Abstract
Background
Historically, bifidobacteria were the dominant intestinal bacteria in breastfed infants. Still abundant in infants in developing nations, levels of intestinal bifidobacteria are low among infants in developed nations. Recent studies have described an intimate relationship between human milk and a specific subspecies of Bifidobacterium, B. longum subsp. infantis (B. infantis), yet supplementation of breastfed, healthy, term infants with this organism, has not been reported. The IMPRINT Study, a Phase I clinical trial, was initiated to determine the safety and tolerability of supplementing breastfed infants with B. infantis (EVC001).
Methods
Eighty mother-infant dyads were enrolled in either lactation support plus B. infantis supplementation (BiLS) or lactation support alone (LS). Starting with Day 7 postnatal, BiLS infants were fed 1.8–2.8 × 1010 CFU B. infantis EVC001 daily in breast milk for 21 days. Mothers collected fecal samples, filled out health questionnaires, and kept daily logs about their infants’ feeding and gastrointestinal symptoms from birth until Day 61 postnatal. Safety and tolerability were determined from maternal reports.
Results
There were no differences in the mean gestational age at birth, weight 1 and 2 months postnatal, and breast milk intake between groups. The mean Log10 change in fecal Bifidobacterium from Day 6 to Day 28 was higher (p = 0.0002) for BiLS (6.6 ± 2.8 SD) than for LS infants (3.5 ± 3.5 SD). Daily stool number was higher (p < 0.005) for LS and lower (p < 0.05) for BiLS infants during supplementation than at Baseline. During supplementation, watery stools decreased and soft stools increased by 36% over baseline in BiLS infants (p < 0.05) with no significant changes in stool consistency for the LS infants. None of the safety and tolerability endpoints, including flatulence, bloody stool, body temperature, ratings of gastrointestinal symptoms, use of antibiotics or gas-relieving medications, infant colic, jaundice, number of illnesses, sick doctor visits, or diagnoses of eczema were different for the groups at any point.
Conclusions
The B. infantis EVC001 supplement was safely consumed and well-tolerated. Stools were fewer and better formed in infants in the BiLS group compared with LS group. Adverse events were those expected in healthy infants and not different between groups.
Trial registration
ClinicalTrials.gov NCT02457338. Registered May 27, 2015.
Similar content being viewed by others
Background
Breast milk not only provides nutrition but has evolved to protect and support development of the vulnerable infant. Breast milk delivers a wide spectrum of biologically active molecules that aid in the development and maturation of the gut, and the innate and acquired immune systems, and support the growth of protective intestinal microbiota. Advances in mass spectrometry have revealed detailed chemical structures of the complex and diverse free and conjugated glycans in human milk [1]. Specifically, human milk oligosaccharides (HMO), the third most abundant component in human milk (~10–20 g/L) [2, 3], are a group of complex sugars that are non-digestible by the human infant and support the competitive growth of protective bifidobacterial strains within the intestine [4]. Bifidobacteria were first identified in the feces of breastfed infants by Henry Tissier at the Pasteur Institute in 1900 [5]. Recent research has demonstrated that the gut of the breastfed infant is dominated by strains of Bifidobacterium until cessation of breastfeeding [6, 7].
Recent breakthroughs in microbiology have led to a detailed description of the natural colonization of a protective subspecies of Bifidobacterium, (B. infantis) in breastfed infants, and the role of human milk in delivering complex HMO as natural prebiotics to selectively enrich the growth and function of B. infantis. Unlike other bifidobacterial strains, B. infantis is unique in its ability to consume HMO as its sole source of carbon through specific solute binding proteins, transporters and glycosidic hydrolases that are encoded in its genome [8,9,10,11,12,13,14]. The subsequent effects of HMO metabolism by B. infantis include its production of acetate and lactate; its direct binding to intestinal cells; and its stimulation of anti-inflammatory and inhibition of pro-inflammatory cytokines by intestinal cells [15,16,17,18]. In animal models of necretozing enterocolitis (NEC), B. infantis supplementation was found to attenuate the inflammation [19] and increase intestinal permeability [20] associated with NEC.
The dominance of fecal Bifidobacterium and B. infantis has declined over recent decades in developed countries [21, 22]. For example, in a U.S. cohort of exclusively breastfed infants, 30% of the total gut microbiome was represented by the genus Bifidobacterium, whereas only 13% of total intestinal bifidobacterial populations was represented by the subspecies B. infantis. On the other hand, in a trial conducted in Bangladeshi breastfed term infants, 77% of the total gut microbiome was represented by the genus Bifidobacterium and 57% was represented by B. infantis [21].
Differences in postnatal intestinal microbial colonization may explain in part the higher incidence of immune-mediated diseases, such as allergy and asthma, in children born by cesarean section compared with those born vaginally [23,24,25,26,27], and the increase in type 1 diabetes and food allergies in children in developed countries [28]. Thus, the early colonization and establishment of a healthy microbiome in infancy is critical for establishing life-long health.
One of the main objectives of the Infant Microbiota Probiotic Intake (IMPRINT) Study was to determine the safety and tolerability of supplementing breastfed, term infants with B. infantis EVC001. Although B. infantis was reported to be well-tolerated when provided to premature infants, such data have not yet been reported for healthy term infants [29]. In this Phase I clinical trial, safety and tolerability were determined by measuring the changes in infant weight, parental reports of gastrointestinal (GI) symptoms, illnesses, use of antibiotics or gas-relieving medications, and sick doctor visits throughout the study duration. Additional outcome measures related to infant fecal microbial composition were prespecified in the study protocol and will be reported elsewhere.
Methods
Study population
Between January 2015 and April 2016, healthy women who were pregnant or who had recently delivered healthy term infants and lived within Yolo and Sacramento counties in California were recruited and subsequently provided written informed consent to enroll in the study. Enrollment criteria for study participation were based on limiting the number of confounding variables that could influence the infant gut microbiome. Inclusion and exclusion criteria for mothers were as follows: women 21 to 45 years of age, in their third trimester of pregnancy or had delivered an infant within the past 4 days, planned to exclusively breastfeed their infants for at least the first 3 months postnatal, lived in a developed nation for the past 10 years, did not plan to administer probiotic supplements to their infants during the study duration unless they were allocated to the B. infantis group, who had not been diagnosed with any chronic metabolic disease or obesity, and who were non-smoking. Medications during labor, including antibiotics, were recorded but not used as an exclusion criterion. Inclusion and exclusion criteria for infants born to qualified mothers included gestational age at birth ≥37 weeks, birth without medical complications (such as respiratory distress syndrome, birth defects, and infection), no exposure to any oral or intravenous antibiotics 72 h postnatal, and no consumption of infant formula 24 h prior to the Day 7 postnatal at-home lactation consultation visit.
Study design
This IMPRINT study was a parallel, partially-randomized, controlled 2-month trial. The University of California Davis Institutional Review Board approved all aspects of the study (IRB #: 631,099). This trial was registered on ClinicalTrials.gov Identifier: NCT02457338. Prior to the initiation of the study, three separate randomization schemes were generated using a random number generator in Excel. Participants were stratified to one of the three randomization schemes based on mode of delivery—vaginal delivery, cesarean section (time of membrane rupture before delivery ≤6 h), or cesarean section (time of membrane rupture before delivery >6 h). Stratified randomization was utilized because mode of delivery, as well as the time when membranes rupture before cesarean section delivery, have been shown to influence early infant intestinal microbial colonization [30]. Randomization to lactation support alone (LS) or lactation support plus B. infantis supplementation (BiLS) was in a 1:1 ratio for all three randomization schemes in blocks of ten. After receiving informed consent for the infant, the clinical coordinator assigned enrollment identification numbers according to the schedule. The first fifteen participants enrolled in the study were not included in the stratified randomization schedule due to unavailability of the B. infantis product during the trial period. The first eight infants enrolled in the study were assigned to the LS group, but three had withdrawn or were screen-failed and thus only five infants received the intervention. The subsequent seven infants were assigned to the BiLS group, but three had withdrawn or were screen-failed and thus only four infants received the intervention. Parity and mode of delivery were not different between the two assigned groups for these fifteen participants.
After meeting major postpartum study criteria at enrollment (Day 3 or 4), infants were randomized into the BiLS or LS group. On Day 7, infants were screened for the consumption of infant formula within the past 24 h. On Days 3 or 4, 7, 15, 22, 33, and 61, study personnel visited mothers’ homes to conduct study procedures. On all six visits, mothers filled out questionnaires about their and their infants’ health, GI symptoms, occurrence of fever, illness, and number and reasons for sick doctor visits. Mothers collected infant stool samples from their infants’ diapers before Day 6 (baseline) and on Days 10, 14, 21, 25, 29, 32, 40, 50, and 60 and stored them in their kitchen freezers. Infant weight was measured by study personnel with a digital infant scale (Tanita) on Days 33 and 61. Participants received breastfeeding support at their homes by the study’s internationally board certified lactation consultant (IBCLC) prenatally and on Days 3 or 4, 7, and 15. On Days 22, 33, and 61 postnatal, study personnel transported samples from participants’ homes to the UC Davis campus on dry ice and stored at −80 °C.
Infants randomized into the BiLS group received one daily serving of B. infantis in their homes for 21 consecutive days starting on Day 7 and continuing through Day 27. During the Day 7 lactation consultation visit, mothers were trained by their lactation consultant to mix each B. infantis serving with 5 mL of their breast milk in a plastic medicine cup, and to syringe or finger-feed the mixture to their infants. Each daily serving of B. infantis EVC001 (ATCC accession Number SD-7035) consisted of one 625-mg sachet, delivering a minimum 156 mg of live bacteria (minimum 1.8 × 1010 CFU) plus 469 mg of lactose as the excipient. The 18 billion CFU per sachet was the minimum guaranteed CFU count as determined by the product specification. Because this is a live microorganism there is potential loss over time. As such, the sachets were produced with a 50% overage to account for potential losses during packaging and long term storage. This means the range of the dose delivered was 18–28 billion CFU per dose. The product was stored in the freezer at −20 °C and suffered no loss from the first infant enrolled to the last infant enrolled. Mothers received 21 sachets, plus four extra sachets that were to be used in the event of damage or misplacement. All sachets were kept frozen in mothers’ kitchen freezers until time of use, and mothers were instructed to keep all used and unused sachets provided. Compliance was assessed on Days 22 and 33 by counting and recording the number of empty B. infantis sachets.
Infant stool samples without labeled group assignments were provided to Evolve BioSystems, Inc. (Davis, CA USA) for the analysis of total infant fecal Bifidobacterium. Group assignments were unblinded to Evolve BioSystems, Inc. post microbial analysis. For DNA extraction, approximately 100 mg of the frozen collected stool samples were extracted using the Zymo Research Fecal DNA kit, according to the manufacturer’s instructions. Polymerase chain reaction (PCR) amplification was conducted using methods as previously described, with minor modifications [31]. Briefly, 5 μL of extracted DNA were used as template for a 20-μL reaction, using primers Bif F (5′-GCGTGCTTAACACATGCAAGTC-3′), Bif R (5′- CACCCGTTTCCAGGAGCTATT-3′), and Bif P (5′-TCACGCATTACTCACCCGTTCGCC-3′). Reactions were carried out with Taqman Universal MasterMix II with Uracil-N glycosylase (Life Technologies) [31] using a Life Technologies QuantStudio 3 Real-Time PCR machine. Samples were assayed in duplicate. A standard curve was prepared from Bifidobacterium longum subsp. infantis EVC001 using the same extraction protocol as used for the stool samples for quantification of fecal Bifidobacterium.
Infant gastrointestinal health and tolerability
Infant GI tolerability during B. infantis EVC001 supplementation was assessed by mothers on a daily basis starting with Day 1 (or retrospectively if mothers were enrolled on Day 4 postnatal) until Day 61. On each day, mothers recorded the following information about their infants in daily logs: consumption of breast milk defined as suckling at the breast for at least five minutes or consuming any volume in a bottle; intake of other liquids or solids; amount of infant formula consumed; intake of probiotics that were not used in the study; intake of any oral antibiotics or administration of intravenous antibiotics; intake of any over-the-counter or prescribed medications; intake of vitamins, supplements, and herbs; number of spit-ups—less than five, five to ten, or more than ten; number of stools; consistency of stools using a modified Amsterdam infant stool scale—watery, soft, formed, hard [32] (Additional file 1); blood in the stool; body temperature above 100.3 °F; ratings of GI-related symptoms using a continuous scale of 0 (“not noticeable”) to 10 (“most severe”), including general irritability (“how irritable was your baby?”), upset (“if your baby vomited or spit up, how upset was he/she after?”), and discomfort (“rate your baby’s discomfort in passing stool or gas”). Mothers also rated the frequency of their infant’s flatulence as “never, sometimes, often, very often” on a daily basis. Mothers filled out questionnaires to report any adverse events experienced by their infants during each at-home visit (Days 7, 15, 22, 33 and 61). Mothers recorded the following about their infants on weekly questionnaires: episodes of colic—defined as crying for more than 3 h per day for at least 3 days per week [33], eczema diagnosis by a primary-care provider, number of sick doctor visits, illnesses, and medications used (Additional file 2).
Statistics
Data from the daily logs and retrospective questionnaires were binned into three time periods: baseline (Days 1–6), intervention (Days 7–27), and post-intervention (Days 28–61). For retrospective questionnaires, Day 7 data were binned as baseline. Means and proportions were calculated for continuous variables and categorical variables across all three time periods. Proportions for binary categorical variables were calculated as number of days reported/total number of days in each study period, and number of infants/total number of infants in each intervention group. The calculated values were multiplied by 100 to generate percentages.
For this Phase I study, the sample size was based on differences in infant fecal B. infantis, which was calculated using the means and standard deviations from a previous study on breastfed infants [22]. To detect a standardized inter-group difference of 1.3 z-scores in infant fecal B. infantis with 90% power and α = 0.05, assuming equal standard deviations with a 20% attrition rate, 30 infants were needed in each group. Intent-to-treat analysis was performed of mother-infant dyads who initiated the study by Day 7 when final screening criteria were met. Statistical analyses were performed in IBM SPSS Statistics version 24 and figures were generated in PRISM v.7. Statistical significance was considered as p < 0.05. Continuous data were checked visually for normality with histograms and quintile-quintile plots as well as numerically with the Shapiro-Wilk test and equality of variances using Levene’s statistic. Non-normal data were Log10 transformed and confirmed again for normality prior to conducting parametric analyses.
To determine differences in total infant fecal Bifidobacterium between groups, Mann-Whitney U test was conducted using GraphPad Prism v7. Baseline demographics, maternal health, pregnancy history, and infant feeding and GI symptoms were compared between the LS and BiLS groups using the Pearson Chi-square Test for Independence (categorical variables), Mann-Whitney U Test, or one-way ANOVA (continuous variables). For normally-distributed continuous data, repeated measures ANOVA was performed with group and time as fixed factors, parity as the covariate, and group by time as the interaction term. If time was significant, multiple comparison post-hoc analysis with Bonferroni correction was carried out to compare baseline, intervention, and post-intervention data. Group differences in stool consistency, flatulence, and spitting-up were analyzed by logistic regression.
Results
Study participation
One-hundred and eight mothers were screened for eligibility to participate in the study. Eighty women met initial study criteria, of which fifteen were non-randomly assigned and sixty-five were randomly assigned into the LS (n = 39) and BiLS (n = 41) groups (Fig. 1). Screen failures were due to the use of infant formula within 24 h of the Day 7 lactation consultation visit. Mothers withdrew from study participation for feeling overwhelmed with a new infant and/or unexpectedly discontinuing breastfeeding due to difficulty with lactation (n = 8). Sixty-eight mother-infant dyads met final study criteria. Data for all participants in each group (n = 34 per group) are reported except for the post-intervention period for the one participant who was enrolled into the LS group and withdrew on Day 26 postnatal. The overall attrition rate for this study was 15%, consistent with probiotic studies in healthy, breastfed, term infants [34, 35]. Based on study compliance assessments, of the 21 desired once-daily servings of B. infantis, 94% of the BiLS infants consumed 20–25 daily servings and 6% consumed 13–19 daily servings. No infant received more than one serving per day.
Maternal characteristics
Maternal age at enrollment (Additional file 3: Table S1), weight gain during pregnancy, time when lactogenesis II ensued (< 72 h), and time when membranes ruptured prior to delivery were not significantly different between the LS and BiLS groups (Additional file 4: Table S2). However, women enrolled in the BiLS group had a higher pre-pregnancy BMI than women enrolled in the LS group (p < 0.05). There were significantly (p < 0.01) more multiparous women (n = 20, BiLS; n = 8, LS) in the BiLS group and fewer primiparous women (n = 14, BiLS; n = 26, LS) compared with the LS group (Additional file 4: Table S2). These differences were not a result of the non-random enrollment of the first fifteen participants.
Infant characteristics
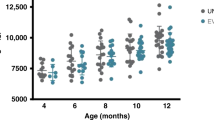
Infant birth weight, birth length, gestational age at birth, and gender were not different between groups (Table 1). Infant weight was not different between groups at birth, or Days 33 and 61 (Additional file 5: Figure S1).
Infant diet
According to maternal reports, the mean number of breastfeeds at the breast or with breast milk bottles by their infants was the same for intervention groups at each time period (Additional file 6: Figure S2). The number of days, number of infants who were mixed-fed (consumed some amount of infant formula), or the mean amount of infant formula consumed were not significantly different between the BiLS and LS groups (Additional file 7: Table S3). One mother in the BiLS group and two mothers in the LS group reported feeding her infant non-study probiotics during the post-intervention period (Additional file 7: Table S3). The intake of vitamin D by infants was not different between the intervention groups (data not shown).
Parity did not influence any of the feeding variables except for vitamin D intake during the intervention and post-intervention periods (p < 0.01 for both). Primiparous women fed their infants vitamin D 30% of the intervention period and 38% of the post-intervention period compared with multiparous mothers feeding only 7% and 6% of the intervention periods, respectively. Additionally, infant intake of vitamin D significantly (p < 0.01) increased over time for both BiLS and LS groups in primiparous (p < 0.0005) but not multiparous mothers.
Infant gastrointestinal health and tolerability
The number of infant bowel movements during the baseline period was the same for the BiLS and LS groups but was significantly (p < 0.0005) different during the intervention (BiLS: mean, 3.2/d, range, 0.50–7.2; LS: mean, 5.5/d, range, 2.6–10.6), and post-intervention (BiLS: mean, 1.7/d, range, 0.30–4.8); LS: mean, 4.4/d, range, 0.97–9.9) periods (Fig. 2). The mean number of bowel movements was not only different between groups (p < 0.01) but also different across time within each group (p < 0.0005). Parity was unrelated to the reported mean number of bowel movements per day across all three time periods. Maternal reports for the proportion of watery and soft stools during the intervention period for infants in the BiLS vs. the LS group (0.20 vs. 0.33) and (0.79 vs. 0.67), respectively, were not statistically significant (Fig. 3a). Yet, the percentage of watery stools decreased from baseline to the intervention period by 36% in infants assigned to the BiLS group (p < 0.05) and only by 7% in infants assigned to the LS group. As expected, the percentage of soft stools increased from baseline to the intervention period by 36% in infants assigned to the BiLS group (p < 0.05) but only increased by 7% in infants assigned to the LS group (Fig. 3b). There was no difference in the change in consistency from intervention to post-intervention between the groups. Stool consistency was also not influenced by parity.
Number of infant stools per day. Mean ± SD of reported number of daily infant stools for the LS (red dot plot) and BiLS (blue dot plot) groups during the Baseline, Intervention, and Post-intervention periods. n = 34 for each group during the Baseline and Intervention periods, and n = 33 for the LS, and n = 34 for the BiLS groups during the Post-intervention period. Different superscripts represent significant differences within and between interventions. There was a significant time effect (p < 0.01), time*trt interaction (p < 0.0005), and intervention effect (p < 0.0005). Based on multiple comparison post hoc analysis with Bonferroni corrections, compared with baseline the mean number of stools increased (b p < 0.0005) during the intervention period for the LS group and decreased (c p < 0.05) for the BiLS group. During the Post-intervention period, the mean number of stools returned to Baseline levels for the LS group and decreased from the Intervention period for the BiLS group (d p < 0.0005)
Infant stool consistency. a Mean + SD of the proportion in reported infant stool consistency for the LS (red bar) and BiLS (blue bar) groups during the Baseline, Intervention, and Post-intervention periods. n = 34 for each group during the Baseline and Intervention periods, n = 33 for the LS group, and n = 34 for the BiLS group during the Post-intervention period. b Mean ± SD of the change in the percentage of reported infant stool consistency for the LS (red bar) and BiLS (blue bar) groups for difference between Intervention and Baseline (Intervention – Baseline), and Post-intervention and Intervention (Post-intervention – Intervention) periods. n = 34 for each group for Intervention – Baseline, and n = 33 for the LS and n = 34 for the BiLS groups for Post-intervention – Intervention. *p < 0.05
Infant illness and adverse events were not different between BiLS and LS groups (Table 2). The types of illnesses and reasons for any sick doctor visits reported by mothers are shown in Additional file 8: Table S4. None of the infants in the BiLS group received antibiotics; two infants in the LS group received intravenous antibiotics (at birth and Days 10–18). The number of spit-ups per day as less than five, five to ten, and more than ten were not significantly different at any time period between the two groups (Additional file 9: Figure S3). There were no differences in mean irritability scores (Fig. 4a), mean scores for discomfort after spit-ups (Fig. 4b), or mean scores for discomfort when passing gas or stool (Fig. 4c) between the groups at any time period. Interestingly, maternal parity was significantly associated with rating of irritability. Higher irritability scores were rated by primiparous than multiparous mothers during the baseline period (2.6 and 1.3, respectively, p < 0.01) and intervention period (2.5 and 1.7, respectively, p < 0.05) but not during the post-intervention period. There were no differences in infant flatulence between groups (Additional file 10: Figure S4).
Infant tolerability scores. Mean ± SD of reported tolerability scores (red dot plot) and BiLS (blue dot plot) groups during the Baseline, Intervention, and Post-intervention periods. n = 34 for each group during the Baseline and Intervention periods, and n = 33 for the LS and n = 34 for the BiLS groups during the Post-intervention period. a Infant irritability, (b) infant upset after spit-ups, and (c) infant discomfort in passing gas or stool
Fecal Bifidobacterium
To correlate safety endpoints with the supplementation of B. infantis EVC001 and colonization of the genus Bifidobacterium in the infant gut, we compared the mean differences for total fecal Bifidobacterium from baseline to the end of the supplementation period for the LS and BiLS groups. The mean Log10 change in total fecal Bifidobacterium from Day 6 to Day 28 was significantly (p = 0.0002) higher for infants in the BiLS group (6.6 ± 2.8 SD) compared with infants in the LS group (3.5 ± 3.5 SD). The median Log10 change from Day 6 to Day 28 for total fecal Bifidobacterium was median 0.0 for infants in the LS group and 7.5 for infants in the BiLS group (p = 0.0002).
Discussion
The hygiene hypothesis suggests that changes in colonizing microbes related to a developed or Western lifestyle have long-term impacts on the risks of developing allergic, inflammatory, and autoimmune diseases [21,22,23,24,25,26,27,28]. In an effort to shift the intestinal microbiome toward beneficial populations in early infancy, the Infant Microbiota Probiotic Intake (IMPRINT) Study was designed to determine the safety and tolerability in breastfed term infants supplemented with B. infantis. We found that B. infantis EVC001 was well-tolerated and safely consumed by healthy term infants for 21 consecutive days. All adverse events reported by mothers enrolled in the study were typical of infants this age and the incidences were not increased by the B. infantis feedings.
To assess infant GI function as a metric of tolerability, mothers recorded the number of bowel movements and the consistency of the first bowel movement produced by their infants each day during the two-month study period. Based on daily reports, the mean number of bowel movements passed by infants in both groups are consistent with other reports on the frequency of bowel movements in breastfed infants. The number of bowel movements in breastfed infants has been found to be highly variable and to decrease with postnatal age, with a mean of about 4 per day and a median of about 4 per day and a range of 0.3 to 8.5 per day during the first month of age [36,37,38,39,40]; and a mean of 1.8 per day and median of 1.8 per day at 5 months of age [36,37,38,39,40,41,42]. Thus, the frequency in bowel movements of infants in the LS and BiLS groups was within normal a range.
The infants in the BiLS group passed fewer daily stools than infants in the LS group. Additionally, infants in the BiLS group were reported to pass “soft” stools more often and “watery” stools less often compared with infants in the LS group. These data may reflect maturation of the gut in response to B. infantis supplementation. Compared with other reports, the LS group produced bowel movements more similar to one-month-old infants, and the BiLS group produced bowel movements more similar to three-month-old infants [36, 38]. In infants, a reduction in stool frequency and increase in stool firmness has been found to be associated with postnatal age and with the maturation of the gut [32, 36, 38]. In addition to infant age and diet [36, 39], stool consistency was recently reported to be associated with the intestinal bacterial species richness, enterotypes (or microbial classification), and community composition in adults [43]. We found a 1000-fold higher change in total fecal Bifidobacterium from baseline to the end of the supplementation period in infants supplemented with B. infantis EVC001 compared with unsupplemented infants. The changes in total fecal Bifidobacterium are biologically relevant and can logically be attributed to the supplementation of B. infantis EVC001. We hypothesize that supplementation of infants with B. infantis facilitates maturation of the gut mucosa. This hypothesis is supported by the findings that intestinal Bifidobacterium and B. infantis increase the mRNA expression of intestinal epithelial tight junction proteins [15], enhance intestinal barrier function through the production of acetate [44], and promote the maturation of dendritic cells in intestinal Peyer’s Patches [45].
To investigate overall GI tolerability, mothers were asked to rate their infants’ general irritability, upset feelings after spitting-up, and discomfort when passing gas or stool on a daily basis throughout the two-month study period. Generally, reports of infants’ general irritability, upset feelings, and discomfort scores were low and not different between the groups. Interestingly, maternal parity was significantly associated with rating irritability during the baseline and intervention but not the post-intervention period. Mean infant irritability scores were higher by primiparous than multiparous mothers, reflecting an over-assessment of infant behavior in first-time mothers [46]. The number of days blood in stool was present, number of daily spit-ups, and daily flatulence frequency were not different between the groups. Adverse events occurred in both groups based on evaluation of the presence of colic, number of sick doctor visits, illnesses, eczema diagnoses by a primary care providers, and use of antibiotics or gas-relieving medications. The types of events, however, were normal for infants of this age, were not serious in nature, and the incidence of adverse events was not greater in the BiLS group than in the LS group. The adverse events were not deemed related to the study procedures or feeding of B. infantis.
One limitation of our study was that a placebo was not supplied for the control arm and subjects were not blinded to their treatment assignment. Although these measures are critical for larger efficacy studies, they are not imperative for small Phase I trials. At the time the study was initiated, a placebo was not feasible, however we have recently identified a safe placebo that would not elicit a prebiotic effect in infants and feasible for future trials. Another limitation is a potential source of bias with the involvement of the clinical coordinator in allocating group assignments at enrollment. This was due to limited resources in using a neutral third party for randomization. Bias was checked weekly by the principal investigator to ensure the clinical coordinator had allocated group assignments in chronological order and according to the randomization scheme that was created prior to study initiation. Another limitation was that mothers were instructed to assess stool consistency by comparing their infants’ bowel movements with images of four typical stool consistencies. Assessing stool consistency by appearance using a 4-point system is subjective, and more objective metrics of stool quality are needed in the clinical setting. Furthermore, in contrast with studies in adolescents [47], the infant stool scale used in this study has not been correlated with colonic transit time [32], making interpretation with GI function challenging. Another limitation was that mothers were not instructed to report the amount of infant stool produced, which has been found to be a reliable metric of GI maturation [32]. We did not include bowel movement size because of difficulty in assessing the amount of stool as a percentage of total surface on the diaper due to the excellent absorbency of today’s disposable diapers. Lastly, balancing the number of primiparous and multiparous women would have better controlled confounding effects of assessing infant symptoms.
Conclusions
In this study of normal, healthy, term infants, supplementation of B. infantis EVC001 for 21 consecutive days in maternal breast milk was well-tolerated and increased total infant fecal Bifidobacterium. There was no difference in the number or type of reported adverse events between supplemented and non-supplemented infants.
Change history
15 August 2017
An erratum to this article has been published.
Abbreviations
- ANOVA:
-
Analysis of variance
- B. infantis :
-
Bifidobacterium longum subspecies infantis
- BiLS:
-
Lactation support plus B. infantis supplementation
- GI:
-
Gastrointestinal
- HMO:
-
Human milk oligosaccharides
- IBCLC:
-
internationally board certified lactation consultant
- IMPRINT:
-
Infant microbiota probiotic intake study
- IRB:
-
Institutional Review Board
- LS:
-
Lactation support alone
- PCR:
-
Polymerase chain reaction
- UC:
-
University of California
References
Smilowitz JT, Lebrilla CB, Mills DA, German JB, Freeman SL. Breast milk oligosaccharides: structure-function relationships in the neonate. Annu Rev Nutr. 2014;34:143–69.
Coppa GV, Gabrielli O, Pierani P, Catassi C, Carlucci A, Giorgi P. Changes in carbohydrate composition in human milk over 4 months of lactation. Pediatrics. 1993;91(5):637–41.
Chaturvedi P, Warren CD, Altaye M, Morrow AL, Ruiz-Palacios G, Pickering LK, et al. Fucosylated human milk oligosaccharides vary between individuals and over the course of lactation. Glycobiology. 2001;11(5):365–72.
Zivkovic AM, German JB, Lebrilla CB, Mills DA. Human milk glycobiome and its impact on the infant gastrointestinal microbiota. Proc Natl Acad Sci U S A. 2011;108(Suppl 1):4653–8.
Tissier H. Recherches sur la flore intestinale des nourrissons: état normal et pathologique. Paris: G. Carré et C. Naud; 1900.
Subramanian S, Blanton LV, Frese SA, Charbonneau M, Mills DA, Gordon JI. Cultivating healthy growth and nutrition through the gut microbiota. Cell. 2015;161(1):36–48.
Bäckhed F, Roswall J, Peng Y, Feng Q, Jia H, Kovatcheva-Datchary P, et al. Dynamics and stabilization of the human gut Microbiome during the first year of life. Cell Host Microbe. 2015;17(5):690–703.
Sela D, Chapman J, Adeuya A, Kim J, Chen F, Whitehead T, et al. The genome sequence of Bifidobacterium longum subsp. infantis reveals adaptations for milk utilization within the infant microbiome. Proc Natl Acad Sci. 2008;105(48):18964.
LoCascio R, Ninonuevo M, Freeman S, Sela D, Grimm R, Lebrilla C, et al. Glycoprofiling of bifidobacterial consumption of human milk oligosaccharides demonstrates strain specific, preferential consumption of small chain glycans secreted in early human lactation. J Agric Food Chem. 2007;55(22):8914–9.
Garrido D, Ruiz-Moyano S, Lemay DG, Sela DA, German JB, Mills DA: Comparative transcriptomics reveals key differences in the response to milk oligosaccharides of infant gut-associated bifidobacteria. Scientific reports. 2015;5:1-7.
Garrido D, Barile D, Mills DA. A molecular basis for bifidobacterial enrichment in the infant gastrointestinal tract. Advances in Nutrition: An International Review Journal. 2012;3(3):415S–21S.
Kim JH, An HJ, Garrido D, German JB, Lebrilla CB, Mills DA. Proteomic analysis of Bifidobacterium longum subsp. infantis reveals the metabolic insight on consumption of prebiotics and host glycans. PLoS One. 2013;8(2):e57535.
Garrido D, Ruiz-Moyano S, Mills DA. Release and utilization of N-acetyl-D-glucosamine from human milk oligosaccharides by Bifidobacterium longum subsp. infantis. Anaerobe. 2012;18(4):430–5.
Ward R, Niñonuevo M, Mills D, Lebrilla C, German J. In vitro fermentability of human milk oligosaccharides by several strains of bifidobacteria. Mol Nutr Food Res. 2007;51(11):1398–405.
Chichlowski M, De Lartigue G, German JB, Raybould HE, Mills DA. Bifidobacteria isolated from infants and cultured on human milk oligosaccharides affect intestinal epithelial function. J Pediatr Gastroenterol Nutr. 2012;55(3):321–7.
Underwood MA, German JB, Lebrilla CB, Mills DA: Bifidobacterium longum subspecies infantis: champion colonizer of the infant gut. Pediatr Res. 2014;77(1-2):229-35.
Pokusaeva K, Fitzgerald GF, van Sinderen D. Carbohydrate metabolism in Bifidobacteria. Genes Nutr. 2011;6(3):285–306.
Ganguli K, Meng D, Rautava S, Lu L, Walker WA, Nanthakumar N. Probiotics prevent necrotizing enterocolitis by modulating enterocyte genes that regulate innate immune-mediated inflammation. American Journal of Physiology-Gastrointestinal and Liver Physiology. 2013;304(2):G132–41.
Underwood MA, Arriola J, Gerber CW, Kaveti A, Kalanetra KM, Kananurak A, et al. Bifidobacterium longum subsp. infantis in experimental necrotizing enterocolitis: alterations in inflammation, innate immune response, and the microbiota. Pediatr Res. 2014;76(4):326–33.
Bergmann KR, Liu SX, Tian R, Kushnir A, Turner JR, Li H-L, et al. Bifidobacteria stabilize claudins at tight junctions and prevent intestinal barrier dysfunction in mouse necrotizing enterocolitis. Am J Pathol. 2013;182(5):1595–606.
Huda M, Lewis Z, Kalanetra K, Rashid M, Raqib R, Qadri F, et al. Stool microbiota and vaccine responses of infants. Pediatrics. 2014;134:1–11.
Lewis ZT, Totten SM, Smilowitz JT, Popovic M, Parker E, Lemay DG, et al. Maternal fucosyltransferase 2 status affects the gut bifidobacterial communities of breastfed infants. Microbiome. 2015;3(1):13.
Bager P, Wohlfahrt J, Westergaard T. Caesarean delivery and risk of atopy and allergic disesase: meta-analyses. Clinical & Experimental Allergy. 2008;38(4):634–42.
Thavagnanam S, Fleming J, Bromley A, Shields M, Cardwell C. A meta-analysis of the association between Caesarean section and childhood asthma. Clinical & Experimental Allergy. 2008;38(4):629–33.
Negele K, Heinrich J, Borte M, Berg A, Schaaf B, Lehmann I, et al. Mode of delivery and development of atopic disease during the first 2 years of life. Pediatr Allergy Immunol. 2004;15(1):48–54.
Renz-Polster H, David M, Buist A, Vollmer W, O'Connor E, Frazier E, et al. Caesarean section delivery and the risk of allergic disorders in childhood. Clinical & Experimental Allergy. 2005;35(11):1466–72.
Eggesbø M, Botten G, Stigum H, Nafstad P, Magnus P. Is delivery by cesarean section a risk factor for food allergy? J Allergy Clin Immunol. 2003;112(2):420–6.
Vatanen T, Kostic AD, d’Hennezel E, Siljander H, Franzosa EA, Yassour M, et al. Variation in microbiome LPS immunogenicity contributes to autoimmunity in humans. Cell. 2016;165(4):842–53.
Underwood MA, Kalanetra KM, Bokulich NA, Lewis ZT, Mirmiran M, Tancredi DJ, Mills DA: A Comparison of Two Probiotic Strains of Bifidobacteria in Premature Infants. J Pediatr. 2013;163(6):1585-91.
Håkansson S, Axemo P, Bremme K, Bryngelsson A-L, Carlsson Wallin M, Ekström C-M, et al. Group B streptococcal carriage in Sweden: a national study on risk factors for mother and infant colonisation. Acta Obstet Gynecol Scand. 2008;87(1):50–8.
Penders J, Vink C, Driessen C, London N, Thijs C, Stobberingh EE. Quantification of Bifidobacterium spp., Escherichia coli and Clostridium Difficile in faecal samples of breast-fed and formula-fed infants by real-time PCR. FEMS Microbiol Lett. 2005;243(1):141–7.
Bekkali N, Hamers SL, Reitsma JB, Van Toledo L, Benninga MA. Infant stool form scale: development and results. J Pediatr. 2009;154(4):521–6. e521
Wessel MA, Cobb JC, Jackson EB, HARRIS GS, Detwiler AC. Paroxysmal fussing in infancy, sometimes called" colic". Pediatrics. 1954;14(5):421–35.
Hoy-Schulz YE, Jannat K, Roberts T, Zaidi SH, Unicomb L, Luby S, et al. Safety and acceptability of lactobacillus reuteri DSM 17938 and Bifidobacterium longum subspecies infantis 35624 in Bangladeshi infants: a phase I randomized clinical trial. BMC Complement Altern Med. 2016;16(1):1.
Kalliomäki M, Salminen S, Arvilommi H, Kero P, Koskinen P, Isolauri E. Probiotics in primary prevention of atopic disease: a randomised placebo-controlled trial. Lancet. 2001;357(9262):1076–9.
Weaver LT, Ewing G, Taylor LC. The bowel habit of milk-fed infants. J Pediatr Gastroenterol Nutr. 1988;7(4):568–71.
Shrago LC, Reifsnider E, Insel K. The neonatal bowel output study: indicators of adequate breast milk intake in neonates. Pediatr Nurs. 2006;32(3):195.
Çamurdan AD, Beyazova U, Özkan S, Tunç VT. Defecation patterns of the infants mainly breastfed from birth till the 12th month: prospective cohort study. Turk J Gastroenterol. 2014;25(1):1–5.
Tham E, Nathan R, Davidson G, Moore D. Bowel habits of healthy Australian children aged 0-2 years. J Paediatr Child Health. 1996;32(6):504–7.
Fontana M, Bianchi C, Cataldo F, Nibali SC, Cucchiara S, Casali L, et al. Bowel frequency in healthy children. Acta Paediatr. 1989;78(5):682–4.
Nyhan WL. Stool frequency of normal infants in the first week of life. Pediatrics. 1952;10(4):414–25.
Tunc VT, Camurdan AD, İlhan MN, Sahin F, Beyazova U. Factors associated with defecation patterns in 0–24-month-old children. Eur J Pediatr. 2008;167(12):1357–62.
Vandeputte D, Falony G, Vieira-Silva S, Tito RY, Joossens M, Raes J. Stool consistency is strongly associated with gut microbiota richness and composition, enterotypes and bacterial growth rates. Gut. 2015;65(1):57–62. doi:10.1136/gutjnl-2015-309618.
Fukuda S, Toh H, Hase K, Oshima K, Nakanishi Y, Yoshimura K, et al. Bifidobacteria can protect from enteropathogenic infection through production of acetate. Nature. 2011;469(7331):543–7.
Dong P, Yang Y. Wang W-p: the role of intestinal bifidobacteria on immune system development in young rats. Early Hum Dev. 2010;86(1):51–8.
Crockenberg SB, Smith P. Antecedents of mother-infant interaction and infant irritability in the first three months of life. Infant Behavior and Development. 1982;5(2–4):105–19.
Russo M, Martinelli M, Sciorio E, Botta C, Miele E, Vallone G, et al. Stool consistency, but not frequency, correlates with total gastrointestinal transit time in children. J Pediatr. 2013;162(6):1188–92.
Acknowledgements
We thank the mothers and their infants enrolled in this study for collecting information and samples with methodological detail and for complying with the study procedures during a stressful time in their busy lives. We thank our excellent support staff and collaborators: Michaela Carrick, visiting scholar from the University of Dublin who conducted data acquisition and its quality control; Deborah Albert PhD, BSN, IBCLC for rigorously recruiting and supporting the study; Heather Conway IBCLC, Marie-Celine Farver RN, BSN, IBCLC, RLC, Shirley German IBCLC, and Lonna Hampton MA, PA, IBCLC, the study’s lactation consultants who provided the study’s participants with the support and guidance to accomplish their breastfeeding goals; and Peter Trovitch PharmD, senior pharmacist and his team at Investigational Drug Services pharmacy at UC Davis Medical Center who managed and coordinated the storage, handling, and the dispensing of B. infantis EVC001 for the study.
Funding
This study was funded by Evolve BioSystems, Inc. (Evolve). Evolve performed the molecular methods for the infant fecal microbiome samples and was blinded to treatment assignments. Data analysis of the infant stools was conducted by Evolve after unblinding.
Availability of data and materials
Data are available as supplemental material.
Authors’ contributions
JTS conceived, designed the trial, analyzed and interpreted the data; wrote the manuscript; JM, MAB, CC acquired and analyzed the tolerability data; AF acquired data; KA analyzed the data and critically revised the manuscript; MAU conceived, designed, and critically revised the manuscript. All authors read and approved the final manuscript.
Competing interests
JTS is a private consultant for Evolve BioSystems Inc.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The University of California Davis Institutional Review Board approved all aspects of the study (IRB #: 631,099). Written informed consent was received by each participant prior to their participation (mothers provided consent on behalf of their newborns).
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Additional information
The original version of this article was revised to correct Figure 3a and its caption.
An erratum to this article is available at https://doi.org/10.1186/s12887-017-0932-7.
Additional files
Additional file 1:
Infant Stool Scale. Stool consistency rating scale from the validated Amsterdam Scale that was used in this study. (PDF 81 kb)
Additional file 2:
Weekly Health Questionnaire. The weekly health questionnaire used in this study that mothers filled out each week or every two weeks. (PDF 495 kb)
Additional file 3: Table S1.
Maternal baseline demographics. (DOCX 20 kb)
Additional file 4: Table S2.
Baseline maternal pregnancy and related characteristics. (DOCX 21 kb)
Additional file 5: Figure S1.
Mean ± SD of reported infant birthweight and infant weight measured on Days 33 and 61 postnatal for the LS (red dot plot) and BiLS (blue dot plot). n = 34 for each group for birthweight, n = 33 for the LS, and n = 34 for the BiLS groups on Days 33 and 61 postnatal. (DOCX 91 kb)
Additional file 6: Figure S2.
Mean ± SD of reported number of infant breast milk intake at the breast and by bottle for the LS (red dot plot) and BiLS (blue dot plot) groups during the Baseline, Intervention, and Post-intervention periods. n = 34 for each group during the Baseline and Intervention periods, n = 33 for the LS, and n = 34 for the BiLS groups during the Post-intervention period. (DOCX 91 kb)
Additional file 7: Table S3.
Infant diet throughout the study period. (DOCX 19 kb)
Additional file 8: Table S4.
Maternal reports of infant illnesses and reasons for infant sick-doctor visits throughout the study period. (DOCX 21 kb)
Additional file 9: Figure S3.
Mean ± SD of the change in the proportion of infant spit-ups for the LS (red dot plot) and BiLS (blue dot plot) groups during the Baseline, Intervention, and Post-intervention periods. n = 34 for each group during the Baseline and Intervention periods, and n = 33 for the LS and n = 34 for the BiLS groups during the Post-intervention period. (DOCX 43 kb)
Additional file 10: Figure S4.
Mean ± SD of the proportion of infant flatulence reported by mothers (red dot plot) and BiLS (blue dot plot) groups during the Baseline, Intervention, and Post-intervention periods. n = 17 for the LS and n = 12 for the BiLS groups for all time periods. (DOCX 48 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Smilowitz, J.T., Moya, J., Breck, M.A. et al. Safety and tolerability of Bifidobacterium longum subspecies infantis EVC001 supplementation in healthy term breastfed infants: a phase I clinical trial. BMC Pediatr 17, 133 (2017). https://doi.org/10.1186/s12887-017-0886-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-017-0886-9