Abstract
Background
This is a case of spontaneous toric implantable collamer lens (TICL) rotation that occurred twice in the left eye of a patient.
Case presentation
A 24-year-old gentleman received TICL implantation for treatment of myopic astigmatism encountered with spontaneous rotation of approximately 90° from its original position. TICL reposition procedure was performed with visual outcome of 20/16. Surprisingly, a re-rotation of TICL occurred. The patient underwent a replacement of non-toric ICL with a larger size after careful re-evaluation with final visual outcome of 20/20. A short and small ciliary process with shallow ciliary sulcus and posteriorly positioned ciliary body was found by Ultrasound Biomicroscopy (UBM).
Conclusions
The unique morphology of the ciliary body may have a potential association with the vault and instability of implanted ICL. Careful examination of the ciliary body morphology is essential in preoperative evaluation.
Similar content being viewed by others
Background
The Visian Toric Implantable Collamer Lens (TICL) (STAAR Surgical, Nidau, Switzerland) is a foldable lens designed to correct myopia and myopic astigmatism. Previous studies have revealed that the position of the V4C TICL in the eye is stable with an average rotation angle of 3.39 ± 2.36° [1]. According to the current literature, there is only few reports of spontaneous TICL rotation that led significant decrease in visual acuity and required further surgical procedures [2, 3].Here, we present a rare case in which a TICL spontaneously rotated approximately 90° twice and analyze the possible causes of the rotation and the finally successful management strategy.
Case presentation
A 24-year-old gentleman with no history of systemic and ocular diseases and surgery presented for refractive surgery. The patient’s uncorrected distance visual acuity (UDVA) was 20/160 in the right eye and 20/200 in the left eye, with refractive error of − 7.00 -1.00 × 5° and - 9.50 - 2.00 × 175°. The anterior segment and fundus evaluations were unremarkable. Keratometric values, central corneal thickness, anterior chamber depth from the endothelium of the cornea in bilateral eyes measured by Pentacam HR (Oculus, Germany) were 43.3@96/42.1@6 and 43.8@93/42.3@3, 574 μm and 571 μm, 3.27 mm and 3.20 mm, respectively, while white-to-white distance obtained with a caliper were both 10.93 mm, horizontal sulcus-to-sulcus distance assessed by the UBM (Model SW-3200 L;Tianjin Suowei Electonic Technology Co, Ltd., Tianjin, China) were 11.28 mm and 11.16 mm.
After a thorough discussion with the patient, regarding the risks and benefits of surgery, an informed consent was obtained. The right eye undergone a LASIK procedure, while in the left eye TICL calculation software developed by the STAAR Surgical company recommended V4C (model: TICM12.1) with a power of - 12.50 + 2.0 × 91° and 6° clockwise rotation after horizontal implantation 7 days later. Zero and 180 degree limbus reference marking was identified under the slit-lamp with patient sitting upright preoperatively. After topical anesthesia, an inferior paracentesis and 3.0 mm temporal clear corneal incision were made. The TICL was inserted through the temporal incision with four haptics tucked behind the iris and subsequently axis adjusted to the desired alignment axis after the anterior chamber maintained by a cohesive viscosurgical device (Iviz, Bausch&Lomb). Finally, the surgery was uneventful after the viscosurgical device was removed manually using the balanced salt solution.
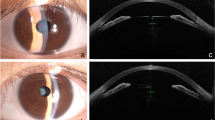
On the first postoperative day, the left eye achieved an UDVA of 20/16 without any complications, while the vault was 360 μm. Twenty days after the surgery the patient presented urgently due to a sudden drop in visual acuity of his left eye when he woke up in the morning. He denied any trauma or other conditions. The UDVA decreased to 20/100 with a refraction of + 1.50–2.75 × 5°. After pupillary dilatation, a rotation of approximately 90° of the TICL from its original position was observed (Fig. 1). The vault was 336 μm. Thus, we decided to perform TICL reposition procedure in the operating room. The TICL remained stable with an UDVA of 20/16 and a vault of 365 μm until 1 month postoperatively, when the patient presented again with an exactly similar complaint. Conventional ophthalmic examination revealed almost the same angle and orientation of TICL rotation as the last time, while the vault was 342 μm.
After a careful and discreet re-evaluation, a replacement of the TICL with a larger size non-toric ICL was decided. A V4C (model: VICM12.6) with a power of − 11.5 D was chosen and placed in a horizontal position uneventfully. On 1 day postoperatively, the eye achieved an UDVA of 20/20 without any further complications, while the vault was 381 μm. During the next 2 months of follow-up, the patient’s condition has remained stable with an excellent post-operative outcome.
Discussion and conclusion
A key factor in determining refractive outcome after TICL implantation is postoperative rotational stability. Packer et al. [4] reported that 0.33% (10/2970) of patients that underwent V4C implants required a second adjustment surgery and completely achieved the desired results subsequently. Similar occurrence rate (0.32%) was disclosed in retrospective analysis of 310 TICLs implantations in our refractive center since 2014 after one patient with a clear history of trauma was excluded. Theoretically, a rotation of 30° in the axis would result in a total loss of astigmatism correction [5]. The subject of the current report experienced spontaneous rotation of nearly 90° twice in the same eye. To the best of our knowledge, few studies have reported recurrent, significant, spontaneous rotation of a TICL.
TICL rotation has been reported to be associated with a very low postoperative TICL vaulting (<80 μm), [6] it is clear that a smaller TICL size will lead to a lower vaulting and more frequent rotation. Since the postoperative vault was in the normal range, we initially performed a TICL reposition, but unfortunately, rotation reoccurred 1 month postoperatively. Finally replacement for a larger size non-toric of ICL was performed. Traditionally, a lager vault responds to a larger size of ICL. However, in this patient the vault remained unchanged despite replacement with a larger ICL, this phenomenon reminded us the TICL rotation in this patient could not be simply explained by the vaulting and the size of the TICL.
Previously published work showed the ciliary sulcus measurement can improve the accuracy of the ICL sizing [7].The UBM imaging drawn our attention in which all the four footplates of ICL were constantly not in the ciliary sulcus postoperatively (Fig.2 a-d). Similarly, Park et al. [8] revealed a case with just one of four footplates located below the ciliary sulcus occurred a rotation of TICL with an angle of 11° after surgery. Zhang et al. [9] considered the main reason for the dislocation of the footplate was the surgical intrinsic drawback— blindly performed underneath the iris. We hypothesize the variation of ciliary sulcus structure is a main factor infecting the position of the footplates and the subsequent rotation of the TICL. Considering that the ciliary body was the major tissue composing the ciliary sulcus, we further analyzed the characteristics of the ciliary body on the UBM imaging and detected some unusual morphological features. In particular, the maximum ciliary body thickness (CBTmax), trabecular ciliary process distance (TCPD) and trabecular-ciliary angle (TCA) measured in this patient (Fig. 3) was 0.64 mm,1.43 mm and 140.2° respectively, significantly different from the mean values (1.053 ± 0.103 mm, 0.834 ± 0.234 mm and 75.1° ± 17.9°) reported in normal subjects [10, 11]. In summary, this patient had a posteriorly positioned ciliary body, a short and small ciliary process and a shallow ciliary sulcus. Part quadrant of the ciliary sulcus lost its normal length or exhibited a nearly obtuse angle. The “specious” ciliary sulcus leads the footplates to slide down to ciliary body easily or even cross over the small ciliary body coupled with changes in the accommodation states and finally rest on the lens periphery and zonules. When most footplates lost intrinsic support, a large rotation of the loosed TICL may occurred.
Assessment of the ciliary body parameters. Trabecular-ciliary process distance (TCPD) is the length of the line extending from the corneal endothelium 500 μm from the scleral spur perpendicularly to the line which passing through the most inner point of the ciliary body and parallel to the iris. Maximum ciliary body thickness (CBTmax) is the distance from the most inner point of the ciliary body to the inner wall of sclera or its extended line. Trabecular-ciliary angle (TCA) is the angle between the posterior corneal surface and the anterior surface of the ciliary body
Close and long-term follow-up was warranted to observe if a recurrent rotation would happen in the future. Although the patient would not present with a sudden loss of visual acuity by the rotation of a ICL, the resulting impact on the lens and zonules still needed to be concerned.
This unique case revealed the potential association between the vault and instability of implanted ICL with the ciliary body morphology. Careful examination of UBM image can provide clinicans with valuable information in the preoperative ICL assessment. Further work including a large sample size with prospective design would be necessary to elucidate the actual mechanism.
Availability of data and materials
Not applicable.
Abbreviations
- CBTmax:
-
Maximum ciliary body thickness
- ICL:
-
Implantable collamer lens
- TCPD:
-
Trabecular ciliary process distance
- TCA:
-
Trabecular-ciliary angle
- TICL:
-
Toric implantable collamer lens
- UBM:
-
Ultrasound biomicroscopy
- UDVA:
-
Uncorrected distance visual acuity
References
Hyun J, Lim DH, Eo DR, et al. A comparison of visual outcome and rotational stability of two types of toric implantable collamer lenses (TICL) : V4 versus V4c. PLoS One. 2017;12(8):e0183335.
Navas A, Munoz-Ocampo M, Graue-Hernandez EO, et al. Spontaneous rotation of a Toric implantable Collamer Lens. Case Rep Ophthalmol. 2010;1(2):99–104.
Hashem AN, El Danasoury AM, Anwar HM. Axis alignment and rotational stability after implantation of the toric implantable collamer lens for myopic astigmatism. J Refract Surg. 2009;25(10 Suppl):S939–43.
Packer M. The implantable Collamer Lens with a central port: review of the literature. Clin Ophthalmol. 2018;12:2427–38.
Ma JJ, Tseng SS. Simple method for accurate alignment in toric phakic and aphakic intraocular lens implantation. J Cataract Refract Surg. 2008;34(10):1631–6.
Sheng XL, Rong WN, Jia Q, et al. Outcomes and possible risk factors associated with axis alignment and rotational stability after implantation of the Toric implantable collamer lens for high myopic astigmatism. Int J Ophthalmol. 2012;5(4):459–65.
Dougherty PJ, Rivera RP, Schneider D, et al. Improving accuracy of phakic intraocular lens sizing using high-frequency ultrasound biomicroscopy. J Cataract Refract Surg. 2011;37(1):13–8.
Park SC, Kwun YK, Chung ES, et al. Postoperative astigmatism and axis stability after implantation of the STAAR Toric implantable Collamer Lens. J Refract Surg. 2009;25(5):403–9.
Zhang X, Chen X, Wang X, et al. Analysis of intraocular positions of posterior implantable collamer lens by full-scale ultrasound biomicroscopy. BMC Ophthalmol. 2018;18(1):114.
Wang Z, Chung C, Lin J, et al. Quantitative measurements of the Ciliary body in eyes with acute primary-angle closure. Invest Ophthalmol Vis Sci. 2016;57(7):3299–305.
He N, Wu L, Qi M, et al. Comparison of Ciliary body anatomy between American Caucasians and ethnic Chinese using ultrasound biomicroscopy. Curr Eye Res. 2016;41(4):485–91.
Acknowledgements
Not applicable.
Funding
This study was financially supported by grants from the Science Research Foundation of Aier Eye Hospital Group (Grant NO.AF1909D2).
Author information
Authors and Affiliations
Contributions
QC performed the examination and surgery of the patient, and was a major contributor to writing the manuscript. QYZ and ZW collected the data and helped in designing of tables and Figs. CP provided statistical analysis. XHL collected data. WNT Critically revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Institutional review board approval from the Hankou Aier Eye Hospital was obtained and the tenets of the Declaration of Helsinki were followed.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consents is available for review by the Editor of the journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chen, Q., Zeng, Q., Wang, Z. et al. Spontaneous rotation of a toric implantable collamer lens related to abnormal ciliary body morphology: a case report. BMC Ophthalmol 20, 350 (2020). https://doi.org/10.1186/s12886-020-01597-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-020-01597-5