Abstract
Background
Physical activity (PA) is associated with changes in body composition that affect insulin sensitivity and leptin levels. Few studies have assessed the effect of lifestyle interventions on changes in objectively measured PA levels in obese children. To evaluate the effects of a multidisciplinary lifestyle intervention on anthropometric indices, biochemical parameters and accelerometer measured PA in abdominal obese children.
Methods
A randomized control trial was performed in 106 children and adolescents with abdominal obesity. Participants were randomly assigned to usual or intensive care group for 8-week. PA was measured by accelerometry over four days including, at least, two weekdays in all participants. Both groups were encouraged to accumulate an extra time of 200 min per week in their PA.
Results
At baseline, 75% of subjects do not fulfill the WHO recommendation of being more than 60 min/day on moderate-to-vigorous PA (MVPA). The intensive care group achieved a significant reduction in anthropometric indexes compared to the usual care but no significant change was found in biochemical or PA parameters. Both groups achieved a significant reduction in light PA. Interestingly, intensive care participants significantly increased MVPA in 5.5 min/day. Moreover, an inverse association between changes in MVPA and leptin levels was found.
Conclusion
The two lifestyle intervention reduced anthropometric indexes and lowered light PA in abdominal obese children. No significant differences were observed between intensive care and usual care in regard to PA. Intensive care participants significantly increase physical activity (MVPA) and, changes in MVPA were inversely associated with changes in leptin levels after the intervention.
Trial registration
ClinicalTrials.gov, Identifier: NCT03147261. Registered 10 May 2017. Retrospectively registered.
Similar content being viewed by others
Background
Dyslipidemia, hypertension, insulin resistance or type 2 diabetes, are the main alterations that derive from obesity and contribute to aggravate cardiometabolic risk in pediatric populations [1]. Obese children with waist circumference at/or above the 90th percentile are at higher risk for dyslipidemia and insulin resistance than obese children with normal waist circumference [2, 3]. The factors that contribute to childhood obesity are complex, and include an excessive energy intake, a decrease in physical activity and an increase in sedentary behaviors, for example, the screen-time activities [4].
Sedentary lifestyle, the fourth leading cause of global mortality, is becoming more frequent in pediatric populations [5, 6]. “Global Recommendations on Physical Activity for Health” by the WHO state that children and youth aged 5–17 should accumulate a minimum of 60 min of moderate-to-vigorous intensity physical activity (MVPA) every day [5]. But, in Spain, only a 35.2% of children and 11.9% of adolescents (over 13 years) achieved that recommendation [7]. Different approaches for obesity treatment have been proposed over the last decades, but the evidence suggests that successful intervention does include diet and physical activity recommendations, behavioral therapy and family implication [8, 9]. Physical activity is associated with changes in body weight and body fat that ultimately affect insulin sensitivity [7, 10]. In obesity, the described expansion of adipose tissue leads to an increase in leptin levels. This hyperleptinemia has been associated with a pro-inflammatory status with deleterious effects on children’s health [11]. In regard to this, several intervention studies reported a decrease of leptin levels after aerobic PA in obese adolescents [11,12,13]. Thus, increased physical activity, specifically MVPA, may lead to a decrease of leptin levels [14]. To our knowledge, few studies have evaluated the effect of lifestyle interventions on changes in objectively measured PA levels in obese children at high metabolic risk [4, 15,16,17,18,19]. We hypothesized that a successful lifestyle intervention based on PA recommendations is able to modify BMI-SDS, metabolic parameters and objectively measured PA. Hence, the aims of this RCT were: [1] to assess the effectiveness of the two interventions (usual care vs. intensive care group) based on BMI-SDS changes (primary outcome), [2] to evaluate changes on biochemical and PA parameters (secondary outcome) between the two lifestyle interventions. Specifically, in our study we will assess: differences between the two lifestyle interventions and also changes (pre vs. post intervention) in the measured variables in each group.
Methods
Participants
The IGENOI (Intervention Grupo Estudio Navarro de Obesidad Infantil) study is a randomized control trial (NCT03147261) conducted in Pamplona, Navarra (Spain). It is a 2-year family-based lifestyle intervention program for children with abdominal obesity. Seven to sixteen year-old children were recruited from the Endocrinology Pediatric Units of the University of Navarra Clinic, Navarra’s Hospital Complex and Primary Health Care Centers in Pamplona. General inclusion criteria for enrollment was waist circumference above the 90th percentile, according to national data [20, 21]. Subjects with pre-diabetes or food intolerance, following special diets, regular alcohol consumption, major psychiatric illness, eating disorders or medical therapy were excluded. The study protocol was performed in accordance with the ethical standards laid down in the 2013 Declaration of Helsinki (Fortaleza, Brasil, October 2013) and was approved by the Ethics Committee of the University of Navarra (Reference number 044/2014). The parents and/or legal guardians and children involved in the trial received detailed explanations about the aim of the study. Informed assent was obtained from every child and all parents and/or legal guardians signed an informed consent according to the Helsinki declaration.
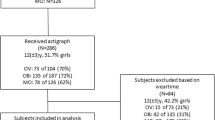
121 of the 126 recruited participants met the inclusion criteria, and 114 successfully concluded the 8-week program. The dropout rate was 6.5% and the main reasons were discouragement, social problems, inability to comply the weekly visits (school exam periods, and change of address for the notifications), as described in other trials with pediatric populations [22]. One hundred and six participants with completed data of objectively measured physical activity both at baseline and after the 8-week (Fig. 1).
The primary endpoint of the IGENOI study was to assess the effectiveness of the lifestyle interventions based on BMI-SDS values. Changes in BMI-SDS are the main outcome since successful interventions should decrease BMI-SDS near 0.5 units in order to reduce cardiometabolic risk [23]. Taking this information into consideration, sample size was estimated with the assumption of: an error of 5%, a power of 90%, a 1:3 ratio and a mean difference of 0.50 (SD 0.47) units in BMI-SDS after the lifestyle intervention. The sample size calculation indicated that 13 and 39 subjects were needed for usual care and intensive care group, respectively. The rationale for the difference in the size of both groups relies on the fact that a high number of subjects could benefit from intensive intervention as indicated in other program for obese children [24].
Study design/ lifestyle intervention
The IGENOI study is a family-based lifestyle program carried out by a multidisciplinary team (dietitians, pediatricians, psychologist, physical activity experts, and nurses) in a clinical setting. It consists of a two-year program that comprises an 8-week phase with individual and group sessions and a follow-up period of 22 months. Our research group has different weight loss interventions where we have observed that in a short time period (8 to 10 weeks) there are substantial changes in weight loss and other metabolic parameters [8, 9]. In this study we present data from the treatment period corresponding to the first 8-weeks, since the study is still on going.
Participants were randomly assigned to the usual or intensive care group with a ratio of 1:3. The randomization was performed using a computer-generate randomization. The intensive care group was advised to follow a fully-day meal plan during the intensive phase. This diet consists on a moderate hypocaloric Mediterranean diet to not to interfere with children’s growth. Energy restriction (10 to 40%) was calculated according to obesity degree and physical activity levels, as described elsewhere [9, 25]. The dietary pattern was based on a high consumption of fruits (3 portions per day) and vegetables (2 portions per day), legumes, whole grains and olive oil; moderate consumption of dairy products, poultry and fish, and the reduction of processed and red meats, limiting them to 1 portion per week. Standard paediatric recommendations on healthy diet were given to usual care subjects. Participants of both groups were aimed to accumulate an extra time per week of 200 min of PA at a 60–75% of their maximum heart rate.
Intensive care participants and their parents received six 30 min-sessions lead by the dietitian during the 8-week period in order to monitor the accomplishment of the diet. One parallel group sessions was organized for 1) intensive care participants and 2) their parents or legal tutors. During the group sessions parents were told their role in the intervention and the obesity related comorbidities, while children were taught about different topics such as energy balance, portion sizes, groups of foods, the importance of the breakfast and physical activity [25]. On the other hand, usual care participants and their parents received one 30-min individual session with the dietitian and five monitoring visits to assess anthropometric parameters.
Anthropometric, clinical and biochemical measurements
Anthropometric measurements (body weight, height) were evaluated by trained personnel following standard procedures. Body mass index (BMI) was calculated as weight divided by squared height (Kg/m2), and these values were converted into standard deviations (BMI-SDS) using age and sex-specific cut-off points according to Spanish reference growth charts [20]. Waist and hip circumferences were assessed with a non-stretchable measuring tape (Type SECA 200) following standard procedures.
Clinical outcomes such as pubertal stage (Tanner stage) and the presence of acanthosis nigricans were examined by pediatricians of the team [26].
Venous blood samples were obtained after an overnight fast. Glucose, insulin and lipid profiles were determined by standard autoanalyzer techniques. Homeostasis model assessment of insulin resistance (HOMA-IR) was calculated from fasting glucose and insulin values. Leptin levels were measured by ELISA (R&D Systems, Minneapolis, MN). All the measurements were taken at baseline and after the 8 week period.
Physical activity and sleep duration
Physical activity and sedentary time were objectively assessed using triaxial accelerometry over four days, including, at least, two weekdays in all participants. Participants and parents were instructed on wearing the accelerometer (Actigraph wGT3X-BT, Actigraph LLC,Penascola,Florida, USA) around the non-dominant waist all the time, including sleep time, and removing it just for water-related activities (bathing or showering). The monitors were initialized using 60-s epochs, as described elsewhere [15].
Accelerometry data were analyzed using ActiLife 6.0 software (Actigraph LLC, Penascola, Florida, USA). Continuous 24-h accelerometer data were recorded from weekdays and weekend days and were analyzed separately. Total PA was obtained by weighting 5 times weekdays plus two times weekend days by two and dividing the result by seven, as previously reported [27]. Data were expressed as counts per minute (CPM). PA intensity was categorized using validated cut-points (Evensons) for children and adolescents. CPM were under 100 was considered sedentary time. CPM between 101 and 2295 was considered light PA. Moderate and vigorous physical activity were combined into moderate-to-vigorous PA (MVPA) when counts were over 2296 CPM.
Sleep was assessed using the accelerometer Actigraph wGT3X-BT, and the data was analysed using the Sadeh algorithm derived from fundamental research performed by Avi Sadeh et al. [28] .This algorithm was commonly used in younger adolescents [29](10 to 11 years old) .
Statistical analysis
All statistical analyses were two-tailed and a p value < 0.05 was considered as statistically significant. Variables were described using mean ± SD. Student’s t test was used for the comparison between groups (two independent groups test) and for the comparison within group (paired test) before and after the intervention. The change in each variable was calculated as the difference between post- and pre- intervention values for each subject.
Analyses of covariance (ANCOVA) were performed to assess the changes in anthropometric, biochemical and PA variables between usual care and intensive care groups after the adjustment for potential confounders: the studied variable at baseline, baseline BMI-SDS, sex and Tanner stage." Stata 12.0 (StataCorp, USA) for Windows was used in all the analyses.
Furthermore, we fitted a multivariable adjusted linear regression to examine the association of changes in leptin with changes in metabolic parameters and PA intensity.
Results
The study population includes 106 children with obesity (BMI-SDS 2.89 ± 1.05) (37.7% boys), with waist circumference over the sex and age-specific 90th percentile and a mean age of 11.31 ± 2.47 years old. At baseline, participants spent, on average, 997.9 (101.6) min/day on sedentary activities, including sleep time, 43.9 (23.4) min/day in MVPA activities, and 394.2 (95.9) min/day on light PA.
Most abdominal obese children (74.5%) do not fulfilled the WHO recommendations of being more than 60 min/day on MVPA at baseline. Participants were more active during weekdays compared to weekend days (Additional file 1).
Effectiveness of the lifestyle intervention
As expected, due to the randomization, participants in the two groups were similar for most of the clinical parameters at baseline, except for blood glucose levels (Table 1). The usual care group (n = 27) had significantly higher glucose levels compared with the intensive care group (n = 79) (p = 0.016). We did not find significant differences between groups regarding age, sex or Tanner stage.
The decrease in BMI-SDS (p = 0.029) and hip circumference (p = 0.019) was significantly higher in the intensive care group compared to the usual care group after adjusting for potential confounders (Table 1). Notably, participants in both groups achieved a significant reduction in waist circumference (Δ – 4.42 cm for usual care vs. Δ − 3.93 cm for intensive care group).
Regarding biochemical parameters, no differences were found between the two lifestyle interventions. A reduction in glucose (p = 0.004), insulin (p = 0.010), and leptin (p < 0.001) levels were observed in the intensive care group. Meanwhile, subjects in the usual care group did also significantly decrease glucose (p < 0.001) and leptin (p < 0.001) levels.
Changes in physical activity after the lifestyle intervention
As this is a randomized study, no differences were found on PA levels at baseline between groups (Additional file 2). No differences were found between the two lifestyle interventions in PA levels (Table 2). Interestingly, light PA significantly decreased in both the intensive and usual care group after the intervention. Participants from the intensive care group MVPA significantly increased from 43.5 min to 49.1 min (p = 0.024) in the intensive care group (Table 2). Interestingly, when all participants were analyzed in a multivariable-adjusted model, an inverse association between the percentage of change in MVPA and the percentage of change in leptin levels was found (B: -2.17; 95% CI: -3.73 to − 0.61). Moreover, changes in leptin were also associated with changes in anthropometric and metabolic parameters (Table 3).
Discussion
In this study the two lifestyle interventions reduced anthropometric indexes and lowered light PA in abdominal obese children. No significant differences were observed between intensive care and usual care in PA levels. Intensive care participants significantly increase MVPA levels after the intervention. Moreover, changes in MVPA were inversely associated with changes in leptin levels after the intervention.
Concerning objectively measurement PA levels, our participants spent 44 min/day on MVPA at baseline. These data are similar to those found in overweight and obese pediatric populations from Madrid, Spain (9 years old: 58.6 min/day in MVPA, and 15 years old: 49.3 min/day) [7]. Both studies reported an appropriate management of the accelerometers concerning the cut-off points and epoch rate used. It is worth mentioning that our participants were 11.31 years old and had abdominal obesity.
Evidence shows that PA levels are different between normal-weight and obese subjects. Besides, PA levels are higher in children than in adolescents and in boys than in girls, with accelerometer-measured MVPA ranging from 49.1 to 85.1 min/day in normal-weight children and adolescents [7, 30,31,32].
We addressed the achievement of WHO recommendations on MVPA levels in our population. Only 25% of participants accumulated more than 60 min/day of MVPA at baseline. When considering the day of the week, 32% of the participants achieved the recommendations during the weekdays but only 16% of them did it at weekends. The evidence regarding this point is controversial. Some authors recommend the promotion of PA during the weekdays because children have PA lessons at the school [33, 34], while many others have observed that children are more physically active during the weekends, probably due to the fact that they have more spare time [7, 35] at the weekends. In our study, we observed that abdominal obese children are more physically active during the weekdays and more sedentary during the weekends. This could be explained because during the weekdays children attend school-based activities and sport games after the classes as well. However, in the weekends they may not have that many organized activities, the opportunities of being physically active are less and thus they spend more time in sedentary activities [36].
In the literature we found several lifestyle intervention studies that examined both adiposity indexes (i.e. BMI-SDS) and objectively measured PA levels [15, 16, 18] in obese children. First, a family-based behavioral program in 210 families of obese children achieved a reduction in − 0.1 units of BMI-SDS but did not report changes in MVPA after 12-week intervention [15]. Another study performed in 41 Latino families of obese children did not observe changes in either BMI-SDS or MVPA levels after a 6 months intervention [16]. In contrast, Hughes et al. (2008) performed a controlled trial with an intervention based on a traffic light diet and advice to increase PA on 1 h per day [18]. They found significant changes in sedentary behavior and light PA after 6 months of follow-up in the intervention group, but no changes were found in MVPA levels. Two more trials reported no changes in MVPA despite using novel approaches, such as active video games and motivational interviewing treatment [4, 17].
To our knowledge, this is the first intervention program that achieved a significantly increase in MVPA (+ 5.5 min/day,) in intensive care subjects. We did not found differences in PA between intervention groups. Intensive care subjects were under a moderate hypocaloric Mediterranean diet and achieved a successful weight loss (Δ BMI-SDS = − 0.51) that was higher than usual care group. It has been described that the combination of PA and Mediterranean diet might provide greater health benefits that those acquired separately in a recent meta-analysis [37]. In addition, a close follow-up of the participants (i.e number of visits and duration) and family enrolment are important issues in regard to the effectiveness of a paediatric intervention [38].
Leptin is a peptide hormone secreted by adipose tissue which plays a central role in regulating human energy homeostasis [24, 25]. Leptin levels are higher in obese adult and children, but physical activity might effectively reduce adipose tissue and lower leptin levels [26]. Obese children in this study reduced leptin levels after the intervention. Moreover, an inverse association between changes in MVPA and leptin levels was observed. Similar findings were reported in other intervention studies using objectively measured PA levels in adults [14].
The strengths of our study include: [1] the longitudinal design; [2] the effectiveness of the intervention with obese participants achieving a substantial weight loss; [3] the use of objectively measured physical activity. On the other hand, the diversity in important variables such as age and pubertal stage of the studied population is a limitation of this study. In order to control these potential confounders, sex, age and Tanner stages were included in the statistical models. Another limitation could be a possible lack of statistical power for PA analysis between the two lifestyle interventions.
Conclusion
In conclusion, the two lifestyle interventions were successful, since a reduction in anthropometric indexes and light PA in abdominal obese children was achieved. No significant differences were observed between intensive care and usual care groups in regard to PA. Intensive care participants following a hypocaloric Mediterranean diet significantly increased MVPA. Changes in MVPA were inversely associated with changes in leptin levels after the intervention.
Abbreviations
- BMI:
-
body mass index
- BMI-SDS:
-
body mass index standard deviation
- CPM:
-
counts per minute
- HOMA-IR:
-
homeostasis model assessment for insulin resistance
- MVPA:
-
moderate to vigorous physical activity
- PA:
-
physical activity
- WHO:
-
world health organization
References
Morell-Azanza L, García-Calzón S, Rendo-Urteaga T, Martin-Calvo N, Chueca M, Martínez JA, et al. Serum oxidized low-density lipoprotein levels are related to cardiometabolic risk and decreased after a weight loss treatment in obese children and adolescents. Pediatr Diabetes. 2017;18(5):392–8.
Bassali R, Waller JL, Gower B, Allison J, Davis CL. Utility of waist circumference percentile for risk evaluation in obese children. Int J Pediatr Obes. 2011;5:97–101.
Velásquez-Rodriguez CM, Velásquez-Villa M, Gómez-Ocampo L, Bermudez-Cardona L. Abdominal obesity and low physical activity are associated with insulin resistance in overweight adolescents: a cross-sectional study. BMC Pediatr. 2014;14:1–9.
Maddison R, Foley L, Mhurchu CN, Jiang Y, Jull A, Prapavessis H, et al. Effects of active video games on body composition: a randomized. Am J Clin Nutr. 2011;94:156–63.
Who WHO. Global recommendations on physical activity for health. Geneva World Heal Organ. 2010;60.
Borde R, Smith JJ, Sutherland R, Nathan N, Lubans DR. Methodological considerations and impact of school-based interventions on objectively measured physical activity in adolescents: a systematic review and meta-analysis. Obes Rev. 2017;18:476–90.
Laguna M, Ruiz JR, Gallardo C, García-Pastor T, Lara MT, Aznar S. Obesity and physical activity patterns in children and adolescents. J Paediatr Child Health. 2013;49:942–9.
Rendo-Urteaga T, García-Calzón S, Martínez-Ansó E, Chueca M, Oyarzabal M, Azcona-Sanjulián MC, et al. Decreased cardiotrophin-1 levels are associated with a lower risk of developing the metabolic syndrome in overweight/obese children after a weight loss program. Metabolism. 2013;62:1429–36.
Marqués M, Moleres A, Rendo-Urteaga T, Gómez-Martínez S, Zapatera B, Romero P, et al. Design of the nutritional therapy for overweight and obese Spanish adolescents conducted by registered dieticians: the EVASYON study. Nutr Hosp. 2012;27:165–76.
Jáuregui A, Villalpando S, Rangel-Baltazar E, Lara-Zamudio YA, Castillo-García MM. Physical activity and fat mass gain in Mexican school-age children: a cohort study. BMC Pediatr. 2012;12.
Sirico F, Bianco A, D’Alicandro G, Castaldo C, Montagnani S, Spera R, et al. Effects of physical exercise on adiponectin, leptin, and inflammatory markers in childhood obesity: systematic review and meta-analysis. Child Obes. 2018;14:207–17.
Carnier J, Lofrano MC, Prado WL, Caranti DA, De Piano A, Tock L, et al. Hormonal alteration in obese adolescents with eating disorder: effects of multidisciplinary therapy. Horm Res. 2008;70:79–84.
Elia CA, Carnier J, Buengo C, Campos R, Sanchez P, Clemente A, et al. Effects of different physical exercises on leptin concentration in obese adolescents. Sport Med. 2014:164–71.
Nurnazahiah A, Lua PL, Shahril MR. Adiponectin, leptin and objectively measured physical activity in adults: a narrative review. Malaysian J Med Sci. 2016;23:7–24.
Davis AM, Daldalian MC, Mayfield CA, Dean K, Black WR, Sampilo ML, et al. Outcomes from an urban pediatric obesity program targeting minority youth: the healthy hawks program. Child Obes. 2013;9:492–500.
Boudreau ADA, Kurowski DS, Gonzalez WI, Dimond MA, Oreskovic NM. Latino families, primary care, and childhood obesity: a randomized controlled trial. Am J Prev Med. 2013;44:S247–57.
Taylor RW, Cox A, Knight L, Brown DA, Meredith-Jones K, Haszard JJ, et al. A tailored family-based obesity intervention: a randomized trial. Pediatrics. 2015;136:281–9.
Hughes AR, Stewart L, Chapple J, McColl JH, Donaldson MDC, Kelnar CJH, et al. Randomized, controlled trial of a best-practice individualized behavioral program for treatment of childhood overweight: Scottish childhood overweight treatment trial (SCOTT). Pediatrics. 2008;121:e539–46.
Mead E, Brown T, Rees K, Lb A, Whittaker V, Jones D, et al. Diet , physical activity and behavioural interventions for the treatment of overweight or obese children from the age of 6 to 11 years ( review ) diet , physical activity and behavioural interventions for the treatment of overweight or obese children from. Cochrane Database Syst Rev. 2017.
Sobradillo B, Aguirre A, Uresti U, Bilbao A, Fernández-Ramos C, Lizarraga A, et al. Curvas y tablas de crecimiento. Estudios longitudinal y transversal Bilbao: Fundación Faustino Orbegozo Eizaguirre [Internet]. Isbn 84-607-9967-0. 2004. 1-31 p.
Serra Majem L, Aranceta Bartrina J, Ribas Barba L, Pérez Rodrigo C, García Closas R. Estudio enKid: objetivos y metodología. Crecimiento y desarrollo. Estudio enKid, vol. 4: Masson S.A. Barcelona; 2000.
De Miguel-Etayo P, Muro C, Santabárbara J, López-Antón R, Morandé G, Martín-Matillas M, et al. Behavioral predictors of attrition in adolescents participating in a multidisciplinary obesity treatment program: EVASYON study. Int J Obes. 2016;40:84–7.
Ford AL, Hunt LP, Cooper A, Shield JPH. What reduction in BMI SDS is required in obese adolescents to improve body composition and cardiometabolic health? Arch Dis Child. 2010;95:256–61.
Knop C, Singer V, Uysal Y, Schaefer A, Wolters B, Reinehr T. Extremely obese children respond better than extremely obese adolescents to lifestyle interventions. Pediatr Obes. 2015;10:7–14.
Ojeda-Rodríguez A, Zazpe I, Morell-Azanza L, Chueca MJ, Azcona-Sanjulian MC, Marti A. Improved diet quality and nutrient adequacy in children and adolescents with abdominal obesity after a lifestyle intervention. Nutrients. 2018;10.
Burke JP, Hale DE, Hazuda HP, Stern MP. A quantitative scale of acanthosis nigricans. Diabetes Care. 1999;22:1655–9.
Konstabel K, Veidebaum T, Verbestel V, Moreno LA, Bammann K, Tornaritis M, et al. Objectively measured physical activity in European children: the IDEFICS study. Int J Obes. 2014;38:S135–43.
Sadeh A, Sharkey KM, Carskadon MA. Activity-based sleep-wake identification: an empirical test of methodological issues. Sleep. 1994;17:201–7.
Kinder JR, Lee KA, Thompson H, Hicks K, Topp K, Madsen KA. Validation of a hip-worn accelerometer in measuring sleep time in children. J Pediatr Nurs. 2012;27:127–33.
García-Cervantes L, Rodríguez-Romo G, Esteban-Cornejo I, Cabanas-Sanchez V, Alfonso AD, Castro-Piñero J, et al. Perceived environment in relation to objective and self-reported physical activity in Spanish youth. The UP&DOWN study. J Sports Sci. 2016;34:1423–9.
Martinez-Gomez D, Tucker J, Heelan KA, Welk GJ, Eisenmann JC. Associations between sedentary behavior and blood pressure in young children. Arch Pediatr Adolesc Med. 2009;163:724–30.
Moliner-Urdiales D, Ruiz JR, Ortega FB, Rey-Lopez JP, Vicente-Rodriguez G, Espãa-Romero V, et al. Association of objectively assessed physical activity with total and central body fat in Spanish adolescents; the HELENA study. Int J Obes. 2009;33:1126–35.
Brooke HL, Atkin AJ, Corder K, Brage S, van Sluijs EM. Frequency and duration of physical activity bouts in school-aged children: a comparison within and between days. Prev Med Reports. 2016;4:585–90.
De Baere S, Lefevre J, De Martelaer K, Philippaerts R, Seghers J. Temporal patterns of physical activity and sedentary behavior in 10-14 year-old children on weekdays. BMC Public Health. 2015;15:1–13.
Dishman RK, Motl RW, Saunders R, Felton G, Ward DS, Dowda M, et al. Self-efficacy partially mediates the effect of a school-based physical-activity intervention among adolescent girls. Prev Med (Baltim). 2004;38:628–36.
Gubelmann C, Marques-Vidal P, Bringolf-Isler B, Suggs LS, Vollenweider P, Kayser B. Correlates of weekday compliance to physical activity recommendations in Swiss youth non-compliant in weekend days. Prev Med Reports. 2018;9:86–91.
Malakou E, Linardakis M, Armstrong MEG, Zannidi D, Foster C, Johnson L, et al. The combined effect of promoting the Mediterranean diet and physical activity on metabolic risk factors in adults: a systematic review and meta-analysis of randomised controlled trials. Nutrients. 2018;10.
Berge JM, Everts JC. Family-based interventions targeting childhood obesity: a meta-analysis. Child Obes. 2011;7:110–21.
Acknowledgments
We thank all the children and families in the trial for their enthusiastic and maintained collaboration, and other investigators of IGENOI group for their participation in the recruitment process and the acquisition of the data. AOR is fully acknowledged for the fellowships to Asociación de Amigos de la Universidad de Navarra (ADA). LMA and the research leading to these results has received funding from “la Caixa” Banking Foundation.
Funding
The IGENOI study was supported by the MERCK foundation grant and the Laboratories ORDESA (Sant Boi de Llobregat; Barcelona, España)-FEI-AEP grant. None of the sponsors participated in the design and conduct of the study; collection, management, analysis, and interpretation of the data; or preparation, review, or approval of the manuscript.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
The authors’ contributions were as follows: LMA contributed to the data collection, performed the statistical analyses and wrote the manuscript; AOR contributed to the data collection. AOE contributed to the data analysis; NMC, MC, AM, CAS were responsible of the follow-up, design, financial management and editing of the manuscript. All the authors actively participated in the manuscript preparation, as well as revise and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study protocol was performed in accordance with the ethical standards laid down in the 2013 Declaration of Helsinki (Fortaleza, Brasil, October 2013) and was approved by the Ethics Committee of the University of Navarra (Reference number 044/2014).
Informed assent was obtained from every child and all parents and/or legal guardians signed an informed consent according to the Helsinki declaration.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional files
Additional file 1:
Table S1. Physical activity characteristics measured by accelerometry before lifestyle intervention in children with abdominal obesity (N = 106). (DOCX 13 kb)
Additional file 2:
Table S2. Baseline characteristics in participants with abdominal obesity divided by type of intervention. (DOCX 14 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Morell-Azanza, L., Ojeda-Rodríguez, A., Ochotorena-Elicegui, A. et al. Changes in objectively measured physical activity after a multidisciplinary lifestyle intervention in children with abdominal obesity: a randomized control trial. BMC Pediatr 19, 90 (2019). https://doi.org/10.1186/s12887-019-1468-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-019-1468-9