Abstract
Background
The object of this study is to investigate the effect of early bleb parameters measured by three-dimensional anterior-segment optical coherence tomography on the surgical success of trabeculectomy.
Methods
This retrospective study included 45 patients with 19 of exfoliation glaucoma, 17 of primary open angle glaucoma, 4 of neovascular glaucoma, 4 of uveitic glaucoma and 1 of glaucoma caused from familial amyloid polyneuropathy who underwent trabeculectomy. Bleb parameters, such as total bleb height, the position and the width of filtration openings on the scleral flap, bleb wall thickness, fluid-filled cavity height, and bleb wall intensity were assessed by three-dimensional anterior-segment optical coherence tomography 0.5 months after trabeculectomy, and were subjected to a Cox proportional hazard model as potential prognostic factors. Surgical success was defined as: IOP < 21 mmHg (A), < 18 mmHg (B), < 15 mmHg (C) with (qualified success) or without medication (complete success). Complete failure was defined as hypotony and additional glaucoma surgeries required.
Results
The width of filtration openings was identified as a prognostic factor for all criteria. By multivariable analysis, the width of the filtration openings was a prognostic factor in all criteria tested, and the preoperative IOP were significant prognostic factors for surgical success in qualified success in criteria B and C. Separate from the median widths of filtration openings, wide filtration opening showed significant survival ratio for qualified success in criteria A and B and for complete success in all criteria, respectively.
Conclusions
The width of filtration opening at an early stage is a prognostic factor for surgical success of trabeculectomy.
Similar content being viewed by others
Background
Trabeculectomy is one of the standard surgical modalities worldwide for glaucoma to prevent the progression of visual loss by lowering intraocular pressure (IOP). After a trabeculectomy, aqueous humor flows into the filtering bleb, consisting of the fluid-filled cavity, the scleral flap, and the wall of conjunctival tissue, and is then absorbed into surrounding tissues. Because the IOP-lowering effect of a trabeculectomy depends on the outflow volume of aqueous humor through the filtering bleb, management of the bleb is a key for surgical success. The function of the bleb is related to its morphology and its internal structures; thus, filtering blebs have been observed clinically by various imaging methods, such as slit-lamp examination, photography, ultrasound biomicroscopy (UBM), and optical coherence tomography (OCT) [1,2,3,4,5,6,7,8,9]. Among the OCT devices, three-dimensional anterior segment OCT (3D AS-OCT) can be useful to identify the aqueous route after a trabeculectomy and exploring the bleb morphology (internal and external) [10, 11].
Our previous studies revealed that the width of the filtration openings on the scleral flap, detectable using 3D AS-OCT, decreased in a time-dependent manner and that the width at an early stage correlated with future IOP [12, 13]. Thus, early bleb parameters may be potential prognostic factors for surgical success after trabeculectomy. However, whether these parameters actually affect the success after trabeculectomy, according to various criteria, remains unclear. Here, we report the predictive value of the width of the filtration openings on surgical results in patients with open angle glaucoma using a Cox proportional hazard model.
Methods
The Institutional Review Board of Kumamoto University approved the present study. Every investigation adhered to the tenets of the Declaration of Helsinki. Included were patients who received trabeculectomy with mitomycin C between January 2012 and October 2012 at the Kumamoto University Hospital, with analyzable 3D AS-OCT (Casia; Tomey, Nagoya, Japan) images of bleb 2 weeks after trabeculectomy, and be followed more than 1 year. Patients who had undergone combined surgery of trabeculectomy and phacoemulsification were excluded. Data were collected from medical records. When both eyes in one patient met the criteria, one eye treated first was included in this analysis. Prior to analyses, all patient data were anonymized by an independent person of the authors.
Trabeculectomy and postoperative management were performed as described previously [12]. Briefly, a limbus-based or fornix-based conjunctival flap was made, after which a single triangle scleral flap was made. Exposed tissues were treated with 0.04% mitomycin C for 4 min, and subsequently the tissues were washed by balanced salt solution (200 mL). Then, a trabecular block and peripheral iris were excised. Finally, the scleral flap and conjunctival flap were sutured by 10–0 nylon. In all cases, antibiotic eye drop and betamethasone eye drop were used 4 times a day for 3 months.
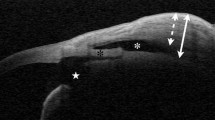
We evaluated OCT images using CASIA Bleb Assessment Software, ver. 4.0 L, (Tomey), as described previously [12, 13]. Briefly, consecutive filtration openings (pits and/or troughs in the fluid-filled cavities) on the scleral flap were examined, and width of the filtration opening was determined. After identification of the filtration openings, reviewers measured the total bleb height, fluid-filled cavity height, bleb wall thickness, and bleb wall intensity in the horizontal image at the center of the filtration opening, or at the center of the scleral flap when the filtration opening was unidentifiable (Fig. 1). Bleb wall intensity was automatically calculated as a mean of optical intensity in the selected area by a built-in software. The mean values of the bleb parameters from three independent reviewers were utilized for further analysis.
a Schematic description of a triangle scleral flap in the filtering bleb, and the width of filtration opening (blue box). b-d. An OCT image of the filtering bleb in the C-scan image showing a triangle scleral flap (b), and in the horizontal image (c, d). The red and blue lines indicate the horizontal and vertical axes, respectively. The yellow line represents the z-axis for C-scan image (b). The cross points of the colored lines indicate filtration opening
We defined surgical success along the World glaucoma Association guidelines as described previously [14]. Briefly, an IOP of < 21 mmHg (criterion A), < 18 mmHg (criterion B), or < 15 mmHg (criterion C) with (qualified success) or without (complete success) the use of topical ocular hypotensive medication(s). Follow up was stopped when any additional non-glaucoma related surgery was performed. We defined complete failure as the requirement for additional glaucoma surgeries including needle bleb revision and hypotony less than 4 mmHg. The IOPs obtained at 2 months or more after trabeculectomy were utilized to avoid any effect of short-term postoperative IOP fluctuations for this definition of surgical success. We used Kaplan-Meier survival-curve analysis and the Cox proportional hazards test to evaluate the cumulative success probability and to estimate the effect of prognostic factors in the univariable analysis. We analyzed the following variables as potential prognostic factors for surgical success: gender, age at the time of the trabeculectomy, history of cataract surgery, preoperative IOP value, design of scleral flap, and 3D AS-OCT parameters. Potential prognostic factors for surgical success (P < 0.10 by univariable analysis) were assessed using subsequent multivariate analysis. We analyzed data by the JMP (ver. 10) statistical package (SAS Institute, Cary, NC). A probability (P) value of < 0.05 was considered to indicate statistical significance.
Results
In total, 52 eyes (52 patients) were enrolled, and 45 eyes completed more than 1-year of follow-up (Table 1). Seven eyes (15.6%) were excluded from the analysis because of loss to follow-up or failure to acquire reliable 3D AC-OCT images during the observational period. In 45 eyes, needling bleb revisions for 3 eyes, repeat trabeculectomy for 7 eyes, additional glaucoma drainage-device surgery for 4 eyes, a conjunctival bleb reconstruction for 1 eye, cataract surgery for 7 eyes and an intraocular lens repositioning for 1 eye were conducted. Two eyes were considered surgical failures due to postoperative hypotony.
In the Cox proportional hazards test, univariate analysis indicated that the width of the filtration openings was a significant prognostic factor for surgical success of the trabeculectomy (Table 2). The lower preoperative IOP had a potential to relate to qualified success in criteria B and C and for complete success in criterion B (P < 0.10). Thus, we assessed influence of width of filtration opening and preoperative IOP by multivariate analysis. The width of the filtration openings was a prognostic factor in all criteria tested, and the lower preoperative IOP were significant prognostic factors for qualified success in criteria B and C (Table 3).
Then we subdivided the cases into two groups: those with wide filtration openings (greater than the median width of filtration openings, 1.78 mm; n = 22) and those with narrow filtration openings (= < 1.78 mm; n = 23). Kaplan-Meier survival analysis and Wilcoxon tests showed significant differences in success probabilities between the two groups for qualified success in criteria A and B and for complete success in all criteria, respectively (Fig. 2). The numbers at risk in the survival analysis are shown in Table 4. Typical images of the successful bleb with wide filtration opening and the failing bleb with narrow opening are shown (Fig. 3).
Kaplan-Meier survival plots of groups according to the width of the filtration openings on the scleral flap: eyes with filtration opening of > 1.78 mm, the median value of the patients (22 patients, solid line), and eyes with filtration opening of = < 1.78 mm (23 patients, dotted line). The y-axis indicates the success ratio (%), and the x-axis indicates the number of days after trabeculectomy
a Typical OCT images of the successful bleb with wide filtration opening at 2 weeks after trabeculectomy. The red and blue lines represent the horizontal and vertical axes, respectively. The yellow line indicates the z-axis of the data for C-scan images. The cross points of the colored lines show filtration openings, that continued to neighboring horizontal sections (not shown). IOP was 10 mmHg at 1 year after trabeculectomy without additional surgery or medication. b Typical OCT images of the failing bleb with no detectable filtration opening at 2 weeks after trabeculectomy. This case required needling bleb revision at 2 weeks after trabeculectomy
Discussion
In the previous study, the width of filtration opening at 0.5 months after trabeculectomy was inversely-correlated with the IOP value at 12 months after the operation [13]. In the present study, the long term IOP was also related with the width of filtration opening at 0.5 months after trabeculectomy. On the other hand, other bleb parameters including the thickness and intensity of the bleb wall did not show the relationship with the long term IOP control. That was contradicted with the previous knowledge conducted by OCT. [8, 15] The disaggregation might be given by the poverty of sample numbers in the present study. However, in spite of the limitation of the number or the observation periods, the significant correlation of the widths of filtration opening and long-term IOP is of great interest. Thus, the width of filtration opening might be more powerful than other bleb parameters to predict surgical success. We may be able to predict surgical success by assessing bleb by 3D AS-OCT.
In the present study, preoperative IOP was an independent prognostic factor for long term surgical success. In agreement with the present study, a previous prospective cohort study revealed that preoperative higher IOP was a risk factor for trabeculectomy success [16]. Based on these findings, glaucoma eyes with higher IOPs resistant to topical treatment may be more prone to excessive wound healing after filtration surgery. This may be due to presence of cytokines in the aqueous humor that have been associated with both higher IOPs and excessive wound healing. Of note, the concentration of aqueous MCP-1 tended to be high in refractory glaucoma types, including neovascular glaucoma and uveitic glaucoma [17,18,19], and was related to the width of filtration openings [13]. Indeed, the MCP-1 concentration in aqueous humor was a prognostic factor in open angle glaucoma [20].
In the past studies, the findings in the AS-OCT images of bleb wall were correlated to the IOP control [8, 9, 15]. Napoli et al retrospectively examined 20 filtering blebs using 2 types of OCTs working at a wavelength of 840 and 1310 nm, and found a significant association between good functionality and cystoid type at that time with both devices. In this study, the period between surgery and AS-OCT examination ranged from 3 months to 2 years [8]. These results may agree with the results of our past prospective study, presenting that the high-intensity bleb wall at 12 months post-trabeculectomy reflected the IOP and bleb wall vascularity at that time [21]. On the other hand, Nakano et al prospectively examined 48 eyes, and reported that blebs with uniform reflectivity at 2 weeks were significantly more likely to have worse function at 6 months [9]. In addition, Narita et al retrospectively assessed 99 eyes, and found that the striping phenomenon of the bleb wall at 2 weeks post-trabeculectomy was significantly associated with success at 1 year post-trabeculectomy [15]. These results suggest that the early bleb wall condition is a predictive factor of surgical success. Though bleb wall thickness or intensity did not relate to later IOP control in the present study, further large-scale prospective studies may clarify the relationship between early bleb wall condition and later IOP control.
The limitations of the present study were a relatively small sample size (45 eyes) and the retrospective study design. Additionally, the follow-up period (37 months in average) may not be enough to predict long-term outcomes, because the progression of wound healing after trabeculectomy is chronic, extending for years in some cases. Thus, we should interpret the data with caution. Prospective larger-scale studies with a longer follow-up period are essential.
Conclusion
The width of filtration opening at an early stage may be a prognostic factor for surgical success of trabeculectomy in eyes with open-angle glaucoma.
Availability of data and materials
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
Abbreviations
- 3D AS-OCT:
-
Three-dimensional anterior segment optical coherence tomography
- IOP:
-
Intraocular pressure
- OCT:
-
Optical coherence tomography
- UBM:
-
Ultrasound biomicroscopy
References
Picht G, Grehn F. Classification of filtering blebs in trabeculectomy: biomicroscopy and functionality. Curr Opin Ophthalmol. 1998;9:2–8.
Cantor LB, Mantravadi A, WuDunn D, Swamynathan K, Cortes A. Morphologic classification of filtering blebs after glaucoma filtration surgery: the Indiana bleb appearance grading scale. J Glaucoma. 2003;12:266–71.
Wells AP, Ashraff NN, Hall RC, Purdie G. Comparison of two clinical bleb grading systems. Ophthalmology. 2006;113:77–83.
Sacu S, Rainer G, Findl O, Georgopoulos M, Vass C. Correlation between the early morphological appearance of filtering blebs and outcome of trabeculectomy with mitomycin C. J Glaucoma. 2003;12:430–5.
Yamamoto T, Sakuma T, Kitazawa Y. An ultrasound biomicroscopic study of filtering blebs after mitomycin C trabeculectomy. Ophthalmology. 1995;102:1770–6.
Leung CK, Yick DW, Kwong YY, Li FC, Leung DY, Mohamed S, Tham CC, Chung-chai C, Lam DS. Analysis of bleb morphology after trabeculectomy with Visante anterior segment optical coherence tomography. Br J Ophthalmol. 2007;91:340–4.
Singh M, Chew PT, Friedman DS, Nolan WP, See JL, Smith SD, Zheng C, Foster PJ, Aung T. Imaging of trabeculectomy blebs using anterior segment optical coherence tomography. Ophthalmology. 2007;114:47–53.
Nakano N, Hangai M, Nakanishi H, Inoue R, Unoki N, Hirose F, Ojima T, Yoshimura N. Early trabeculectomy bleb walls on anterior-segment optical coherence tomography. Graefes Arch Clin Exp Ophthalmol. 2010;248:1173–82.
Napoli PE, Zucca I, Fossarello M. Qualitative and quantitative analysis of filtering blebs with optical coherence tomography. Can J Ophthalmol. 2014;49:210–6.
Miura M, Kawana K, Iwasaki T, Kiuchi T, Oshika T, Mori H, Yamanari M, Makita S, Yatagai T, Yasuno Y. Three-dimensional anterior segment optical coherence tomography of filtering blebs after trabeculectomy. J Glaucoma. 2008;17:193–6.
Kawana K, Kiuchi T, Yasuno Y, Oshika T. Evaluation of trabeculectomy blebs using 3-dimensional cornea and anterior segment optical coherence tomography. Ophthalmology. 2009;116:848–55.
Inoue T, Matsumura R, Kuroda U, Nakashima K, Kawaji T, Tanihara H. Precise identification of filtration openings on the scleral flap by three-dimensional anterior segment optical coherence tomography. Invest Ophthalmol Vis Sci. 2012;53:8288–94.
Kojima S, Inoue T, Nakashima K, Fukushima A, Tanihara H. Filtering blebs using 3-dimensional anterior-segment optical coherence tomography: a prospective investigation. JAMA Ophthalmol. 2015;133:148–56.
Nishizawa A, Inoue T, Ohira S, Takahashi E, Saruwatari J, Iwao K, Tanihara H. The influence of phacoemulsification on surgical outcomes of trabeculectomy with mitomycin-C for uveitic glaucoma. PLoS One. 2016;11:e0151947.
Narita A, Morizane Y, Miyake T, Seguchi J, Baba T, Shiraga F. Characteristics of early filtering blebs that predict successful trabeculectomy identified via three-dimensional anterior segment optical coherence tomography. Br J Ophthalmol. 2018;102:796–801.
Sugimoto Y, Mochizuki H, Ohkubo S, Higashide T, Sugiyama K, Kiuchi Y. Intraocular pressure outcomes and risk factors for failure in the collaborative bleb-related infection incidence and treatment study. Ophthalmology. 2015;122:2223–33.
Inoue T, Kawaji T, Inatani M, Kameda T, Yoshimura N, Tanihara H. Simultaneous increases in multiple proinflammatory cytokines in the aqueous humor in pseudophakic glaucomatous eyes. J Cataract Refract Surg. 2012;38:1389–97.
Ohira S, Inoue T, Shobayashi K, Iwao K, Fukushima M, Tanihara H. Simultaneous increase in multiple proinflammatory cytokines in the aqueous humor in neovascular glaucoma with and without intravitreal bevacizumab injection. Invest Ophthalmol Vis Sci. 2015;56:3541–8.
Ohira S, Inoue T, Iwao K, Takahashi E, Tanihara H. Factors influencing aqueous proinflammatory cytokines and growth factors in uveitic glaucoma. PLoS One. 2016;11:e0147080.
Inoue T, Kawaji T, Tanihara H. Monocyte chemotactic protein-1 level in the aqueous humour as a prognostic factor for the outcome of trabeculectomy. Clin Exp Ophthalmol. 2014;42:334–41.
Watanabe-Kitamura F, Inoue T, Kojima S, Nakashima KI, Fukushima A, Tanihara H. Prospective 3D investigation of bleb wall after trabeculectomy using anterior-segment OCT. J Ophthalmol. 2017;2017:8261364.
Acknowledgements
None.
Funding
This work was supported by Grants-in-Aid for Scientific Research from the Ministry of Health, Labor and Welfare, Tokyo, Japan. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
UT and TI drafted the manuscript. UT, SK, AF, KN, and KI examined the patient, and collected data. HT and TI conceived of the study and interpreted the patient data. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures conformed to the Declaration of Helsinki. This study was approved by the Institutional Review Board of Kumamoto University. Written informed consent was not obtained due to the retrospective manner of the study. Alternatively, this study was carried out by the opt-out method of our department website. The medical records accessed and used in this study are not available in public databases. Patient data were de-identified upon data collection.
Consent for publication
Not Applicable.
Competing interests
Dr. Tanihara has received consulting fees from Kowa, and MSD, board membership fees from Senju Pharmaceutical, Santen Pharmaceutical, Alcon Japan, and Pfizer Japan, and research grant from Kowa, Senju Pharmaceutical, Santen Pharmaceutical, Alcon Japan, Pfizer Japan, and Otsuka Pharmaceutical. Dr. Inoue has received research grant from Novartis Pharma. Other authors have no financial interest. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Tsutsumi-Kuroda, U., Kojima, S., Fukushima, A. et al. Early bleb parameters as long-term prognostic factors for surgical success: a retrospective observational study using three-dimensional anterior-segment optical coherence tomography. BMC Ophthalmol 19, 155 (2019). https://doi.org/10.1186/s12886-019-1159-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-019-1159-1