Abstract
Background
Intraocular pressure (IOP) is an important physiological measure of the eye and is associated with some ocular disorders. We aimed to assess the influence of topical beta blocker-induced IOP reduction on lens-induced axial elongation in young guinea pigs.
Methods
The experimental study included 20 pigmented guinea pigs (age: 2–3 weeks). Myopia was induced in the right eyes for 5 weeks with − 10 diopter lenses. The right eyes additionally received either one drop of carteolol 2% (study group, n = 10) or one drop of artificial tears daily (control group, n = 10), while the contralateral eyes of all animals remained untouched. The outcome parameter was axial elongation during the follow-up period. The mean of all IOP measurements taken during the study was referred to as mean IOP.
Results
Greater axial elongation was associated with a shorter axial length at baseline (P < 0.001; standardized regression coefficient beta: − 0.54) and lens-induced myopization (P < 0.001; beta: 0.55). In the multivariable model, axial elongation was not significantly correlated with the IOP at study end (P = 0.59), the mean IOP during the study period (P = 0.12), the mean of all IOP measurements (P = 0.17), the difference between the IOP at study end and baseline IOP (P = 0.38), the difference between the mean IOP during the study period and the baseline IOP (P = 0.11), or the application of carteolol eye drops versus artificial tears eye drops (P = 0.07). The univariate analysis of the relationships between axial elongation and the IOP parameters yielded similar results. The inter-eye difference between the right eye and the left eye in axial elongation was significantly associated with the inter-eye difference in baseline axial length (P = 0.001; beta:-0.67) but not significantly correlated with the inter-eye difference in any of the IOP-related parameters (all P > 0.25).
Conclusions
In young guinea pigs with or without lens-induced axial elongation, neither the physiological IOP nor the IOP reduced by carteolol, a topical beta-blocker, was associated with the magnitude of axial elongation. These results suggest that IOP, regardless of whether it is influenced by carteolol, does not play a major role in axial elongation in young guinea pigs.
Similar content being viewed by others
Background
Intraocular pressure (IOP) is an important part of the physiology and pathophysiology of the eye. A minimum IOP of approximately 2 to 5 mmHg is necessary for the eye to maintain a consistent form and shape and to be resistant to deformations induced by inner forces, such as caused by the ciliary muscle, and by external forces such as caused by the eyelids and extraocular muscles [1]. A minimum IOP of approximately 2 to 5 mmHg is also needed to prevent thickening of the choroidal compartment and to promote the orthograde axoplasmic flow in the retinal ganglion axons through the lamina cribrosa of the optic nerve head [2], to mention only few aspects. Axial myopia is characterized by the enlargement of the globe and can be differentiated between primary axial myopia and secondary axial myopia. In cases of primary axial myopia, mostly the posterior half of the globe enlarges. In cases of secondary myopia in eyes with congenital glaucoma, the eye wall in the anterior segment, including the cornea, and that in the posterior segment expands as the IOP increases [3,4,5,6,7]. Based on observations made in eyes with congenital glaucoma and in adult hypotonic phthisic eyes, the possibility that the IOP may also play a role in primary axial myopia has been discussed, and it has been debated whether IOP in the upper normal range contributes to the expansion and elongation of the globe [8,9,10,11,12]. The hypothesis is supported by findings reported in some population-based studies. In these investigations, a higher IOP was associated with a longer axial length and higher myopic refractive errors after the statistical model was adjusted for parameters influencing IOP [13, 14]. Similar results have been observed in hospital-based investigations [15,16,17]. However, other studies reported contradictory results: in the population-based investigations of the Central India Eye and Medical Study and the Beijing Eye Study, axial length was not significantly related to IOP [18, 19].
In view of the attention that myopia has received in recent decades and to obtain more information about the processes of emmetropization and myopization, we conducted this study to determine whether IOP and axial length are associated in young guinea pigs [20, 21].
Methods
The experimental study included 20 pigmented guinea pigs (Cavia porcellus) with an age of 2–3 weeks and a body weight of 150–200 g at baseline. The Ethics Committee of the Beijing Tongren Hospital approved the study, and the ARVO Statement and the ARRIVE Guidelines for the use of animals in ophthalmic and vision research were taken into account. The animals were purchased from the Fang Yuanyuan farm in Beijing, China.
The guinea pigs were randomly divided into a study group (n = 10) and a control group (n = 10). For the guinea pigs in the study group, the right eyes underwent lens-induced myopization and additionally received one eye drop of carteolol hydrochloride 2% daily (Mikelan, Otsuka Pharmaceutical Co., Tokyo, Japan). For the guinea pigs in the control group, the right eyes also underwent lens-induced myopization and additionally received one eye drop of preservative free artificial tears daily (Hycosan, Ursapharm Arzneimittel GmbH, Saarbrücken, Germany). The topical application of the drug or artificial tears was performed daily at 3 pm. The left eyes in both groups did not undergo any interventions, nor did they receive any eye drops.
To induce myopization, we glued goggles (refractive power: − 10 diopters; diameter: 15 mm, optical zone: 12 mm) at the start of the study onto the skin of the orbital rim of the right eyes after the skin had been cleaned and shaved. The goggles were removed daily to administer the eye drops and to perform weekly examinations. The examinations included tonometry (Tono-Pen, Reichert Inc., NY, USA) under topical anesthesia (oxybuprocaine hydrochloride eye drops; Santen Co., Osaka, Japan), followed by refractometry (streak retinoscopy, 66 vision tech Co., Jiangsu, China) under cycloplegia (using one drop of tropicamide), and ocular biometry (A/B-mode scan ultrasonography, oscillator frequency: 11 MHz, Quantel Co., Les Ulis, France). The axial length was defined as the distance from the anterior border of the cornea to the inner surface of the retina. The animals were awake during the examinations, and lid retractors were not used. The IOP was measured at 4 pm on each examination day. For each measure, three IOP measurements were taken, and the mean value was used for further statistical analysis. Care was taken that the guinea pigs could open their eyes and blink freely under the goggles. The goggles were examined daily to ensure they were clean and placed appropriately; otherwise, they were detached, cleaned, and reattached. The application of the eye drops and the application of the goggles were started on the same day.
All guinea pigs remained in an environment at a constant temperature of 26 °C. The circadian day/night rhythm was set to be 12 h/12 h (the lighting automatically changed at 8 am and 8 pm) with a luminous intensity of 500 lx. After the study, all animals were sacrificed by an intraperitoneal injection of pentobarbital sodium with an overdose of 600 mg per kg weight.
For statistical analysis, we used a commercially available statistical analysis program (SPSS, version 25.0, IBM-SPSS, Chicago, IL, USA). We first calculated the mean and standard deviation (SD) of axial length, refractive error and IOP. We then compared the parameters between the left and right eyes using Student’s t-test for paired samples and we compared the parameters of the two different groups using Student’s t-test for unpaired samples. To assess the relationships between the variables, we first performed a univariate analysis followed by a multivariable analysis (defined as a statistical model with multiple independent or response variables). We calculated the standardized regression coefficient beta, the non-standardized regression coefficient B, and its 95% confidence interval (CI). A P-value was considered to indicate statistical significance if it was smaller than 0.05.
Results
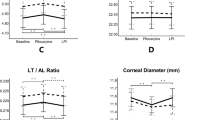
Immediately before treatment, the IOP, refractive error and axial length did not differ significantly between the study group and the control group in terms of the right eyes only or the left eyes only, and they did not significantly differ between the right eyes and left eyes in general (all P > 0.20) (Tables 1, 2). For the whole study population, the mean IOP at baseline was 15.0 ± 3.0 mmHg, the mean axial length was 7.98 ± 0.05 mm, and the mean refractive error was + 1.89 ± 0.66 diopters (Tables 1 & 2).
At the end of the study, the IOP was significantly (P < 0.001) lower in the right eyes of the study group, in which carteolol was applied, than in the right eyes of the control group, in which artificial tears were applied (Table 1). Correspondingly, within the study group, the IOP was lower (P = 0.035) at the end of the study than at baseline in the eyes in which carteolol was applied, while the IOP at study end did not differ significantly from the IOP at baseline in the eyes in which artificial tears were applied (P = 0.79). Within the control group, the right eyes, in which artificial tears were applied and which underwent lens-induced myopization, had a significantly (P = 0.007) higher IOP at study end than at baseline, while the IOP in the left eyes, in which eye drops were not applied and which did not undergo lens-induced myopization, did not differ significantly between baseline and study end (P = 0.79) (Table 1).
At study end, the refractive error was significantly (P < 0.001) more negative (more myopic), and the axial length was significantly (P < 0.001) longer than at baseline for all groups in the study population, including the left eyes without lens-induced myopization. At study end, the axial length was significantly shorter in the right eyes of the study group (carteolol application and lens-induced myopization) than in the right eyes of the control group (artificial tears application and lens-induced myopization) (8.61 ± 0.12 mm versus 8.70 ± 0.06 mm; P = 0.038). The change in axial length from baseline to study end (magnitude of axial elongation) did not differ significantly between both groups (0.62 ± 0.15 mm versus 0.73 ± 0.09 mm; P = 0.07). Similarly, the refractive error at study end was significantly less negative (less myopic) in the right eyes of the study group (carteolol application and lens-induced myopization) than in the right eyes of the control group (− 1.65 ± 1.80 diopters versus − 3.48 ± 2.06 diopters; P = 0.049), while the change in refractive error did not differ significantly (− 3.48 ± 1.75 diopters versus − 5.40 ± 2.38 diopters; P = 0.055) between the two groups.
Taking into consideration the whole study population and both eyes of each animal, greater axial elongation was associated with a shorter axial length at baseline (P < 0.001; beta: − 0.51). Axial elongation was more pronounced in the right eyes than in the left eyes (P < 0.001) (univariate analysis). The magnitude of axial elongation was not significantly correlated with the IOP at baseline (P = 0.48), the mean IOP during the study period (P = 0.41) (Fig. 1), the difference in IOP at study end and at baseline (P = 0.53), the difference between the mean IOP during the study period and the IOP at baseline (P = 0.26) (Fig. 2), or the mean of all IOP measurements (P = 0.51) (univariate analysis). When only the right eyes were taken into account and when the study population was subdivided into the study group (carteolol application) and the control group (artificial tears application), similar results were observed.
Scattergram showing the association between the mean intraocular pressure during the study period (measured at weekly intervals) and axial elongation (the final axial length minus the initial axial length) in the total study population. The treated eyes correspond to the right eyes, which underwent lens-induced myopia and received either carteolol 2% (red circles) or artificial tears (green circles); the control eyes correspond to the left eyes, which did not undergo any interventions or therapies (black circles)
Scattergram showing the association between the change in intraocular pressure during the study period (at weekly intervals) and axial elongation (the final axial length minus the initial axial length) in the total study population. The treated eyes correspond to the right eyes, which underwent lens-induced myopia and received either carteolol 2% (red circles) or artificial tears (green circles); the control eyes correspond to the left eyes, which did not undergo any interventions or therapies (black circles)
The multivariable analysis included the magnitude of axial elongation as the dependent variable and axial length at baseline and right eye versus left eye (i.e., lens-induced myopization versus no lens-induced myopization) as independent variables. Both independent variables remained to be significantly (P < 0.001) associated with axial elongation (Table 3). When IOP-related parameters were included as independent variables in that model, they were not found to be significantly associated with the magnitude of axial elongation during the study period. The IOP-related parameters included the IOP at study end (P = 0.59), the mean IOP during the study period (P = 0.12), the mean of all IOP measurements (P = 0.17), the difference between the IOP at study end and the baseline IOP (P = 0.38), and the difference between the mean IOP during the study period and the baseline IOP (P = 0.11). Similarly, when the group parameter for the study group (carteolol application) and the control group (artificial tears application) was included as an independent variable, it was not significantly (P = 0.07) correlated with axial elongation.
In univariate analysis, the inter-eye difference in axial elongation between the right eyes and the left eyes was significantly associated with the inter-eye difference in baseline axial length (P = 0.001; beta: -0.67; B: -1.57; 95%CI: − 2.43, − 0.71) but not significantly correlated with the inter-eye difference in any of the IOP-related parameters (difference between the IOP at study end and IOP at baseline: P = 0.19; difference between the mean of all IOP measurements during the study period and baseline IOP: P = 0.09; mean of all IOP measurements: P = 0.25; mean of all IOP measurements during the study period: P = 0.19). Correspondingly, when any IOP-related parameter was included in the model of the association between inter-eye differences in axial elongation and inter-eye differences in baseline axial length, it did not reveal any other significant associations (difference between IOP at study end and IOP at baseline: P = 0.35; difference between the mean of all IOP measurements during the study period and baseline IOP: P = 0.25; mean of all IOP measurements: P = 0.27; mean of all IOP measurements during the study period: P = 0.25).
Similarly, the difference between the right eyes and the left eyes in the change in refractive error during the study period was not significantly related to any of the IOP-related parameters (all P ≥ 0.19).
Discussion
In this experimental study in young guinea pigs, greater axial elongation was associated with a shorter axial length at baseline (P < 0.001) and with lens-induced myopization (P < 0.001), while it was not significantly correlated with the IOP at study end, mean IOP during the study period, difference in IOP at study end and at baseline, difference between the mean IOP during the study period and the baseline IOP, or the study group (carteolol application) versus control group (artificial tears application). In a similar manner, the inter-eye difference between the right eye and the left eye in axial elongation was significantly associated with the inter-eye difference in baseline axial length (P = 0.001) but not with the inter-eye difference in any of the IOP-related parameters. In young guinea pigs with or without lens-induced axial elongation, neither the physiological IOP measurements nor the reduced IOP measurements induced by a topical beta-blocker were associated with the magnitude of axial elongation.
The results of our study agree with the findings shown in previous investigations, some of which used the form-deprived myopic chick model (Table 4). In the study by Schmidt and colleagues, reduction of IOP by topical application of the beta-blocker timolol was not markedly effective against the development of myopia in chicks [9]. Similarly, our study showed that the topical application of the beta-blocker carteolol was not associated with axial elongation in young guinea pigs. Correspondingly, a clinical trial that compared children who received 0.25% timolol eye drops and children who used bifocal spectacles showed that these interventions did not significantly affect the progression of myopia [23]. Additionally, other clinical studies showed that topically applied beta-blockers did not affect the rate of myopia progression [24, 25]. Jin and Stjernschantz examined the influence of prostaglandins on the development of myopia in chicks and found that indomethacin administered intramuscularly, subconjunctivally or intravitreally as well as exogenous prostaglandin PGE2, prostaglandin PGF2alpha and latanoprost acid administered subconjunctivally or topically, did not have a significant effect on myopia development [10]. Interestingly, the intravitreal application of PGF2alpha significantly attenuated myopia development. Moreover, Jin and Stjernschantz reported that prostaglandins presumably lowered the IOP; however, they did not measure the IOP.
The observations made in these investigations, including our study, are inconsistent with the results of the recent study by El-Nimri and Wildsoet conducted in two-week-old pigmented guinea pigs with unilateral form deprivation myopia; compared with the control group, that received artificial eye drops, the study group, that received latanoprost eye drops, showed a significant reduction in IOP and axial elongation [12]. At the 9-week follow-up, compared to the contralateral eyes, the eyes that received latanoprost eye drops showed significantly lower IOP readings, and the intereye difference was significantly larger in the study group, which unilaterally received latanoprost eye drops, than in the control, which unilaterally received artificial eye drops (− 5.17 ± 0.96 mmHg versus 1.80 ± 1.16 mmHg; P < 0.001). The interocular differences in axial length did not change significantly from baseline to the study end in the study group (from 0.02 ± 0.02 to 0.06 ± 0.02 mm; P = 0.20), while the interocular differences in axial length had significantly increased at the study end in the control group (from 0.00 ± 0.02 to 0.29 ± 0.04 mm; P < 0.001). Correspondingly, the inter-eye difference in refractive error slightly increased in the study group (from − 0.15 ± 0.35 diopters to − 2.25 ± 0.54 diopters; P = 0.03) and markedly increased in the control group (from + 0.03 ± 0.36 diopters to − 8.2 ± 0.71 diopters; P < 0.001). These discrepancies in the results of the studies may be explained by the differences between beta-blockers and prostaglandin derivatives as well as differences in the species studied, as the chick sclera has an inner cartilage layer in addition to the fibrous layer; thus, the mechanisms of globe elongation may differ between chicks and guinea pigs.
In another study in guinea pigs, the reduction of IOP by topical application of the α-adrenergic agonist brimonidine was also associated with a reduction in the rate of progression of myopia [11]. In that study, Liu and colleagues studied the right eyes of 36 guinea pigs, in which myopia was induced by goggles, as in our study. In the study groups that topically received 0.1% brimonidine eye drops only or 0.2% brimonidine eye drops only, the refractive error was less myopic (P = 0.024 and P = 0.006, respectively), and the axial length was shorter (P = 0.005 and P = 0.0017, respectively) than in the control group. Similarly, the combination of brimonidine 1% or 2% with 2% pirenzepine was associated with similar effects in reducing the progression of myopic refractive error (P = 0.016 and P = 0.0006, respectively) and axial elongation (P = 0.017and P = 0.0004, respectively). In a study performed by Carr and colleagues, intravitreally injected brimonidine (20 nmol and 200 nmol) and clonidine (200 nmol) inhibited experimentally induced increases in myopic refractive error and axial elongation in white Leghorn chicks with form deprivation myopia [22]. While IOP was not measured in Carr’s study, the authors concluded that high concentrations of α2-adrenoceptor agonists inhibited form deprivation myopia in chicks.
The discrepancy in the results between El-Nimri’s study and Liu’s study as well as our investigation may have been due to differences in the IOP-lowering agent (latanoprost versus brimonidine versus carteolol), including differences in the duration of the IOP-lowering effect. In humans, the IOP-lowering effect lasts for approximately 24 h with prostaglandin derivatives such as latanoprost, while the ocular hypotensive effect of beta-blockers is mostly limited to daytime hours [26].
The IOP measurements reported in our study (15.0 ± 3.0 mmHg at the age of 2 weeks at baseline; 15.5 ± 3.5 mm in the left control eyes at study end) were slightly higher than those reported in some previous investigations. In the study by Cairó and colleagues, guinea pigs aged 4 weeks and guinea pigs aged 3 to 36 months showed tonometric measurements of 8.53 ± 1.28 mmHg and 13.20 ± 1.28 mmHg, respectively, as measured by a rebound tonometry between 4 pm and 6 pm [27]. Applanation tonometry revealed values of 10.9 ± 3.6 mmHg for the adult group. In the investigation performed by Rajaei and associates, IOP was measured by rebound tonometry (TonoVet tonometer, iCare, Tiolat, Helsinki, Finland) in guinea pigs aged 12 to 15 months and was 6.81 ± 1.41 mmHg [28]. The IOP measurements obtained in our study by applanation tonometry were considerably lower than the IOP readings obtained by rebound tonometry in the recent study by El-Nimri, with mean values ranging between 22.2 ± 1.0 mmHg and 24.2 ± 0.09 mmHg in the various subgroups at baseline (Table 4).
Interestingly, the idea that IOP does not promote axial elongation is supported by observations in several different animal models, in which sectorial form deprivation or sectorial negative defocus induced sectorial axial myopia, although the IOP was equal in all regions of the eyes. It is also supported by the clinical finding that a marked increase in IOP does not lead to excessive elongation in emmetropic eyes and the normalization of an elevated IOP does not lead to the shortening of the axial length.
Limitations of our study should be discussed. First, we looked for associations between IOP and axial elongation. Even if we had found a statistically significant correlation, we would not have been able to conclude that the reduction in IOP caused the reduction in axial elongation since the reverse of such a causal relationship would also have been possible. Such a limitation may also be valid for previous studies. Similarly, the higher IOP that was observed in individuals with a longer axial length, as measured in hospital-based studies as well as in population-based investigations, might have been a secondary effect of axial elongation on the anterior segment. Second, we did not record calibration measurements for the tonometer we used in our study. Third, we did not assess the effect of carteolol in normal eyes without lens-induced myopization. Fourth, the differences in axial length and axial elongation were relatively small, so the statistical power of the study might not have been sufficient to reveal a statistically significant association. Fifth, we used a Tono-Pen device for tonometry, while in some studies, devices for rebound tonometry have shown better performance (Table 4) [29]. Sixth, the results of this study may be specific to carteolol rather than beta blockers in general since the group of beta blockers with substances such as carteolol and timolol differ in their pharmacodynamics and receptor specificity. The negative result regarding the use of carteolol may therefore not lead to generalized conclusions for other IOP lowering drugs including other beta blockers or prostaglandins. Seventh, the sample size in this study was relatively small, so the lack of statistical significance in the results might have been caused by a limited amount of statistical power regarding the study sample. Eighth, we used topically applied carteolol to lower the IOP and to determine whether an association exists between IOP and axial elongation. To test Koch’s hypotheses, future studies should be conducted to determine the effect of an elevated IOP on the ocular axial length.
Conclusions
In young guinea pigs with or without lens-induced axial elongation, neither the physiological IOP nor the IOP reduced by a topical beta-blocker, carteolol, was significantly associated with the magnitude of axial elongation. These results suggest that IOP, regardless of whether it is influenced by carteolol, does not play a major role in axial elongation in young guinea pigs.
Availability of data and materials
The original data of the current study are available from the corresponding author upon reasonable request.
Abbreviations
- IOP:
-
Intraocular pressure
- RE:
-
Refractive error
- D:
-
Diopter
- AL:
-
Axial length
- CI:
-
Confidence interval
- Fig:
-
Figure
References
Davson H. The Aqueous Humour and the Intraocular Pressure. In: Davson H, editor. Physiology of the Eye. Switzerland: Springer Nature; 2020. p. 3–95.
Tso MO, Hayreh SS. Optic disc edema in raised intracranial pressure. IV. Axoplasmic transport in experimental papilledema. Arch Ophthalmol. 1977;95(8):1458–62.
Heine L. Beiträge zur Anatomie des myopischen Auges. Arch Augenheilkd. 1899;38:277–90.
Vurgese S, Panda-Jonas S, Jonas JB. Scleral thickness in human eyes. PLoS One. 2012;7(1):e29692.
Ohno-Matsui K, Kawasaki R, Jonas JB, Cheung CM, Saw SM, Verhoeven VJ, et al. For the META-analysis for pathologic myopia (META-PM) study group. International classification and grading system for myopic maculopathy. Am J Ophthalmol. 2015;159(5):877–883.e7.
Shen L, You QS, Xu X, Xu X, Gao F, Zhang Z, et al. Scleral and choroidal thickness in secondary high axial myopia. Retina. 2016;36(8):1579–85.
Zagora SL, Funnell CL, Martin FJ, Smith JE, Hing S, Billson FA, et al. Primary congenital glaucoma outcomes: lessons from 23 years of follow-up. Am J Ophthalmol. 2015;159(4):788–96.
Jensen H. Myopia progression in young school children. A prospective study of the myopia progression and the effect of a trial with bifocal lenses and beta blocker eye drops. Acta Ophthalmol. 1991;200:1–79.
Schmid KL, Abbott M, Humphries M, Pyne K, Wildsoet CF. Timolol lowers intraocular pressure but does not inhibit the development of experimental myopia in chick. Exp Eye Res. 2000;70(5):659–66.
Jin N, Stjernschantz J. Effects of prostaglandins on form deprivation myopia in the chick. Acta Ophthalmol Scand. 2000;78(5):495–500.
Liu Y, Wang Y, Lv H, Jiang X, Zhang M, Li X. Α-adrenergic agonist brimonidine control of experimentally induced myopia in guinea pigs: A pilot study. Mol Vis. 2017;23:785–98.
El-Nimri NW, Wildsoet CF. Effects of topical latanoprost on intraocular pressure and myopia progression in young Guinea pigs. Invest Ophthalmol Vis Sci. 2018;59(6):2644–51.
Wong TY, Klein BEK, Klein R, Knudtson M, Lee KE. Refractive errors, intraocular pressure, and glaucoma in a white population. Ophthalmology. 2003;110(1):211–7.
Mitchell P, Hourihan F, Sandbach J, Wang JJ. The relationship between glaucoma and myopia: the Blue Mountains eye study. Ophthalmology. 1999;106(10):2010–5.
Quinn GE, Berlin JA, Young TL, Ziylan S, Stone RA. Association of intraocular pressure and myopia in children. Ophthalmology. 1995;102(2):180–5.
Lee AJ, Saw SM, Gazzard G, Cheng A, Tan DT. Intraocular pressure associations with refractive error and axial length in children. Br J Ophthalmol. 2004;88(1):5–7.
Saeedi O, Pillar A, Jefferys J, Arora K, Friedman D, Quigley H. Change in choroidal thickness and axial length with change in intraocular pressure after trabeculectomy. Br J Ophthalmol. 2014;98(7):976–9.
Nangia V, Jonas JB, Sinha A, Matin A, Kulkarni M, Panda-Jonas S. Ocular axial length and its associations in an adult population of central rural India. The Central India eye and medical study. Ophthalmology. 2010;117(7):1360–6.
Yin G, Wang YX, Zheng ZY, Yang H, Xu L, Jonas JB, et al. Ocular axial length and its associations in Chinese. The Beijing eye study. PLoS One. 2012;7(8):e43172.
Flaxman SR, Bourne RRA, Resnikoff S, Ackland P, Braithwaite T, Cicinelli MV, et al. Global causes of blindness and distance vision impairment 1990-2020: a systematic review and meta-analysis. Lancet Glob Health. 2017;5(12):e1221–34.
Holden BA, Fricke TR, Wilson DA, Jong M, Naidoo KS, Sankaridurg P, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123(5):1036–42.
Carr BJ, Nguyen CT, Stell WK. Alpha2 -adrenoceptor agonists inhibit form-deprivation myopia in the chick. Clin Exp Optom. 2019;102(4):418–25.
Jensen H. Myopia progression in young school children. A prospective study of myopia progression and the effect of a trial with bifocal lenses and beta blocker eye drops. Acta Ophthalmol Suppl. 1991;200:1–79.
Goldschmidt E. Myopia in humans: can progression be arrested? CIBA Found Symp. 1990;155:222–9.
Hosaka A. The growth of the eye and its components: Japanese studies. Acta Ophthalmol. 1988;66(suppl):65–8.
Liu JHK, Kripke DF, Weinreb RN. Comparison of the nocturnal effects of once-daily timolol and latanoprost on intraocular pressure. Am J Ophthalmol. 2004;138(3):389–95.
Cairó M, Peña MT, Rios J, Melero A, Martorell J, Leiva M. Assessment of intraocular pressure by applanation tonometry and rebound tonometry in Guinea pigs of different ages. J Exot Pet Med. 2018;27:25–31.
Rajaei SM, Mood MA, Sadjadi R, Azizi F. Intraocular pressure, tear production, and ocular echobiometry in guinea pigs (Cavia porcellus). J Am Assoc Lab Animal Sci. 2016;554:475–9.
Pease ME, Hammond JC, Quigley HA. Manometric calibration and comparison of TonoLab and TonoPen tonometers in rats with experimental glaucoma and in normal mice. J Glaucoma. 2006;15(6):512–9.
Acknowledgements
The authors thank those who participate in this study.
Funding
This study was supported by National Natural Science Foundation of China (81570891); Beijing Natural Science Foundation (7151003); Supported by the Beijing Municipal Administration of Hospitals’ Ascent Plan (DFL20150201); Advanced Health Care Professionals Development Project of Beijing Municipal Health Bureau (2014–2-003); The Capital Health Research and Development of Special (2020–1-2052); Beijing Municipal Administration of Hospitals Clinical Medicine Development of Special Funding Support (ZYLX201307); Science & Technology Project of Beijing Municipal Science & Technology Commission (Z181100001818003). The funding organization played no role in the study design or data collection.
Author information
Authors and Affiliations
Contributions
Study design: L.D., W.B.W., J.B.J.; Conducting the study: L.D., Y.F.L., H.T.W., H.D.K., Y.J.L., Y.X.W. W.B.W.; Statistical analysis and writing of the first draft of the manuscript: L.D., J.B.J.; Revision and final approval of the draft: all authors.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Ethics Committee of the Beijing Tongren Hospital study approved the study, and the ARVO Statement for the use of animals in ophthalmic and vision research was taken into account.
Consent for publication
Not applicable.
Competing interests
Jost B. Jonas: Patent application with University of Heidelberg (Heidelberg, Germany) (Title: Agents for use in the therapeutic or prophylactic treatment of myopia or hyperopia; European Patent Number: 3 070 101).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Dong, L., Li, Y.F., Wu, H.T. et al. Lens-induced myopization and intraocular pressure in young guinea pigs. BMC Ophthalmol 20, 343 (2020). https://doi.org/10.1186/s12886-020-01610-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-020-01610-x