even when employing a broader definition of work than is normally the case in supported employment studies.
The reasons for the reduced inpatient care in the current study are likely multifaceted. One explanation may be that JUMP participants increased the use of outpatient mental health services, which probably contributed to fewer hospitalisations. Another important factor could be the close follow-up and two weekly CBT or CR sessions the participants received from the trained employment specialists. In addition to perhaps being therapeutic in itself, the close follow-up enabled the employment specialists to intervene, either directly or by alerting clinicians, if they observed signs of symptom increase.
Past cost-effectiveness studies have primarily examined programs where competitive employment has been the only employment outcome measured. Although competitive employment was the ultimate aim of the JUMP study, work placements and sheltered work were also considered a success in accordance with the Scandinavian model of vocational rehabilitation. It should be noted that the use of work placements and sheltered work was an important factor that enabled 77% of the participants in the JUMP study to maintain their job during the ten-month intervention period [22].
Apart from the reduction in mental health service costs all costs except social security remained stable between T0 and T1. We believe the change was primarily due to participants having their entitlements revised upon inclusion in the project. Consequently, many were shifted from a disability pension to a work assessment allowance, which provided them with a higher benefit. At two-year follow-up 16.4% of all JUMP participants had transitioned from disability benefits to paid employment as their primary source of income. Any long-term effect on social security costs will be explored in the forthcoming five-year follow-up of the JUMP study.
Strengths and weaknesses
A major strength of this study was the use of comprehensive and compulsory health- and welfare registers, which provided detailed records of participants’ societal costs over a period of four years. The main limitation of the study is the lack of a randomised control group. Due to recruitment problems we were forced to abandon the original design of including a control group and thus drew a TAU group from the NPR for this study. Although the TAU group consisted of a random selection, there were large mean differences in resource utilisation between the TAU and JUMP groups at baseline. This may indicate that there were clinical differences between the two groups but as we do not have any clinical information about the TAU group, we are unable to determine if such differences were, in fact, present. By controlling for baseline differences, the effect of this difference is likely to have been reduced. Due to the lack of a control group receiving VR only, we were unable to disentangle the effects of the CR and CBT interventions. Also, no direct measure of health related quality of life was included in the design of the study; hence tariff scores from the literature were used. Although this method is commonly used in health economic evaluations where measures of health-related quality of life are not available, the validity of this estimation should be interpreted with caution as health related quality of life can be influenced by a number of factors [20]. The lack of employment and quality of life data for the control group is also a limitation that affects the validity of the results. Another limitation is that less than half of the participants in the JUMP study consented to extraction of register data. There were, however no significant differences on key variables between those who consented and those who did not. Finally, the high intervention costs of the JUMP study as well as Norway’s high treatment costs and strong welfare system affect the generalisability of our results.
Conclusion
The current study identified non-significant cost reductions and improvements in QALYs among JUMP participants compared to TAU. The main cost-effect was driven by reduced inpatient services. The reductions in mental health costs were similar both for those who gained competitive employment and those who had work placements or sheltered work. This indicates that JUMP was a beneficial mental health treatment approach, which should be of great interest to service providers. This is particularly relevant given the current need in Norway to reduce the substantial economic burden of unemployment/risk of unemployment due to severe mental illness [8]. Although the point estimate indicates that JUMP both increased quality adjusted life years (QALY) and reduced costs, there is uncertainty concerning both variables.
Abbreviations
- CBT:
-
Cognitive behaviour therapy
- CR:
-
Cognitive remediation
- DDD:
-
Defined daily dose
- DSM-IV:
-
Diagnostic and statistical manual - iv
- EQ-5D:
-
EuroQol – 5 dimensions
- GLM:
-
Generalized linear model
- HELFO:
-
The Norwegian Health Economics Administration
- HoNOS:
-
Health of the Nation Outcome Scales
- IBM SPSS:
-
IBM (International Business Machines) Statistical analysis software package
- IPLOS:
-
The Individual-based Register of Care Services
- IQ:
-
Intelligence quotient
- JUMP:
-
Job management program
- NAV:
-
The Norwegian Labour and Welfare Administration
- NOK:
-
Norwegian kroner
- NorPD:
-
The Norwegian Prescription Database
- NPR:
-
The Norwegian Patient Register
- QALY:
-
Quality adjusted life years
- TAU:
-
Treatment as usual
- VR:
-
Vocational Rehabilitation
References
McGurk SR, Mueser KT, Feldman K, Wolfe R, Pascaris A. Cognitive training for supported employment: 2-3 year outcomes of a randomized controlled trial. Am J Psychiatry. 2007;164(3):437–41.
Alonso J, Croudace T, Brown J, Gasquet I, Knapp MR, Suarez D, Novick D. Health-related quality of life (HRQL) and continuous antipsychotic treatment: 3-year results from the schizophrenia health outcomes (SOHO) study. Value Health. 2009;12(4):536–43.
Bouwmans C, de Sonneville C, Mulder CL, Hakkaart-van Roijen L. Employment and the associated impact on quality of life in people diagnosed with schizophrenia. Neuropsychiatr Dis Treat. 2015;11:2125–42.
Burns T, Catty J, White S, Becker T, Koletsi M, Fioritti A, Rossler W, Tomov T, van Busschbach J, Wiersma D, et al. The impact of supported employment and working on clinical and social functioning: results of an international study of individual placement and support. Schizophr Bull. 2009;35(5):949–58.
Jonsdottir A, Waghorn G. Psychiatric disorders and labour force activity. Ment Health Rev J. 2015;20(1):13.
Davidson M, Kapara O, Goldberg S, Yoffe R, Noy S, Weiser M. A nation-wide study on the percentage of schizophrenia and bipolar disorder patients who earn minimum wage or above. Schizophr Bull. 2015;42:443–7.
Evensen S, Wisloff T, Lystad JU, Bull H, Ueland T, Falkum E. Prevalence, employment rate, and cost of schizophrenia in a high-income welfare society: a population-based study using comprehensive health and welfare registers. Schizophr Bull. 2016;42(2):476–83.
OECD: Mental Health and Work: Norway. In.; 2013.
Burns T, White SJ, Catty J. Individual placement and support in Europe: the EQOLISE trial. Int Rev Psychiatry. 2008;20(6):498–502.
Bond GR, Drake RE. Making the case for IPS supported employment. Admin Pol Ment Health. 2014;41(1):69–73.
Bond GR, Drake RE, Becker DR. An update on randomized controlled trials of evidence-based supported employment. Psychiatr Rehabil J. 2008;31(4):280–90.
Bond GR, Drake RE, Campbell K. Effectiveness of individual placement and support supported employment for young adults. Early Interv Psychiatry. 2014.
Burns T, Catty J, Becker T, Drake RE, Fioritti A, Knapp M, Lauber C, Rossler W, Tomov T, van Busschbach J, et al. The effectiveness of supported employment for people with severe mental illness: a randomised controlled trial. Lancet. 2007;370(9593):1146–52.
Mueser KT, Becker DR, Torrey WC, Xie H, Bond GR, Drake RE, Dain BJ. Work and nonvocational domains of functioning in persons with severe mental illness: a longitudinal analysis. J Nerv Ment Dis. 1997;185(7):419–26.
Luciano A, Bond GR, Drake RE. Does employment alter the course and outcome of schizophrenia and other severe mental illnesses? A systematic review of longitudinal research. Schizophr Res. 2014;159(2–3):312–21.
Evensen S, Ueland T, Lystad JU, Bull H, Klungsoyr O, Martinsen EW, Falkum E. Employment outcome and predictors of competitive employment at 2-year follow-up of a vocational rehabilitation programme for individuals with schizophrenia in a high-income welfare society. Nord J Psychiatry. 2017;71(3):180–7.
Marino LA, Dixon LB. An update on supported employment for people with severe mental illness. Curr Opin Psychiatry. 2014;27(3):210–5.
Salkever D. Social costs of expanding access to evidence-based supported employment: concepts and interpretive review of evidence. Psychiatr Serv. 2013;64(2):111–9.
Knapp M, Patel A, Curran C, Latimer E, Catty J, Becker T, Drake RE, Fioritti A, Kilian R, Lauber C, et al. Supported employment: cost-effectiveness across six European sites. World Psychiatry. 2013;12(1):60–8.
Husereau D, Drummond M, Petrou S, Carswell C, Moher D, Greenberg D, Augustovski F, Briggs AH, Mauskopf J, Loder E. Consolidated health economic evaluation reporting standards (CHEERS)--explanation and elaboration: a report of the ISPOR health economic evaluation publication guidelines good reporting practices task force. Value Health. 2013;16(2):231–50.
Spjelkavik Ø. Supported employment in Norway and in the other Nordic countries. J Vocational Rehabil. 2012;37:163–72.
Falkum E, Klungsøyr O, Lystad JU, Bull HC, Evensen S, Martinsen E, Friis S, Ueland T. Vocational rehabilitation for adults with psychotic disorders in a Scandinavian welfare society. BMC Psychiatry. 2017:17, 24.
Lystad JU, Falkum E, Haaland VO, Bull H, Evensen S, McGurk SR, Ueland T. Cognitive remediation and occupational outcome in schizophrenia spectrum disorders: a 2year follow-up study. Schizophr Res. 2017;185:122–9.
Lystad JU, Falkum E, Haaland VO, Bull H, Evensen S, Bell MD, Ueland T. Neurocognition and occupational functioning in schizophrenia spectrum disorders: the MATRICS consensus cognitive battery (MCCB) and workplace assessments. Schizophr Res. 2016;170(1):143–9.
APA: Diagnostic and statistical manual of mental disorders: DSM-IV; 1994.
Bull H, Ueland T, Lystad JU, Evensen S, Friis S, Martinsen EW, Falkum E. Validation of the work behavior inventory. Nord J Psychiatry. 2015;69(4):300–6.
Berge T, Falkum E. Se mulighetene: Arbeidsliv og psykisk helse. Oslo: Gyldendal Akademisk; 2013.
Evensen S, Ueland T, Lystad JU, Bull H, Klungsoyr O, Martinsen EW, Falkum E. Employment outcome and predictors of competitive employment at 2-year follow-up of a vocational rehabilitation programme for individuals with schizophrenia in a high-income welfare society. Nord J Psychiatry. 2016:1–8.
Wing JK, Curtis RH, Beevor AS. HoNOS: health of the nation outcome scales: report on Research and Development July 1993–December 1995. London: Royal College of Psychiatrists; 1996.
Helsedirektoratet. In: Divisjon helseøkonomi og finansiering A, DRG fo, editor. Guidelines for economic evaluation in the health sector. Oslo: Helsedirektoratet v/ Trykksaksekspedisjonen; 2012.
StatisticsNorway. Consumer price index, February 2016. Oslo, Norway: Statistics Norway; 2016.
NorgesBank. Annual exchange rates (from 1960). Oslo: Norges Bank; 2016.
Helle S, Gråwe R. Employment and social benefit among persons with schizophrenia in Norway. J Norwegian Psychol Assoc. 2007;44(11):1358–62.
Tandberg M, Ueland T, Sundet K, Haahr U, Joa I, Johannessen JO, Larsen TK, Opjordsmoen S, Rund BR, Rossberg JI, et al. Neurocognition and occupational functioning in patients with first-episode psychosis: a 2-year follow-up study. Psychiatry Res. 2011;188(3):334–42.
Melle I, Friis S, Hauff E, Vaglum P. Social functioning of patients with schizophrenia in high-income welfare societies. Psychiatr Serv. 2000;51(2):223–8.
Bobinac A, van Exel J, Rutten FF, Brouwer WB. The value of a QALY: individual willingness to pay for health gains under risk. Pharmacoeconomics. 2014;32(1):75–86.
IBM: IBM SPSS statistics for windows. 21.0 edn. Armonk, NY: IBM Corp; 2012.
StataCorp. Stata for Windows. College Station: StataCorp LP; 2013.
Kahn I. Design & Analysis of clinical trials for Economic Evaluation & Reimbursement: an applied approach using SAS & STATA. Boca Raton, Florida: CRC Press, Taylor & Francis Group; 2016.
Mihaylova B, Briggs A, O'Hagan A, Thompson SG. Review of statistical methods for analysing healthcare resources and costs. Health Econ. 2011;20(8):897–916.
Drummond MF, Schulpher MJ, Claxton K, Stoddart GL, Torrance GW. Methods for the economic evaluation of health care Programmes. 4th ed. Oxford: Oxford University Press; 2015.
Sælensminde K: Helseeffekter i samfunnsøkonomiske analyser Edited by Health NDo: Norwegian Directorate of Health; 2007.
Bang H, Zhao H. Cost-effectiveness analysis: a proposal of new reporting standards in statistical analysis. J Biopharm Stat. 2014;24(2):443–60.
Bush PW, Drake RE, Xie H, McHugo GJ, Haslett WR. The long-term impact of employment on mental health service use and costs for persons with severe mental illness. Psychiatr Serv. 2009;60(8):1024–31.
Schneider J, Boyce M, Johnson R, Secker J, Slade J, Grove B, Floyd M. Impact of supported employment on service costs and income of people with mental health needs. J Ment Health. 2009;18(6):533–42.
Perkins DV, Born DL, Raines JA, Galka SW. Program evaluation from an ecological perspective: supported employment services for persons with serious psychiatric disabilities. Psychiatr Rehabil J. 2005;28(3):217–24.
Reme S, Monstad K, Fyhn T, Øverland S, Ludvigsen K, Sveinsdottir V, Løvvik C, Lie SA: Effektevaluering av Individuell jobbstøtte (IPS). In.: Uni research Helse & Uni research Rokkansenteret; 2016.
Black WC. The cost-effectiveness plane: a graphic representation of cost-effectiveness. Med Decis Mak. 1990;10(3):212–5.
Acknowledgments
The authors thank all participants who took part in the study and all their collaborators for making this research possible. We also thank the NPR, NorPD, NAV, and the IPLOS registers for providing data for this study.
Funding
This work was supported by The Norwegian Directorate of Health (14/4607–13), the Norwegian Labour and Welfare Administration, The South Eastern Norway Health Authority (9297), and The National Council for Mental Health/Health and Rehabilitation (2008/2/0310).
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
SE: Data collection; analysis and interpretation of data; drafting the manuscript; final approval of the manuscript. TW: Analysis and interpretation of data; critical revision of the manuscript; final approval of the manuscript. JL: Data collection; analysis and interpretation of data; critical revision of the manuscript; final approval of the manuscript. HB: Data collection; analysis and interpretation of data; critical revision of the manuscript; final approval of the manuscript. EM: Conceptualisation and design of the JUMP study; critical revision of the manuscript; final approval of the manuscript. TU: Conceptualisation and design of the JUMP study; critical revision of the manuscript; final approval of the manuscript. EF: Conceptualisation and design of the JUMP study; critical revision of the manuscript; final approval of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The JUMP study was approved by the Regional Committee of Medical Research Ethics and the Norwegian Data Protection Authority. ClinicalTrials.gov Identifier: NCT01139502. The cost-effectiveness evaluation was approved by the Norwegian Data Protection Authority (14/00035–5/EOL). All participants provided written informed consent after a complete description of the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Evensen, S., Wisløff, T., Lystad, J.U. et al. Exploring the potential cost-effectiveness of a vocational rehabilitation program for individuals with schizophrenia in a high-income welfare society. BMC Psychiatry 19, 140 (2019). https://doi.org/10.1186/s12888-019-2130-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12888-019-2130-7