Abstract
Background
Despite significant advances in neonatology, bronchopulmonary dysplasia (BPD) remains the most common cause of serious morbidity and mortality in premature infants. The aim of the present study was to determine associations between the respiratory severity score (RSS) with death or BPD in premature infants.
Methods
This was a retrospective study conducted between January 2010 and December 2014. We enrolled preterm infants with a gestational age of less than 28 weeks who were supported by mechanical ventilation for more than a week during the first 4 weeks of life. We collected the RSS scores on day of life 2, 7, 14, 21 and 28. The correlations between postnatal RSSs and death or severe BPD were analyzed using multivariate logistic regression.
Results
Of the 138 eligible infants, 66 infants (47.8%) either died or developed severe BPD. The RSS cut-off values for predicting severe BPD or death were 3.0 for postnatal day (PND) 14 with an odds ratio (OR) of 11.265 (p = 0.0006, 95% confidence interval (CI), 2.842 to 44.646), 3.6 for PND 21 with an OR of 15.162 (p = 0.0003, 95% CI, 3.467 to 66.316), and 3.24 for PND 28 with an OR of 10.713 (p = 0.0005, 95% CI, 2.825 to 40.630).
Conclusion
Strong correlations were observed between the RSSs on PND 14, 21, and 28 and death or subsequent severe BPD. The RSS could provide a simple estimate of severe BPD or death., Further research with a larger study population is necessary to validate the usefulness of the RSS for predicting severe BPD or death.
Similar content being viewed by others
Background
Bronchopulmonary dysplasia (BPD) is a serious pulmonary condition and one of the most common causes of mortality and morbidity in preterm infants. Although numerous studies have been performed to identify risk factors of BPD to develop preventative therapies, the exact pathogenesis and predictors for BPD remain unclear [1]. In addition, the incidence of BPD has increased over the past 2 to 3 decades despite many advances in neonatal care for preventing BPD, such as gentle ventilation strategies, antenatal steroids, surfactants, and postnatal steroids [2,3,4,5]. Because infants with severe BPD require prolonged mechanical ventilation and are associated with the long-lasting burdens of pulmonary and neurodevelopmental sequelae [6,7,8,9,10,11], research for identifying predictive factors for the earlier diagnosis of BPD severity is valuable; the accurate detection of severe BPD at an early stage may enable the initiation of therapies when they may be more effective and may avoid unnecessary therapies, such as corticosteroids, thereby reducing their potential hazards [12].
The respiratory severity score (RSS) is a simplified severity score consisting of the mean airway pressure (MAP) multiplied by the fraction of inspired oxygen (FiO2). The RSS has been used in place of the oxygen index (OI) to assess the need for respiratory support in infants requiring assisted ventilation because the lack of arterial access in infants precludes monitoring the partial pressure of arterial oxygen (PaO2) [13]. A previous study revealed a strong association between the RSS and OI at saturation levels of arterial oxygen (SaO2) between 88 and 94% in intubated infants [14]. Recently, Malkar et al. demonstrated that an RSS ≥6 on day 30 of life was associated with increased mortality and mechanical ventilation duration in premature infants supported by mechanical ventilation for more than 30 days [15]. The study also suggested the possible usefulness of the RSS as a predictive factor for outcomes in neonatal respiratory conditions.
The objective of the current study was to evaluate the correlation between the RSS and subsequent severe BPD or death.
Methods
This was a retrospective study conducted in the neonatal intensive care unit at Seoul National University Children’s Hospital between January 2010 and December 2014. Approval for this study was obtained from the Seoul National University Hospital Institutional Review Board.
Subjects
We enrolled preterm infants with a gestational age of less than 28 weeks who were supported by mechanical ventilation for more than a week during the first 4 weeks of life. The exclusion criteria were as follows: 1) patients with major congenital malformations; 2) patients who died within the first 7 days; or 3) patients who were intubated for ≤7 days or were never intubated.
All infants in this study who needed surfactant instillation were intubated, and minimally invasive surfactant therapy techniques were not applied during the study period. We updated our institutional neonatal resuscitation protocols according to the 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care during the study period [16]. Per the guidelines of neonatal resuscitation, preterm infants who were spontaneously breathing and had respiratory distress were considered for application of positive end expiratory pressure (PEEP) in the delivery room and the selective use of surfactants.
During the first 4 weeks of life, in order to avoid over-distension and atelectasis and consequent injury, we usually start mechanical ventilation rates of 40–60 breaths per minute, inspiration time of 0.25–0.35 s and tidal volume (Vt) of 4–6 ml/kg, and for high frequency oscillation ventilator (HFOV) use of the minimum MAP and amplitude required to achieve clinical goals. In most cases, a PEEP of 4 to 7 cmH2O was applied, and FiO2 was titrated to achieve an oxygen saturation (SpO2) value between 90 and 95%. The ventilator graphics and lung mechanics were monitored at the bedside, and for some severe cases with weaning difficulty, we adjusted the ventilator settings individually according to the information from the ventilator. A high-frequency oscillation ventilator was usually considered when a plateau pressure of 25 cmH2O on pressure-controlled time-cycled ventilation did not reach a sufficient tidal volume or when it was not possible to maintain an SpO2 greater than 90% with a FiO2 value of at most 0.4–0.6. The ventilator settings were established at the discretion of the clinical teams, and FiO2 was preferentially titrated to minimize oxygen concentration level within a SpO2 range of 90 and 95% before minimizing MAP.
Extubation was considered in patients who showed the following minimal ventilator settings for > 12 h according to the protocol of our center: (1) MAP ≤8 cmH2O; (2) FiO2 ≤ 0.4; and (3) mandatory respiratory frequency ≤ 35/min.
Data collection
The charts of the study population were reviewed. Demographic, perinatal and neonatal data were obtained; prenatal factors included preterm premature rupture of the membrane, chorioamnionitis, oligohydramnios, preeclampsia, and antenatal steroid administration. Demographic and neonatal factors included gestational age, birth weight, small for gestational age (SGA), sex, postnatal systemic steroid use, mechanical ventilation duration, and ventilator settings. Ventilator settings on day of life 2, 7, 14, 21, and 28 were collected, and RSSs were calculated. MAP was calculated as MAP = PEEP + ((PIP-PEEP) x (ti/ti + te)), where PIP is the peak inspiratory pressure, ti is the inspiratory time, and te is the expiratory time [17]. Systemic steroid treatment was used as only a rescue therapy for selected severe cases which needed maximal ventilator and oxygen supports according to the American Academy of Pediatrics statement [18]. However systemic steroid treatment could be associated with a reduction in respiratory support, RSSs after systemic steroid administration were excluded from the analysis.
Outcomes
The primary outcome was death or severe BPD. BPD was defined using the National Institute of Child Health criteria for BPD and graded as mild, moderate, or severe according to the FiO2 or positive pressure ventilation (PPV) [19]. Mild BPD was defined as breathing room air, moderate BPD was defined as an FiO2 value less than 0.30, and severe BPD was defined as an FiO2 value of at least 0.3 or PPV at a postmenstrual age of 36 weeks. Secondary outcomes included the duration of mechanical ventilation or supplemental oxygen, pulmonary arterial hypertension, the duration of hospitalization, and other morbidities such as surfactant use for respiratory distress syndrome, the occurrence of grade 3–4 intraventricular hemorrhage (IVH), cerebral palsy, periventricular leukomalacia, necrotizing enterocolitis (NEC) ≥ stage 2 by Bell’s classification, retinopathy of prematurity (ROP), and culture proven late-onset sepsis.
Statistical analysis
The chi-square and independent t-tests were used to compare variables. The associations of severe BPD or death with the RSS were analyzed using a multiple logistic regression model. To determine the most predictive time point for severe BPD or death, stepwise backward regression was used. The minimum p value approach was applied for selecting the optimal RSS cut-off [20]. Cubic splines were used to allow flexible forms of RSS to be modeled for finding optimal cut-points. A steep and definitive increase in the spline function near a threshold value which is relatively flat before the threshold provides evidence in favor of a cut-point model [21]. Determining the existence of a threshold effect and estimating an optimal cut-point for RSS uses a series of two-sample tests for the multiple possible candidate dichotomizations of RSS. We excluded the outer 10% of RSS distribution to avoid having small numbers in one of the groups following dichotomization, thereby preventing substantial loses in the statistical power. The optimal cut-point was defined as that candidate cut-point with the smallest p-value [22]. And cross-validation was performed for measuring the predictive performance of the optimal cut-off value [23]. Statistical analyses were performed using statistical software (SAS, version 9.4; SAS Institute Inc., Cary, NC, USA).
Ethics statement
The Institutional Review Board of Seoul National University Hospital approved the collection and use of the clinical information of the patients for research purposes before the investigation was started and waived the requirement for informed consent. (IRB No. 1602–026-739).
Results
Patients
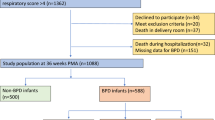
A flow diagram of our study population is presented in Fig. 1. During the 5-year study period, a total of 205 neonates born at less than 28 weeks of gestation were eligible for inclusion. After excluding infants who died within the first 7 days, were never intubated, or were intubated for less than a week, a total of 138 patients were enrolled. Of these, 66 (47.8%) infants either died (n = 17) or developed severe BPD (n = 57). 3 patients required tracheostomy at discharge. Systemic dexamethasone was administered in 7 patients within 4 weeks after birth; all patients required mechanical ventilatory support with FiO2 > 0.5 and RSS > 5.0, and a total dose of systemic dexamethasone administered in each patient was 1.1 mg/kg.
Comparison between the groups with and without severe BPD or mortality
The basal characteristics and clinical data of subjects with and without severe BPD or mortality are compared in Table 1. Infants who died or developed severe BPD had significantly lower gestational ages and birth weights, longer durations of assisted ventilation and supplemental oxygen, increased use of postnatal steroids for BPD, and higher incidences of pulmonary arterial hypertension than survivors without severe BPD. Other morbidities, such as NEC, IVH, ROP, and sepsis were similar between the two groups.
Association of RSSs with severe BPD or death
The comparison of RSS values at postnatal days 2, 7, 14, 21 and 28 between the two groups are shown in Table 2. Infants who died or developed severe BPD showed consistently higher RSSs than did those who survived without severe BPD. RSSs at postnatal days 14, 21 and 28 were significantly associated with death or severe BPD. After adjusting for prenatal and postnatal factors that were associated with the development of BPD, the multivariate logistic regression analysis demonstrated that RSSs at postnatal day 14 (odds ratio (OR), 2.135; 95% confidence interval (CI), 1.126 to 4.049), 21 (OR, 2.7; 95% CI, 1.432 to 5.464), and 28 (OR, 3.526; 95% CI, 1.601 to 7.764) remained significantly associated with a higher risk of death or severe BPD.
RSS cut-off value for predicting death or severe BPD
Higher RSSs at 14, 21 and 28 days of life were significantly associated with a higher risk of death or severe BPD. To develop the RSS as a predictive factor for death or severe BPD, optimal cut-off values were analyzed using a minimum p value approach for each of three time points: RSS value was 3.0 for postnatal day 14 with an OR of 11.265 (p = 0.0006, 95% CI, 2.842 to 44.646), 3.6 for postnatal day 21 with an OR of 15.162 (p = 0.0003, 95% CI, 3.467 to 66.316), and 3.24 for postnatal day 28 with an OR of 10.713 (p = 0.0005, 95% CI, 2.825 to 40.630), respectively (Table 3). The sensitivity, specificity, positive and negative predictive values of each RSS values are shown in Table 4. We also performed multivariable logistic regression analyses with including patients who were completely administered the systemic steroid as a secondary sensitivity analysis, the results did not change and the optimal cut-off values for predicting death or severe BPD were same.
Discussion
Recently, several trials have focused on the prevention of BPD in very preterm infants, using methods such as steroid administration, inhaled nitric oxide, and stem cell therapy [24,25,26,27,28,29,30]. Although those therapies might be beneficial for reducing the incidence of BPD, a lack of evidence exists regarding their safety and effectiveness. Hence, research on preventing BPD must focus on high-risk populations for severe BPD by assessing the balance between potential benefits and harms.
Many clinical models have been developed to predict the risk of BPD. The Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network has developed a predictive model for BPD that is available as a web-based tool to provide estimates of BPD based on demographic variables and respiratory support by postnatal day [31]. This tool might be helpful to identify patients who are at a higher risk for BPD and are most likely to benefit from postnatal preventive treatment. However, Asian race was not considered in this model. Later, Onland et al. reviewed 26 clinical prediction models for BPD in 2013 and concluded that most existing clinical prediction models are poor to moderate predictors of BPD [32]. None of the previous BPD prediction models have been widely adopted.
In the present study, we focused on using the RSS to predict severe BPD or death. RSSs at postnatal days 14, 21, and 28 were significantly associated with death or severe BPD after adjusting for other BPD-related factors. In addition, the RSS could provide an estimate of severe BPD or death at a relatively early stage. At the aspect for prediction, RSS at postnatal day 14 might provide early identification of infants at high risk for BPD or death whilereas RSS at postnatal day 28 might have less meaningful in practice. RSS at postnatal day 21 was the most highly associated with severe BPD or death.
The RSS has been used in several major randomized control trials as a surrogate for the OI in assessing the severity of respiratory illness [25, 33]. The OI is one of well-known respiratory indices for quantifying the severity of oxygenation failure [34, 35]. However, the OI requires an indwelling arterial catheter, which in turn is associated with multiple complications including thromboembolism and ischemic injury. In addition, the OI cannot reflect real-time pulmonary status and needs frequent blood samplings which lead to severe anemia in preterm infants [36]. In current clinical practice, arterial blood sampling is much less common than in the past. As alternative non-invasive methods of assessing the severity of respiratory failure, oxygen saturation index calculated by substituting SpO2 for PaO2 showed a good correlation with OI [37]. As a strong association between the RSS and the OI in preterm infants under mechanical ventilation at oxygen saturation between 88 and 94% was revealed [14], the RSS can be used instead of the OI when preterm infants maintain at targeted saturation. The RSS can easily determine the need for and assess the response to therapeutic interventions in infants requiring mechanical ventilation.
In this study, we included only patients who required intubated ventilatory support. The intubation rate during the first day of life was 92.6%, which was similar to the value of 89% reported by the Neonatal Research Network, and the moderate to severe BPD rate was 47%, which was similar to or slightly higher than the rates of other studies. We did not use any minimally invasive surfactant therapy techniques during the study period. Although that might have increased the risk of intubation for surfactant instillation, we initially considered the application of PEEP in the delivery room according to the guidelines of the neonatal resuscitation program, as well as the selective use of surfactants. The association between a longer duration of mechanical ventilation and chronic lung disease is well known. Avoiding intubation and using non-invasive ventilator support are necessary to minimize exposure to mechanical ventilation. However, in the Surfactant, Positive Pressure, and Oxygenation Randomized Trial (SUPPORT), 83% of extremely low birth weight infants initially assigned to non-invasive support required endotracheal intubation and mechanical ventilator care [38]. Morley CJ et al. also showed that among preterm infants 25 to 28 weeks in gestational age who had adequate respiratory effort and were assigned to non-invasive support, almost half required endotracheal intubation and mechanical ventilation [39]. In practice, preterm infants with younger gestational ages still require invasive mechanical ventilatory support. The present study showed that the RSS can be used for one of predictors of severity of BPD in these infants who require intubation and mechanical ventilator support. However, there are some limitations that infants who require intubation because of other causes instead of lung conditions, such as airway problems or apnea of prematurity, were included in the study. In addition, RSS can be highly affected on ventilatory support strategies and need to be standardized for validation. Recently, several new modalities for non-invasive respiratory support, such as non-invasive intermittent positive pressure ventilation, and non-invasive neurally adjusted ventilatory assist, have been developed. Those new techniques might provide more sophisticated respiratory support without intubation to extremely preterm infants in near future. Therefore, further investigation would be important to determine the effect of various non-invasive techniques on the outcomes of the present study.
Additionally, because this analysis was retrospective and based on experiences within a single unit, further research with a larger prospective cohort study is necessary to validate the usefulness of the RSS for predicting the outcome at a postmenstrual age of 40 weeks. RSS can be used one of covariates for developing a better clinical model to predict the risk of severe BPD or death.
Conclusion
In conclusion, the present study demonstrated that there were strong correlations between RSSs at postnatal days 14, 21, and 28 and subsequent severe BPD or death. Furthermore, an RSS ≥ 3.0 at postnatal day 14 and an RSS ≥ 3.6 at postnatal day 21 were reliable values for predicting severe BPD or death. The RSS could provide a simple estimate of severe BPD or death at various postnatal ages and might be helpful for determining the proper time for early interventions.
Change history
31 July 2019
.
Abbreviations
- BPD:
-
Bronchopulmonary dysplasia
- CI:
-
Confidence interval
- FiO2:
-
Fraction of inspired oxygen
- IVH:
-
Intraventricular hemorrhage
- MAP:
-
Mean airway pressure
- NEC:
-
Necrotizing enterocolitis
- OI:
-
Oxygen index
- OR:
-
Odds ratio
- PaO2:
-
Partial pressure of arterial oxygen
- PEEP:
-
Positive end expiratory pressure
- PND:
-
Postnatal day
- PPV:
-
Positive pressure ventilation
- ROP:
-
Retinopathy of prematurity
- RSS:
-
Respiratory severity score
- SaO2:
-
Saturation levels of arterial oxygen
- SGA:
-
Small for gestation
References
Halliday H, O’neill C. What is the evidence for drug therapy in the prevention and management of bronchopulmonary dysplasia. In: Bancalari E, editor. The newborn lung: neonatal questions and controversies. 1st ed. Amsterdam: Saunders Elsevier; 2008. p. 208–32.
Manktelow BN, Draper ES, Annamalai S. Factors affecting the incidence of chronic lung disease of prematurity in 1987, 1992, and 1997. Arch Dis Child Fetal Neonatal Ed. 2001;85:F33–5.
Smith VC, Zupancic JA, McCormick MC, Croen LA, Greene J, Escobar GJ, et al. Trends in severe bronchopulmonary dysplasia rates between 1994 and 2002. J Pediatr. 2005;146:469–73.
Shah PS, Sankaran K, Aziz K, Allen AC, Seshia M, Ohlsson A, et al. Outcomes of preterm infants <29 weeks gestation over 10-year period in Canada: a cause for concern? J Perinatol. 2012;32:132–8.
Stoll BJ, Hansen NI, Bell EF, Walsh MC, Carlo WA, Shankaran S, et al. Trends in care practices, morbidity, and mortality of extremely preterm neonates, 1993-2012. JAMA. 2015;314:1039–51.
Cristea AI, Carroll AE, Davis SD, Swigonski NL, Ackerman VL. Outcomes of children with severe bronchopulmonary dysplasia who were ventilator dependent at home. Pediatrics. 2013;132:e727–34.
Smith VC, Zupancic JA, McCormick MC, Croen LA, Creene J, Escobar GJ, et al. Rehospitalization in the first year of life among infants with bronchopulmonary dysplasia. J Pediatr. 2004;144:799–803.
Schmidt B, Asztalos EV, Roberts RS, Robertson CM, Sauve RS, Whitfield MF, et al. Impact of bronchopulmonary dysplasia, brain injury, and severe retinopathy on the outcome of extremely low-birth-weight infants at 18 months: results from the trial of indomethacin prophylaxis in preterms. JAMA. 2003;289(9):1124–9.
Anderson PJ, Doyle LW. Neurodevelopmental outcome of bronchopulmonary dysplasia. Semin Perinatol. 2006;30:227–32.
Doyle LW, Anderson PJ. Long-term outcomes of bronchopulmonary dysplasia. Semin Fetal Neonatal Med. 2009;14:391–5.
Jeng SF, Hsu CH, Tsao PN, Chou HC, Lee WT, Kao HA, et al. Bronchopulmonary dysplasia predicts adverse developmental and clinical outcomes in very-low-birth-weight infants. Dev Med Child Neurol. 2008;50:51–7.
Lal CV, Ambalavanan N. Biomarkers, early diagnosis, and clinical predictors of bronchopulmonary dysplasia. Clin Perinatol. 2015;42:739–54.
Kim EH, Cohen RS, Ramachandran P. Effect of vascular puncture on blood gases in the newborn. Pediatr Pulmonol. 1991;10:287–90.
Iver NP, Mhanna MJ. Non-invasively derived respiratory severity score and oxygenation index in ventilated newborn infants. Pediatr Pulmonol. 2013;48:364–9.
Malkar MB, Gardner WP, Mandy GT, Stenger MR, Nelin LD, Shepherd EG, et al. Respiratory severity score on day of life 30 is predictive of mortality and the length of mechanical ventilation in premature infants with protracted ventilation. Pediatr Pulmonol. 2015;50(4):363–9.
Kattwinkel J, Perlman JM, Aziz K, Colby C, Fairchild K, Gallagher J, et al. Part 15: neonatal resuscitation: 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2010;122:S909–19.
Glenski JA, Marsh HM, Hall RT. Calculation of mean airway pressure during mechanical ventilation in neonates. Crit Care Med. 1984;12:642–4.
American Academy of Pediatrics Committee on Fetus and Newborn. Postnatal corticosteroids to treat or prevent chronic lung disease in preterm infants. Pediatrics. 2002;109(2):330–8.
Jobe AH, Bancalari E. Bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2001;163:1723–9.
Williams BA, Mandrekar JN, Mandrekar SJ, Cha SS, Furth AF. Finding optimal cutpoints for continuous covariates with binary and time to event outcomes. Technical Reports Series #79. Department of Health Sciences Research, Mayo Clinic, Rochester, MN, June 2006. https://www.mayo.edu/research/documents/biostat-79pdf/doc-10027230.
Greenland S. Avoiding power loss associated with categorization and ordinal scores in dose-reposne and trend analysis. Epidemiology. 1995;6:450–4.
Altman DG, Lausen B, Sauerbrei W, Schumacher M. Danger of using “optimal” cutpoints in the evaluation of prognostic factors. J Natl Cancer Inst. 1994;84:829–35.
Faraggi D, Simon R. A simulation study of cross-validation for selecting an optimal cutpoint in univariate survival analysis. Statist Med. 1996;15:2203–13.
McEvoy CT, Jain L, Schmidt B, Abman S, Bancalari E, Aschner JL. Bronchopulmonary dysplasia: NHLBI workshop on the primary prevention of chronic lung disease. Ann Am Thorac Soc. 2014;11(Suppl3):S146–53.
Ballard RA, Truog WE, Cnaan A, Martin RJ, Ballard PL, Merrill JD, et al. Inhaled nitric oxide in preterm infants undergoing mechanical ventilation. N Engl J Med. 2006;355:343–53.
Askie LM, Ballard RA, Cutter GR, Dani C, Elbourne D, Field D, et al. Inhaled nitric oxide in preterm infants: an individual-patient data meta-analysis of randomized trials. Pediatrics. 2011;128(4):729–39.
Doyle LW, Ehrenkranz RA, Halliday HL. Dexamethasone treatment after the first week of life for bronchopulmonary dysplasia in preterm infants: a systematic review. Neonatology. 2010;98(4):289–96.
Doyle LW, Ehrenkranz RA, Halliday HL. Postnatal hydrocortisone for preventing or treating bronchopulmonary dysplasia in preterm infants: a systematic review. Neonatology. 2010;98(2):111–7.
van Haaften T, Byrne R, Bonnet S, Rochefort GY, Akabutu J, Bouchentouf M, et al. Airway delivery of mesenchymal stem cells prevents arrested alveolar growth in neonatal lung injury in rats. Am J Respir Crit Care Med. 2009;180:1131–42.
Pierro M, Lonescu L, Montemurro T, Vadivel A, Weissmann G, Oudit G, et al. Short-term, long-term and paracrine effect of human umbilical cord-derived stem cells in lung injury prevention and repair in experimental bronchopulmonary dysplasia. Thorax. 2013;68:475–84.
Laughon MM, Langer JC, Bose CL, Smith PB, Ambalavanan N, Kennedy KA, et al. Prediction of bronchopulmonary dysplasia by postnatal age in extremely premature infants. Am J Respir Crit Care Med. 2011;183:1715–22.
Onland W, Debray TP, Laughon MM, Meidema M, Cools F, Askie LM, et al. Clinical prediction models for bronchopulmonary dysplasia: a systematic review and external validation study. BMC Pediatr. 2013;13:207. https://doi.org/10.1186/1471-2431-13-207.
Mercier JC, Hummler H, Durrmeyer X, Sanchez-Luna M, Carnielli V, Field D, et al. Inhaled nitric oxide for prevention of bronchopulmonary dysplasia in premature babies (EUNO): a randomized controlled trial. Lancet. 2010;376:346–54.
Schreiber MD, Gin-Mestan K, Marks JD, Huo D, Lee G, Srisuparp P. Inhaled nitric oxide in premature infants with the respiratory distress syndrome. N Engl J Med. 2003;349:2099–107.
Kinsella JP, Cutter GR, Walsh WF, Gerstmann DR, Bose CL, Hart C, et al. Early inhaled nitric oxide therapy in premature newborns with respiratory failure. N Engl J Med. 2006;355:354–64.
Obladen M, Sachsenweger M, Stahnke M. Blood sampling in very low birth weight infants receiving different levels of intensive care. Eur J Pediatr. 1988;147:399–404.
Rawat M, Chandrasekharan PK, Williams A, Gugino S, Koenigshnecht C, Swartz D, et al. Oxygen saturation index and severity of hypoxic respiratory failure. Neonatology. 2015;107:106–66.
Support Study Group of the Eunice Kennedy Shriver NICHD Neonatal Research Network, Finer NN, Carlo WA, Walsh MC, Rich W, Grantz MG, Laptook AR, et al. Early CPAP versus surfactant in extremely preterm infants. N Engl J Med. 2010;362:1970–9.
Morley CJ, Davis PG, Doyle LW, Brion LP, Hascoet JM, Carlin JB. Nasal CPAP or intubation at birth for very preterm infants. N Engl J Med. 2008;358(7):700–8.
Acknowledgements
A special acknowledgement is extended to the Medical Research Collaborating Center of Seoul National University Hospital.
Funding
None
Availability of data and materials
The dataset supporting the conclusions of this article is included within the article and its Additional file 1.
Author information
Authors and Affiliations
Contributions
YHJ and JHJ conceptualized and designed the study, and wrote the first draft of the manuscripts. HSK conceptualized and designed the study and reviewed and revised the manuscripts. SHS, EKK participated in conducting the study and analyzing the data. CCW, BIK conceived of study, participated in coordinating study and revised the manuscript for important intellectual content. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Institutional Review Board of Seoul National University Hospital approved the collection and use of the clinical information of the patients for research purposes before the investigation was started and waived the requirement for informed consent (IRB No. 1602–026-739).
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional information
This work was performed at the Neonatal Intensive Care Unit of Seoul National University Children’s Hospital, Seoul National University College of Medicine, Seoul, Korea
Additional file
Additional file 1:
Raw data RSS. (XLSX 507 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Jung, Y.H., Jang, J., Kim, HS. et al. Respiratory severity score as a predictive factor for severe bronchopulmonary dysplasia or death in extremely preterm infants. BMC Pediatr 19, 121 (2019). https://doi.org/10.1186/s12887-019-1492-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-019-1492-9